Abstract
Objective:
To compare the accuracy of pulse oximetry oxygen saturation (SpO2) measured on the wrist compared with the ipsilateral palm, and SpO2 measured on the ankle compared with the ipsilateral sole.
Study Design:
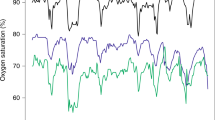
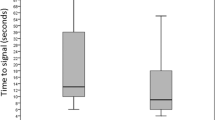
In this prospective observational study, neonates admitted to the neonatal intensive care unit were enrolled. We recorded SpO2 (Masimo Radical-7 pulse oximeter) detected at the palm and ipsilateral wrist initially, then at 30 s, and at 1 min, and we repeated the same procedure over the sole and ipsilateral ankle. We recorded the time to obtain the SpO2 readings from all these sites. Regression analysis was performed to determine the relationship between paired SpO2 measurements. The mean difference (bias) and standard deviation of the paired SpO2 differences (precision) were calculated (Bland–Altman plots).
Result:
A total of 150 patients (birth weight 2381±1020 g, gestational age 34.3±4.3 weeks, median postnatal age 3.5 days (25th–75th percentile 1–16 days)) were enrolled. There was a good correlation between SpO2 measured at the palm versus the wrist (r=0.95, P<0.001 (right); r=0.97, P< 0.001 (left)) and between SpO2 measured at the sole versus the ankle (r=0.92, P<0.001 (right); r=0.91, P<0.001 (left)). There was also a good agreement between paired SpO2 measurements from these sites. The bias and precision for SpO2 at the right palm and right wrist was 0.08±0.94% and for the left palm and left wrist 0.22±0.87%. Similarly, the bias and precision for SpO2 at the right sole and right ankle was −0.03±0.93% and for the left sole and left ankle was −0.01±0.93%.
Conclusion:
Our results show that the wrist and ankle can be used as alternative sites to measure SpO2 in newborn infants in place of the routinely used palm or sole.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Neff TA . Routine oximetry: a fifth vital sign? Chest 1988; 94: 227a–227.
Hay Jr WW, Brockway J, Eyzaguirre M . Neonatal pulse oximetry: accuracy and reliability. Pediatrics 1989; 83: 717–722.
Tobin MJ . Respiratory monitoring. JAMA 1990; 264: 244–251.
Severinghaus JW, Kelleher JF . Recent developments in pulse oximetry. Anesthesiology 1992; 76: 1018–1038.
Iyer P, McDougall P, Loughnan P, Mee RB, Al-Tawil K, Carlin J . Accuracy of pulse oximetry in hypothermic neonates and infants undergoing cardiac surgery. Crit Care Med 1996; 24: 507–511.
Durand M, Ramanathan R . Pulse oximetry for continuous oxygen monitoring in sick newborn infants. J Pediatr 1986; 109: 1052–1056.
Dawson JA, Davis PG, O’Donnell CP, Kamlin CO, Morley CJ . Pulse oximetry for monitoring infants in the delivery room: a review. Arch Dis Child Fetal Neonatal Ed 2007; 92: F4–F7.
Barker SJ, Tremper KK, Hyatt J . Effects of methemoglobinemia on pulse oximetry and mixed venous oximetry. Anesthesiology 1989; 70: 112–117.
Wukitsch MW, Petterson MT, Tobler DR, Pologe JA . Pulse oximetry: analysis of theory, technology and practice. J Clin Monit 1988; 4: 290–301.
Barker SJ, Shah NK . Effects of motion on the performance of pulse oximeters in volunteers. Anesthesiology 1996; 85: 774–781.
Mengelkoch LJ, Martin D, Lawler J . A review of the principles of pulse oximetry and accuracy of pulse oximeter estimates during exercise. Phys Ther 1994; 74: 40–49.
Rabi Y, Yee W, Chen SY, Singhal N . Oxygen saturation trends immediately after birth. J Pediatr 2006; 148: 590–594.
Gehring H, Hornberger C, Matz H, Konecny E, Schmuker P . The effect of motion artifact and low perfusion on the performance of new generation of pulse oximeters in volunteers undergoing hypoxemia. Respir Care 2002; 47: 48–60.
O’Donnell CP, Kamlin CO, Davis PG, Morley CJ . Obtaining pulse oximetry data in neonates: a randomised crossover study of sensor application techniques. Arch Dis Child Fetal Neonatal Ed 2005; 90: F84–F85.
Bland JM, Altman DG . Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986; 1: 307–310.
Harikumar G, Egberongbe Y, Nadel S, Wheatley E, Moxham J, Greenough A et al. Tension-time index as a predictor of extubation outcome in ventilated children. Am J Respir Crit Care Med 2009; 180: 982–988.
Wilkins CJ, Moores M, Hanning CD . Comparison of pulse oximeters: effects of vasoconstriction and venous engorgement. Br J Anaesth 1989; 62: 439–444.
Warley AR, Mitchell JH, Stradling JR . Evaluation of the Ohmeda 3700 pulse oximeter. Thorax 1987; 42: 892–896.
Severinghaus JW, Naifeh KH . Accuracy of response of six pulse oximeters to profound hypoxia. Anesthesiology 1987; 67: 551–558.
Young D, Jewkes C, Spittal M, Blogg C, Weissman J, Gradwell D . Response time of pulse oximeters assessed using acute decompression. Anesth Analg 1992; 74: 189–195.
Reynolds LM, Nicolson SC, Steven JM, Escobar AE, McGonigle ME, Jobes DR . Influence of sensor site location on pulse oximetry kinetics in children. Anesth Analg 1993; 76: 751–754.
Poets CF, Southall DP . Noninvasive monitoring of oxygenation in infants and children: practical considerations and areas of concern. Pediatrics 1994; 93: 737–746.
Guan Z, Baker K, Sandberg WS . Case report: Misalignment of disposable pulse oximeter probes results in false saturation readings that influence anesthetic management. Anesth Analg 2009; 109: 1530–1553.
Moyle JTB . Uses and abuses of pulse oximetry. Arch Dis Child 1996; 74: 77–80.
Mardirossian G, Schneider RE . Limitations of pulse oximetry. Anesth Prog 1992; 39: 194–196.
Acknowledgements
We thank the families and our newborn intensive care unit staff for their support and cooperation with the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Presented at the Annual Meeting of the Pediatric Academic Societies, Vancouver, British Columbia, Canada, May 2010.
Rights and permissions
About this article
Cite this article
Phattraprayoon, N., Sardesai, S., Durand, M. et al. Accuracy of pulse oximeter readings from probe placement on newborn wrist and ankle. J Perinatol 32, 276–280 (2012). https://doi.org/10.1038/jp.2011.90
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2011.90