Abstract
Background
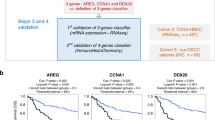
This study was undertaken to develop and validate a gene expression signature that characterises oral potentially malignant disorders (OPMD) with a high risk of undergoing malignant transformation.
Methods
Patients with oral epithelial dysplasia at one hospital were selected as the ‘training set’ (n = 56) whilst those at another hospital were selected for the ‘test set’ (n = 66). RNA was extracted from formalin-fixed paraffin-embedded (FFPE) diagnostic biopsies and analysed using the NanoString nCounter platform. A targeted panel of 42 genes selected on their association with oral carcinogenesis was used to develop a prognostic gene signature. Following data normalisation, uni- and multivariable analysis, as well as prognostic modelling, were employed to develop and validate the gene signature.
Results
A prognostic classifier composed of 11 genes was developed using the training set. The multivariable prognostic model was used to predict patient risk scores in the test set. The prognostic gene signature was an independent predictor of malignant transformation when assessed in the test set, with the high-risk group showing worse prognosis [Hazard ratio = 12.65, p = 0.0003].
Conclusions
This study demonstrates proof of principle that RNA extracted from FFPE diagnostic biopsies of OPMD, when analysed on the NanoString nCounter platform, can be used to generate a molecular classifier that stratifies the risk of malignant transformation with promising clinical utility.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 24 print issues and online access
$259.00 per year
only $10.79 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
El-Naggar, A. K., Chan, J. K. C., Grandis, J. R., Takata, T., Slootweg, P. J., editors WHO Classification of Head and Neck Tumours (International Agency for Research on Cancer, 2017).
Barnes, L., Eveson, J. W., Reichart, P., Sidransky, D., editors Pathology and Genetics of Head and Neck Tumours (World Health Organization, IARC, 2005).
Moore, S., Johnson, N., Pierce, A. & Wilson, D. The epidemiology of lip cancer: a review of global incidence and aetiology. Oral Dis. 5, 185–195 (1999).
Moore, S. R., Johnson, N. W., Pierce, A. M. & Wilson, D. F. The epidemiology of mouth cancer: a review of global incidence. Oral Dis. 6, 65–74 (2000).
Warnakulasuriya, S. Global epidemiology of oral and oropharyngeal cancer. Oral Oncol. 45, 309–316 (2009).
Goodson, M. L. & Thomson, P. J. Management of oral carcinoma: benefits of early precancerous intervention. Br. J. Oral Maxillofac. Surg. 49, 88–91 (2011).
van der Waal, I. Potentially malignant disorders of the oral and oropharyngeal mucosa; terminology, classification and present concepts of management. Oral Oncol. 45, 317–323 (2009).
Warnakulasuriya, S., Johnson, N. W. & van der Waal, I. Nomenclature and classification of potentially malignant disorders of the oral mucosa. J. Oral Pathol. Med. 36, 575–580 (2007).
Warnakulasuriya, S. & Ariyawardana, A. Malignant transformation of oral leukoplakia: a systematic review of observational studies. J. Oral Pathol. Med. 45, 155–166 (2016).
Shariff, J. A. & Zavras, A. I. Malignant transformation rate in patients presenting oral epithelial dysplasia: systematic review and meta-analysis. J. Oral Dis. 2015, 1–10 (2015).
Mehanna, H. M., Rattay, T., Smith, J. & McConkey, C. C. Treatment and follow-up of oral dysplasia—a systematic review and meta-analysis. Head Neck 31, 1600–1609 (2009).
Thomson, P. J., Goodson, M. L. & Smith, D. R. Profiling cancer risk in oral potentially malignant disorders—a patient cohort study. J. Oral Pathol. Med. 46, 888–895 (2017).
Napier, S. S. & Speight, P. M. Natural history of potentially malignant oral lesions and conditions: an overview of the literature. J. Oral Pathol. Med. 37, 1–10 (2008).
Field, E. A., McCarthy, C. E., Ho, M. W., Rajlawat, B. P., Holt, D., Rogers, S. N. et al. The management of oral epithelial dysplasia: the Liverpool algorithm. Oral Oncol. 51, 883–887 (2015).
Villa, A. & Woo, S. B. Leukoplakia—a diagnostic and management algorithm. J. Oral Maxillofac. Surg. 75, 723–734 (2017).
Awadallah, M., Idle, M., Patel, K. & Kademani, D. Management update of potentially premalignant oral epithelial lesions. Oral Surg. Oral Med. Oral. Pathol. Oral Radiol. 125, 628–636 (2018).
Reibel, J. Prognosis of oral pre-malignant lesions: significance of clinical, histopathological, and molecular biological characteristics. Crit. Rev. Oral Biol. Med. 14, 47–62 (2003).
Pitiyage, G., Tilakaratne, W. M., Tavassoli, M. & Warnakulasuriya, S. Molecular markers in oral epithelial dysplasia: review. J. Oral Pathol. Med. 38, 737–752 (2009).
Nankivell, P. & Mehanna, H. Oral dysplasia: biomarkers, treatment, and follow-up. Curr. Oncol. Rep. 13, 145–152 (2011).
Smith, J., Rattay, T., McConkey, C., Helliwell, T. & Mehanna, H. Biomarkers in dysplasia of the oral cavity: a systematic review. Oral Oncol. 45, 647–653 (2009).
Lingen, M. W., Pinto, A., Mendes, R. A., Franchini, R., Czerninski, R., Tilakaratne, W. M. et al. Genetics/epigenetics of oral premalignancy: current status and future research. Oral Dis. 17, 7–22 (2011).
Nikitakis, N. G., Pentenero, M., Georgaki, M., Poh, C. F., Peterson, D. E., Edwards, P. et al. Molecular markers associated with development and progression of potentially premalignant oral epithelial lesions: Current knowledge and future implications. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 125, 650–669 (2018).
Speight, P. M., Khurram, S. A. & Kujan, O. Oral potentially malignant disorders: risk of progression to malignancy. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 125, 612–627 (2018).
De Cecco, L., Nicolau, M., Giannoccaro, M., Daidone, M. G., Bossi, P., Locati, L. et al. Head and neck cancer subtypes with biological and clinical relevance: meta-analysis of gene-expression data. Oncotarget 6, 9627–9642 (2015).
Tonella, L., Giannoccaro, M., Alfieri, S., Canevari, S. & De Cecco, L. Gene expression signatures for head and neck cancer patient stratification: are results ready for clinical application? Curr. Treat. Options Oncol. 18, 32 (2017).
Saintigny, P., Zhang, L., Fan, Y. H., El-Naggar, A. K., Papadimitrakopoulou, V. A., Feng, L. et al. Gene expression profiling predicts the development of oral cancer. Cancer Prev. Res. (Philos.) 4, 218–229 (2011).
Geiss, G. K., Bumgarner, R. E., Birditt, B., Dahl, T., Dowidar, N., Dunaway, D. L. et al. Direct multiplexed measurement of gene expression with color-coded probe pairs. Nat. Biotechnol. 26, 317–325 (2008).
Reis, P. P., Waldron, L., Goswami, R. S., Xu, W., Xuan, Y., Perez-Ordonez, B. et al. mRNA transcript quantification in archival samples using multiplexed, color-coded probes. BMC Biotechnol. 11, 46 (2011).
Balko, J. M., Cook, R. S., Vaught, D. B., Kuba, M. G., Miller, T. W., Bhola, N. E. et al. Profiling of residual breast cancers after neoadjuvant chemotherapy identifies DUSP4 deficiency as a mechanism of drug resistance. Nat. Med. 18, 1052–1059 (2012).
Veldman-Jones, M. H., Brant, R., Rooney, C., Geh, C., Emery, H., Harbron, C. G. et al. Evaluating robustness and sensitivity of the NanoString technologies nCounter platform to enable multiplexed gene expression analysis of clinical samples. Cancer Res. 75, 2587–2593 (2015).
Veldman-Jones, M. H., Lai, Z., Wappett, M., Harbron, C. G., Barrett, J. C., Harrington, E. A. et al. Reproducible, quantitative, and flexible molecular subtyping of clinical DLBCL samples using the NanoString nCounter system. Clin. Cancer Res. 21, 2367–2378 (2015).
Speight, P. M., Abram, T. J., Floriano, P. N., James, R., Vick, J., Thornhill, M. H. et al. Interobserver agreement in dysplasia grading: toward an enhanced gold standard for clinical pathology trials. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 120, 474–482 e2 (2015).
Kujan, O., Oliver, R. J., Khattab, A., Roberts, S. A., Thakker, N. & Sloan, P. Evaluation of a new binary system of grading oral epithelial dysplasia for prediction of malignant transformation. Oral Oncol. 42, 987–993 (2006).
NanoString. nCounter XT Assay User Manual (NanoString Technologies Inc., 2016).
Sathasivam, H. P., Casement, J., Bates, T., Sloan, P., Thomson, P., Robinson, M., et al. Gene expression changes associated with malignant transformation of oral potentially malignant disorders. J. Oral Pathol. Med. https://doi.org/10.1111/jop.13090 (2020).
Lohavanichbutr, P., Méndez, E., Holsinger, F. C., Rue, T. C., Zhang, Y., Houck, J. et al. A 13-gene signature prognostic of HPV-negative OSCC: discovery and external validation. Clin. Cancer Res. 19, 1197 (2013).
Lallemant, B., Evrard, A., Combescure, C., Chapuis, H., Chambon, G., Raynal, C. et al. Reference gene selection for head and neck squamous cell carcinoma gene expression studies. BMC Mol. Biol. 10, 78 (2009).
Taïhi, I., Nassif, A., Berbar, T., Isaac, J., Berdal, A., Gogly, B. et al. Validation of housekeeping genes to study human gingival stem cells and their in vitro osteogenic differentiation using real-time RT-qPCR. Stem Cells Int. 2016, 6261490 (2016).
Rentoft, M., Hultin, S., Coates, P. J., Laurell, G. & Nylander, K. Tubulin α-6 chain is a stably expressed reference gene in archival samples of normal oral tissue and oral squamous cell carcinoma. Exp. Ther. Med. 1, 419–423 (2010).
Haider, S., Yao, C. Q., Sabine, V. S., Grzadkowski, M., Stimper, V., Starmans, M. H. W. et al. Pathway-based subnetworks enable cross-disease biomarker discovery. Nat. Commun. 9, 4746 (2018).
Ye, H., Yu, T., Temam, S., Ziober, B. L., Wang, J., Schwartz, J. L. et al. Transcriptomic dissection of tongue squamous cell carcinoma. BMC Genomics 9, 69 (2008).
van der Waal, I. Potentially malignant disorders of the oral and oropharyngeal mucosa; present concepts of management. Oral Oncol. 46, 423–425 (2010).
Dost, F., Le Cao, K., Ford, P. J., Ades, C. & Farah, C. S. Malignant transformation of oral epithelial dysplasia: a real-world evaluation of histopathologic grading. Oral Surg. Oral Med Oral Pathol. Oral Radiol. 117, 343–352 (2014).
Hald, J., Overgaard, J. & Grau, C. Evaluation of objective measures of smoking status–a prospective clinical study in a group of head and neck cancer patients treated with radiotherapy. Acta Oncol. 42, 154–159 (2003).
von Ahlfen, S., Missel, A., Bendrat, K. & Schlumpberger, M. Determinants of RNA quality from FFPE samples. PLoS ONE 2, e1261 (2007).
Eikrem, O., Beisland, C., Hjelle, K., Flatberg, A., Scherer, A., Landolt, L. et al. Transcriptome sequencing (RNAseq) enables utilization of formalin-fixed, paraffin-embedded biopsies with clear cell renal cell carcinoma for exploration of disease biology and biomarker development. PLoS ONE 11, e0149743 (2016).
Mittempergher, L., de Ronde, J. J., Nieuwland, M., Kerkhoven, R. M., Simon, I., Rutgers, E. J. et al. Gene expression profiles from formalin fixed paraffin embedded breast cancer tissue are largely comparable to fresh frozen matched tissue. PLoS ONE 6, e17163 (2011).
Wimmer, I., Troscher, A. R., Brunner, F., Rubino, S. J., Bien, C. G., Weiner, H. L. et al. Systematic evaluation of RNA quality, microarray data reliability and pathway analysis in fresh, fresh frozen and formalin-fixed paraffin-embedded tissue samples. Sci. Rep. 8, 6351 (2018).
Scott, D. W., Chan, F. C., Hong, F., Rogic, S., Tan, K. L., Meissner, B. et al. Gene expression-based model using formalin-fixed paraffin-embedded biopsies predicts overall survival in advanced-stage classical Hodgkin lymphoma. J. Clin. Oncol. 31, 692–700 (2013).
Saba, N. F., Wilson, M., Doho, G., DaSilva, J., Benjamin Isett, R., Newman, S. et al. Mutation and transcriptional profiling of formalin-fixed paraffin embedded specimens as companion methods to immunohistochemistry for determining therapeutic targets in oropharyngeal squamous cell carcinoma (OPSCC): a pilot of proof of principle. Head Neck Pathol. 9, 223–235 (2015).
Scaltriti, M., Eichhorn, P. J., Cortes, J., Prudkin, L., Aura, C., Jimenez, J. et al. Cyclin E amplification/overexpression is a mechanism of trastuzumab resistance in HER2+ breast cancer patients. Proc. Natl Acad. Sci. USA 108, 3761–3766 (2011).
Cancer Genome Atlas N. Comprehensive genomic characterization of head and neck squamous cell carcinomas. Nature 517, 576–582 (2015).
Hatano, M., Roberts, C. W., Minden, M., Crist, W. M. & Korsmeyer, S. J. Deregulation of a homeobox gene, HOX11, by the t(10;14) in T cell leukemia. Science 253, 79–82 (1991).
Yap, L. F., Lee, D., Khairuddin, A., Pairan, M. F., Puspita, B., Siar, C. H. et al. The opposing roles of NOTCH signalling in head and neck cancer: a mini review. Oral Dis. 21, 850–857 (2015).
Ranganathan, P., Weaver, K. L. & Capobianco, A. J. Notch signalling in solid tumours: a little bit of everything but not all the time. Nat. Rev. Cancer 11, 338–351 (2011).
Agrawal, N., Frederick, M. J., Pickering, C. R., Bettegowda, C., Chang, K., Li, R. J. et al. Exome sequencing of head and neck squamous cell carcinoma reveals inactivating mutations in NOTCH1. Science 333, 1154–1157 (2011).
Alevizos, I., Mahadevappa, M., Zhang, X., Ohyama, H., Kohno, Y., Posner, M. et al. Oral cancer in vivo gene expression profiling assisted by laser capture microdissection and microarray analysis. Oncogene 20, 6196–6204 (2001).
Macabeo-Ong, M., Shiboski, C. H., Silverman, S., Ginzinger, D. G., Dekker, N., Wong, D. T. et al. Quantitative analysis of cathepsin L mRNA and protein expression during oral cancer progression. Oral Oncol. 39, 638–647 (2003).
Kang, C.-J., Chen, Y.-J., Liao, C.-T., Wang, H.-M., Chang, J. T., Lin, C.-Y. et al. Transcriptome profiling and network pathway analysis of genes associated with invasive phenotype in oral cancer. Cancer Lett. 284, 131–140 (2009).
Mallery, S. R., Zwick, J. C., Pei, P., Tong, M., Larsen, P. E., Shumway, B. S. et al. Topical application of a bioadhesive black raspberry gel modulates gene expression and reduces cyclooxygenase 2 protein in human premalignant oral lesions. Cancer Res. 68, 4945 (2008).
Kuriakose, M. A., Chen, W. T., He, Z. M., Sikora, A. G., Zhang, P., Zhang, Z. Y. et al. Selection and validation of differentially expressed genes in head and neck cancer. Cell. Mol. Life Sci. 61, 1372–1383 (2004).
Leemans, C. R., Braakhuis, B. J. & Brakenhoff, R. H. The molecular biology of head and neck cancer. Nat. Rev. Cancer 11, 9–22 (2011).
Brennan, J. A., Boyle, J. O., Koch, W. M., Goodman, S. N., Hruban, R. H., Eby, Y. J. et al. Association between cigarette smoking and mutation of the p53 gene in squamous-cell carcinoma of the head and neck. N. Engl. J. Med. 332, 712–717 (1995).
Apostolou, P. & Papasotiriou, I. Current perspectives on CHEK2 mutations in breast cancer. Breast Cancer (Dove Med. Press) 9, 331–335 (2017).
Cybulski, C., Górski, B., Huzarski, T., Masojć, B., Mierzejewski, M., Debniak, T. et al. CHEK2 is a multiorgan cancer susceptibility gene. Am. J. Hum. Genet. 75, 1131–1135 (2004).
Cybulski, C., Huzarski, T., Górski, B., Masojć, B., Mierzejewski, M., Debniak, T. et al. A novel founder CHEK2 mutation is associated with increased prostate cancer risk. Cancer Res. 64, 2677–2679 (2004).
Chen, Y.-L., Tsai, W.-H., Ko, Y.-C., Lai, T.-Y., Cheng, A.-J., Shiah, S.-G. et al. Discoidin domain receptor-1 (DDR1) is involved in angiolymphatic invasion in oral cancer. Cancers (Basel) 12, 841 (2020).
Wang, W. W., Wang, Y. B., Wang, D. Q., Lin, Z. & Sun, R. J. Integrin beta-8 (ITGB8) silencing reverses gefitinib resistance of human hepatic cancer HepG2/G cell line. Int. J. Clin. Exp. Med. 8, 3063–3071 (2015).
Cui, Y., Wu, F., Tian, D., Wang, T., Lu, T., Huang, X. et al. miR-199a-3p enhances cisplatin sensitivity of ovarian cancer cells by targeting ITGB8. Oncol. Rep. 39, 1649–1657 (2018).
Mertens-Walker, I., Fernandini, B. C., Maharaj, M. S., Rockstroh, A., Nelson, C. C., Herington, A. C. et al. The tumour-promoting receptor tyrosine kinase, EphB4, regulates expression of integrin-beta8 in prostate cancer cells. BMC Cancer 15, 164 (2015).
Lenouvel, D., González-Moles, M. Á., Talbaoui, A., Ramos-García, P., González-Ruiz, L., Ruiz-Ávila, I. et al. An update of knowledge on PD-L1 in head and neck cancers: physiologic, prognostic and therapeutic perspectives. Oral Dis. 26, 511–526 (2020).
Dave, K., Ali, A. & Magalhaes, M. Increased expression of PD-1 and PD-L1 in oral lesions progressing to oral squamous cell carcinoma: a pilot study. Sci. Rep. 10, 9705 (2020).
Saintigny, P., El-Naggar, A. K., Papadimitrakopoulou, V., Ren, H., Fan, Y. H., Feng, L. et al. DeltaNp63 overexpression, alone and in combination with other biomarkers, predicts the development of oral cancer in patients with leukoplakia. Clin. Cancer Res. 15, 6284–6291 (2009).
Matsubara, R., Kawano, S., Kiyosue, T., Goto, Y., Hirano, M., Jinno, T. et al. Increased DeltaNp63 expression is predictive of malignant transformation in oral epithelial dysplasia and poor prognosis in oral squamous cell carcinoma. Int. J. Oncol. 39, 1391–1399 (2011).
Chen, Y. K., Hsue, S. S. & Lin, L. M. Expression of p63 protein and mRNA in oral epithelial dysplasia. J. Oral Pathol. Med. 34, 232–239 (2005).
Chibon, F. Cancer gene expression signatures—the rise and fall? Eur. J. Cancer 49, 2000–2009 (2013).
Acknowledgements
We would like to acknowledge Ms. Anastasia Resteu from the Newcastle NanoString Unit, Newcastle University, for assisting with the NanoString assay.
Author information
Authors and Affiliations
Contributions
H.P.S. conceived and designed the study, performed experiments, analysed data, carried out statistical analysis and wrote major parts of the manuscript. R.K. participated in study design, provided expert advice, performed experiments, interpreted results and edited the manuscript. P.S. participated in study design, provided expert advice, performed dysplasia grading, contributed to retrieval of tissue, interpreted results and edited the manuscript. P.T. and M.N. contributed to case selection, retrieval of follow-up data, quality assurance of data, interpreted results and edited the manuscript. J.A. and S.H. contributed to study design, analysed data, carried out statistical analysis, quality assurance of results, interpreted results and wrote major parts of the manuscript. M.R. conceived and designed the study, provided expert advice, performed dysplasia grading, contributed to retrieval of tissue, analysed data, interpreted results and wrote major parts of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was performed with approval from a Health Research Authority (UK) Research Ethics Committee (North East—Tyne and Wear South Research Ethics Committee; NRES Committee North East—Sunderland 11/NE/0118) and complies with UK legislation and guidelines. Patients were not recruited to the study and therefore individual patient consent was not sought. Link-anonymised patient tissue samples, surplus to diagnostic requirements, were analysed in accordance with the terms of the ethical approval. The study was performed in accordance with the Declaration of Helsinki.
Consent for publication
Not applicable.
Data availability
The datasets used and/or analysed during the current study are available at https://doi.org/10.5281/zenodo.4643470.
Competing interests
The authors declare no competing interests.
Funding information
H.P. Sathasivam was supported by scholarship from Ministry of Health Malaysia. S.H. is supported by Breast Cancer Now as part of Programme Funding to The Breast Cancer Now Toby Robins Research Centre.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Sathasivam, H.P., Kist, R., Sloan, P. et al. Predicting the clinical outcome of oral potentially malignant disorders using transcriptomic-based molecular pathology. Br J Cancer 125, 413–421 (2021). https://doi.org/10.1038/s41416-021-01411-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41416-021-01411-z
This article is cited by
-
Bridging the gap between omics research and dental practice
BDJ Open (2024)
-
Immunophenotypic and Gene Expression Analyses of the Inflammatory Microenvironment in High-Grade Oral Epithelial Dysplasia and Oral Lichen Planus
Head and Neck Pathology (2024)
-
Predicting oral cancer risk in patients with oral leukoplakia and oral lichenoid mucositis using machine learning
Journal of Big Data (2023)
-
Knockdown of PGC1α suppresses dysplastic oral keratinocytes proliferation through reprogramming energy metabolism
International Journal of Oral Science (2023)
-
Transcriptomic analysis predicts the risk of progression of premalignant lesions in human tongue
Discover Oncology (2023)