Abstract
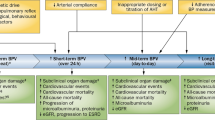
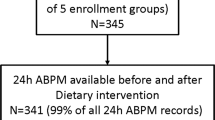
Blood pressure variability is an independent predictor of cardiovascular disease. Defecation status has also been associated with the risk of developing cardiovascular disease. This study aimed to investigate the association between blood pressure variability and defecation status. A total of 184 participants who could measure their home blood pressure for at least 8 days monthly, both at baseline and 1 year later, were included in this study. All participants had their home blood pressure measured using HEM-9700T (OMRON Healthcare). Day-to-day variability of systolic blood pressure was assessed using the coefficient of variation of home systolic blood pressure during 1 month. Data on defecation status was obtained using a questionnaire survey. Eighty-nine patients had an elevated coefficient of variation at 1 year. The proportion of participants with elevated coefficient of variation at 1 year was significantly higher in the no daily bowel movement group than in the daily bowel movement group (72% vs. 42%, P = 0.001). In multivariable logistic regression analysis with the elevated coefficient of variation at 1 year as the objective variable and age, sex, no daily bowel movement, taking medications, including antihypertensive drugs, laxatives, and intestinal preparations, and coefficient of variation at baseline as independent variables, no daily bowel movement was independently associated with the elevated coefficient of variation at 1 year (odds ratio: 3.81, 95% confidence interval: 1.64–8.87, P = 0.0019). In conclusion, no daily bowel movement was independently associated with elevated day-to-day blood pressure variability at 1 year.

Relationship between defecation status and blood pressure level or blood pressure variability.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
SPRINT Research Group, Wright JT Jr, Williamson JD, Whelton PK, Snyder JK, Sink KM, et al. A randomized trial of intensive versus standard blood-pressure control. N. Engl J Med. 2015;373:2103–16.
Rothwell PM, Howard SC, Dolan E, O’Brien E, Dobson JE, Dahlöf B, et al. Prognostic significance of visit-to-visit variability, maximum systolic blood pressure, and episodic hypertension. Lancet. 2010;375:895–905.
Hoshide S, Yano Y, Mizuno H, Kanegae H, Kario K. Day-by-day variability of home blood pressure and incident cardiovascular disease in clinical practice: the J-HOP Study (Japan Morning Surge-Home Blood Pressure). Hypertension. 2018;71:177–84.
Kikuya M, Ohkubo T, Metoki H, Asayama K, Hara A, Obara T, et al. Day-by-day variability of blood pressure and heart rate at home as a novel predictor of prognosis: the Ohasama study. Hypertension. 2008;52:1045–50.
Satoh M, Hosaka M, Asayama K, Kikuya M, Inoue R, Metoki H, et al. Association between N-terminal pro B-type natriuretic peptide and day-to-day blood pressure and heart rate variability in a general population: the Ohasama study. J Hypertens. 2015;33:1536–41.
Kawai T, Ohishi M, Kamide K, Onishi M, Takeya Y, Tatara Y, et al. The impact of visit-to-visit variability in blood pressure on renal function. Hypertens Res. 2012;35:239–43.
Kawai T, Ohishi M, Kamide K, Nakama C, Onishi M, Ito N, et al. Differences between daytime and nighttime blood pressure variability regarding systemic atherosclerotic change and renal function. Hypertens Res. 2013;36:232–9.
Kubozono T, Akasaki Y, Kawasoe S, Ojima S, Kawabata T, Makizako H, et al. The relationship between day-to-day variability in home blood pressure measurement and multiple organ function. Hypertens Res. 2022;45:474–82.
Godai K, Kabayama M, Gondo Y, Yasumoto S, Sekiguchi T, Noma T, et al. Day-to-day blood pressure variability is associated with lower cognitive performance among the Japanese community-dwelling oldest-old population: the SONIC study. Hypertens Res. 2020;43:404–11.
Oishi E, Ohara T, Sakata S, Fukuhara M, Hata J, Yoshida D, et al. Day-to-day blood pressure variability and risk of dementia in a general Japanese elderly population: the Hisayama Study. Circulation. 2017;136:516–25.
Matsumoto A, Satoh M, Kikuya M, Ohkubo T, Hirano M, Inoue R, et al. Day-to-day variability in home blood pressure is associated with cognitive decline: the Ohasama study. Hypertension. 2014;63:1333–8.
Hisamatsu T, Ohkubo T. Home blood pressure variability and target organ damage. Hypertens Res. 2022;45:543–5.
Tang WH, Wang Z, Levison BS, Koeth RA, Britt EB, Fu X, et al. Intestinal microbial metabolism of phosphatidylcholine and cardiovascular risk. N. Engl J Med. 2013;368:1575–84.
Wang Z, Klipfell E, Bennett BJ, Koeth R, Levison BS, Dugar B, et al. Gut flora metabolism of phosphatidylcholine promotes cardiovascular disease. Nature. 2011;472:57–63.
Chang JY, Locke GR 3rd, McNally MA, Halder SL, Schleck CD, Zinsmeister AR, et al. Impact of functional gastrointestinal disorders on survival in the community. Am J Gastroenterol. 2010;105:822–32.
Kubota Y, Iso H, Tamakoshi A. Bowel movement frequency, laxative use, and mortality from coronary heart disease and stroke among Japanese men and women: the Japan Collaborative Cohort (JACC) Study. J Epidemiol. 2016;26:242–8.
Mishima E, Abe T. Role of the microbiota in hypertension and antihypertensive drug metabolism. Hypertens Res. 2022;45:246–53.
Luo S, Zhao Y, Zhu S, Liu L, Cheng K, Ye B, et al. Flavonifractor plautii protects against elevated arterial stiffness. Circ Res. 2023;132:167–81.
Yang T, Santisteban MM, Rodriguez V, Li E, Ahmari N, Carvajal JM, et al. Gut dysbiosis is linked to hypertension. Hypertension. 2015;65:1331–40.
Karlsson FH, Fåk F, Nookaew I, Tremaroli V, Fagerberg B, Petranovic D, et al. Symptomatic atherosclerosis is associated with an altered gut metagenome. Nat Commun. 2012;3:1245.
Zhu L, Liu W, Alkhouri R, Baker RD, Bard JE, Quigley EM, et al. Structural changes in the gut microbiome of constipated patients. Physiol Genom. 2014;46:679–86.
Kassinen A, Krogius-Kurikka L, Mäkivuokko H, Rinttilä T, Paulin L, Corander J, et al. The fecal microbiota of irritable bowel syndrome patients differs significantly from that of healthy subjects. Gastroenterology. 2007;133:24–33.
Khalif IL, Quigley EM, Konovitch EA, Maximova ID. Alterations in the colonic flora and intestinal permeability and evidence of immune activation in chronic constipation. Dig Liver Dis. 2005;37:838–49.
Parthasarathy G, Chen J, Chen X, Chia N, O’Connor HM, Wolf PG, et al. Relationship between microbiota of the colonic mucosa vs feces and symptoms, colonic transit, and methane production in female patients with chronic constipation. Gastroenterology. 2016;150:367–79.e1.
Ali MK, Chen JDZ. Roles of heart rate variability in assessing autonomic nervous system in functional gastrointestinal disorders: a systematic review. Diagnostics (Basel). 2023;13:293.
Ishiyama Y, Hoshide S, Kanegae H, Kario K. Increased arterial stiffness amplifies the association between home blood pressure variability and cardiac overload: the J-HOP study. Hypertension. 2020;75:1600–6.
Grassi G, Bombelli M, Seravalle G, Dell’Oro R, Quarti-Trevano F. Diurnal blood pressure variation and sympathetic activity. Hypertens Res. 2010;33:381–5.
Schiller LR. Definitions, pathophysiology, and evaluation of chronic diarrhoea. Best Pr Res Clin Gastroenterol. 2012;26:551–62.
Liu Z, Wei F, Zhao Y, Lu F, Zhang H, Diao Y, et al. Day-by-day variability of self-measured blood pressure at home associated with cold pressor test norepinephrine, and heart rate variability in normotensive to moderate hypertensive. Int J Cardiol. 2013;168:4574–6.
Nagai M, Fujiwara T, Kario K. Day-to-day blood pressure variability and severity of COVID-19: is sympathetic overdrive a potential link? J Clin Hypertens. 2021;23:1681–3.
Fukui M, Ushigome E, Tanaka M, Hamaguchi M, Tanaka T, Atsuta H, et al. Home blood pressure variability on one occasion is a novel factor associated with arterial stiffness in patients with type 2 diabetes. Hypertens Res. 2013;36:219–25.
Matsui Y, O’Rourke MF, Hoshide S, Ishikawa J, Shimada K, Kario K. Combined effect of angiotensin II receptor blocker and either a calcium channel blocker or diuretic on day-by-day variability of home blood pressure: the Japan Combined Treatment With Olmesartan and a Calcium-Channel Blocker Versus Olmesartan and Diuretics randomized efficacy study. Hypertension. 2012;59:1132–8.
Obara T, Kikuya M, Kobayashi Y, Ishikura K, Ikeda U, Ishikuro M, et al. Associations between visit-to-visit variability in blood pressure measured in the office and antihypertensive drugs: the J-HOME-Morning study. Clin Exp Hypertens. 2013;35:285–90.
Satoh M, Metoki H, Asayama K, Murakami T, Inoue R, Tsubota-Utsugi M, et al. Age-related trends in home blood pressure, home pulse rate, and day-to-day blood pressure and pulse rate variability based on longitudinal cohort data: the ohasama study. J Am Heart Assoc. 2019;8:e012121.
Acknowledgements
We would like to thank Chikashi Yamaguchi and Kohko Horinouchi of the MeRAS Corporation for their help in obtaining BP data measured by the participants. This study was conducted by OMRON HEALTHCARE Co. Ltd. in cooperation with the Department of Cardiovascular Medicine and Hypertension, Graduate School of Medical and Dental Sciences, Kagoshima University. The running cost of this observational study was funded by OMRON Healthcare Co., Ltd.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
TK, AY, and MO received research support from Omron Healthcare Co., Ltd. SF is an employee of OMRON Healthcare Co., Ltd.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kubozono, T., Akasaki, Y., Kawasoe, S. et al. Relationship between defecation status and blood pressure level or blood pressure variability. Hypertens Res 47, 128–136 (2024). https://doi.org/10.1038/s41440-023-01435-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-023-01435-3
Keywords
This article is cited by
-
Reevaluating Adiponectin’s impact on obesity hypertension: a Chinese case-control study
BMC Cardiovascular Disorders (2024)
-
Hypertension facilitates age-related diseases. ~ Is hypertension associated with a wide variety of diseases?~
Hypertension Research (2024)
-
Constipation and high blood pressure variability
Hypertension Research (2024)