Abstract
Background
COVID-19 pandemic responses impacted behaviour and health services. We estimated the impact on incidence, stage and healthcare pathway to diagnosis for female breast, colorectal and non-small cell lung cancers at population level in Wales.
Methods
Cancer e-record and hospital admission data linkage identified adult cases, stage and healthcare pathway to diagnosis (population ~2.5 million). Using multivariate Poisson regressions, we compared 2019 and 2020 counts and estimated incidence rate ratios (IRR).
Results
Cases decreased 15.2% (n = −1011) overall. Female breast annual IRR was 0.81 (95% CI: 0.76–0.86, p < 0.001), colorectal 0.80 (95% CI: 0.79–0.81, p < 0.001) and non-small cell lung 0.91 (95% CI: 0.90–0.92, p < 0.001). Decreases were largest in 50–69 year olds for female breast and 80+ year olds for all cancers. Stage I female breast cancer declined 41.6%, but unknown stage increased 55.8%. Colorectal stages I–IV declined (range 26.6–29.9%), while unknown stage increased 803.6%. Colorectal Q2-2020 GP-urgent suspected cancer diagnoses decreased 50.0%, and 53.9% for non-small cell lung cancer. Annual screen-detected female breast and colorectal cancers fell 47.8% and 13.3%, respectively. Non-smal -cell lung cancer emergency presentation diagnoses increased 9.5% (Q2-2020) and 16.3% (Q3-2020).
Conclusion
Significantly fewer cases of three common cancers were diagnosed in 2020. Detrimental impacts on outcomes varied between cancers. Ongoing surveillance with health service optimisation will be needed to mitigate impacts.
Similar content being viewed by others
Background
Responses to the COVID-19 pandemic, including mandated societal lockdowns [1], citizen behavioural change [2] and health system reconfiguration [3, 4] during 2020, led to paused cancer screening programmes, altered presentation to primary care, and impacted suspected cancer referrals, diagnostic procedures [5] and treatment modalities [6]. Several studies modelled pandemic effects on excess cancer mortality [7,8,9], but despite concern about the impact on cancer services and outcomes [10], most studies reported limited data on observed cancer mortality, incidence, stage and healthcare pathways to diagnosis. These parameters have not been assessed at the population level in the UK. We undertook an analysis of clinically ascertained: (I) female breast (good prognosis and screening programme in place), (II) colorectal (moderate prognosis and screening programme in place) and (III) non-small cell lung cancers (poor prognosis and no current screening programme in Wales) at a whole-population level in Wales during the pandemic’s first full-year of 2020 compared to 2019, to determine the impact on cancer incidence, stage at diagnosis and healthcare pathways to diagnosis, to inform cancer service adaptation to the pandemic and subsequent recovery from it.
Methods
We conducted a retrospective observational study of the resident population of Wales aged 18+ years (n = 2,539,714) [11] in the Con-COV cohort [12] within the Secure Anonymised Information Linkage (SAIL) Databank [13].
Cases of new primary female breast (ICD-10: C50), colorectal (C18, C19, C20) and non-small cell lung cancers (C33, C34 with morphology M8041) between January 1, 2019, and December 31, 2020, inclusive, were identified from the Cancer Network Information System Cymru (CaNISC)—the national electronic clinical cancer patient record system, largely covering the population of Wales.
The exposure evaluated was the effect of the COVID-19 pandemic and pandemic mitigations [14] (Figs. 1 and 2). Diagnosis from January 1, 2020, to December 31, 2020, constituted exposure. Non-exposure (as the comparator) was diagnosed from January 1, 2019, to December 31, 2019.
Outcome measures
Outcome measures included annual and monthly incident case counts, stage at diagnosis and annual and quarterly healthcare pathway to diagnosis. The pathway to diagnosis was derived from CaNISC with person-level linkage to Patient Episode Database Wales hospital admission data (Fig. S2) and categorised into: (I) screening, (II) general practitioner urgent suspected cancer referral, (III) emergency presentation/admission, (IV) in-patient referral, (V) out-patient referral, (VI) other or (VII) not known. The summary stage at diagnosis I–IV, including the unknown stage, was available from CaNISC for female breast and colorectal cancers. CaNISC is awaiting replacement, and until then, it is impossible to correctly record the stage at diagnosis in CaNISC for non-small cell lung cancer.
Co-variates
Co-variates included sex, age (18–49, 50–59, 60–79 and 80+) and quintile of the income domain of the Welsh Index of Multiple Deprivation data [15]. All the index domains were not used together, as its health domain already includes registry-based cancer incidence, so its inclusion would introduce a reverse cause bias.
Analysis
We presented descriptively incident counts by cancer type for 2019 and 2020 and calculated absolute and relative differences in annual counts between years for each cancer. Monthly counts and absolute and relative differences between corresponding months in 2019 and 2020 were also determined.
We used mid-year population estimates to test the null hypotheses that there were no differences in incident cases of the female breast, colorectal and non-small-cell lung cancers in 2020 compared with 2019. Multivariate Poisson regression analyses estimated unadjusted incidence rate ratios (IRR) and IRRs adjusted for age differences, sex (for colorectal and non-small cell cancers) and income deprivation quintile from the Welsh Index of Multiple Deprivation. Similarly, we also calculated the post-Poisson estimated marginal means to undertake a series of pairwise comparisons between 2020 and 2019. In addition, pairwise comparisons in the rates between 2019 and 2020 for the stage at presentation, healthcare pathway to diagnosis, sex, age category and deprivation quintile were carried out. Due to a large number of comparisons, all 95% confidence intervals around the IRR and their subsequent p-values were adjusted using the Bonferroni correction (adjusted alpha = 0.05/number of comparisons). All models were tested for overdispersion, and none was found.
The stage at diagnosis for female breast and colorectal cancers only was estimated as counts/percentage of the total incidence for each stage for each year. The absolute and relative difference in counts between years was calculated for each cancer and each stage. Counts of incident cases in each healthcare pathway to diagnosis category and absolute and relative differences for each pathway between years were determined.
Results
Annual and monthly incidence
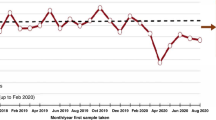
A total of −1011 (−15.2%) fewer cases of the three cancers was diagnosed during 2020 (n = 5640) compared to 2019 (n = 6651). Decreases occurred for female breast (−19.1%, n = −474), colorectal (−17.2%, n = −383) and less so for non-small cell lung cancers (−7.9%, n = −154) (Table 1 and Fig. 3a).
Changes in monthly incidence differed for each cancer (Fig. 3b, Table 1). For all three cancers, steep decreases in monthly incidence did not occur until April 2020. April incidence for female breast cancer was −45.3% lower in 2020 than in 2019, recovering to 2019 levels by September 2020. Colorectal cancer had an even greater decrease of −59.9% in April 2020, partially recovering by June 2020 (−10.5%), but remained below 2019 monthly incidence until December 2020. The April 2020 decrease was less steep for non-small cell lung cancer (−27.7%, n = −41), recovering by June 2020, but decreasing to below 2019 levels at the end of 2020 (2019 vs 2020: −16.3% October, −7.4% November and −15.3% December).
Colorectal cancer cases decreased by −23.7% (n = −233) in females and −12.1% (n = −150) in males between 2019 and 2020 (Table 1), although for non-small cell lung cancer the relative decline was larger for males (−11.7%, n = −119) compared to females (−3.8%, n = −35).
The largest age-group decreases were amongst 50–69-year-old female breast cancer patients (−24.2%, n = −292) (Table 1). Among 80+ year olds, relative incidence declines were similar for all three cancers: female breast −21.9% (n = −86); colorectal −20.2% (n = −117) and non-small cell lung cancers −20.4% (n = −110). Declines occurred in all quintiles of income area-deprivation and were highest in the three least deprived quintiles for female breast cancer, ranging from −23.1 to −26.3%. There was a gradient of increasing relative decline from 2019 to 2020 in the most to the least deprived quintiles for colorectal cancer. For non-small lung cancer, there was no clear gradient.
The results of the Poisson regression and unadjusted and adjusted annual and pairwise monthly IRRs for 2020 compared to 2019 are shown in Table 2. The unadjusted annual IRRs for female breast (0.81 [95% CI 0.76, 0.86; p < 0.001]), colorectal (0.80 [95% CI 0.79, 0.81; p < 0.001]) and non-small cell lung (0.91 [95% CI: 0.90, 0.92; p < 0.001]) cancers were all largely unchanged by adjustment for age, sex (for colorectal and non-small cell cancers) and income area-deprivation quintile (Table 2). The unadjusted IRRs were highly statistically significant for the pairwise comparisons of months between 2020 and 2019, showing large to moderate declines in the descriptive analysis for all three cancer types. However, adjustment removed the IRR statistical significance for all 12 months in non-small cell lung cancer and for all except April and May 2020 for colorectal cancer. For female breast cancer, the large declines in incident cases observed from March to November 2020, except for September, remained highly significant (p < 0.001) during May, July and August 2020 when IRRs were adjusted for age and area-level income deprivation.
Stage at diagnosis
There was a large decrease in stage I female breast cancer −41.6% (n = −374) in 2020 compared to 2019 (Table 1). Relative declines in stages II and III were similar at −20.5% (n = −202) and −18.2% (n = −47), respectively. Stage IV decline was based on smaller case numbers (n = −15). Female breast cancers recorded with stage unknown increased by 55.8% (n = +164) between 2019 and 2020. The relative decrease in colorectal cancer cases was similar across the stages I–IV (ranging between 26.6 and 29.9%). There was a substantial increase of 803.6% (n = +225) in colorectal cancers with stage unknown recorded in 2020, compared to 2019. Cumulative monthly case counts of female breast and colorectal cancers for 2019 and 2020 by stage at diagnosis are shown in Fig. 4a and b.
Healthcare pathway to diagnosis
The annual decrease in screen-detected female breast cancer diagnoses was −47.8% (n = −451) (Table 1), with a large decline between Q2 (April, May and June), 2019 and Q2, 2020 (−86.7%, n = −214), followed by partial recovery to around half the 2019 diagnoses in Q4 (Fig. 5). Female breast cancer diagnosis via GP urgent suspected cancer referral increased slightly (+2.2%, n = +26) over the whole of 2020 compared to 2019. After a slight drop during Q2-2020, GP urgent suspected cancer referral diagnoses rebounded above 2019 levels in Q3 (+1.0%) and Q4 (+11.1%), 2020.
GP urgent suspected cancer referral colorectal cancer diagnoses declined by −19.9% (n = −213) in 2020 compared to 2019 but remained the most frequent pathway to diagnosis (Table 1). Diagnoses via this pathway declined by −50.0% (n = −135) in Q2-2020 compared to Q2 2019, partially recovered in Q3-2020, surpassing 2019 by Q4 (Fig. 5). Emergency presentation/admission diagnoses were maintained and had only a small annual change (−7.8%, n = −38), but were slightly lower in Q1 and Q4 2020 than in corresponding 2019 quarters and slightly higher in Q2 and Q3 (Fig. 5). The screening was the third most frequent pathway to diagnosis; it showed a −13.3% (n = −37) annual reduction in 2020, with an increase in Q1, 2020 compared to Q1 2019, a large decline in Q2-2020 (−56.7%, n = 34), and recovery by Q3 to just below the Q3 2019 level. However, the Q4 diagnoses were below Q4, 2019. An annual decline of −34.3% (n = −69) occurred in the in-patient referral route, occurring during Q2–Q4.
A decline of −18.3% (n = −135) in non-small cell lung cancer GP urgent suspected cancer diagnoses occurred over the whole of 2020, compared to 2019 (Table 1), with a considerable decline of −53.9% (n = −83) in Q2-2020, followed by a partial recovery in Q3 that did not recover further in Q4 (Fig. 5). In Q1 2020, diagnoses via this pathway were slightly higher (+7.0%, n = +14) than cases observed during the same period in 2019. In contrast, there was little annual change in emergency presentation diagnoses (−2.1%, n = −13), although diagnoses were higher in Q2 and Q3-2020, compared with 2019, then declined rapidly in Q4. Diagnosis via referral as an existing in-patient increased slightly above 2019 levels in Q1 and Q3-2020 but decreased in Q2 and Q4.
The trends in incidence, stage at diagnosis and healthcare pathway to diagnosis coincided with the timing of the pandemic and mitigation responses introduced in 2020 (Fig. 1).
Discussion
To our knowledge, this is the first national population-level study using electronic cancer clinical data to quantify COVID-19 pandemic effects on cancer diagnosis, stage and healthcare pathway to diagnosis in detail for the whole of 2020. Our analyses used linked population data to compare the effects on three common cancers of contrasting prognosis and screening programme availability, facilitating consideration of differential outcomes between demographic groups over time and against dynamic changes of the pandemic and mitigation responses.
We observed detrimental changes in incidence, with over a thousand fewer cases in 2020 compared with 2019 across the three cancers, in stage at diagnosis, and in healthcare pathway to diagnosis, coinciding with the timing of pandemic COVID-19 incidence and dynamic responses such as societal restrictions and health service reconfiguration. There was considerable variation between cancer types and demographic groups, particularly affecting older age groups. The pausing of screening had a major impact on early female breast cancer diagnosis, however, decreased diagnoses through GP urgent suspected cancer referral had a greater impact on colorectal cancer and non-small cell lung cancers.
Our data demonstrate that impacts varied considerably between cancers and demographic groups, coinciding with dynamic changes in community COVID-19 cases and pandemic mitigation responses and according to their pre-pandemic pattern of healthcare pathway routes to diagnosis. Other studies that examined cancer incidence during the pandemic used prediction modelling or proxy measures such as diagnostic or treatment activity [5, 6, 8, 16,17,18]. Of the few studies that used clinical data, one study examined colorectal cancer cases from a single tertiary hospital serving a regional Spanish catchment area [19]. Ascertainment fell by 47.7% in spring 2020 compared to spring 2019, whereas we found decreases of almost a fifth in colorectal cancer incidence during 2020 overall, and 59.9% in April 2020 compared to April 2019, greater than the Spanish study, yet of a broadly similar order of magnitude. Our results were also consistent with their finding of no change in colorectal cancer stage distribution and a greater decline amongst women than men. A south-east London clinical-data study [20] examined a smaller urban population, including a tertiary hospital. It compared 6-month periods before and after the March 2020 UK lockdowns rather than corresponding months in 2019 and 2020. Nevertheless, our results demonstrated broadly consistent month-on-month incidence trends with the London study for female breast cancer, colorectal cancer and non-small cell lung cancers, as reported until September 2020.
The main strength of our study was the deployment of clinical data from a single national system with near whole-population coverage. Rapid and confidential data linkage was possible within the SAIL Databank [13] Trusted Research Environment, enabling detailed analysis by demographic factors, area deprivation and granular healthcare pathway to diagnosis. We studied the whole of 2019 and 2020 rather than simply before and after the first national lockdown, allowing a more precise longitudinal analysis of the impact of lockdowns, health service measures, citizen behaviour change and accounted for seasonal variations.
Given health service reconfiguration to maintain essential emergency procedures and surgery during pandemic waves, a clinical diagnosis could still be possible. Limitations included the low completeness of stage data for non-small cell lung cancer, although the missing stage for female breast and colorectal cancers was higher during 2020 (Table 3 and Fig. 4a, b). Information such as from pathology samples, for example, that would allow full and final staging at diagnosis might have been less available during 2020 [5, 6, 19]. Such healthcare restrictions are likely to have affected colorectal cancer patients more than many breast cancer cases, with surgery being required for staging, and this is reflected in the considerable increase in unknown stages for colorectal cancer during 2020. Non-small cell lung cancer staging would have also relied more on staging at surgery than breast cancer, although we could not obtain data on this occasion. Some breast surgery can be performed in a less intensive hospital setting than for advanced colorectal and non-small cell lung cancer. Furthermore, some observed more minor changes in stage distribution may have occurred through misclassification of the stage due to staging occurring without the usual full information sources to clinicians.
Despite preceding COVID-19 cases, specific health system changes and a brief period of societal advisory restrictions (Fig. 1) in Wales during early 2020, our results did not show major impacts on cancer incidence until April 2020, following a strict lockdown implemented on March 23, 2020, and significant health system reconfiguration to prioritise COVID-19 infection control. Using sub-regional primary care data, a study in Catalonia, Spain [21], demonstrated that cancer incidence decreased from March 2020, corresponding to earlier community infections and lockdown. Our findings of changing diagnosis patterns during the summer of 2020 coincided with a partial lifting of restrictions and early readjustment of health services toward managing non-COVID-19 patients. According to our analysis, starting October 2020 (Fig. 1), another brief lockdown coincided with increased monthly declines in diagnoses. Strict restrictions were re-imposed in early December 2020, when diagnoses decreased further. GP urgent suspected cancer referral diagnoses decreased during Q2, 2020, after the first lockdown when primary care access was altered.
Citizen behaviour changed in response to restrictions and instructions to stay at home or ‘shield’ [22], which had the unintended consequence of causing a reluctance by some to seek health care services due to concerns about SARS-Cov-2 infection, and others not wanting to burden a health system busy with COVID-19 [2, 23]. This behaviour change was particularly impactful for those with potential lung cancer. A persistent cough is an early sign of disease and the main symptom of COVID-19 infection. The potential risk from SARS-Cov-2 infection became a reason to stay at home and not consult a GP. Health service data in England, Northern Ireland and Wales indicated measurable decreased cancer-related referrals [5, 6, 8, 24, 25] of similar trends to actual diagnoses via this pathway in our study. We demonstrated that screen-detected female breast cancer diagnoses fell by almost half, consistent with the temporary cessation of screening services from March 2020 (see Fig. 2), although in the interim, during Q2–Q3, breast screening services diverted to support symptomatic patient diagnosis via GP urgent suspected cancer [26]. Increases in screen-detected colorectal cancer diagnoses from Q3, 2019 to Q1, 2020, likely followed the known introduction of faecal immunochemical testing in Wales. During the pausing of colorectal cancer screening, faecal immunochemical testing was diverted to prioritise symptomatic patients awaiting colonoscopy. Cancer screening programmes restarted in a phased approach from the end of June–August 2020, increasing female breast cancer diagnoses. The overall impact on screen-detected colorectal cancer was less, possibly because it was easier to send a faecal immunochemical testing kit to homes, with the uptake in colorectal screen-detected diagnoses improving soon after the service restarted. Existing colorectal cancer screening patients awaiting colonoscopy were reviewed for symptoms during the paused programme and referred to the symptomatic pathway if required.
Despite attendance at emergency departments decreasing [27], colorectal cancer and non-small cell-lung cancers diagnoses through emergency presentations increased in Q2–Q3, 2020. It is unclear if this was due to a shift from other less accessible pathways or increased emergency complications of cancer or non-cancer conditions. Multi-morbidities are common amongst colorectal cancer and non-small cell lung cancers patients [28], making them more likely to be instructed to ‘shield’ at home. Shielding could partly explain their lower recovery in GP urgent suspected cancer diagnoses than female breast cancer and increased emergency presentations with an incidental cancer diagnosis. Patients 80+ years old were more likely to be shielding, which might explain their similar declines of around a fifth in incidence for all three cancers. We observed an increase in non-small cell lung cancer diagnoses as an existing in-patient in Q1 2020 when COVID-19 community infections had started in Wales, which suggested they might have been incidental diagnoses.
We cannot conclude from our current study that a shift to a later stage at diagnosis occurred in the true population cancer incidence during 2020, as many cases remained undiagnosed. Instead, we observed decreases of various extents in all stages for female breast and colorectal cancers. The pausing of screening disproportionately affected stage I female breast cancer detection in 50–69 year-old women. Those cancer patients at a late stage may have died without being diagnosed, as predicted by modelling studies [7, 8].
With over a thousand fewer cases diagnosed across three common cancers during 2020, our study suggests large numbers of undiagnosed cancer patients more widely due to the ongoing pandemic, societal mitigations and health service reconfiguration in response. Although the pandemic has abated somewhat, along with societal and healthcare responses to it, our study still suggests that extensive alterations to healthcare pathways to diagnosis, increases in later-stage diagnoses and an increase in the number of undiagnosed patients with new cancers will occur. With continued research and surveillance, the accumulation of incidence, stage and healthcare pathway data will allow more accurate forecasting through the stage of diagnosis and mortality prediction modelling to inform effective cancer services’ responses. Ongoing optimisation of cancer screening programmes and the transformation of cancer services and primary care referral are urgently required.
Data availability
The data used in this study are available in the SAIL Databank at Swansea University, Swansea, UK, but they are not publicly available as restrictions apply. All proposals to use SAIL data are subject to review by an independent Information Governance Review Panel (IGRP). Before any data can be accessed, approval must be given by the IGRP. The IGRP carefully considers each project to ensure the proper and appropriate use of SAIL data. When access has been granted, it is gained through a privacy-protecting Safe Haven and remote access system referred to as the SAIL Gateway. SAIL has established an application process to be followed by anyone who would like to access data via SAIL at https://www.saildatabank.com/application-process
References
Welsh government. Coronavirus and the law. https://gov.wales/coronavirus-law. 2021. Accessed 12 July 2021.
Cardiff University. COVID Health and Help-seeking Behaviour Study (CABS). https://cabs-study.yolasite.com. 2021. Accessed 12 July 2021.
Welsh government. COVID-19 Hospital Discharge Service Requirements. 2021. https://gov.wales/hospital-discharge-service-requirements-covid-19 Accessed 12 July 2021.
Welsh government. Maintaining Health Services During the Covid-19 Pandemic. https://gov.wales/sites/default/files/publications/2020-05/maintaining-essential-health-services-during-the-covid-19-pandemic-summary-of-services-deemed-essential.pdf. 2021. Accessed 12 July 2021.
Ho KMA, Banerjee A, Lawler M, Rutter MD, Lovat LB. Predicting endoscopic activity recovery in England after COVID-19: a national analysis. Lancet Gastroenterol Hepatol. 2021;6:381–90. https://doi.org/10.1016/S2468-1253(21)00058-3.
Morris EvaJA, Goldacre Raphael, Spata Enti, Mafham Marion, Finan PaulJ, Shelton Jon, et al. Impact of the COVID-19 pandemic on the detection and management of colorectal cancer in England: a population-based study. Lancet Gastroenterol Hepatol. 2021;6:199–208. https://doi.org/10.1016/S2468-1253(21)00005-4.
Lai AG, Pasea L, Banerjee A, Hall G, Denaxas S, Chang WH, et al. Estimated impact of the COVID-19 pandemic on cancer services and excess 1-year mortality in people with cancer and multimorbidity: near real-time data on cancer care, cancer deaths and a population-based cohort study. BMJ Open. 2020;10:e043828. https://doi.org/10.1136/bmjopen-2020-043828.
Maringe C, Spicer J, Morris M, Purushotham A, Nolte E, Sullivan R, et al. The impact of the COVID-19 pandemic on cancer deaths due to delays in diagnosis in England, UK: a national, population-based, modelling study. Lancet Oncol. 2020;21:1023–34.
Sud A, Torr B, Jones ME, Broggio J, Scott S, Loveday C, et al. Effect of delays in the 2-week-wait cancer referral pathway during the COVID-19 pandemic on cancer survival in the UK: a modelling study. Lancet Oncol. 2020;21:1035–44
Vrdoljak E, Sullivan R, Lawler M. Cancer and coronavirus disease 2019; how do we manage cancer optimally through a public health crisis? Eur J Cancer. 2020;132:98–9. https://doi.org/10.1016/j.ejca.2020.04.001
ONS Population estimates for UK, England, Wales, Scotland and Northern Ireland. https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/datasets/populationestimatesforukenglandandwalesscotlandandnorthernireland. 2021. Accessed 05/07/21.
Lyons J, Akbari A, Agrawal U, Harper G, Azcoaga-Lorenzo A, Bailey R, et al. Protocol for the development of the Wales Multimorbidity e-Cohort (WMC): data sources and methods to construct a population-based research platform to investigate multimorbidity. BMJ Open. 2021;11:e047101. 10.1136/bmjopen-2020-047101.
Lyons RA, Jones KH, John G, Brooks CJ, Verplancke JP, Ford DV, et al. The SAIL databank: linking multiple health and social care datasets. BMC Med Inform Decis Mak. 2009;9:3. http://www.biomedcentral.com/1472-6947/9/3.
Davies GA, Alsallakh MA, Sivakumaran S, Eleftheria Vasileiou, Ronan A Lyons, Chris Robertson, et al. Impact of COVID-19 lockdown on emergency asthma admissions and deaths: national interrupted time series analyses for Scotland and Wales. Thorax. 2021. https://doi.org/10.1136/thoraxjnl-2020-216380
Welsh government. Welsh Index of Multiple Deprivation. https://statswales.gov.wales/Catalogue/Community-Safety-and-Social-Inclusion/Welsh-Index-of-Multiple-Deprivation. 2021. Accessed 05/03/2021.
Zadnik V, Mihor A, Tomsic S, Zagar T, Bric N, Lokar K, et al. Impact of COVID-19 on cancer diagnosis and management in Slovenia - preliminary results. Radiol Oncol 2020;54:329–34. https://doi.org/10.2478/raon-2020-0048.
De Vincentiis Ludovica, Carr RichardA, Mariani MariaPaola, Ferrara Gerardo. Cancer diagnostic rates during the 2020 ‘lockdown’, due to COVID-19 pandemic, compared with the 2018–2019: an audit study from cellular pathology. J Clin Pathol. 2020;0:1–3. https://doi.org/10.1136/jclinpath-2020-206833.
Dinmohamed AG, Visser O, Verhoeven RHA, Louwman MWJ, van Nederveen FH, Willems SM, et al. Fewer cancer diagnoses during the COVID-19 epidemic in the Netherlands. Lancet Oncol. 2020;21:750–1. https://doi.org/10.1016/S1470-2045(20)30265-5.
Suárez J, Mata E, Guerra A. Jiménez G, Montes M, Arias F, et al. Impact of the COVID-19 pandemic during Spain’s state of emergency on the diagnosis of colorectal cancer. J Surg Oncol. 2021;123:32–36. 10.1002/jso.26263..
Purushotham A, Roberts G, Haire K, Dodkins J, Harvey-Jones E, Han L, et al. The impact of national non-pharmaceutical interventions (‘lockdowns’) on the presentation of cancer patients. Ecancermedicalscience. 2021;15:1180. https://doi.org/10.3332/ecancer.2021.1180.
Coma E, Guiriguet C, Mora N, Marzo-Castillejo M, Benítez M, Méndez-Boo L, et al. Impact of the COVID-19 pandemic and related control measures on cancer diagnosis in Catalonia: a time-series analysis of primary care electronic health records covering about five million people. BMJ Open. 2021;11:e047567. https://doi.org/10.1136/bmjopen-2020-047567.
Coronavirus and the social impacts on behaviours during different lockdown periods, Great Britain—Office for National Statistics (ons.gov.uk). 2021. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/healthandwellbeing/articles/coronavirusandthesocialimpactsonbehavioursduringdifferentlockdownperiodsgreatbritain/uptofebruary2021 Accessed 9 July 2021.
Jones D, Neal RD, Duffy SRG, Scott SE, Whitaker KL, Brain K. Impact of the COVID-19 pandemic on the symptomatic diagnosis of cancer: the view from primary care. Lancet Oncol. 2020;21:748–50.
Rutter MD, Brookes M, Lee TJ, Rogers P, Sharp L. Impact of the COVID-19 pandemic on UK endoscopic activity and cancer detection: a National Endoscopy Database Analysis. Gut. 2021;70:537–43. https://doi.org/10.1136/gutjnl-2020-322179.
Welsh government. Referrals by treatment function and month (gov.wales). 2021. https://statswales.gov.wales/Catalogue/Health-and-Social-Care/NHS-Hospital-Activity/Referrals/referrals-by-treatmentfunction-month Accessed 9 July 2021.
Hillier S, Director of Screening Services, Public Health Wales. 2021. Personal communication. 21 July.
Welsh government. Attendances in NHS Wales accident and emergency departments, by local health board and date (gov.wales). 2022. https://statswales.gov.wales/Catalogue/Health-and-Social-Care/NHS-Hospital-Activity/nhs-activity-and-capacity-during-the-coronavirus-pandemic/accidentandemergencydepartmentsattendances-by-date-localhealthboard Accessed 14 January 2022.
Welsh Cancer Intelligence and Surveillance Unit, Public Health Wales. Cancer patients with other chronic health conditions in Wales: GP Cluster Network incidence, prevalence and all Wales survival | Tableau Public. 2021. https://public.tableau.com/app/profile/welsh.cancer.intelligence.and.surveillance.unit/viz/FinalWIP/Incidencecomparison Accessed 09 July 2021.
Acknowledgements
We wish to acknowledge the collaborative partnership that enabled the acquisition and access to the de-identified data, which led to this output. The collaboration was led by the Swansea University Health Data Research UK team under the Welsh Government Technical Advisory Cell (TAC) direction. It included the following groups and organisations: the SAIL Databank, Administrative Data Research (ADR) Wales, Digital Health and Care Wales (DHCW), Public Health Wales, NHS Shared Services Partnership (NWSSP) and the Welsh Ambulance Service Trust (WAST).
Funding
This work was supported by the Con-COV team funded by the Medical Research Council (grant number: MR/V028367/1). This work was supported by Health Data Research UK, which receives its funding from HDR UK Ltd (HDR-9006) funded by the UK Medical Research Council, Engineering and Physical Sciences Research Council, Economic and Social Research Council, Department of Health and Social Care (England), Chief Scientist Office of the Scottish Government Health and Social Care Directorates, Health and Social Care Research and Development Division (Welsh Government), Public Health Agency (Northern Ireland), British Heart Foundation (BHF) and the Wellcome Trust. This work was supported by the Administrative Data Research (ADR) Wales work programme. The ADR Wales programme of work aligns with the priority themes identified in the Welsh Government’s national strategy: Prosperity for All. ADR Wales brings together data science experts at Swansea University Medical School, staff from the Wales Institute of Social and Economic Research, Data and Methods (WISERD) at Cardiff University and specialist teams within the Welsh Government to develop new evidence which supports Prosperity for All by using the SAIL Databank at Swansea University, to link and analyse anonymised data. ADR Wales is part of the Economic and Social Research Council (part of UK Research and Innovation) funded ADR UK (grant ES/S007393/1). This work was supported by the Wales COVID-19 Evidence Centre, funded by Health and Care Research Wales. This work was supported by Health Data Research UK funding to DATA-CAN, the UK’s Health Data Research Hub for Cancer and Cancer Research UK (C23434/A23706).
Author information
Authors and Affiliations
Contributions
GG—methodology, project administration, resources, software, supervision, validation, data curation, formal analysis, investigation, writing—original draft, RG—data curation, validation, methodology, investigation, directly accessed and verified the underlying data, writing—review and editing, AA—project administration, resources, data curation, writing—review and editing, JH—data curation, investigation, validation, writing—review and editing, MJ—investigation, supervision, methodology, writing—review and editing, JL—visualisation, investigation, writing—review and editing, ML—funding acquisition, investigation, methodology, resources, writing—review and editing, RL—funding acquisition, investigation, methodology, resources, writing—review and editing, supervision, EM—investigation, methodology, supervision, writing—review and editing, MR—methodology, resources, writing—review and editing, supervision, FT—investigation, writing—review and editing, JW—investigation, methodology, supervision, writing—review and editing, DWH—conceptualisation, writing—original draft, methodology, supervision, resources, investigation, writing—review and editing.
Corresponding author
Ethics declarations
Competing interests
ML has received an unrestricted educational grant from Pfizer for research unrelated to this work. ML has received honoraria from Pfizer, EMF Serono, Roche, Bayer, Novartis and Carnall Farrar unrelated to this work. DWH has received research consultancy fees from Pfizer for research unrelated to this work, and his department (Welsh Cancer Intelligence and Surveillance Unit, Public Health Wales) has received analysis partnership funding from Macmillan Cancer Support for unrelated work. The remaining authors declare no competing interests.
Ethics approval and consent to participate
All research conducted has been completed under the permission and approval of the SAIL independent Information Governance Review Panel (IGRP) project number 0911. The support of DATA-CAN, the UK’s Health data Research Hub for Cancer, is acknowledged. The advice of the Screening Division, Public Health Wales, is also acknowledged.
Consent for publication
This study uses anonymised data held in the Secure Anonymised Information Linkage (SAIL) Databank. This work uses data provided by patients and collected by the NHS as part of their care and support. We would also like to acknowledge all data providers who make anonymised data available for research.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
41416_2022_1830_MOESM2_ESM.docx
Figure S2: Mapping of the healthcare pathway to diagnosis from the Cancer Network Information System Cymru (CaNISC) with additional information from the in-patient Patient Episode Dataset of Wales (P
Rights and permissions
About this article
Cite this article
Greene, G., Griffiths, R., Han, J. et al. Impact of the SARS-CoV-2 pandemic on female breast, colorectal and non-small cell lung cancer incidence, stage and healthcare pathway to diagnosis during 2020 in Wales, UK, using a national cancer clinical record system. Br J Cancer 127, 558–568 (2022). https://doi.org/10.1038/s41416-022-01830-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41416-022-01830-6
This article is cited by
-
Impact of the COVID-19 pandemic on breast cancer patient pathways and outcomes in the United Kingdom and the Republic of Ireland – a scoping review
British Journal of Cancer (2024)
-
The journey of lung cancer patients from symptoms to diagnosis in Greece. A mixed methods approach
npj Primary Care Respiratory Medicine (2024)
-
The impact of the COVID-19 pandemic on community prescription of opioid and antineuropathic analgesics for cancer patients in Wales, UK
Supportive Care in Cancer (2023)