Abstract
The incidence and prevalence of kidney stones have increased over the past four decades. However, the diagnosis of ‘kidney stone’ can range from an incidental asymptomatic finding of limited clinical significance to multiple painful episodes of ureteral obstruction with eventual kidney failure. Some general strategies may be useful to prevent the recurrence of kidney stones. In particular, greater attention to kidney stone classification, approaches to assessing the risk of recurrence and individualized prevention strategies may improve the clinical care of stone formers. Although there have been some advances in approaches to predicting the recurrence of kidney stones, notable challenges remain. Studies of kidney stone prevalence, incidence and recurrence have reported inconsistent findings, in part because of the lack of a standardized stone classification system. A kidney stone classification system based on practical and clinically useful measures of stone disease may help to improve both the study and clinical care of stone formers. Any future kidney stone classification system should be aimed at distinguishing asymptomatic from symptomatic stones, clinically diagnosed symptomatic stone episodes from self-reported symptomatic stone episodes, symptomatic stone episodes that are confirmed from those that are suspected, symptomatic recurrence from radiographic recurrence (that is, with radiographic evidence of a new stone, stone growth or stone disappearance from presumed passage) and determine stone composition based on mutually exclusive categories.
Key points
-
Kidney stones can range from an asymptomatic incidental finding with limited clinical significance to a painful recurrent disorder with substantial morbidity.
-
The prevalence and incidence of kidney stones has increased worldwide, but some of this increase is due to improvements in medical imaging with increased utilization of CT.
-
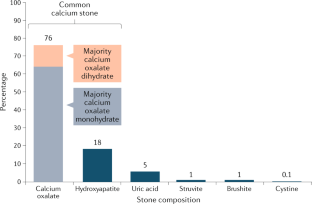
Classifying stone formers according to their clinical presentation and stone composition can help to predict the risk of future symptomatic stone episodes and aid personalization of stone prevention strategies.
-
The wide range of recurrence rates reported between different studies might largely be due to the use of different definitions that include various degrees of symptomatic evidence of recurrence and/or radiographic manifestations of recurrence.
-
Risk factors for symptomatic kidney stone recurrence include younger age, male gender, family history of stones, obesity, pregnancy, rarer stone compositions, higher radiographic kidney stone burden, number of past symptomatic kidney stone episodes and fewer years since last kidney stone episode.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Scales, C. D. Jr., Smith, A. C., Hanley, J. M. & Saigal, C. S. Urologic Diseases in America Project. Prevalence of kidney stones in the United States. Eur. Urol. 62, 160–165 (2012).
Stamatelou, K. K., Francis, M. E., Jones, C. A., Nyberg, L. M. & Curhan, G. C. Time trends in reported prevalence of kidney stones in the United States: 1976–1994. Kidney Int. 63, 1817–1823 (2003).
Trinchieri, A. et al. Increase in the prevalence of symptomatic upper urinary tract stones during the last ten years. Eur. Urol. 37, 23–25 (2000).
Hesse, A., Brandle, E., Wilbert, D., Kohrmann, K. U. & Alken, P. Study on the prevalence and incidence of urolithiasis in Germany comparing the years 1979 vs. 2000. Eur. Urol. 44, 709–713 (2003).
Penniston, K. L., McLaren, I. D., Greenlee, R. T. & Nakada, S. Y. Urolithiasis in a rural Wisconsin population from 1992 to 2008: narrowing of the male-to-female ratio. J. Urol. 185, 1731–1736 (2011).
Liu, Y. et al. Epidemiology of urolithiasis in Asia. Asian J. Urol. 5, 205–214 (2018).
Sorokin, I. et al. Epidemiology of stone disease across the world. World J. Urol. 35, 1301–1320 (2017).
Pearle, M. S., Calhoun, E. A. & Curhan, G. C. Urologic Diseases of America Project. Urologic diseases in America project: urolithiasis. J. Urol. 173, 848–857 (2005).
Kittanamongkolchai, W. et al. The changing incidence and presentation of urinary stones over 3 decades. Mayo Clin. Proc. 93, 291–299 (2018).
Dwyer, M. E. et al. Temporal trends in incidence of kidney stones among children: a 25-year population based study. J. Urol. 188, 247–252 (2012).
Tasian, G. E. et al. Annual incidence of nephrolithiasis among children and adults in South Carolina from 1997 to 2012. Clin. J. Am. Soc. Nephrol. 11, 488–496 (2016).
Edvardsson, V. O., Indridason, O. S., Haraldsson, G., Kjartansson, O. & Palsson, R. Temporal trends in the incidence of kidney stone disease. Kidney Int. 83, 146–152 (2013).
Edvardsson, V. O., Ingvarsdottir, S. E., Palsson, R. & Indridason, O. S. Incidence of kidney stone disease in Icelandic children and adolescents from 1985 to 2013: results of a nationwide study. Pediatr. Nephrol. 33, 1375–1384 (2018).
Yasui, T., Iguchi, M., Suzuki, S. & Kohri, K. Prevalence and epidemiological characteristics of urolithiasis in Japan: national trends between 1965 and 2005. Urology 71, 209–213 (2008).
Krambeck, A. E. et al. Effect of age on the clinical presentation of incident symptomatic urolithiasis in the general population. J. Urol. 189, 158–164 (2013).
Brisbane, W., Bailey, M. R. & Sorensen, M. D. An overview of kidney stone imaging techniques. Nat. Rev. Urol. 13, 654–662 (2016).
Semins, M. J. & Matlaga, B. R. Kidney stones during pregnancy. Nat. Rev. Urol. 11, 163–168 (2014).
Smith-Bindman, R. et al. Ultrasonography versus computed tomography for suspected nephrolithiasis. N. Engl. J. Med. 371, 1100–1110 (2014).
Sternberg, K. M. et al. Is hydronephrosis on ultrasound predictive of ureterolithiasis in patients with renal colic? J. Urol. 196, 1149–1152 (2016).
Chi, T., Miller, J. & Stoller, M. L. Randall plaque versus renal stone? Transl. Androl. Urol. 1, 66–70 (2012).
Dhondup, T. et al. Risk of ESRD and mortality in kidney and bladder stone formers. Am. J. Kidney Dis. 72, 790–797 (2018).
Emamian, S. A., Nielsen, M. B., Pedersen, J. F. & Ytte, L. Sonographic evaluation of renal appearance in 665 adult volunteers. Correlation age obesity. Acta Radiol. 34, 482–485 (1993).
Oshibuchi, M., Nishi, F., Sato, M., Ohtake, H. & Okuda, K. Frequency of abnormalities detected by abdominal ultrasound among Japanese adults. J. Gastroenterol. Hepatol. 6, 165–168 (1991).
Buchholz, N. P. et al. The prevalence of silent kidney stones — an ultrasonographic screening study. J. Pak. Med. Assoc. 53, 24–25 (2003).
Passerotti, C. et al. Ultrasound versus computerized tomography for evaluating urolithiasis. J. Urol. 182, 1829–1834 (2009).
Brenner, D. J. & Hall, E. J. Computed tomography — an increasing source of radiation exposure. N. Engl. J. Med. 357, 2277–2284 (2007).
Lorenz, E. C. et al. Clinical characteristics of potential kidney donors with asymptomatic kidney stones. Nephrol. Dial. Transpl. 26, 2695–2700 (2011).
Durbin, J. M. et al. Genitourinary abnormalities in an asymptomatic screening population: findings on virtual colonoscopy. Clin. Nephrol. 77, 204–210 (2012).
D’Costa, M. R. et al. Symptomatic and radiographic manifestations of kidney stone recurrence and their prediction by risk factors: a prospective cohort study. J. Am. Soc. Nephrol. 30, 1251–1260 (2019).
Li, X. et al. Outcomes of long-term follow-up of asymptomatic renal stones and prediction of stone-related events. BJU Int. 123, 485–492 (2019).
Goldsmith, Z. G. & Lipkin, M. E. When (and how) to surgically treat asymptomatic renal stones. Nat. Rev. Urol. 9, 315–320 (2012).
Selby, M. G. et al. Quantification of asymptomatic kidney stone burden by computed tomography for predicting future symptomatic stone events. Urology 85, 45–50 (2015).
Dropkin, B. M., Moses, R. A., Sharma, D. & Pais, V. M. Jr. The natural history of nonobstructing asymptomatic renal stones managed with active surveillance. J. Urol. 193, 1265–1269 (2015).
Kang, H. W. et al. Natural history of asymptomatic renal stones and prediction of stone related events. J. Urol. 189, 1740–1746 (2013).
Burgher, A., Beman, M., Holtzman, J. L. & Monga, M. Progression of nephrolithiasis: long-term outcomes with observation of asymptomatic calculi. J. Endourol. 18, 534–539 (2004).
Assimos, D. et al. Surgical management of stones: American Urological Association/Endourological Society guideline, part I. J. Urol. 196, 1153–1160 (2016).
Assimos, D. et al. Surgical management of stones: American Urological Association/Endourological Society guideline, part II. J. Urol. 196, 1161–1169 (2016).
Curhan, G. C., Willett, W. C., Speizer, F. E. & Stampfer, M. J. Twenty-four-hour urine chemistries and the risk of kidney stones among women and men. Kidney Int. 59, 2290–2298 (2001).
Chooi, Y. C., Ding, C. & Magkos, F. The epidemiology of obesity. Metabolism 92, 6–10 (2019).
Taylor, E. N., Stampfer, M. J. & Curhan, G. C. Obesity, weight gain, and the risk of kidney stones. JAMA 293, 455–462 (2005).
Geiss, L. S. et al. Prevalence and incidence trends for diagnosed diabetes among adults aged 20 to 79 years, United States, 1980–2012. JAMA 312, 1218–1226 (2014).
Taylor, E. N., Stampfer, M. J. & Curhan, G. C. Diabetes mellitus and the risk of nephrolithiasis. Kidney Int. 68, 1230–1235 (2005).
Meyer, K. A. et al. Twenty-two-year population trends in sodium and potassium consumption: the Minnesota Heart Survey. J. Am. Heart Assoc. 2, e000478 (2013).
Sorensen, M. D. et al. Impact of nutritional factors on incident kidney stone formation: a report from the WHI OS. J. Urol. 187, 1645–1649 (2012).
Muldowney, F. P., Freaney, R. & Moloney, M. F. Importance of dietary sodium in the hypercalciuria syndrome. Kidney Int. 22, 292–296 (1982).
Curhan, G. C., Willett, W. C., Speizer, F. E., Spiegelman, D. & Stampfer, M. J. Comparison of dietary calcium with supplemental calcium and other nutrients as factors affecting the risk for kidney stones in women. Ann. Intern. Med. 126, 497–504 (1997).
Daniel, C. R., Cross, A. J., Koebnick, C. & Sinha, R. Trends in meat consumption in the USA. Public. Health Nutr. 14, 575–583 (2011).
Taylor, E. N., Stampfer, M. J. & Curhan, G. C. Dietary factors and the risk of incident kidney stones in men: new insights after 14 years of follow-up. J. Am. Soc. Nephrol. 15, 3225–3232 (2004).
Breslau, N. A., Brinkley, L., Hill, K. D. & Pak, C. Y. Relationship of animal protein-rich diet to kidney stone formation and calcium metabolism. J. Clin. Endocrinol. Metab. 66, 140–146 (1988).
Gross, L. S., Li, L., Ford, E. S. & Liu, S. Increased consumption of refined carbohydrates and the epidemic of type 2 diabetes in the United States: an ecologic assessment. Am. J. Clin. Nutr. 79, 774–779 (2004).
Curhan, G. C., Willett, W. C., Knight, E. L. & Stampfer, M. J. Dietary factors and the risk of incident kidney stones in younger women: Nurses’ Health Study II. Arch. Intern. Med. 164, 885–891 (2004).
Lemann, J. Jr., Piering, W. F. & Lennon, E. J. Possible role of carbohydrate-induced calciuria in calcium oxalate kidney-stone formation. N. Engl. J. Med. 280, 232–237 (1969).
Bleich, S. N., Wang, Y. C., Wang, Y. & Gortmaker, S. L. Increasing consumption of sugar-sweetened beverages among US adults: 1988–1994 to 1999–2004. Am. J. Clin. Nutr. 89, 372–381 (2009).
Ferraro, P. M., Taylor, E. N., Gambaro, G. & Curhan, G. C. Soda and other beverages and the risk of kidney stones. Clin. J. Am. Soc. Nephrol. 8, 1389–1395 (2013).
Fakheri, R. J. & Goldfarb, D. S. Ambient temperature as a contributor to kidney stone formation: implications of global warming. Kidney Int. 79, 1178–1185 (2011).
Soucie, J. M., Coates, R. J., McClellan, W., Austin, H. & Thun, M. Relation between geographic variability in kidney stones prevalence and risk factors for stones. Am. J. Epidemiol. 143, 487–495 (1996).
Soucie, J. M., Thun, M. J., Coates, R. J., McClellan, W. & Austin, H. Demographic and geographic variability of kidney stones in the United States. Kidney Int. 46, 893–899 (1994).
Boscolo-Berto, R. et al. Do weather conditions influence the onset of renal colic? A novel approach to analysis. Urol. Int. 80, 19–25 (2008).
Chen, Y. K., Lin, H. C., Chen, C. S. & Yeh, S. D. Seasonal variations in urinary calculi attacks and their association with climate: a population based study. J. Urol. 179, 564–569 (2008).
Chauhan, V., Eskin, B., Allegra, J. R. & Cochrane, D. G. Effect of season, age, and gender on renal colic incidence. Am. J. Emerg. Med. 22, 560–563 (2004).
Brikowski, T. H., Lotan, Y. & Pearle, M. S. Climate-related increase in the prevalence of urolithiasis in the United States. Proc. Natl Acad. Sci. USA 105, 9841–9846 (2008).
Rule, A. D. et al. The ROKS nomogram for predicting a second symptomatic stone episode. J. Am. Soc. Nephrol. 25, 2878–2886 (2014).
Vaughan, L. E. et al. Predictors of symptomatic kidney stone recurrence after the first and subsequent episodes. Mayo Clin. Proc. 94, 202–210 (2019).
Singh, P. et al. Stone composition among first-time symptomatic kidney stone formers in the community. Mayo Clin. Proc. 90, 1356–1365 (2015).
Lieske, J. C. et al. Stone composition as a function of age and sex. Clin. J. Am. Soc. Nephrol. 9, 2141–2146 (2014).
Knoll, T. et al. Urolithiasis through the ages: data on more than 200,000 urinary stone analyses. J. Urol. 185, 1304–1311 (2011).
Daudon, M. et al. Sex- and age-related composition of 10 617 calculi analyzed by infrared spectroscopy. Urol. Res. 23, 319–326 (1995).
Ye, Z. et al. The status and characteristics of urinary stone composition in China. BJU Int. 125, 801–809 (2019).
Worcester, E. M., Bergsland, K. J., Gillen, D. L. & Coe, F. L. Mechanism for higher urine pH in normal women compared with men. Am. J. Physiol. Renal Physiol 314, F623–F629 (2018).
Kohri, K. et al. Relationship between metabolic acidosis and calcium phosphate urinary stone formation in women. Int. Urol. Nephrol. 23, 307–316 (1991).
Maalouf, N. M. Metabolic syndrome and the genesis of uric acid stones. J. Ren. Nutr. 21, 128–131 (2011).
Sakhaee, K. & Maalouf, N. M. Metabolic syndrome and uric acid nephrolithiasis. Semin. Nephrol. 28, 174–180 (2008).
Morgan, M. S. & Pearle, M. S. Medical management of renal stones. BMJ 352, i52 (2016).
Pearle, M. S. et al. Medical management of kidney stones: AUA guideline. J. Urol. 192, 316–324 (2014).
Qaseem, A. et al. Dietary and pharmacologic management to prevent recurrent nephrolithiasis in adults: a clinical practice guideline from the American College of Physicians. Ann. Intern. Med. 161, 659–667 (2014).
Skolarikos, A. et al. Metabolic evaluation and recurrence prevention for urinary stone patients: EAU guidelines. Eur. Urol. 67, 750–763 (2015).
D’Costa, M. R., Pais, V. M. & Rule, A. D. Leave no stone unturned: defining recurrence in kidney stone formers. Curr. Opin. Nephrol. Hypertens. 28, 148–153 (2019).
Sternberg, K. M. et al. Ultrasonography significantly overestimates stone size when compared to low-dose, noncontrast computed tomography. Urology 95, 67–71 (2016).
Williams, R. E. Long-term survey of 538 patients with upper urinary tract stone. Br. J. Urol. 35, 416–437 (1963).
Marshall, V., White, R. H., De Saintonge, M. C., Tresidder, G. C. & Blandy, J. P. The natural history of renal and ureteric calculi. Br. J. Urol. 47, 117–124 (1975).
Sutherland, J. W., Parks, J. H. & Coe, F. L. Recurrence after a single renal stone in a community practice. Min. Electrolyte Metab. 11, 267–269 (1985).
Steyerberg, E. W. et al. Assessing the performance of prediction models: a framework for traditional and novel measures. Epidemiology 21, 128–138 (2010).
Iremashvili, V. et al. External validation of the recurrence of kidney stone nomogram in a surgical cohort. J. Endourol. 33, 475–479 (2019).
Emmott, A. S., Brotherhood, H. L., Paterson, R. F., Lange, D. & Chew, B. H. Complications, re-intervention rates, and natural history of residual stone fragments after percutaneous nephrolithotomy. J. Endourol. 32, 28–32 (2018).
Chew, B. H. et al. Natural history, complications and re-intervention rates of asymptomatic residual stone fragments after ureteroscopy: a report from the EDGE research consortium. J. Urol. 195, 982–986 (2016).
Alexander, C. E., Gowland, S., Cadwallader, J., Reynard, J. M. & Turney, B. W. Shock wave lithotripsy (SWL): outcomes from a national SWL database in New Zealand. BJU Int. 117 (Suppl. 4), 76–81 (2016).
Javanmard, B., Kashi, A. H., Mazloomfard, M. M., Ansari Jafari, A. & Arefanian, S. Retrograde intrarenal surgery versus shock wave lithotripsy for renal stones smaller than 2 cm: a randomized clinical trial. Urol. J. 13, 2823–2828 (2016).
Albala, D. M. et al. Lower pole I: a prospective randomized trial of extracorporeal shock wave lithotripsy and percutaneous nephrostolithotomy for lower pole nephrolithiasis-initial results. J. Urol. 166, 2072–2080 (2001).
Bozzini, G. et al. A prospective randomized comparison among SWL, PCNL and RIRS for lower calyceal stones less than 2 cm: a multicenter experience: a better understanding on the treatment options for lower pole stones. World J. Urol. 35, 1967–1975 (2017).
Ferraro, P. M., Curhan, G. C., D’Addessi, A. & Gambaro, G. Risk of recurrence of idiopathic calcium kidney stones: analysis of data from the literature. J. Nephrol. 30, 227–233 (2017).
Fink, H. A. et al. Medical management to prevent recurrent nephrolithiasis in adults: a systematic review for an American College of Physicians clinical guideline. Ann. Intern. Med. 158, 535–543 (2013).
Author information
Authors and Affiliations
Contributions
C.T. and A.D.R. researched data for the article. All authors contributed to discussion of the article’s content, writing and review/editing of the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Peer review information
Nature Reviews Nephrology thanks D. Goldfarb and R. Pálsson for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
Recurrence of Kidney Stone (ROKS) tool: https://qxmd.com/calculate/calculator_438/roks-recurrence-of-kidney-stone-2018
Glossary
- Shockwave lithotripsy
-
A procedure for treating stones in the kidney or ureter using a high-energy shock wave from outside the body to break stones into fragments that are small enough to spontaneously pass in urine.
- Ureteroscopy
-
A procedure in which a small scope is inserted into the ureter via the urethra and bladder to diagnose and treat a variety of problems in the urinary tract. In the case of urinary stones, it allows the urologist to actually look into the ureter or kidney, find the stone and remove or fragment the stone.
- Nephrolithotomy
-
A procedure used to remove kidney stones from the body when they cannot pass spontaneously.
Rights and permissions
About this article
Cite this article
Thongprayoon, C., Krambeck, A.E. & Rule, A.D. Determining the true burden of kidney stone disease. Nat Rev Nephrol 16, 736–746 (2020). https://doi.org/10.1038/s41581-020-0320-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41581-020-0320-7
This article is cited by
-
The SOX4/EZH2/SLC7A11 signaling axis mediates ferroptosis in calcium oxalate crystal deposition-induced kidney injury
Journal of Translational Medicine (2024)
-
Exploring the impact of digital health literacy on quality of life in patients undergoing retrograde intrarenal surgery for kidney stone treatment: a prospective, single-center study
Urolithiasis (2024)
-
Cymbopogon proximus and Petroselinum crispum seed ethanolic extract/Gum Arabic nanogel emulsion: Preventing ethylene glycol and ammonium chloride-induced urolithiasis in rats
Urolithiasis (2024)
-
Surgical procedure and recurrence of upper urinary tract stone: a national-wide study based on hospitalized patients
World Journal of Urology (2024)
-
Gaps in kidney stone disease management: From clinical theory to patient reality
Urolithiasis (2024)



