Abstract
Visceral adiposity is a major risk factor of cardiometabolic diseases. Visceral adipose tissue (VAT) is usually measured with expensive imaging techniques which present financial and practical challenges to population-based studies. We assessed whether cardiometabolic conditions were associated with VAT by using a new and easily measurable anthropometric index previously published and validated. Data (1529 participants) came from the European Health Examination Survey in Luxembourg (2013–2015). Logistic regressions were used to study associations between VAT and cardiometabolic conditions. We observed an increased risk of all conditions associated with VAT. The total adjusted odds ratio (AOR, [95% CI]) for hypertension, prediabetes/diabetes, hypercholesterolemia, and hypertriglyceridemia for the fourth quartile of VAT compared to the lowest were 10.22 [6.75, 15.47]), (5.90 [4.02, 8.67]), (3.60 [2.47, 5.25]) and (7.67 [5.04, 11.67]. We observed higher odds in women than in men for all outcomes with the exception of hypertension. Future studies should investigate the impact of VAT changes on cardiometabolic health and the use of anthropometrically predicted VAT as an accurate outcome when no biomedical imaging is available.
Similar content being viewed by others
Introduction
Over the past 20 years there has been a significant global increase in the prevalence of cardiovascular (CVD) and metabolic conditions such as hypertension, type 2 diabetes, hypercholesterolemia, hypertriglyceridemia and metabolic syndrome1,2,3,4. Despite downward trends in mortality rates due to CVD in high-income countries over the last decades, new evidence suggests a possible plateau in CVD mortality in recent years5. This has contributed to cardiovascular diseases being the leading cause of mortality and early morbidity worldwide5,6 with nearly 30% of global causes of death due to CVD diseases7.
An excess of visceral fat is linked to chronic diseases such as metabolic and cardiovascular conditions emphasizing the strong association between cardiometabolic health and excess of ectopic fat8. Adipose tissue is a complex organ with different roles on energy metabolism, endocrine function and inflammation9,10. A malfunction produced by an excess of adipose tissue is associated with metabolic disorders11. In particular, an excess of ectopic fat, located in the abdominal cavity surrounding the organs, also known as visceral adipose tissue (VAT), is considered a major risk factor for metabolic and cardiovascular diseases, independently of general adiposity9,12. VAT can be accurately measured through biomedical imaging techniques such as magnetic resonance imaging (MRI) and computed tomography-scan (CT-Scan)13. However, these techniques are expensive, limited to specialised medical use and show high exposures to radiation (e.g. CT-Scan)13, thus being ineffective for population-based studies. Due to those limitations, simple anthropometric measurement (e.g. waist circumference (WC), waist-to-hip circumference ratio) are used for the indirect assessment of visceral adiposity in both clinical and population-based studies14,15,16. Nevertheless, these measurements have the major limitation of not being able to differentiate between VAT and subcutaneous abdominal adipose tissue (SAAT). Recently, Samouda et al. suggested a more accurate anthropometric prediction of VAT by subtracting the most correlated anthropometric measurement with SAAT from an abdominal anthropometric measurement highly correlated with total abdominal adipose tissue and the most possible correlated with VAT17. Using this equation, VAT can be readily predicted by combining a small number of easy to measure anthropometric features (e.g. WC, proximal thigh circumference and body mass index (BMI)). The anthropometric predictive models of VAT developed by Samouda et al. in 2013, were validated by Brown et al. in 2017 and 2018. They observed that compared to BMI and WC, predicted models of VAT were the most accurate predictors of cardiometabolic conditions as well as all-cause and cause-specific mortality (e.g. CVD, cancer) in Europid descendants from the Third National Health and Nutrition Examination Survey, 1988–1994 (NHANES III), when biomedical imaging data are not available or feasible18,19.
Results from the European Health Examination Survey in Luxembourg (EHES-LUX) have shown that the prevalence of hypertension and obesity is high in the country, with one third of the population showing hypertension and obesity rates reaching 20%20,21. Despite having information on the health situation, up-to-date and exhaustive characterizations of the cardiometabolic health are still missing for the Luxembourgish population, particularly in regards to specific risk factors such as VAT accumulation.
The present study aims to assess whether anthropometrically predicted visceral adipose tissue was associated with hypertension, prediabetes and diabetes, as well as hypercholesterolemia and hypertriglyceridemia, after adjusting for socio-demographic and behavioural characteristics in a population-based study.
Results
Participants’ characteristics
Nearly half of participants were women (52%) (Supplementary Table S1). Differences were observed between men and women. Men were more likely to have higher BMI, WC, and anthropometrically predicted VAT while women had higher thigh circumference. Men were more likely to have higher systolic and diastolic blood pressure, LDL cholesterol, triglycerides and fasting plasma glucose levels. Men had almost twice as much hypertension (40.09%), combined prediabetes and diabetes (42.63%) and hypertriglyceridemia (40.17%) as in women (23.40%, 22.16% and 19.09% respectively). Women smoked and consumed alcoholic drinks less than men.
Cardiometabolic conditions by quartiles of VAT
The proportion of hypertension, combined prediabetes and diabetes, hypertriglyceridemia and metabolic syndrome increased with VAT quartiles in both men and women (Table 1). The largest prevalence gradient was observed for metabolic syndrome in both men (from 1.7% in the first quartile to 82.1% observed in the fourth quartile) and women (from 1.1% in the first quartile to 62.2% observed in the fourth quartile). The proportion of hypercholesterolemia increased with VAT in both men and women. We observed that median values of WC and thigh circumference increased with VAT, but when we visualized VAT for similar WC values (Supplementary Figure S1), we observed that thigh circumference decreased for both men and women. Similar results were observed in the prevalence of cardiometabolic conditions by quartiles of WC (Supplementary Table S2).
VAT association with all cardiometabolic conditions
Results from logistic regression analysis examining the association between anthropometrically predicted VAT and cardiometabolic conditions are presented in Table 2. We observed an increase in the odds of all metabolic and cardiovascular conditions associated with VAT in both men and women. The strength of the association was reduced but remained statistically significant after adjusting for socioeconomic status (education and employment status) (model 1), and lifestyle (model 2). The association observed was strongest in men for hypertension: adjusted OR [95% CI] for men were 2.51 [1.46, 4.29], 4.08 [2.40, 6.93], and 11.83 [6.82, 20.49] for the second, third and fourth quartile of VAT. For women, the values were 1.93 [0.92, 4.00], 3.41 [1.69, 6.85], and 8.21 [4.12, 16.36] for the second, third and fourth quartile of VAT. Nevertheless, women observed a strongest association for combined prediabetes and diabetes 7.57 [3.93, 14.59] for the fourth quartile of VAT in women compared to 5.41 [3.26, 8.97 in men), hypercholesterolemia (5.28 [3.09, 9.00] for the fourth quartile of VAT in women compared to 2.26 [1.33, 3.84] in men) and hypertriglyceridemia (14.62 [6.30, 33.90] for the fourth quartile of VAT in women compared to 6.78 [3.97, 11.56] in men.
Discussion
The present study highlighted an increase of all metabolic and cardiovascular conditions associated with anthropometrically predicted VAT in adults aged 25–64. The association observed was independent of socioeconomic status and lifestyles. Our findings confirm that VAT is a major independent predictor risk factor of cardiometabolic risk as observed in previous epidemiological studies22. This can be explained by the high metabolic activity of VAT and its pro-inflammatory activity (production of cytokines with inflammatory effects and blocking of those anti-inflammatory)23,24. Moreover, compared to other fat deposits, VAT has larger and dysfunctional adipocytes, which are less insulin sensitive and with increased lipolytic activity. As the adipocytes grow, they accumulate triglycerides, becoming leptin resistant and promoting the synthesis and release of free fatty acids23. We observed that both WC and thigh circumference increased with VAT, but as previously reported, when WC and age were constant thigh circumference decreased with VAT for both men and women25. This is in line with previous evidence showing that VAT is the major risk factor of cardiometabolic morbidity and premature mortality, while lower-body fat mas plays a protective role and should be maintained when reducing VAT26. We observed sex differences in cardiometabolic conditions with men having a higher prevalence of all conditions compared to women, in line with previous evidence among middle-aged adults27,28. Hypertension, combined diabetes and prediabetes and hypertriglyceridemia prevalence were almost twice as high in men compared to women. Metabolic syndrome was 1.5 times higher in men compared to women. Closely related to these results are differences observed in WC and VAT being both higher in men compared to women as well as certain risk behaviours and socioeconomic differences such as lower consumption of alcohol and cigarettes and lower socioeconomic status in women compared to men. Sex differences on VAT are expected, since men are characterized by having a greater concentration of fat in the abdominal area compared to women that usually concentrates in the thighs and hip (gluteo-femoral pattern)29. Luxembourg is a small European country whose cultural diversity—nearly one in two residents is of foreign origin—accounts for the country’s well-documented heterogeneous and complex health profile. As in other high-income countries, in Luxembourg CVD is the leading cause of death (31.8%) while deaths due to endocrine, nutritional and metabolic diseases have more than doubled in the past 15 years, in both men and women30,31. Results from the present study show that compared to a previous study conducted in 2007 in Luxembourg, no reduction in cardiometabolic conditions has been observed over the last decade32 and even an increase has been noted in certain conditions such as diabetes or metabolic syndrome33. This could explain why cardiovascular diseases remained the main cause of mortality in Luxembourg in 201630. These results provide compelling evidence on the current burden of cardiovascular and metabolic conditions in Luxembourg in both men and women, and the need for public health initiatives to alleviate the societal impact of these highly prevalent disease conditions. Moreover, VAT management should be considered as a privilege area of study to tackle metabolic and cardiovascular health issues. As reported in other studies34,35, we observed that cardiometabolic conditions were more prevalent among individuals with poor nutritional status, smoking, consuming alcohol, and with sedentary habits. As observed by Shi et al. 2011, abstention from smoking, regular physical activity, and a moderate consumption of alcohol were related with less cardiometabolic conditions34. Moreover, studies have observed that a combination of a healthy diet and physical activity (regardless of the quantity/intensity) have a strong effect on reducing VAT, even with minimal weight loss, thus representing a cost effective non-pharmacological intervention to reduce the impact of VAT on cardiometabolic health22. At present, there is no specific treatment to reduce VAT without also reducing lower-body fat mass. There are only experimental clinical studies in progress with the aim of personalizing treatments to each specific situation/individual36,37. Studies also observed an effect of socioeconomic conditions, with those with lower socioeconomic status being at higher risk of developing cardiometabolic diseases38,39,40. Both lifestyle and socioeconomic characteristics explained in part, but not completely, the association between VAT and cardiometabolic conditions, as we observed that the association remained statistically significant even after adjusting for those factors. Although there is evidence showing that the socioeconomic effect could be mediated by health behaviours (e.g. smoking)35, we observed two independent effects (model 1 and model 2).
Results of this study must be interpreted with caution, taking into account the following limitations. The design of the present study was cross-sectional, hence no temporal relationship or causality can be inferred. The participation rate was rather low yet still representative of the target population41. VAT was measured indirectly. Instead of using biomedical imaging techniques (e.g. MRI, CT-Scan), we estimated VAT with anthropometric measurements. Nevertheless, the predictive anthropometric models of VAT used in the present study were previously developed and validated as the most accurate predictor of biological cardiometabolic risk factors, all-cause and cause-specific mortality in Europid descendants, when biomedical imaging data are not available17,18,19. Results from these studies observed a high correlation of VAT (assessed by imaging techniques) with anthropometric VAT models, whereas other studies observed that WC was higher correlated with SAT and fat mass than with VAT42. Finally, we did not have information on other potential biomarkers of cardiometabolic risk such as markers of inflammation. In summary, anthropometrically predicted VAT was associated in the present work with all metabolic and cardiovascular conditions in both men and women even after adjusting for socio-demographic and behavioural characteristics. This reinforces the role played by VAT as a major independent risk factor for cardiometabolic health. Anthropometrically predicted VAT should be used in future epidemiological studies to investigate metabolic and cardiovascular disease when no biomedical imaging measurements are available and replicated in other contexts /populations. Likewise, prospective and intervention studies should place greater focus on the impact of changes in VAT on cardiometabolic health.
Methods
Study population
Data for the present study came from EHES-LUX, a cross-sectional population based survey done in 2013–2015. The study was performed following a one-stage sampling procedure stratified by age, sex, and district of residence. Residents in Luxembourg aged 25–64 years old were invited randomly to participate in the survey with the exception of those individuals living in institutions such as hospitals, nursing homes or prisons. A total of 1529 individuals participated in the study and signed an informed consent20,41. The survey consisted in 3 sections: a health questionnaire, a medical examination and the collection of biological samples. The questionnaire and examination were performed by trained nurses in German, French, Portuguese and/or English. The analysis of biological samples was performed in a National certified laboratory. Out of all participants, 21 were pregnant women (excluded from the present analysis) and 1469 underwent biological analysis. A total of 1448 individuals had complete information in the three health sections of the survey (94.7%). While objective measures of VAT (e.g. CT-Scan, MRI) are not covered by EHES-LUX, the survey does dispose of accurate and complete set of anthropometric measurements. In the present study we excluded 5 individuals with values of visceral adipose tissue inferior or equal to zero. One individual did not have a measure of height and thus VAT was not possible to calculate. The final sample size of the present study was 1441 participants. The study was approved by the National Research Ethics Committee (CNER, No. 201205/07) and notified to the Luxemburgish National Commission for Data Protection (CNPD). All methods were performed in accordance with the relevant guidelines and regulations.
Cardiovascular and metabolic conditions
Hypertension was defined as systolic/diastolic blood pressure of ≥ 140/90 mm Hg, self-report of a physician diagnosis, or on antihypertensive medication41. Fasting plasma glucose, haemoglobin A1c, total cholesterol, high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C) and triglycerides were measured in participant’s blood samples41. Prediabetes and diabetes were defined as fasting glucose of ≥ 100 mg/dL, self-report of physician diagnosis, or on antidiabetic medication. Hypercholesterolemia was defined as total cholesterol ≥ 190 mg/dL or on medication to reduce cholesterol. High LDL-C was defined as LDL-C ≥ 115 mg/dL for both men and women43. Low HDL-C was defined as HDL-C < 50 mg/dL for women and 40 mg/dL for men. In this paper, we use the term hypercholesterolemia in reference to total cholesterol. Hypertriglycemia was defined as triglycerides ≥ 150 mg/dL or on medication. Metabolic Syndrome was defined following the International Diabetes Federation44. This definition includes the presence of central obesity WC ≥ 94 cm for men and WC ≥ 80 cm for women) and at least two of the following factors: total triglycerides ≥ 150 mg/dL or on medication, low HDL-C (< 40 mg/dL for men, < 50 mg/dL for women) or on medication, high blood pressure (systolic blood pressure ≥ 130 mm Hg or diastolic blood pressure ≥ 85 mm Hg) or on medication, high fasting plasma glucose (≥ 100 mg/dL) or self-report of a physician diagnosis.
Anthropometric variables
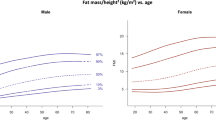
Weight and height, together with waist, hip and thigh circumferences were measured by trained nurses following Lohman recommendations45. BMI was calculated as weight divided by height squared (kg/m2). Estimated VAT was calculate as: 6*waist circumference − 4.41*proximal thigh circumference + 1.19*age – 213.65 for men and as 2.15*waist circumference – 3.63*proximal thigh circumference + 1.46*age + 6.22* BMI − 92.713 for women17. The equations used to estimate VAT are based on the strong correlation observed between thigh circumference and subcutaneous fat, as assessed by CT-Scan. The anthropometric VAT model assumed that by subtracting the most correlated anthropometric measurement with SATT from the most correlated anthropometric measurement with total abdominal and VAT as assessed by CT-Scan (WC), we can obtain the most accurate prediction of VAT by anthropometry. The population used to develop the equation was 253 individuals aged 18–78 years old, from Southern Europe, and with BMI values ranged between 16 and 53 kg/m2. Multiple linear regressions with an empirical selection of the variables were performed and validated. Model variances, collinearity, and errors (e.g. Bland and Altman plots representation) were assessed. Sensitivity and specificity of the anthropometric models for the diagnosis of visceral adiposity excess in a clinical setting, along with the positive and negative predictive value of the models for predicting a cut-off of 130 cm2, were also assessed. Models were validated in a second sample of 139 participants (77 women, BMI range: 19.25–47.96 kg/m2 and 62 men, BMI range: 18.55–52.94 kg/m2)17. Models were further validated as predictors of cardiometabolic conditions, cancer and early death in 10.624 participants from the US National Health and Nutrition Examination Survey (NHANES), followed for 20 years18,19.
Covariates
Based on the literature review we selected a list of potential covariates27,34,38. Demographic characteristics included age and sex (men and women). Lifestyle characteristics included smoking status (current smoking or quit < 12 months vs non-smokers or quit > 12 months), alcohol consumption (non-alcohol consumption, ≤ 6 drinks/week, > 6 drinks/week) and aerobic physical activity (min/week). For both alcohol and physical activity, we used validated questionnaires with standardized questions for European populations from the European Health Interview Survey (EHIS). Socioeconomic characteristics included education (tertiary education vs secondary and primary), and job status (employed vs not employed).
Statistical data analysis
We calculated VAT score quartiles (Q) based on statistical distribution (data-driven), clinical utility and for comparison with most previous studies using the same approach, for both men and women as follows: Q1 (≤ 113.84), Q2 (113.85–151.59), Q3 (151.60–196.65), and Q4 (≥ 196.66) for men and Q1 (≤ 58.78), Q2 (58.79–89.38), Q3 (89.39–127.35), and Q4 (≥ 127.36) for women. We test normality with the Kolmogorov–Smirnov test. Medians were used for continuous variables and frequencies for categorical variables. To analyse associations between cardiometabolic outcomes (e.g. hypertension, prediabetes and diabetes and total cholesterol) and covariates, we used a Pearson's chi-squared test (for probabilities related to frequencies) or Wilcoxon–Mann–Whitney U two-sample test (for probabilities related to medians) to compare characteristics between men and women. We used non parametric test because data was not normally distributed. Distributions of cardiometabolic conditions across VAT quartiles were measured with the Cochran-Armitage P-trend test for categorical variables and Jonckheere-Terpstra test for continuous variables. We performed multivariable logistic regression analyses to study the association between VAT quartiles and cardiometabolic outcomes in unadjusted (Model 1) and adjusted models for education and employment status (Model 2), and lifestyle (e.g. smoking, alcohol consumption and physical activity) and socioeconomic conditions (Model 3). All analyses were stratified by sex, given the well-known differences in visceral adiposity distribution and cardiometabolic disease prevalence between women and men46. Only variables with a P-value < 0.20 in univariate analyses were included in the final model. Although the main objective of the paper was to analyze VAT quartiles related to cardiometabolic outcomes, we performed additional analyses dividing individuals by quartiles of waist circumference. The aim was to assess whether the results were similar, better, or worse than those obtained with estimated VAT (Supplementary Table S2).We used the Akaike information criterion (AIC) to evaluate the model fit quality of the univariate analyses using VAT and WC quartiles. We calculated WC score quartiles for both men and women as follows: Q1 (≤ 88.50), Q2 (88.51–95.45), Q3 (95.46–103.99), and Q4 (≥ 104.00) for men and Q1 (≤ 76.00), Q2 (76.01–84.00), Q3 (84.01–93.49), and Q4 (≥ 93.50) for women. Models with VAT were best fitted (lower AIC values), with the exception of Metabolic Syndrome for men (Supplementary Table S3). The number of events per variable in the multivariable logistic regression were greater than 1047. Multicollinearity between covariates were tested. Weighted regression was used to correct for possible heteroscedasticity. A two-tailed P-value < 0.05 was considered statistically significant. Analyses were performed using SAS version 9.4 (SAS Institute, Inc, Cary, NC).
Data availability
The data generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Change history
25 August 2021
A Correction to this paper has been published: https://doi.org/10.1038/s41598-021-96667-z
References
Danaei, G. et al. National, regional, and global trends in fasting plasma glucose and diabetes prevalence since 1980: systematic analysis of health examination surveys and epidemiological studies with 370 country-years and 2· 7 million participants. The Lancet 378, 31–40 (2011).
Danaei, G. et al. National, regional, and global trends in systolic blood pressure since 1980: systematic analysis of health examination surveys and epidemiological studies with 786 country-years and 5· 4 million participants. The Lancet 377, 568–577 (2011).
Farzadfar, F. et al. National, regional, and global trends in serum total cholesterol since 1980: systematic analysis of health examination surveys and epidemiological studies with 321 country-years and 3· 0 million participants. The Lancet 377, 578–586 (2011).
Han, T. S. & Lean, M. E. A clinical perspective of obesity, metabolic syndrome and cardiovascular disease. JRSM Cardiovasc. Dis. 5, 2048004016633371 (2016).
Roth, G. A. et al. Global, regional, and national burden of cardiovascular diseases for 10 causes, 1990 to 2015. J. Am. Coll. Cardiol. 23715 (2017).
Naghavi, M. et al. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980–2016: A systematic analysis for the Global Burden of Disease Study 2016. The Lancet 390, 1151–1210 (2017).
Deaton, C. et al. The global burden of cardiovascular disease. Eur. J. Cardiovasc. Nurs. 10, S5–S13 (2011).
Lee, J. J. et al. Visceral and intrahepatic fat are associated with cardiometabolic risk factors above other ectopic fat depots: The Framingham heart study. Am. J. Med. 131, 684-692.e612. https://doi.org/10.1016/j.amjmed.2018.02.002 (2018).
Mathieu, P., Poirier, P., Pibarot, P., Lemieux, I. & Despres, J. P. Visceral obesity: the link among inflammation, hypertension, and cardiovascular disease. Hypertension (Dallas, Tex. : 1979) 53, 577–584. https://doi.org/10.1161/hypertensionaha.108.110320 (2009).
Kershaw, E. E. & Flier, J. S. Adipose tissue as an endocrine organ. J. Clin. Endocrinol. Metab. 89, 2548–2556 (2004).
Vegiopoulos, A., Rohm, M. & Herzig, S. Adipose tissue: Between the extremes. EMBO J. 36, 1999–2017. https://doi.org/10.15252/embj.201696206 (2017).
Nicklas, B. J. et al. Visceral adipose tissue cutoffs associated with metabolic risk factors for coronary heart disease in women. Diabetes Care 26, 1413–1420 (2003).
Fang, H., Berg, E., Cheng, X. & Shen, W. How to best assess abdominal obesity. Curr. Opin. Clin. Nutr. Metab. Care 21, 360–365. https://doi.org/10.1097/mco.0000000000000485 (2018).
Despres, J. P., Prud’homme, D., Pouliot, M. C., Tremblay, A. & Bouchard, C. Estimation of deep abdominal adipose-tissue accumulation from simple anthropometric measurements in men. Am. J. Clin. Nutr. 54, 471–477. https://doi.org/10.1093/ajcn/54.3.471 (1991).
Lemieux, S., Prud’homme, D., Bouchard, C., Tremblay, A. & Despres, J. P. A single threshold value of waist girth identifies normal-weight and overweight subjects with excess visceral adipose tissue. Am. J. Clin. Nutr. 64, 685–693. https://doi.org/10.1093/ajcn/64.5.685 (1996).
Wajchenberg, B. L. Subcutaneous and visceral adipose tissue: their relation to the metabolic syndrome. Endocr. Rev. 21, 697–738 (2000).
Samouda, H. et al. VAT=TAAT-SAAT: innovative anthropometric model to predict visceral adipose tissue without resort to CT-Scan or DXA. Obesity (Silver Spring, Md.) 21, E41–50. https://doi.org/10.1002/oby.20033 (2013).
Brown, J. C., Harhay, M. O. & Harhay, M. N. Anthropometrically-predicted visceral adipose tissue and mortality among men and women in the third national health and nutrition examination survey (NHANES III). Am. J. Hum. Biol. 29. https://doi.org/10.1002/ajhb.22898 (2017).
Brown, J. C., Harhay, M. O. & Harhay, M. N. Anthropometrically predicted visceral adipose tissue and blood-based biomarkers: A cross-sectional analysis. Eur. J. Nutr. 57, 191–198. https://doi.org/10.1007/s00394-016-1308-8 (2018).
Ruiz-Castell, M. et al. Hypertension burden in Luxembourg: Individual risk factors and geographic variations, 2013 to 2015 European Health Examination Survey. Medicine 95, e4758. https://doi.org/10.1097/md.0000000000004758 (2016).
Samouda, H. et al. Geographical variation of overweight, obesity and related risk factors: Findings from the European Health Examination Survey in Luxembourg, 2013–2015. PLoS ONE 13, e0197021. https://doi.org/10.1371/journal.pone.0197021 (2018).
Neeland, I. J. et al. Visceral and ectopic fat, atherosclerosis, and cardiometabolic disease: A position statement. Lancet Diabetes Endocrinol. 7, 715–725. https://doi.org/10.1016/s2213-8587(19)30084-1 (2019).
Ibrahim, M. M. Subcutaneous and visceral adipose tissue: structural and functional differences. Obes. Rev. 11, 11–18. https://doi.org/10.1111/j.1467-789X.2009.00623.x (2010).
Gruzdeva, O., Borodkina, D., Uchasova, E., Dyleva, Y. & Barbarash, O. Localization of fat depots and cardiovascular risk. Lipids Health Dis. 17, 218. https://doi.org/10.1186/s12944-018-0856-8 (2018).
Kuk, J. L., Janiszewski, P. M. & Ross, R. Body mass index and hip and thigh circumferences are negatively associated with visceral adipose tissue after control for waist circumference. Am. J. Clin. Nutr. 85, 1540–1544. https://doi.org/10.1093/ajcn/85.6.1540 (2007).
Stefan, N. Causes, consequences, and treatment of metabolically unhealthy fat distribution. Lancet Diabetes Endocrinol. 8, 616–627. https://doi.org/10.1016/s2213-8587(20)30110-8 (2020).
Regitz-Zagrosek, V., Lehmkuhl, E. & Weickert, M. O. Gender differences in the metabolic syndrome and their role for cardiovascular disease. Clin. Res. Cardiol. 95, 136–147. https://doi.org/10.1007/s00392-006-0351-5 (2006).
Hu, G. et al. The increasing prevalence of metabolic syndrome among Finnish men and women over a decade. J. Clin. Endocrinol. Metab. 93, 832–836. https://doi.org/10.1210/jc.2007-1883 (2008).
Karpe, F. & Pinnick, K. E. Biology of upper-body and lower-body adipose tissue–link to whole-body phenotypes. Nat. Rev. Endocrinol. 11, 90–100. https://doi.org/10.1038/nrendo.2014.185 (2015).
S., L. Statistiques des causes de décès pour l'année 2016. Ministère de la Santé / Direction de la Santé - Service des Statistiques (2018).
Lehners, S. (Ministère de la Santé / Direction de la Santé - Service des Statistiques, 2015).
Alkerwi, A. et al. First nationwide survey on cardiovascular risk factors in Grand-Duchy of Luxembourg (ORISCAV-LUX). BMC Public Health 10, 468. https://doi.org/10.1186/1471-2458-10-468 (2010).
Alkerwi, A. et al. Prevalence of the metabolic syndrome in Luxembourg according to the Joint Interim Statement definition estimated from the ORISCAV-LUX study. BMC Public Health 11, 4. https://doi.org/10.1186/1471-2458-11-4 (2011).
Shi, L., Morrison, J. A., Wiecha, J., Horton, M. & Hayman, L. L. Healthy lifestyle factors associated with reduced cardiometabolic risk. Br. J. Nutr. 105, 747–754. https://doi.org/10.1017/s0007114510004307 (2011).
Petrovic, D. et al. The contribution of health behaviors to socioeconomic inequalities in health: A systematic review. Prevent. Med. (2018).
Kodama, N. et al. Effects of pioglitazone on visceral fat metabolic activity in impaired glucose tolerance or type 2 diabetes mellitus. J. Clin. Endocrinol. Metab. 98, 4438–4445. https://doi.org/10.1210/jc.2013-2920 (2013).
Stanley, T. L. et al. Effect of tesamorelin on visceral fat and liver fat in HIV-infected patients with abdominal fat accumulation: A randomized clinical trial. JAMA 312, 380–389. https://doi.org/10.1001/jama.2014.8334 (2014).
Elovainio, M. et al. Socioeconomic differences in cardiometabolic factors: social causation or health-related selection? Evidence from the Whitehall II Cohort Study, 1991–2004. Am. J. Epidemiol. 174, 779–789. https://doi.org/10.1093/aje/kwr149 (2011).
Ogunsina, K., Dibaba, D. T. & Akinyemiju, T. Association between life-course socio-economic status and prevalence of cardio-metabolic risk ractors in five middle-income countries. J. Glob. Health 8, 020405. https://doi.org/10.7189/jogh.08.020405 (2018).
Puckrein, G. A., Egan, B. M. & Howard, G. Social and medical determinants of cardiometabolic health: The big picture. Ethn. Dis. 25, 521–524. https://doi.org/10.18865/ed.25.4.521 (2015).
Bocquet, V. et al. Study design and characteristics of the Luxembourg European Health Examination Survey (EHES-LUX). BMC Public Health 18, 1169. https://doi.org/10.1186/s12889-018-6087-0 (2018).
Camhi, S. M. et al. The relationship of waist circumference and BMI to visceral, subcutaneous, and total body fat: sex and race differences. Obesity (Silver Spring, Md.) 19, 402–408. https://doi.org/10.1038/oby.2010.248 (2011).
Graham, I. et al. European guidelines on cardiovascular disease prevention in clinical practice: executive summary: Fourth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (Constituted by representatives of nine societies and by invited experts). Eur. Heart J. 28, 2375–2414. https://doi.org/10.1093/eurheartj/ehm316 (2007).
the rationale and the results. Zimmet, P., KG, M. M. A. & Serrano Ríos, M. A new international diabetes federation worldwide definition of the metabolic syndrome. Rev. Esp. Cardiol. 58, 1371–1376 (2005).
Lohmann TG, R. A., Martorell R. Anthropometric standardization reference manual. Abriged edition (1988).
Karastergiou, K., Smith, S. R., Greenberg, A. S. & Fried, S. K. Sex differences in human adipose tissues: The biology of pear shape. Biol. Sex Differ. 3, 13. https://doi.org/10.1186/2042-6410-3-13 (2012).
Peduzzi, P., Concato, J., Kemper, E., Holford, T. R. & Feinstein, A. R. A simulation study of the number of events per variable in logistic regression analysis. J. Clin. Epidemiol. 49, 1373–1379 (1996).
Acknowledgements
We are grateful to the population of Luxembourg and to all the EHES-LUX team who have contributed to this study. We would like to thank Couffignal S, Kuemmerle A, Dincau M, Mormont D, Barre J, Chioti A, Delagardelle C, Michel G, Schlesser M, Schmit JC, Gantenbein M, Lieunard C, Columeau A, Kiemen M, Weis J, Ambroset G, Billy A, Larcelet M, Marcic D, Gauthier C, and Viau-Courville M for their valuable contributions. We would like to thank the national laboratory Ketterthill for the analysis of the biological samples. This research was funded by the National Research Fund of Luxembourg ([C17/BM/11653863/iMPACT.lu to MRC)], the Directorate and Ministry of Health, and the Ministry of Higher Education and Research (MESR).
Funding
This work was supported by the National Research Fund of Luxembourg [C17/BM/11653863/iMPACT.lu to MRC], the Directorate and Ministry of Health and the Ministry of Higher Education and Research (MESR).
Author information
Authors and Affiliations
Contributions
M.R.-C., H.S. and L.H. conceptualized and designed the study. M.R.-C. and V.B. performed the statistical analysis. S.S. and G.F. provided scientific consultancy. M.R.-C., S.S., G.F., H.S. and L.H. interpreted the data. M.R.-C. drafted the article. L.H. supervised the study. All authors participated in the revision of the article. All authors contributed to and have approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this Article was revised: Modifications have been made to the Abstract, Results, Table 1 and the Methods section. Full information regarding the corrections made can be found in the correction for this Article.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ruiz-Castell, M., Samouda, H., Bocquet, V. et al. Estimated visceral adiposity is associated with risk of cardiometabolic conditions in a population based study. Sci Rep 11, 9121 (2021). https://doi.org/10.1038/s41598-021-88587-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-88587-9
This article is cited by
-
How effective are anthocyanins on healthy modification of cardiometabolic risk factors: a systematic review and meta-analysis
Diabetology & Metabolic Syndrome (2023)
-
Visceral fat and cardiometabolic future in children and adolescents: a critical update
Pediatric Research (2023)
-
Low Perception of Obesity as a Pathological Condition Among Italian Cardiologists
High Blood Pressure & Cardiovascular Prevention (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.