Abstract
Background
General movements (GMs) in infants occur as fidgety movements (FMs) between postterm 9 and 20 weeks. We aimed to evaluate FMs and motor repertoire in infants with cystic fibrosis (CF) and their relation with clinical findings.
Methods
Demographic and clinical characteristics were recorded. FMs and motor repertoire were analyzed from a 5-min video recording of each infant. Videos were rated based on the Prechtl General Movement Assessment and motor optimality score (MOS) was calculated.
Results
The analysis included 18 infants with CF and 20 healthy infants at postterm age of 3−5 months. MOS was significantly lower in the infants with CF compared to controls (p < 0.05). Fifty percent of the infants with CF had abnormal or absent/sporadic FMs. MOS was negatively associated with hospitalization duration (r = −0.378, p = 0.036); and positively associated with vitamin A level in CF infants (r = 0.665, p = 0.026).
Conclusions
Infants with genetically anticipated severe CF phenotype tended to have lower MOS. MOS may be used in addition to genetic testing to predict disease severity in infants with CF. Infants with CF, absent/sporadic FMs, and lower MOS could be considered for planning specific age-adequate early intervention programs.
Impact
-
Motor repertoire was age-inadequate in infants with cystic fibrosis (CF).
-
50% of infants with CF had abnormal or absent/sporadic fidgety movements (FMs).
-
Motor optimality score (MOS) was positively associated with vitamin A level and negatively correlated with hospitalization duration in infants with CF.
-
MOS tended to decrease as genetically anticipated disease severity increased; thus, MOS might enable us to predict disease severity in CF. The relationship between motor repertoire and phenotype and genotype is unclear and warrants further study.
-
CF infants with absent/sporadic FMs, and lower MOS could be considered for planning early intervention.
Similar content being viewed by others
Introduction
Cystic fibrosis (CF) is a systemic, progressive, and life-threatening autosomal recessive disease caused by a mutation of the gene which encodes CF transmembrane regulator (CFTR) protein, resulting in CFTR dysfunction.1 CF transmembrane regulator serves as an ion channel protein throughout the body, and dysfunction of CFTR results in multisystem manifestations and comorbidities such as pulmonary, pancreatic, hepatobiliary, and gastrointestinal diseases in patients with CF.
The developing nervous system produces general movements (GMs), which emerge at 9 weeks gestation and persist until about 20 weeks postterm.2 General movements are referred as preterm GMs from preterm birth to term-equivalent age, as writhing movements (WMs) from term to approximately 8 weeks postterm. At 6−9 weeks postterm, a new GM pattern called fidgety movements (FMs) emerges and continues until 20 weeks.3
Fidgety movements are tiny to small movements of the head, neck, shoulder, trunk, and limbs with variable acceleration and moderate speed in all directions. Although FMs can be seen as early as postterm 6 weeks, they usually appear from postterm week 9 until the end of weeks 16−20. FMs fade in infants as antigravity muscle activation and voluntary movements begin to dominate.4,5,6 The absence of FMs is highly predictive of later neurological impairments.7,8 The motor repertoire of infants at 3−5 months includes not only FMs but also age-adequate movements patterns such as swipes, smiles, head rotation, wiggling/oscillating, mouth and tongue movements, or postural patterns such as head in midline, symmetrical body segments, and variable finger postures.3
There are a few studies in the literature examining neurodevelopment in patients with CF. In one study, hospitalization duration longer than 60 days, low stature, and low weight were significantly associated with motor delay in infants with CF.9 However, that study did not include a control group. A recently published study related to developmental and behavioral problems in preschool-age children with primary ciliary dyskinesia (PCD) and CF showed that delay in fine motor skills was more common in children with CF compared to healthy subjects.10
In the present study, we aimed to characterize the FMs and motor repertoire of infants with CF compared to controls from the ages of 3−5 months using the Prechtl General Movement Assessment (GMA). Specific questions were: (a) is there a difference in FMs and motor repertoire between infants with CF and controls and (b) is GMA of CF infants associated with vitamin A and vitamin E levels, hospitalization duration, or genetically anticipated disease severity?
Methods
Study design
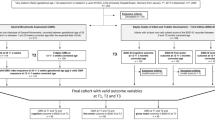
This case−control study was conducted at the Faculty of Physical Therapy and Rehabilitation, Developmental and Early Physiotherapy Unit between October 2017 and October 2018. Infants with CF were referred from the Hacettepe University, Department of Pediatric Pulmonology. The Hacettepe University Ethics Board approved this study (27.09.2017, GO 17/733-05), which is registered in the Clinical Trials (NCT03381157). Written informed consent was obtained from the legal guardians of all infants in the study.
Participants
Twenty clinically stable infants with CF and 20 healthy infants were assessed for eligibility. Two infants with CF were excluded because one died before the fidgety period began and the other infant’s parents did not appear for video recording. Therefore, 18 infants with CF at 12−19 weeks corrected postterm age (median = 14 weeks) and 20 healthy infants at 10−18 weeks corrected postterm age (median = 13 weeks) were analyzed using Prechtl GMA. The control group included infants who were followed in our unit until the age of 2 years, had typical developmental parameters and normal neurological outcome, and were confirmed as neurotypical by a pediatric neurologist. Clinical characteristics and videos of the control infants recorded at postterm 3−5 months of age were obtained from the Developmental and Early Physiotherapy Unit Database.
A power analysis program (G*Power, ver. 3.1., Universität Düsseldorf, Düsseldorf, Germany) was used to calculate the sample size based on two-tailed calculations. Based on 5% type I error and 80% power to detect was at least a correlation coefficient of 0.5, the required sample size for each group was 18.11
Study procedure
Demographic and clinical characteristics, including gender, types of birth, gestational and corrected age, weight at birth, weight, height and head circumference at assessment, maternal age, incubator history, and hospitalization history, were obtained from the parents and clinical records of the CF and control infants. Parental/sibling history, diagnostic age, and medications were recorded for the CF group.
Laboratory parameters
Infants were diagnosed as having CF by sweat test. The sweat test is mandatory for diagnostic confirmation and a sweat chloride value above 59 mmol/L is one of the diagnostic criteria for CF.12,13 In addition, vitamin A and E levels were obtained from clinical records in the CF group. As pancreatic insufficiency in CF leads to the risk of fat-soluble vitamin (A, D, E, and K) deficiency, these vitamins are routinely investigated and administered as supplements to CF patients, if required.14 CFTR mutations were also recorded in infants with CF. Clinical disease severity based on CFTR mutations was classified and described as follows: patients with two copies of class I, II, III mutations generally have almost no CFTR function due to defective CFTR production, ineffective CFTR processing, and impaired CFTR-Chlor regulation, respectively. Classes I, II, and III are associated with genetically anticipated severe phenotypes (more severe disease) in patients with CF. Although there are some CFTR functions including altered CFTR channel conduction, abnormal CFTR level (often splicing), and unstable CFTR protein in patients with class IV, V, and VI mutations, respectively, this is not enough to prevent all the consequences of CFTR dysfunction. Classes IV, V, and VI are associated with genetically anticipated mild phenotypes (less severe disease) in patients with CF.15,16
General movement assessment (GMA)
Five-minute video recordings were analyzed for both groups. The videos were analyzed based on the Prechtl GMA5 and motor optimality scores (MOS)17 were calculated according to motor optimality list including five subcategories: FMs, repertoire of co-occurring movements, quality of other movements, posture, and the movement character. FMs were evaluated as normal (12 points), abnormal (i.e., excessive amplitude, speed, and jerkiness) (4 points), or absent/sporadic (1 point). Repertoire of co-occurring movements was evaluated as age-adequate (4 points), reduced (2 points), or absent (1 point). The quality of other movements (except FMs) was scored according to: predominantly normal movement was scored as 4 points, an even number of normal and abnormal movements was scored as 2 points, and predominantly abnormal movement was scored as 1 point. Similarly, posture was evaluated as normal or abnormal and scored as 4 points if observed postural patterns were normal, 2 points if evenly mixed, and 1 point if predominantly abnormal. Overall movement character was scored as 4 points if all movements were smooth and fluent. Jerkiness, stiffness, and reduced complexity of movements were considered abnormal but not cramped-synchronized (CS) and scored as 2 points. Movements characterized by rigid movements of the limb and trunk muscles were considered CS and scored as 1 point. The resulting MOS ranged from a maximum of 28 (best possible performance) to a minimum of 5 (worst performance).17
A digital camera (NIKON-Coolpix-A100-Silver, Thailand) and tripod (HAMA-4133-Star-700 EF, China) were used for recordings. The videos were analyzed by two physiotherapists (A.M. and A.L.) who were specialists in pediatric physiotherapy and rehabilitation, with GMs certification and 15 years of experience in GMA. The examiners were blinded to the clinical characteristics of the infants. In case of disagreement on an infant’s assessment, they reviewed that infant to reach a consensus on final score.
Statistical methods
Statistical analyses were performed using the IBM SPSS Statistics 23.0 (SPSS, Chicago, IL, USA). The variables were tested with visual (histograms/probability plots) and analytical methods (Kolmogorov−Smirnov/Shapiro−Wilk test) to check normal distribution of variables. Descriptive data were presented as median and interquartile range or mean and standard deviation, as adequate. Mann−Whitney U test was used to compare ordinal parameters between the CF group and control group. Categorical variables were compared between the groups using chi-square test or Fisher’s exact test. Correlation coefficients and their significance were calculated using the Spearman test to investigate the relationships between non-normally distributed and/or ordinal variables. A p value of <0.05 was considered to be statistically significant.
Results
Gender, types of birth, gestational age, corrected age, birth weight, height, body weight, and head circumference did not differ significantly between the CF and control group (p > 0.05; Table 1). The diagnostic age in infants with CF was between 0 and 16 weeks (median = 5.75 weeks) (Table 2). Fifteen of the infants with CF (83.4%) had a history of hospitalization.
Admission frequency, number of hospitalizations, and hospitalization duration were higher in infants with CF than those of the control group (p < 0.01; Table 2). The reasons for admission or hospitalization were acute exacerbation and gastrointestinal and pulmonary complications.
Vitamin E and A levels were lower in the 13 CF infants whose records included these data (Table 2). Five of the infants with CF did not have vitamin E and A test results.
Infants in the CF group were receiving the following medications and supplements: pancreatic enzyme replacement therapy in 11 (61.1%), antibiotics in 5 (27.7%), dornase alfa in 6 (33.34%), bronchodilator in 2 (11.1%), multivitamin in 15 (83.34%), and salt supplement in 17 (94.4%). They also were referred to chest physiotherapy.
Motor optimality score was significantly lower in infants with CF (median = 18.5, range = 7–28) compared to the healthy infants (median = 26, range = 16–28) (p < 0.01; Table 3). Nine CF infants (50%) displayed normal FMs. One (5.6%) displayed abnormal FMs, and 8 (44.4%) displayed absent/sporadic FMs. In the control group, 19 infants (95%) had normal FMs, and only 1 (5%) had abnormal FMs. There was a significant difference in FMs score between the CF and control group (p < 0.01; Table 3). Repertoire of co-occurring movements was predominantly age-adequate or reduced in both the CF group and the control group (p > 0.05; Table 3). Quality of other movements (other than FMs) was predominantly normal in the CF group (83.3%) and control group (100%) (p > 0.05; Table 3). Fifteen infants with CF (83.3%) and 18 healthy infants (90%) had a normal posture (p > 0.05; Table 3). In addition, five infants in the CF group displayed smooth and fluent movement character (27.8%), and 13 infants (72.2%) displayed abnormal but not CS movement character in the CF group. Eleven neurotypical infants (55%) displayed smooth and fluent movement character and nine (45%) displayed abnormal but not CS movement character (p > 0.05; Table 3). We also compared the MOS of infants with CF + normal FMs (n = 9) and CF + abnormal + absent/sporadic FMs (n = 9). Infants with CF + normal FMs had significantly higher MOS (median = 26, range = 20–28) than infants with CF + abnormal + absent/sporadic FMs (median = 13, range = 7–17) (p < 0.001). In the CF group, MOS was positively associated with vitamin A level (r = 0.556; p = 0.048; Fig. 1) and negatively correlated with the hospitalization duration (r = −0.378; p = 0.036; Fig. 2), but not correlated with vitamin E level and sweat chloride values.
Nine (50%) of the 18 CF infants had data regarding classification of CFTR mutation and disease severity. These parameters in addition to the FMs and MOS in the CF infants are presented in Table 4. Based on CFTR mutation classes, clinical severity was severe in five infants and mild in four infants. Motor optimality score tended to be lower in infants with genetically anticipated severe phenotypes compared to the infants with genetically anticipated mild phenotypes (Table 4).
Discussion
The present study is the first case−control study to examine and compare FMs and motor repertoire between CF and healthy control group. Based on our findings, FMs score and MOS were lower in infants with CF than healthy infants.
Apart from FMs, other subcategories, including repertoire of co-occurring movements, quality of other movements, posture, and movement character, were similar between the CF group and the control group. Only half of the CF infants displayed normal FMs. All but one infant in the control group had normal FMs, and the single control infant with abnormal FMs had normal neurological outcome with typical neurodevelopment at 2 years of age. There was heterogeneity in the motor repertoire of infants with CF. Motor optimality score tended to be lower in infants with genetically anticipated severe phenotypes according to CFTR mutation classes. In a recently published paper, Einspieler et al. reported that Gross Motor Function Classification System (GMFCS) level was strongly correlated with MOS in children with cerebral palsy (CP). A MOS higher than 14 was most likely associated with GMFCS outcomes I or II (more severe functional impairment). Motor optimality score was reported to contribute to providing later CP prognosis, type, and severity in this study.17 This relationship between functional impairment and MOS in CP can be considered in CF as the relationship among genotype class, genetically anticipated phenotype, and MOS. To date, there has been no data about this relationship in the literature. One study reported that there was no association between CFTR functional genotype class and maximal exercise capacity in patients with CF but that overall, maximal exercise capacity was lower in patients with at least one copy of an F508del-CFTR mutation and a single class V mutation.18 Our results indicated that MOS decreases as the severity of the disease increases in infants with CF. Therefore, MOS might enable us to predict disease severity in infants with CF apart from genetic testing. However, it is still not clear exactly how motor repertoire and MOS are associated with genetically anticipated phenotype and genotype class in CF, and this may be an interesting topic for future research.
A few previous studies have investigated motor development and performance in patients with CF.9,10,19 The first of these studies revealed that motor performance was better in children with CF than healthy peers. Gruber et al.19 attributed this speculative outcome to the chest physiotherapy received by children with CF. These results cannot be compared with the findings of the present study because of the differences in the chronological age of the studied groups. The second study showed that motor development delay can occur in infants with CF.9 Although the findings were similar to those of our study, the assessment tool was different and the study lacked a healthy control group, sufficient sample size, and homogeneous age distribution. Finally, in a recently published study, gross motor domain delay was not observed in the CF group but delay in fine motor domain was more common in children with CF compared to healthy subjects.10 Groen et al.8 showed that abnormal GMs were associated with coordination problems and fine manipulative disability at 9–12 years of age. Einspieler et al.20 concluded that whether GMs were predictive of minor neurological dysfunction (MND) or fine motor disability was still a controversial issue. Further follow-up studies investigating the relationship between GMs and fine motor skills in CF may clarify this issue.
An infant’s development is influenced by not only individual factors related to biological and genetic characteristics, but also environmental factors including the microsystem environment (family, home, surroundings, peers, etc.) and the exosystem environment (extended family, neighborhood, school, etc.), as well as the macrosystem environment (community, economic system, culture, etc.).21 Furthermore, Thomazinho et al.9 reported that patients with CF had a high prevalence of hospitalization in first year of life (73.3%) and a positive correlation between hospitalization and motor delay, suggesting that hospitalization is a factor that might lead to motor delay. In the present study, infants with CF had higher hospital admission frequency, number of admissions, and duration. Increased hospitalization duration was accompanied by a decrease in MOS in infants with CF. A supportive and enriched environment are necessary for typical development, so the lower MOS and poorer motor repertoire in the CF infants may be attributable to hospitalization.
In patients with CF, deficiency of vitamin E and A may lead to increased risk for some disorders such as neurologic, cognitive, and visual impairments.22,23 In a study investigating the effect of vitamin E deficiency on neurological function in patients with CF, it was reported that while low vitamin E levels led to an increase in mean nerve conduction latency, there was a decrease in nerve action potential amplitude in the sural nerve.24 Also, bioactive metabolite of vitamin (retinoid acid) is an important and potent modulator of gene expression, neurogenesis, neuron survival, and synaptic plasticity in the brains of animals.25 In our study, although vitamin E and A levels were low in infants with CF, MOS was only associated with vitamin A level, but not vitamin E level. This may be due to the small sample size, as we could not obtain vitamin E and A data for all of the CF infants. Further studies with larger sample sizes are needed to focus on the effects of vitamin E and A deficiency and their relation with FMs and motor repertoire in infants with CF.
The present study has certain limitations that should be mentioned. As discussed above, vitamin E and A levels were not available for all infants with CF. Similarly, the genetic test results had not been returned for some of the infants in the CF group. We did not perform some laboratory tests in healthy infants due to ethical considerations. Furthermore, some infants in both groups were born preterm. Although we are aware that this is a confounding factor, there was not a sufficient sample size to divide into subgroups and compare their GMA as preterm and term separately. Finally, one of the CF infants was recorded at the age of 19 weeks, and this might be late to assess FMs. Although the initial results of our study suggest a relationship between motor repertoire and genotype, genetically anticipated phenotype, and vitamin A, the evidence is not sufficient to generalize our findings to the entire CF infant population.
Conclusion
In conclusion, there was heterogeneity in the motor repertoires of infants with CF. Although the reasons for absent/sporadic FMs are unclear, MOS was positively associated with vitamin A level and negatively correlated with the hospitalization duration. Motor optimality score tended to decrease as genetically anticipated disease severity increased; thus, MOS might enable us to predict disease severity in infants with CF apart from genetic testing. The relationship between motor repertoire and phenotype and genotype in CF is still unclear and warrants further study. Cystic fibrosis infants with absent/sporadic FMs, and lower MOS could be considered for planning specific age-adequate early intervention programs.
References
Rowe, S. M., Miller, S. & Sorscher, E. J. Cystic fibrosis. N. Engl. J. Med. 352, 1992–2001 (2005).
Einspieler, C. & Prechtl, H. F. Prechtl’s assessment of general movements: a diagnostic tool for the functional assessment of the young nervous system. Ment. Retard. Dev. Disabil. Res. Rev. 11, 61–67 (2005).
Einspieler, C., Marschik, P. B. & Prechtl, H. F. Human motor behavior: prenatal origin and early postnatal development. J. Psychol. 216, 147–153 (2008).
Prechtl, H. F. et al. An early marker for neurological deficits after perinatal brain lesions. Lancet 349, 1361–1363 (1997).
Einspieler, C., Prechtl, H., Bos, A., Ferrari, F. & Cioni, G. Prechtl’s Method on the Qualitative Assessment of General Movements in Preterm, Term and Young Infants 1st edn (Mac Keith Press, London, 2004).
Einspieler, C., Peharz, R. & Marschik, P. B. Fidgety movements—tiny in appearance, but huge in impact. J. Pediatr. 92, 64–70 (2016).
Herrero, D. et al. The motor repertoire in 3-to 5-month old infants with Down syndrome. Res. Dev. Disabil. 67, 1–8 (2017).
Groen, S. E., de Blécourt, A. C., Postema, K. & Hadders-Algra, M. General movements in early infancy predict neuromotor development at 9 to 12 years of age. Dev. Med. Child. Neurol. 47, 731–738 (2005).
de Almeida Thomazinho, P., de Miranda Chaves, C. R. M., Pássaro, C. P. & Meio, M. D. Motor delay in cystic fibrosis infants: an observational study. Early Hum. Dev. 87, 769–773 (2011).
Zengin, P. A. et al. Developmental and behavioral problems in preschool-aged primary ciliary dyskinesia patients. Eur. J. Pediatr. 178, 995–1003 (2019).
Guenther, W. C. Desk calculation of probabilities for the distribution of the sample correlation coefficient. Am. Stat. 31, 45–48 (1977).
Farrell, P. M. et al. Guidelines for diagnosis of cystic fibrosis in newborns through older adults: Cystic Fibrosis Foundation consensus report. J. Pediatr. 153, 4–14 (2008).
De Boeck, K. et al. Cystic fibrosis: terminology and diagnostic algorithms. Thorax 61, 627–635 (2006).
Smyth, A. R. et al. European cystic fibrosis society standards of care: best practice guidelines. J. Cyst. Fibros. 13, 23–42 (2014).
Marson, F. A. L., Bertuzzo, C. S. & Ribeiro, J. D. Classification of CFTR mutation classes. Lancet Respir. Med. 4, e37–e38 (2016).
Lommatzsch, S. T. & Aris, R. Genetics of cystic fibrosis. Semin. Respir. Crit. Care Med. 30, 531–538 (2009).
Einspieler, C. et al. Cerebral palsy: early markers of clinical phenotype and functional outcome. J. Clin. Med. 8, 1616 (2019).
Radtke, T. et al. CFTR genotype and maximal exercise capacity in cystic fibrosis: a cross-sectional study. Ann. Am. Thorac. Soc. 15, 209–216 (2018).
Gruber, W. et al. Motor performance is better than normal in preschool children with cystic fibrosis. Pediatr. Pulmonol. 45, 527–535 (2010).
Einspieler, C. et al. Are abnormal fidgety movements an early marker for complex minor neurological dysfunction at puberty? Early Hum. Dev. 83, 521–525 (2007).
Harbourne, R. T. & Dusing, S. in Campbell’s Physical Therapy for Children 5th edn (eds Palisano, R. J. et al.) (Elsevier, Canada, 2017).
Okebukola, P. O., Kansra, S. & Barrett, J. Vitamin E supplementation in people with cystic fibrosis. Cochrane Database Syst. Rev. 3, CD009422 (2014).
Bonifant, C. M., Shevill, E. & Chang, A. B. Vitamin A supplementation for cystic fibrosis. Cochrane Database Syst. Rev. 5, CD006751 (2014).
Cynamon, H. A., Milov, D. E., Valenstein, E. & Wagner, M. Effect of vitamin E deficiency on neurologic function in patients with cystic fibrosis. J. Pediatr. 113, 637–640 (1988).
Olson, C. R. & Mello, C. V. Significance of vitamin A to brain function, behavior and learning. Mol. Nutr. Food Res. 54, 489–495 (2010).
Acknowledgements
The authors are grateful to Dr. Christa Einspieler from the Medical University Graz, Austria for her comments on an earlier version of the manuscript.
Author information
Authors and Affiliations
Contributions
Substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data: H.T., A.M., D.I.-I., A.L., A.K., S.E.-P., J.K., and U.O. Drafting the article or revising it critically for important intellectual content: H.T., A.M., D.I.-I., and U.O. Final approval of the version to be published: H.T., A.M., D.I.-I., and U.O.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Informed consent
Written informed consent was obtained from parents of all infants.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tekerlek, H., Mutlu, A., Inal-Ince, D. et al. Motor repertoire is age-inadequate in infants with cystic fibrosis. Pediatr Res 89, 1291–1296 (2021). https://doi.org/10.1038/s41390-020-1082-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-020-1082-4
This article is cited by
-
The effect of hyperbilirubinemia on motor repertoire of infants between 3 and 5 months of age
European Journal of Pediatrics (2022)