Abstract
Bacterial vaginosis (BV) causes genital inflammation and increased HIV acquisition risk. The standard-of-care for BV, antibiotic therapy, is associated with high recurrence rates. Probiotics may improve treatment outcomes, although substantial heterogeneity in efficacy has been observed during clinical trials. To evaluate the potential to improve existing probiotics, we compared the inflammatory and antimicrobial (adhesion, H2O2, D-lactate and L-lactate production) characteristics of 23 vaginal Lactobacillus isolates from South African women, commercial vaginal probiotics (L. casei rhamnosus, L. acidophilus) and 4 reference strains. All lactobacilli induced inflammatory cytokine production by genital epithelial cells and produced D-lactate. Of six isolates assessed, five suppressed inflammatory responses to Gardnerella vaginalis. Although the L. acidophilus probiotic was the most adherent, many clinical isolates produced greater amounts of H2O2, D-lactate and L-lactate than the probiotics. The most L-lactate and H2O2 were produced by L. jensenii (adjusted p = 0.0091) and L. mucosae (adjusted p = 0.0308) species, respectively. According to the characteristics evaluated, the top 10 isolates included 4 L. jensenii, 2 L. crispatus, 1 L. mucosae, 1 L. vaginalis and the L. acidophilus probiotic. There is potential to develop an improved vaginal probiotic using clinical Lactobacillus isolates. Inflammatory profiles are critical to evaluate as some isolates induced substantial cytokine production.
Similar content being viewed by others
Introduction
Bacterial vaginosis (BV) is a highly prevalent dysbiosis of the vaginal microbiota that is characterized by a shift from predominantly Lactobacillus species to a diverse population including pathogenic bacteria, such as Gardnerella vaginalis and Prevotella spp1. BV has been found to increase the risk of HIV acquisition in women, mother-to-child transmission and transmission from women with BV to their male partners, as well as reduce the efficacy of some forms of antiretroviral pre-exposure prophylaxis2,3,4,5,6. Additionally, BV is associated with increased susceptibility to other sexually transmitted infections (STIs) and severe reproductive complications in women7,8. Although the underlying mechanisms are not fully understood, these outcomes may be partly mediated by increases in vaginal pro-inflammatory cytokine concentrations and immune cell activation in the female genital tracts (FGTs) of women with BV9. The relationship between BV and HIV is particularly concerning in South Africa, where approximately 18% of the adult population aged 15–49 years is HIV-infected10 and BV prevalence rates are reported to exceed 50% in some regions11.
Lactobacillus species, which dominate in a healthy FGT, are thought to protect against BV, HIV and other STIs by a number of mechanisms. Lactic acid produced by lactobacilli hinders the growth of potential pathogens and inactivates HIV12,13, partly by maintaining the physiological pH of the vagina below 4.514. Lactic acid exists as both D- and L-isomers; while L-lactic acid has been found to inactivate HIV more effectively than D-lactic acid15, D-lactic acid is thought to play a more important role in inhibiting bacterial pathogens, including Chlamydia trachomatis16,17. Many lactobacilli also produce hydrogen peroxide (H2O2), which has a virucidal effect on HIV by inhibiting viral adhesion and replication18. However, the role of H2O2 in protection against BV-associated bacteria is controversial, as some studies have reported that physiological concentrations are not microbicidal and that, at microbicidal concentrations, H2O2 inhibits lactobacilli more effectively than pathogenic bacteria19. Competitive exclusion is another important protective mechanism utilized by lactobacilli, whereby adherent lactobacilli prevent the adhesion of pathogens to the vaginal epithelium and thus colonization20. Genital inflammation caused by BV and STIs increases risk of HIV acquisition21. Suppression of inflammatory responses by lactobacilli and lactic acid is another proposed mechanism for reduced susceptibility to HIV in women with Lactobacillus-dominant microbiota22.
As the standard-of-care for BV, antibiotic treatment, is associated with high recurrence rates14,23, there is an urgent need to develop better treatment strategies, particularly in regions of high HIV prevalence. Several randomized clinical trials have evaluated Lactobacillus-containing probiotics for BV treatment, alone or as adjunctive therapy with antibiotics24,25. Although some trials have demonstrated improved BV outcomes with probiotics, the results have been heterogeneous, with some studies finding no benefit24,25. One of the limitations of many of these probiotic formulations is that they include bacterial species that are not adapted for survival in the FGT and are not usually found in women with healthy vaginal microbiota26. It is also possible that probiotics containing Lactobacillus isolates from one population may have reduced efficacy when used in another population, as major geographical and ethnic differences have been observed in the vaginal microbiota and host factors that may influence bacterial colonization27,28. Therefore, using vagina-specific Lactobacillus species with effective antimicrobial properties that have been isolated from within the population of intended use may improve BV treatment outcomes. The aims of this study were to compare the antimicrobial and inflammatory characteristics of existing vaginal probiotics on the South African market to those of clinical Lactobacillus isolates from the FGTs of South African women.
Results
Study population and Lactobacillus isolates
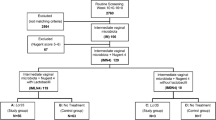
Clinical Lactobacillus strains (n = 23) were isolated from cervicovaginal samples from nine women residing in Cape Town, South Africa (Table 1)29. Of these, six women had no STIs or BV, two had BV and one was infected with Chlamydia trachomatis. All of the women were PCR negative for other STIs including: Neisseria gonorrhoeae, Trichomonas vaginalis, Mycoplasma genitalium, herpes simplex virus (HSV)-1, HSV-2 and Treponema pallidum. The 23 clinical Lactobacillus isolates included seven L. crispatus (LC1–7), one L. gasseri (LG1), five L. jensenii (LJ1–5), four L. mucosae (LM1–4) and six L. vaginalis (LV1–6). Two commercial vaginal probiotics were found on the South African market and lactobacilli isolated from these probiotics were evaluated. One probiotic contained L. acidophilus in vaginal tablet and oral capsule formulations, and the other contained L. casei rhamnosus Lcr35 in a vaginal capsule. Four American Type Culture Collection (ATCC) reference strains [33197 (L. crispatus), 33820 (L. crispatus), 9857 (L. gasseri), 25258 (L. jensenii)] were also included.
The sizes and growth rates (under anaerobic conditions) of the clinical and probiotic lactobacilli, both inter- and intra-species were varied (Fig. 1). The L. acidophilus probiotic isolate tended to be larger than the majority of the clinical isolates, with the exception of some of the L. crispatus and L. jensenii isolates (Fig. 1A). The probiotic isolate L. casei rhamnosus grew most rapidly, followed by L. crispatus isolates and the L. acidophilus probiotic (Fig. 1B), although these differences were not statistically significant.
Size, growth rates and adhesion of Lactobacillus isolates. (A) Bacterial length was evaluated using microscopy and lengths of different isolates grouped by species are shown, with species ordered from largest to smallest. Lines indicate medians of species (5 measurements per isolate), bars indicate the interquartile ranges and error bars indicate the ranges. (B) Growth rates were evaluated by inoculating MRS broth with 4.18 × 106 colony forming units (CFU) of each isolate, incubating anaerobically at 37 °C, and measuring the optical densities (600 nm) of cultures at various time-points. Growth rates by species are shown with symbols indicating means and error bars indicating the standard errors of the means of different isolates of the same species. (C–H) Lactobacillus adhesion to CaSki (ectocervical epithelial) cells was assessed by adding optical density (OD)-adjusted bacteria (OD600 0.1 ± 0.01) to cell monolayers, incubating for 2 h and washing to remove unbound bacteria. (C) Adhesion was evaluated in three separate experiments for each isolate. Following addition of bacteria and a 2 h incubation period, cells were lifted and plated on MRS agar and colony-forming units were counted. Adhesion is expressed as the percentage of the number of bacteria added to the monolayers that remained adherent. Different isolates of the same species were grouped together and species are ordered from the most to least adhesive. Lines indicate medians, bars indicate the interquartile ranges and error bars indicate the ranges. (D) The level of adhesion of each isolate is shown separately, with bars indicating medians and error bars indicating the ranges of adhesion evaluated in three separate experiments. (E–H) Adhesion was assessed qualitatively by Gram staining and collecting images at 1000x magnification using a light microscope. Mann-Whitney test was used for comparisons between species and p-values < 0.05 after adjustment for multiple comparisons were considered statistically significant. LA: Lactobacillus acidophilus probiotic (n = 2); LC: Lactobacillus crispatus (n = 9); LCR: Lactobacillus casei rhamnosus probiotic (n = 1); LG: Lactobacillus gasseri (n = 2); LM: Lactobacillus mucosae (n = 4); LV: Lactobacillus vaginalis (n = 6); LJ: Lactobacillus jensenii (n = 6). *ATCC reference strains.
Lactobacillus adhesion to genital epithelial cells
Lactobacillus isolates were tested for their ability to adhere to CaSki (ectocervical epithelial) cells (Fig. 1C–H). Overall, the L. acidophilus probiotic isolate was the most adherent, although there was a large difference between the adhesion of the isolate obtained from the capsule (0.006%) versus the isolate obtained from the tablet (2.022%) (Fig. 1C,D). Although there were no statistically significant differences in adhesion between species (Fig. 1C), among the clinical isolates, L. jensenii 1 (LJ1) exhibited the greatest adhesion, with approximately 1.663% of bacteria adhering to the cells (Fig. 1D). Several species included a relatively large proportion of highly adherent strains, with 1/2 (50%) L. acidophilus, 4/6 (67%) L. jensenii, and 1/2 (50%) L. gasseri relatively highly adherent. It has previously been suggested that bacterial size and growth rates may influence adhesion ability30. However, neither bacterial size nor growth rates correlated with Lactobacillus adhesion in this study (Spearman rho = 0.2209, p = 0.2407 and rho = 0.2843, p = 0.1278, respectively; data not shown).
Hydrogen peroxide production
L. mucosae isolates produced the most H2O2 relative to the other strains collectively (p = 0.0044; adjusted p = 0.0308), after a 3 h incubation period under aerobic conditions, followed by L. jensenii isolates (p = 0.0061; adjusted p = 0.0427; data not shown). The other species evaluated produced comparably lower amounts of H2O2 (Fig. 2A). Only one L. crispatus isolate, none of the L. vaginalis isolates and none of the probiotic Lactobacillus isolates produced significant amounts of H2O2 (Fig. 2B). The rates of H2O2 production were similar for all producing isolates, with production being evident within 2 h (Fig. 2B). The level of H2O2 production was not associated with the growth rates of the lactobacilli (rho = −0.1136, p = 0.5501; data not shown).
Antimicrobial characteristics of Lactobacillus isolates. (A,C,E,G) Different isolates of the same species were grouped together and the overall antimicrobial properties of different species are shown, with species ordered according to the amounts of hydrogen peroxide (H2O2), D- and L-lactate produced and culture pH. Lines indicate medians, bars indicate the interquartile ranges and error bars indicate the ranges. (B,D,F,H) Antimicrobial properties for individual isolates are also shown with bars indicating the medians and error bars indicating the ranges of technical replicates within each assay. (A,B) Hydrogen peroxide production after 3 h of aerobic culture was measured in duplicate within the same assay. (C,D) pH levels of bacterial cultures were measured using a pH meter following anaerobic culture at 37 °C for 24 hours. (E,F) D-lactate and (G,H) L-lactate concentrations after a 24 h incubation period at 37 °C under anaerobic conditions were measured in duplicate within the same assays using Lactate Colorimetric kits. Mann-Whitney test was used for comparisons between species and p-values < 0.05 after adjustment for multiple comparisons were considered statistically significant. **Associations that remained statistically significant after adjustment for multiple comparisons. LA: Lactobacillus acidophilus probiotic (n = 2); LC: Lactobacillus crispatus (n = 9); LCR: Lactobacillus casei rhamnosus probiotic (n = 1); LG: Lactobacillus gasseri (n = 2); LM: Lactobacillus mucosae (n = 4); LV: Lactobacillus vaginalis (n = 6); LJ: Lactobacillus jensenii (n = 6). *ATCC reference strains.
D- and L-lactate production and culture acidification
When the lactobacilli were cultured in MRS, it was found that the probiotics lowered the culture pH levels most, followed by the L. crispatus isolates (Fig. 2C,D). In contrast, L. vaginalis and L. mucosae culture pH levels were the highest. Most Lactobacillus isolates produced large amounts of D-lactate, with no significant differences between species after multiple comparisons adjustment (Fig. 2E,F). L-lactate production was however highly varied between isolates (Fig. 2G,H), with L. jensenii isolates producing significantly greater amounts of L-lactate than the other isolates collectively (p = 0.0013, adjusted p = 0.0091; data not shown), followed by L. gasseri and L. vaginalis (Fig. 2G). While all the probiotic isolates produced large amounts of D-lactate, only the probiotic capsule L. acidophilus isolate produced detectable levels of L-lactate (Fig. 2F,H).
The concentration of total lactic acid, calculated using the Henderson-Hasselbalch equation31, correlated with culture pH (rho = 0.8626, p < 0.0001; data not shown). Additionally, there was a trend towards a significant correlation between D-lactate and L-lactate production (Spearman rho = 0.3272, p = 0.0776; data not shown). Although there was a trend towards an inverse correlation between culture pH and bacterial growth rates (rho = −0.3079, p = 0.0978), neither D-lactate (rho = 0.07787, p = 0.6825) nor L-lactate (rho = 0.2520, p = 0.1791) correlated with growth rates (data not shown).
Inflammatory cytokine responses
Inflammatory cytokines produced by CaSki cells in response to 4.18 × 106 colony forming units (CFU) of each Lactobacillus isolate were assessed using Luminex. While several cytokines [including interleukin (IL)-1α, IL-1β, IL-6, IL-8, IFN-γ-inducible protein (IP)-10, macrophage inflammatory protein (MIP)-1α, MIP-1β, MIP-3α, regulated on activation, normal T cell expressed and secreted (RANTES)] were induced, others [including tumor necrosis factor (TNF)-α, interferon (IFN)-γ, IL-17A and IL-10] were not produced (below the minimum levels of detection for all samples; not shown). The relative cytokine production elicited by each of the isolates is shown as a heatmap (Fig. 3A). While most lactobacilli induced very little cytokine production by CaSki cells, some of the isolates were substantially more inflammatory than others, including two L. crispatus isolates, two L. jensenii isolates and the L. acidophilus vaginal tablet isolate which clustered separately from the other isolates assessed (Fig. 3A). Factor analysis was used to group all of the inflammatory cytokines together onto one factor and generate overall inflammatory scores for each isolate (Fig. 3B,C). L. acidophilus was most inflammatory, while L. gasseri isolates were the least inflammatory according to inflammatory factor scores (Fig. 3B), although these differences were not statistically significant. Of the individual isolates assessed, LJ1 was the most inflammatory, while LG1 was the least inflammatory (Fig. 3C).
Inflammatory cytokine production by CaSki cells in response to Lactobacillus isolates. Cytokine production by CaSki cells in response to lactobacilli after a 24 h incubation period at 37 °C under 5% CO2 was measured using Luminex. (A) Unsupervised hierarchical clustering was used to group lactobacilli isolates according to inflammatory responses induced. Inflammatory cytokine concentrations are shown as a heat map, with blue, through white, to red indicating low-high cytokine concentrations, respectively. Data was log10-transformed and scaled in R. Two clustering dendrograms are shown in the figure. The dendrogram above the heat map illustrates degrees of relatedness between different cytokines measured. The dendrogram on the left hand side of the heat map indicates relationships between the expression profiles of the analysed cytokines in response to different clinical Lactobacillus isolates. (B) Different isolates of the same species were grouped together and overall inflammatory responses to each species were determined by grouping all 9 inflammatory cytokines measured onto 1 factor and generating factor scores for the isolates. Species are ordered from most to least inflammatory; lines indicate medians, bars indicate interquartile ranges and error bars indicate ranges. Mann-Whitney test was used for comparisons between species; no significant differences in inflammatory responses were observed between species. (C) Overall inflammatory responses to each isolate. LA: Lactobacillus acidophilus probiotic (n = 2); LC: Lactobacillus crispatus (n = 9); LCR: Lactobacillus casei rhamnosus probiotic (n = 1); LG: Lactobacillus gasseri (n = 2); LM: Lactobacillus mucosae (n = 4); LV: Lactobacillus vaginalis (n = 6); LJ: Lactobacillus jensenii (n = 6). *ATCC reference strains.
To evaluate the impact of D- and L-lactate concentrations on inflammatory responses, these metabolites were measured in lactobacilli-CaSki co-cultures following a 24 hour incubation at 37 °C under aerobic conditions (Fig. 4). It was found that neither D-lactate nor L-lactate correlated significantly with inflammatory cytokine production by CaSki cells (data not shown).
L-lactate and D-lactate production by lactobacilli after a 24 h incubation period with CaSki cells at 37 °C under 5% CO2. D-lactate and L-lactate concentrations after a 24 h incubation period at 37 °C under 5% CO2 in antibiotic-free cell culture medium were measured in duplicate within the same assays using Lactate Colorimetric kits. (A) D- and (C) L-lactate production by isolates grouped according to species are shown. Lines indicate medians, bars indicate the interquartile ranges and error bars indicate the ranges. (B,D) Lactate production by individual isolates is also shown with bars indicating the medians and error bars indicating the ranges of technical replicates within each assay. Mann-Whitney test was used for comparisons between species and p-values < 0.05 after adjustment for multiple comparisons were considered statistically significant. **Associations that remained statistically significant after adjustment for multiple comparisons. LA: Lactobacillus acidophilus probiotic (n = 2); LC: Lactobacillus crispatus (n = 7); LCR: Lactobacillus casei rhamnosus probiotic (n = 1); LG: Lactobacillus gasseri (n = 1); LM: Lactobacillus mucosae (n = 4); LV: Lactobacillus vaginalis (n = 6); LJ: Lactobacillus jensenii (n = 5).
To validate these findings using an alternative experimental approach, cytokine responses to isolates adjusted to optical densities at a wavelength of 600 nm (OD600) of 0.1 ± 0.01 were evaluated. It was found that the cytokine factor scores between assays (OD-adjusted bacteria versus 4.18 × 106 CFU of bacteria used for stimulation) were significantly associated [β-coefficient = 0.396, 95% confidence interval (CI): 0.036–0.756, p = 0.032], particularly after adjustment for bacterial length (β-coefficient = 0.462, 95% CI: 0.088–0.835, p = 0.017), which influences the OD of cultures.
To evaluate the impact of lactobacilli on cytokine responses elicited by pathogenic, BV-associated bacteria, we pre-incubated CaSki cells with six Lactobacillus isolates [2 L. jensenii (LJ2 and 5), 1 L. crispatus (LC2), 1 L. mucosae (LM2), 1 L. vaginalis (LV6) and 1 L. gasseri (LG1)] before adding G. vaginalis ATCC 14018 and incubating the cultures for a further 20 hours. When comparing the concentrations of the four inflammatory cytokines assessed (IL-1α, IL-6, IL-8, IP-10) and anti-inflammatory IL-1 receptor antagonist (RA), it was found that 5/6 of the lactobacilli reduced inflammatory responses to G. vaginalis (Fig. 5). Using Student’s t test to compare log10-transformed cytokine concentrations, it was found that IL-6 concentrations were significantly lower following pre-incubation with LC2 (p = 0.0085, adjusted p = 0.0425), LV6 (p = 0.0091, adjusted p = 0.02275), LM2 (p = 0.0124; adjusted p = 0.0207), LG1 (p = 0.0179; adjusted p = 0.0224) and LJ2 (p = 0.0306; adjusted p = 0.0306), while pre-incubation with LJ5 significantly increased cytokine production relative to incubation with G. vaginalis alone (p = 0.0191; adjusted p = 0.0191). LC2 also significantly reduced IL-1α, IL-8 and IL-1RA production, while LJ2 reduced IL-8 and LG1 and LV6 reduced production of IL-1RA relative to G. vaginalis alone, although these changes were not significant after adjusting for multiple comparisons (p = 0.0337, p = 0.0196, p = 0.0312, p = 0.0124, p = 0.0217 and p = 0.0190, respectively).
Lactobacilli-mediated changes in inflammatory cytokine production by CaSki cells in response to Gardnerella vaginalis. Cytokine production by CaSki cells in response to G. vaginalis alone and G. vaginalis following pre-incubation with lactobacilli. CaSki monolayers in 24 well plates were incubated with lactobacilli for 5 hours at 37 °C under 5% CO2. G. vaginalis was then added to the cultures and incubated as above for a further 20 hours. Cytokine concentrations were measured using Luminex. Unsupervised hierarchical clustering was used to group the co-cultures according to inflammatory responses induced. Inflammatory cytokine concentrations are shown as a heat map, with blue, through white, to red indicating low-high cytokine concentrations, respectively. Data was log10-transformed and scaled in R. Two clustering dendrograms are shown in the figure. The dendrogram above the heat map illustrates degrees of relatedness between different cytokines measured. The dendrogram on the left hand side of the heat map indicates relationships between the expression profiles of the analysed cytokines in response to different clinical Lactobacillus isolates. GV: G. vaginalis; LC: L. crispatus, LJ: L. jensenii; LM: L. mucosae; LG: L. gasseri; LV: L. vaginalis.
Inhibition of G. vaginalis growth
The six Lactobacillus isolates above were selected for G. vaginalis inhibition assays, including 2 L. jensenii (LJ2 and 5), 1 L. crispatus (LC2), 1 L. mucosae (LM2), 1 L. vaginalis (LV6) and 1 L. gasseri (LG1) strains. It was found that 4/6 isolates significantly inhibited G. vaginalis growth (Fig. 6A) and viability (Fig. 6B). The culture pH levels of the isolates that inhibited G. vaginalis growth and viability, LJ2, LJ5, LM2 and LG1, were significantly lower than those of the isolates that were not inhibitory, LC2 and LV6 [mean: 4.551 (range: 4.398–4.826) versus 5.478 (range: 5.283–5.673), respectively; p = 0.0082]. D-lactate, L-lactate and lactic acid levels did not differ significantly between the groups (p = 0.0703, p = 0.2711 and p = 0.0690, respectively), although the sample size was small and the differences in D-lactate and lactic acid concentrations approached significance. Furthermore, reduction of H2O2 and degradation of bacteriocins using proteolytic enzymes did not influence the inhibitory activities of LJ2, LM2 and LG1 (Fig. 6C,D), suggesting that culture medium acidification was the primary mechanism for G. vaginalis inhibition in these assays.
Inhibition of Gardnerella vaginalis growth by Lactobacillus culture supernatants. (A) Growth of G. vaginalis was determined by measuring the optical density of cultures at a wavelength of 600 nm (OD600), after culture with lactobacilli supernatants in duplicate within the same assay for 24 h at 37 °C. The fold change in growth of G. vaginalis only cultures was compared to those cultured with lactobacilli supernatants using an unpaired two-tailed t-test. (B) Colony forming units (CFU)/ml of G. vaginalis pretreated with lactobacilli supernatants on brain heart infusion (BHI) agar after incubation for 48 h at 37 °C were assessed in duplicate within the same assay. (C,D) Lactobacillus jensenii (LJ)5, L. mucosae (LM)2 and L. gasseri (LG)1 were used to determine the mechanism underlying the inhibition of G. vaginalis by lactobacilli supernatant in triplicate within the same assay. (C) The effects of hydrogen peroxide reduction by catalase and (D) bacteriocin degradation by proteolytic enzymes in Lactobacillus culture supernatants on the growth of G. vaginalis. Lines indicate means and error bars indicate the standard deviations of technical replicates. Student’s t-tests were used for comparisons. **Adjusted p-values < 0.05 were considered statistically significant. CFU: colony forming units, LC: L. crispatus, LV: L. vaginalis, Cat: catalase, Enz = proteolytic enzymes.
Overall probiotic-relevant performance of isolates
A scoring system was devised to compare and rank the isolates based on all of the characteristics investigated. Each isolate was given scores out of a maximum score of three per characteristic, according to (1) growth rates; (2) culture pH acidification; the levels of (3) H2O2, (4) L- and (5) D-lactate produced, (6) ability to adhere to epithelial cells and (7) induction of inflammatory responses by CaSki cells (Table 2). Relative scores per category were assigned as follows: <25th percentile (score = 0); 25th−50th percentile (score = 1); 50th-75th percentile score = 2); ≥75th (score = 3). Lower pH levels and lower levels of inflammation were considered advantageous, so isolates were scored as follows: <25th percentile (score = 3); 25th-50th percentile (score = 2); 50th-75th percentile score = 1); ≥75th (score = 0). The L. jensenii strain (LJ5) ranked highest with a score of 18/21, higher than the probiotic isolates (L. acidophilus and L. casei rhamnosus). Interestingly, the top 10 isolates included 4 L. jensenii, 2 L. crispatus, 1 L. mucosae, and 1 L. vaginalis strain and the L. acidophilus probiotic isolates. The commercial vaginal probiotics were ranked 6th (LA capsule; 13/21), 10th (LA tablet; 12/21) and 20th (LCR; 9/21). The performance of the LA strains was inconsistent between tablets and capsules, while both grew rapidly and lowered the culture pH levels effectively, both induced inflammatory responses and the capsule LA isolate was poorly adherent to epithelial cells, while the tablet LA isolate produced very little H2O2 and L-lactate. The LCR probiotic strain fared worse with poor adhesion to epithelial cells and low H2O2, L- and D-lactate production in comparison to clinical isolates. Similar rankings were obtained if H2O2 was omitted, with the top 10 containing 3 L. jensenii, 2 L. crispatus, 1 L. mucosae, 2 L. vaginalis, and the 2 L. acidophilus probiotic isolates.
Discussion
BV, an imbalance in vaginal microbiota that predisposes women to HIV infection and reproductive complications, remains prevalent, in part because standard-of-care antibiotic therapy is largely ineffective14,32. Adjunctive probiotic treatment for BV may promote vaginal recolonization with healthy lactobacilli, however BV treatment outcomes have been heterogeneous in probiotic clinical trials. Here, we show that the performance of the only vaginal probiotics available on the South African market were highly varied based on the criteria evaluated in this study, providing a possible explanation for the heterogeneous efficacy of probiotic treatment in BV. Neither L. acidophilus nor L. casei rhamnosus species predominate in the FGTs of women with healthy microbiota27 and were not isolated from the cohort of women included in this study, suggesting that these species might not be ideal for treatment of BV in South African women. In this study, we evaluated Lactobacillus species that have been associated with vaginal health, including L. crispatus, L. gasseri, L. jensenii, L. mucosae and L. vaginalis. L. iners was not included as this species is associated with increased risk of conversion from a healthy to a dysbiotic vaginal microbiome33, and acquisition of STIs34. We found that several of the clinical isolates performed better than the probiotic strains, demonstrating the potential to improve existing probiotic formulations and treatment outcomes using novel clinical isolates. We also found that, although some Lactobacillus isolates induced inflammatory responses when cultured with ectocervical epithelial cells in isolation, when we pre-incubated the cells with a subset of six isolates prior to addition of G. vaginalis, 5/6 of the lactobacilli significantly reduced pro-inflammatory cytokine responses to G. vaginalis.
Several antimicrobial and other characteristics that are thought to be important for effective probiotic activity were evaluated for each Lactobacillus isolate16,18,20. Adhesion, thought to be mediated by specialized pili35, is an essential probiotic property as it enables the bacteria to persist in the FGT36. In this study, there were no significant differences in the level of adhesion between species. Larger bacterial size has been linked to superior adhesion capabilities30, however the relative length of bacteria in this study did not correlate significantly with adhesion. Moreover, although it has been reported that rapid bacterial multiplication leads to a high adhesion capacity30, in the present study, bacterial growth rates were not significantly associated with adhesion. H2O2 production differed between species, with L. mucosae isolates producing the most H2O2, followed by L. jensenii isolates, while the others produced minimal H2O2. The importance of H2O2 in protection against pathogens in the FGT is controversial. Earlier clinical studies found that women with H2O2-producing lactobacilli were at reduced risk of dysbiosis8,18,37. However, it has since been found that, under hypoxic conditions like those found in the vagina, lactobacilli produce very little H2O238 and H2O2 may not be microbicidal at physiological concentrations19,39. Furthermore, at microbicidal concentrations H2O2 inactivated lactobacilli more effectively than BV-associated bacteria in vitro19,39. It is important to note that, using an in vitro model to evaluate the characteristics of Lactobacillus isolates has limitations as this environment does not perfectly mimic in vivo conditions.
In contrast, lactic acid at physiological concentrations was shown to be microbicidal against pathogenic BV-associated bacteria (including G. vaginalis, P. bivia and P. corporis), but not vaginal lactobacilli16,17,19,39. Physiological concentrations of lactic acid have also been shown to have broad-spectrum virucidal activity against HIV that is dramatically more rapid and potent than media acidified to the same pH with HCl or acetic acid15,40. Interestingly, all isolates in this study produced D-lactate with no significant differences between species. However, L-lactate production was highly varied, with L. jensenii isolates producing the most L-lactate in both MRS under anaerobic conditions and in DMEM under aerobic conditions overall. The relative importance of L-lactic acid versus D-lactic acid is also controversial. L-lactic acid was found to be 17-fold more potent than D-lactic acid in inactivating HIVBaL in vitro15,40. However, D-lactic acid was found to have a greater inhibitory effect on C. trachomatis infectivity than L-lactic acid, which was partly41 or entirely39 pH-dependant.
Similar to the finding that lactic acid concentrations correlate inversely with pH in the FGTs of women with Lactobacillus-dominated microbiota31, we found that lactic acid concentrations correlated significantly with culture pH. As found in the present study, a previous study showed that the vaginal acidity achieved by L. crispatus was the highest compared to L. jensenii and L. gasseri27. Interestingly, in the present study, the L. casei rhamnosus probiotic isolate was associated with the lowest culture pH, followed by L. acidophilus probiotic.
We measured inflammatory responses to lactobacilli, as genital inflammation has been found to increase risk of HIV acquisition in women21 and it is thus essential that probiotics induce little or no inflammation. Most of the isolates in isolation induced low levels of cytokine production by CaSki cells following a 24 h incubation period. However we also found that most of the lactobacilli evaluated were able to significantly suppress inflammatory cytokine production by CaSki cells in response to the BV-associated pathogen, G. vaginalis. In vivo, in the same cohort from whom the lactobacilli were isolated, we found that endogenous L. reuteri, L. gasseri, L. crispatus and L. jensenii were all significantly associated with low inflammation in the FGT42. Other studies have reported that lactobacilli and lactic acid suppress inflammatory responses to pathogens and pattern recognition receptor ligands in vitro22,26. It is interesting that, in this study, some of the lactobacilli in isolation were able to induce increases in pro-inflammatory cytokine production and 1/6 of the lactobacilli included in the G. vaginalis co-culture experiment had an additive effect on cytokine induction. Additionally, anti-inflammatory IL-10 production was not detected in these cultures and IL-1RA production was suppressed by lactobacilli. Another study showed that, while L. rhamnosus and L. reuteri suppressed the expression of certain inflammatory mediators by vaginal epithelial cells in response to Candida albicans [including nuclear factor-kappa B inhibitor kinase alpha, toll-like receptor (TLR)-2, TLR-6, IL-8, and TNF-α], the lactobacilli also induced expression of pro-inflammatory cytokines IL-1α and IL-1β43. The authors suggested that the lactobacilli may suppress inflammatory responses induced by the NF-κB signal transduction pathway, but induce other inflammatory responses via an alternate signal pathway, such as the mitogen activated protein kinase and activator protein-1 (MAPK/AP-1) signal transduction pathway43. Similarly Rose et al. (2012) found that lactobacilli induced non-significant increases in the production of some inflammatory cytokines by vaginal epithelial cells cultured in transwell culture systems44. Proteins present in the peptidoglycan layer of the Lactobacillus cell wall and lipoteichoic acids present in the cell membrane may have inflammatory properties and the inflammatory nature of particular Lactobacillus strains has been found to be partly dependent on the structure of the peptidoglycan and the presence of exopolysaccharides which prevent the interaction of these TLR agonists with pattern recognition receptors45. Therefore it is not surprising that some isolates are capable of inducing inflammatory responses. Lactic acid itself was found to have direct pro-inflammatory effects on immune and vaginal epithelial cells in some studies46,47, but anti-inflammatory effects in others22. In this study, we found that neither D-lactate nor L-lactate production correlated with cytokine production by CaSki cells in response to the lactobacilli isolates. In addition to influencing inflammatory pathways directly, lactobacilli may alter inflammatory responses to pathogens by means of competitive exclusion, preventing pathogens from interacting with vaginal epithelial cells20,30. Interestingly, although the lactic acid concentrations measured in these cultures were lower than those present in FGT secretions31, we still observed suppression of pro-inflammatory responses to G. vaginalis and inhibition of G. vaginalis growth by Lactobacillus isolates and culture supernatants, respectively. Inflammatory cytokine induction by some of the lactobacilli demonstrates the need to evaluate inflammatory profiles of bacterial isolates being considered for vaginal probiotic therapy. A limitation of this study is that an ectocervical cancer cell line was used to evaluate lactobacilli adhesion and inflammatory properties to allow for high-throughput screening. However, the inflammatory properties of these cells may differ from healthy cells and it will thus be important to confirm that probiotic candidates do not induce inflammatory responses using other models.
Interestingly, the characteristics of the Lactobacillus isolates from South African women investigated in this study differed in some respects to the characteristics of isolates from other geographical regions and women of different ethnicities27,28. While studies in other regions, including America and Spain37,48, have found that L. crispatus strains produce high levels of H2O2 and lactic acid, this study found that these South African L. crispatus isolates generally produced relatively little of these antimicrobials. Similarly, major geographical and ethnic differences in the vaginal microbiome have been noted. African women were found to have a low abundance of Lactobacillus that was not associated with sexual behavior, contraceptive usage, or demographic characteristics4.
A lower frequency of L. crispatus and L. jensenii has been observed in black and Hispanic women compared to white and Asian women in the United States, suggesting that host genetic or dietary factors may play a role in bacterial colonization of the FGT5,27,49. However it is also possible that the characteristics of the predominant Lactobacillus strains present in certain populations influence the species distribution.
According to the characteristics that were assessed in this study that may influence Lactobacillus antimicrobial activity (including growth rates, culture pH, adhesion, H2O2, lactic acid and inflammatory responses), several South African clinical isolates performed better than the commercial probiotic Lactobacillus isolates evaluated. Of the top ten Lactobacillus isolates, L. jensenii and L. crispatus were well represented, while L. mucosae and L. vaginalis strains were mostly absent. Five clinical isolates performed better than the probiotic L. acidophilus strain, suggesting that there is indeed potential to improve existing probiotics that may, in turn, improve BV treatment outcomes.
Methods
Study participants
A cohort of 149 young women (16–22 years old) was recruited as part of the Women’s Initiative in Sexual Health (WISH) study in Cape Town29. Demographic data was collected and lateral wall and vulvovaginal swabs were obtained for testing of STIs (C. trachomatis, N. gonorrhoeae, T. vaginalis, M. genitalium, HSV-1, HSV-2 and T. pallidum) by PCR, and candidiasis and BV by Gram stain. This study was approved by the University of Cape Town Human Research Ethics Committee and all methods were performed in accordance with the relevant guidelines and regulations. Women older than 18 years old provided written informed consent, while those 16–17 years provided assent and written informed consent was obtained from their parents or legal guardians.
Bacterial isolation and culture
Cervicovaginal fluid was collected in menstrual cups (Softcup®, Evofem Inc, USA), diluted in phosphate buffered saline (PBS) and frozen in 20% glycerol at −80 °C. Cervicovaginal fluid was thawed and cultured in sterile de Man, Rogosa, Sharpe (MRS) broth anaerobically for 48 h at 37 °C, streaked on MRS-agar and incubated anaerobically at 37 °C for 48 h. Morphologically distinct single colonies were picked and inoculated in MRS broth and incubated anaerobically at 37 °C for 72 h. Bacterial isolates (n = 50) were cultured from 20 participants and identified using MALDI biotyping (Bruker Daltonik, USA). From these, 23 isolates from 9 women were identified as Lactobacillus species and were included. Microscopy was used to measure the length of 5 bacteria per isolate (Leica ICC50 HD, Leica Microsystems, Germany). Growth rates were evaluated by inoculating MRS broth with 4.18 × 106 CFU47 of each isolate in triplicate and measuring the OD600 of cultures over time. The area under the curve (AUC) was calculated for each isolate between 0 and 12 h, after which stationary phase was reached.
Bacterial adhesion to genital epithelial cells
The ability of the lactobacilli to adhere to human ectocervical epithelial cells, CaSki (CRL-1550, ATCC, USA), was evaluated as described previously50. CaSki cells were grown to 80% confluency in complete cell culture medium [Dulbecco’s Modified Eagle’s Medium (DMEM) with L-Glutamine (Lonza, Switzerland), 10% fetal calf serum (Capricorn-Scientific, Germany) and 1% penicillin (50U/ml) and streptomycin (50U/ml; Sigma-Aldrich, USA)] in 24 well plates and then washed with PBS. Bacteria adjusted to OD600 of 0.1 ± 0.01 in antibiotic-free cell culture medium were added and incubated for 2 h at 37 °CC, 5% CO2. Culture medium was removed and plates were washed 3 times with PBS to remove unbound bacteria. 0.1% TritonX-100 (Sigma-Aldrich, USA) was added and the monolayers were lifted with cell scrapers. Serial dilutions were plated on MRS agar and colonies were counted following anaerobic incubation at 37 °C for 48 h. CFU/ml was calculated and expressed as a percentage of the baseline CFU/ml added to each monolayer. This experiment was repeated three times.
For visual confirmation of bacterial adhesion to CaSki cells, bacteria were added to cell monolayers in NuncTM Lab-TekTM II Chamber Slides (Thermo Fisher Scientific Inc., USA) and incubated for 2 h at 37 °C, 5% CO2. Cell culture medium was removed and wells were washed 3 times with PBS. Chambers were removed before each slide was heat-fixed and Gram-stained. Representative images were captured (Leica ICC50 HD, Leica Microsystems, Germany).
Hydrogen peroxide production
H2O2 production was evaluated in aerobic cultures in order to assess the maximal H2O2 production capacity of the isolates. Cultures were incubated aerobically with agitation at 170 rpm for 3 h at 37 °C. Aliquots were collected hourly for 3 h, centrifuged and the supernatants stored at −80 °C. pH levels of the cultures were measured using a pH meter (Jenway Bench pH Meter 2510, Bibby Scientific, UK). Measurement of Lactobacillus H2O2 concentrations was performed using a tetramethylbenzidine assay in duplicate as described previously51.
Inflammatory cytokine responses to lactobacilli
CaSki monolayers were grown to near confluence in 24 well plates. Culture medium was removed and 4.18 × 106 CFU of each bacterial species or OD600 of 0.1 ± 0.01 adjusted bacteria were added to the cells in antibiotic-free cell culture medium (DMEM with L-Glutamine, 10% fetal calf serum) and incubated aerobically at 37 °C for 24 h under 5% CO2. Culture supernatants were removed, centrifuged at 6000xg and stored at −80 °C. CaSki cell viability in these co-cultures was confirmed using an MTT assay (Roche Diagnostics, Germany). In order to account for the impact of cleavage of the yellow tetrazolium salt MTT to purple formazan crystals by metabolically active lactobacilli, lactobacilli-only cultures incubated in antibiotic-free cell culture medium under aerobic conditions were included as controls. In all cases, the metabolic activity of the CaSki cells in co-culture with the lactobacilli was either comparable to or higher than the CaSki cells-only controls. A Magnetic Luminex Screening Assay kit (R&D Systems, Minneapolis, USA) was used to measure the concentrations of 13 cytokines (TNF-α, IL-1α, IL-1β, IL-6, IL-17A, IFN-γ, RANTES, IL-8, IP-10, MIP-3α, MIP-1α and MIP-1β, IL-10). To evaluate whether cytokine responses to G. vaginalis were modulated by Lactobacillus isolates, CaSki cells were pre-incubated with 4.18 × 106 CFU of six Lactobacillus isolates [2 L. jensenii (LJ2 and 5), 1 L. crispatus (LC2), 1 L. mucosae (LM2), 1 L. vaginalis (LV6) and 1 L. gasseri (LG1) strains] for 5 hours under the same conditions as described above. G. vaginalis ATCC 14018 (4.18 × 107 CFU) was then added to each well and cultures were incubated for a further 20 hours. Supernatants were collected and processed as above and a Magnetic Luminex Screening Assay kit (R&D Systems, Minneapolis, USA) was then used to measure IL-1α, IL-6, IL-8, IP-10 and IL-1RA concentrations. Data was collected using a Bio-PlexTM Suspension Array Reader and a 5 parameter logistic regression was used to calculate cytokine concentrations from the standard curves using BIO-plex manager software (version 4; Bio-Rad Laboratories Inc®, USA). Cytokine concentrations below the detectable limit were assigned the value of half the lowest recorded concentration of that cytokine.
D- and L-lactic acid production
Following a 24 h incubation period at 37 °C under anaerobic conditions, 4.18 × 106 CFU of each isolate was added to 15 ml MRS broth and incubated for an additional 24 h at 37 °C under anaerobic conditions. Supernatants were collected and D-and L-lactate concentrations were measured in duplicate using D-Lactate Colorimetric and Lactate Assay kits according to the manufacturer’s instructions (Sigma-Aldrich, USA). Both D- and L-lactate concentrations were also measured in lactobacilli-CaSki cell co-cultures following aerobic incubation at 37 °C for 24 h under 5% CO2 using D-Lactate Colorimetric and Lactate Assay kits according to the manufacturer’s instructions (Sigma-Aldrich, USA).
G. vaginalis inhibition assay
Six Lactobacillus isolates [2 L. jensenii (LJ2 and 5), 1 L. mucosae (LM2), 1 L. crispatus (LC2), 1 L. gasseri (LG1), 1 L. vaginalis, (LV6)] were cultured in MRS for 24 h under anaerobic conditions. Cultures were standardized to 4.18 × 106 CFU/ml in MRS and incubated for an additional 20 h at 37 °C under anaerobic conditions, after which they were filtered using 0.2 μm cellulose acetate filters (Sigma-Aldrich, USA). Following 48 h incubation in brain heart infusion (BHI) broth at 37 °C under anaerobic conditions, G. vaginalis was standardized to 1 × 108 CFU/ml and cultured with each lactobacilli cell-free supernatant anaerobically for 24 h at 37 °C. Absorbance at OD600 was measured at baseline and 24 h after incubation. Following the 24 h incubation, G. vaginalis cultures were plated on BHI agar and incubated for 24 h at 37 °C under anaerobic conditions, after which CFUs were counted12.
Effect of hydrogen peroxide and bacteriocins on G. vaginalis inhibition
Three Lactobacillus isolates (LJ2, LM2 and LG1), that were found to inhibit G. vaginalis growth, were standardized to 4.18 × 106 CFU/ml and cultured in MRS broth for 20 h at 37 °C under anaerobic conditions. To abrogate the possible effect of H2O2 and bacteriocins, lactobacilli cell-free supernatants and MRS were pre-treated for 1 h at 37 °C with catalase (100 µg/ml) or proteolytic enzymes [trypsin (200 µg/ml), pepsin (200 µg/ml), pronase (200 µg/ml) and proteinase K (100 µg/ml)]. Pre-treated lactobacilli cell-free supernatants, pre-treated MRS and untreated MRS were then added 1 × 108 CFU/ml of G. vaginalis. Absorbance at OD600 was measured at baseline, 24 and 48 h after incubation at 37 °C under anaerobic conditions12.
Statistical Analysis
GraphPad Prism 5® (GraphPad Software, USA), STATA version 11.0 (StataCorp, USA), and R were used for statistical analyses. Mann Whitney U and Student’s t-tests were used for unpaired comparisons of non-parametric and parametric data, respectively; Spearman Rank test was used for non-parametric correlations. A false-discovery rate (FDR) step-down procedure was used to adjust p-values for multiple comparisons and adjusted p-values < 0.05 were considered statistically significant. Unsupervised hierarchical clustering was used to evaluate the relationship between lactobacilli and cytokine profiles. To compare overall inflammatory cytokine responses, confirmatory factor analysis was used to generate inflammatory factor scores, which are linear combinations of the concentrations of each inflammatory cytokine (IL-1α, IL-1β, IL-6, IL-8, IP-10, MIP-1α, MIP-1β, MIP-3α, RANTES) in the factor, weighted according to their factor loadings.
Ethics approval and consent to participate
The parent study was approved by the University of Cape Town (UCT) human research ethics committee (UCT HREC: 267/2013). The microbiological sub-study was approved by the UCT human research ethics committee (UCT HREC: 551/2016). Women older than 18 years provided written informed consent, while those who were 16–17 years old provided assent and written informed consent was obtained from their parents or legal guardians.
Data Availability
The datasets used and/or analysed during this study are available from the corresponding author on reasonable request.
References
Forsum, U. et al. Bacterial vaginosis - A microbiological and immunological enigma. Apmis. 113, 81–90 (2005).
Cohen, C. R. et al. Bacterial Vaginosis associated with increased risk of female-to-male HIV-1 transmission: A prospective cohort analysis among African couples. PLoS Med. 9, 1–9 (2012).
Taha, T. E. et al. Bacterial vaginosis and disturbances of vaginal flora: association with increased acquisition of HIV. AIDS. 13, 1699–706 (1998).
Gosmann, C. et al. Lactobacillus-deficient cervicovaginal bacterial communities are associated with increased HIV acquisition in young South African women. Immunity. 46, 29–37 (2017).
Williams, B., Landay, A. & Presti, R. M. Microbiome alterations in HIV infection a review. Cell. Microbiol. 18, 645–51 (2016).
Klatt, N. R. et al. Vaginal bacteria modify HIV tenofovir microbicide efficacy in African women. Science. 356, 938–45 (2017).
Wiesenfeld, H. C., Hillier, S. L., Krohn, M. A., Landers, D. V. & Sweet, R. L. Bacterial vaginosis is a strong predictor of Neisseria gonorrhoeae and Chlamydia trachomatis infection. Clin Infect Dis. 36, 663–8 (2003).
Witkin, S. S. The vaginal microbiome, vaginal anti‐microbial defence mechanisms and the clinical challenge of reducing infection‐related preterm birth. BJOG: Int J Obstet Gynaecol. 122, 213–8 (2015).
Anahtar, M. N. et al. Cervicovaginal Bacteria are a major modulator of host inflammatory responses in the female genital tract. Immunity. 42, 965–76 (2015).
STATS SA. Statistical release: Mid-year Population Estimates. Stats Sa. 2017. http://www.statssa.gov.za/publications/P0302/P03022017.pdf. Acessed 11Dec 2017.
Masson, L. et al. Defining genital tract cytokine signatures of sexually transmitted infections and bacterial vaginosis in women at high risk of HIV infection: a cross-sectional study. Sex. Transm. Infect. 90, 580–7 (2014).
Atassi, F., Brassart, D., Grob, P., Graf, F. & Servin, A. L. Lactobacillus strains isolated from the vaginal microbiota of healthy women inhibit Prevotella bivia and Gardnerella vaginalis in coculture and cell culture. FEMS Immunol. Med. Microbiol. 48, 424–432 (2006).
Tyssen, D. et al. Anti-HIV-1 Activity of Lactic Acid in Human Cervicovaginal Fluid. mSphere. 3(4) (2018).
Barrons, R. & Tassone, D. Use of Lactobacillus probiotics for bacterial genitourinary infections in women: A review. Clin. Ther. 30, 453–68 (2008).
Aldunate, M. et al. Vaginal concentrations of lactic acid potently inactivate HIV. J. Antimicrob. Chemother. 68, 2015–25 (2013).
Nardini, P. et al. Lactobacillus crispatus inhibits the infectivity of Chlamydia trachomatis elementary bodies, in vitro study. Sci. Rep. 6, 29024 (2016).
Valore, E. V., Park, C. H., Igreti, S. L. & Ganz, T. Antimicrobial components of vaginal fluid. Am. J. Obstet. Gynecol. 187, 561–8 (2002).
Klebanoff, S. J. & Coombs, R. W. Viricidal effect of Lactobacillus acidophilus on human immunodeficiency virus type 1: possible role in heterosexual transmission. J. Exp. Med. 174, 289–92 (1991).
O’Hanlon, D. E., Moench, T. R. & Cone, R. A. In vaginal fluid, bacteria associated with bacterial vaginosis can be suppressed with lactic acid but not hydrogen peroxide. BMC Infect. Dis. 11, 200 (2011).
Chan, R. C. Y., Reid, G., Irvin, R. T., Bruce, A. & Costerton, J. W. Competitive exclusion of uropathogens from human uroepithelial cells by Lactobacillus whole cells and cell wall fragments. Infect. Immun. 47, 84–9 (1985).
Masson, L. et al. Genital nflammation and the risk of HIV acquisition in women. Clin. Infect. Dis. 61, 260–9 (2015).
Hearps, A. C. et al. Vaginal lactic acid elicits an anti-inflammatory response from human cervicovaginal epithelial cells and inhibits production of pro-inflammatory mediators associated with HIV acquisition. Mucosal Immunol. 10, 1480–90 (2017).
Workowski, K.A. & Bolan, G.A. Sexually Transmitted Diseases Treatment Guidelines. Morb. Mortal. Wkly. Rep. 2015.
Huang, H., Song, L. & Zhao, W. Effects of probiotics for the treatment of bacterial vaginosis in adult women: A meta-analysis of randomized clinical trials. Arch. Gynecol. Obstet. 289, 1225–34 (2014).
Senok, A. C., Verstraelen, H., Temmerman, M., Botta, G. Probiotics for the treatment of bacterial vaginosis. Cochrane database Syst. Rev. https://doi.org/10.1002/14651858.CD006289 (2009)
Tachedjian, G., Aldunate, M., Bradshaw, C.S., Cone, R.A. The role of lactic acid production by probiotic Lactobacillus species in vaginal health. Res. Microbiol. 1–11 (2017).
Ravel, J. et al. Vaginal microbiome of reproductive-age women. Proc. Natl. Acad. Sci. USA 108, Suppl, 4680–7 (2011).
Petrova, M. I., van den Broek, M., Balzarini, J., Vanderleyden, J. & Lebeer, S. Vaginal microbiota and its role in HIV transmission and infection. FEMS Microbiol. Rev. 37, 762–92 (2013).
Barnabas, S., et al. Converging epidemics of sexually transmitted infections and bacterial vaginosis in Southern African female adolescents at risk of HIV. Int. J. STD AIDS. https://doi.org/10.1177/0956462417740487 (2018)
Mastromarino, P. et al. Characterization and selection of vaginal Lactobacillus strains for the preparation of vaginal tablets. J. Appl. Microbiol. 93, 884–93 (2002).
O’Hanlon, D. E., Moench, T. R. & Cone, R. A. Vaginal pH and microbicidal lactic acid when lactobacilli dominate the microbiota. PLoS One. 8, 1–9 (2013).
Bradshaw, C. S. et al. High recurrence rates of bacterial vaginosis over the course of 12 months after oral metronidazole therapy and factors associated with recurrence. J. Infect. Dis. 193, 1478–86 (2006).
Verstraelen, H. et al. Longitudinal analysis of the vaginal microflora in pregnancy suggests that L. crispatus promotes the stability of the normal vaginal microflora and that L. gasseri and/or L. iners are more conducive to the occurrence of abnormal vaginal microflora. BMC Microbiol. 9, 116 (2009).
van Houdt, R. et al. Lactobacillus iners-dominated vaginal microbiota is associated with increased susceptibility to Chlamydia trachomatis infection in Dutch women: a case–control study. Sex Transm Infect. 94(2), pp. 117–123 (2018).
Danielsson, D., Teigen, P. K. & Moi, H. The genital econiche: Focus on microbiota and bacterial vaginosis. Ann. N. Y. Acad. Sci. 1230, 48–58 (2011).
Boris, S., Suárez, J. E., Vázquez, F. & Barbés, C. Adherence of human vaginal lactobacilli to vaginal epithelial cells and interaction with uropathogens. Infect. Immun. 66, 1985–9 (1998).
Klebanoff, S. J., Hillier, S. L., Eschenbaeh, D. A. & Waltersdorph, A. M. Control of the Microbial Flora of the Vagina by H2O2-Generating Lactobacilli. J. Infect. Dis. 164, 94–100 (1991).
Ocaña, V. S., P D Ruiz Holgado, A. A. & Nader-Macías, M. E. Selection of vaginal H2O2-generating Lactobacillus species for probiotic use. Curr. Microbiol. 38, 279–84 (1999).
Gong, Z., Luna, Y., Yu, P. & Fan, H. Lactobacilli Inactivate Chlamydia trachomatis through Lactic Acid but Not H2O2. PLoS One. 9, 1–12 (2014).
Aldunate, M. et al. Antimicrobial and immune modulatory effects of lactic acid and short chain fatty acids produced by vaginal microbiota associated with eubiosis and bacterial vaginosis. Front. Physiol. 6, 1–23 (2015).
Edwards, V. et al. Lactic acid isomers differentially reduce Chlamydia Trachomatis infection in a pH dependent manner. Sex Transm Dis. 91(Suppl 2), A1–258 (2015).
Lennard, K., et al. Microbial composition predicts genital tract inflammation and persistent bacterial vaginosis in adolescent South African women. Infect. Immun. https://doi.org/10.1128/IAI.00410-17 (2017).
Wagner, R. & Johnson, S. J. Probiotic lactobacillus and estrogen effects on vaginal epithelial gene expression responses to Candida albicans. J. Biomed. Sci. 19, 58 (2012).
Rose, W. A. et al. Commensal Bacteria Modulate Innate Immune Responses of Vaginal Epithelial Cell Multilayer Cultures. PLoS ONE. 7(3) (2012).
Chapot-Chartier, M. & Kulakauskas, S. Cell wall structure and function in lactic acid bacteria. Microbial Cell Factories. 13(Suppl), S9 (2014).
Mossop, H., Linhares, I. M., Bongiovanni, A. M., Ledger, W. J. & Witkin, S. S. Influence of lactic acid on endogenous and viral RNA-induced immune mediator production by vaginal epithelial cells. Obstet. Gynecol. 118, 840–6 (2011).
Witkin, S. S., Alvi, S., Bongiovanni, A. M., Linhares, I. M. & Ledger, W. J. Lactic acid stimulates interleukin-23 production by peripheral blood mononuclear cells exposed to bacterial lipopolysaccharide. FEMS Immunol. Med. Microbiol. 61, 153–8 (2011).
Antonio, M. A. D., Rabe, L. K. & Hillier, S. L. Colonization of the rectum by Lactobacillus species and decreased risk of bacterial vaginosis. J. Infect. Dis. 192, 394–8 (2005).
Zhou, X. et al. Differences in the composition of vaginal microbial communities found in healthy Caucasian and black women. ISME J. 112, 121–33 (2007).
Coudeyras, S., Jugie, G., Vermerie, M., Forestier, C. Adhesion of human probiotic Lactobacillus rhamnosus to cervical and vaginal cells and interaction with vaginosis-associated pathogens. Infect. Dis. Obstet. Gynecol. https://doi.org/10.1155/2008/549640 (2008)
Martín, R. & Suárez, J. E. Biosynthesis and degradation of H2O2 by vaginal lactobacilli. Appl. Environ. Microbiol. 76, 400–5 (2010).
Acknowledgements
The authors would like to acknowledge the women enrolled in the WISH cohort, as well as the clinical study staff. This work was supported by a South African Medical Research Council (MRC) Self-Initiated Research grant. The cohort was supported by the European and Developing Countries Clinical Trials Partnership (EDCTP; http://www.edctp.org). L.M. was supported by the National Research Foundation (NRF) of South Africa (http://www.nrf.ac.za), the UCT Clinical Infectious Diseases Research Initiative/Wellcome Trust (http://www.cidri.uct.ac.za) and the Carnegie Corporation. M.T.M. was supported by the NRF, the Poliomyelitis Research Foundation and the Letten Foundation administered by B. Stray-Pedersen. A.G.A. was supported by the NRF.
Author information
Authors and Affiliations
Contributions
E.C., M.T.M. and A.G.A. generated the data, analyzed the data and prepared the manuscript; R.F. and H.G. processed clinical samples, conducted some of the laboratory work and contributed to manuscript preparation; H.J. assisted with the management of the WISH cohort, generated some of the data, and contributed to manuscript preparation; S.Z.J. and S.D. assisted with the management of the WISH cohort, processed clinical samples, and contributed to manuscript preparation; S.L.B. managed the WISH cohort, generated some of the data and contributed to manuscript preparation; A.U.H. analyzed the data and contributed to manuscript preparation; D.B. and L.D. conducted some of the laboratory work and contributed to manuscript preparation; J.A.S.P. was Principal Investigator of the WISH cohort, supervised the acquisition and analysis of the data and contributed to manuscript preparation; L.M. conceptualized the study, supervised the acquisition of the data, analysed the data, and wrote the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chetwin, E., Manhanzva, M.T., Abrahams, A.G. et al. Antimicrobial and inflammatory properties of South African clinical Lactobacillus isolates and vaginal probiotics. Sci Rep 9, 1917 (2019). https://doi.org/10.1038/s41598-018-38253-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-38253-4
This article is cited by
-
The right bug in the right place: opportunities for bacterial vaginosis treatment
npj Biofilms and Microbiomes (2022)
-
Immobilization Techniques on Bioprocesses: Current Applications Regarding Enzymes, Microorganisms, and Essential Oils
Food and Bioprocess Technology (2022)
-
Lactic acid from vaginal microbiota enhances cervicovaginal epithelial barrier integrity by promoting tight junction protein expression
Microbiome (2022)
-
Bacterial vaginosis and health-associated bacteria modulate the immunometabolic landscape in 3D model of human cervix
npj Biofilms and Microbiomes (2021)
-
Quantitative modeling predicts mechanistic links between pre-treatment microbiome composition and metronidazole efficacy in bacterial vaginosis
Nature Communications (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.