Abstract
Little is known about the early-life cardiovascular health impacts of fine particulate air pollution (PM2.5) and oxidant gases. A repeated-measures panel study was used to evaluate associations between outdoor PM2.5 and the combined oxidant capacity of O3 and NO2 (using a redox-weighted average, Ox) and retinal vessel diameter and blood pressure in children living in a region impacted by residential biomass burning. A median of 6 retinal vessel and blood pressure measurements were collected from 64 children (ages 4–12 years), for a total of 344 retinal measurements and 432 blood pressure measurements. Linear mixed-effect models were used to estimate associations between PM2.5 or Ox (same-day, 3-day, 7-day, and 21-day means) and retinal vessel diameter and blood pressure. Interactions between PM2.5 and Ox were also examined. Ox was inversely associated with retinal arteriolar diameter; the strongest association was observed for 7-day mean exposures, where each 10 ppb increase in Ox was associated with a 2.63 μm (95% CI − 4.63, − 0.63) decrease in arteriolar diameter. Moreover, Ox modified associations between PM2.5 and arteriolar diameter, with weak inverse associations observed between PM2.5 and arteriolar diameter only at higher concentrations of Ox. Our results suggest that outdoor air pollution impacts the retinal microvasculature of children and interactions between PM2.5 and Ox may play an important role in determining the magnitude and direction of these associations.
Similar content being viewed by others
Introduction
Outdoor air pollution is associated with adverse cardiovascular outcomes1,2. Although cardiovascular disease (CVD) manifests in adulthood, preclinical changes that contribute to and accelerate the development of CVD begin in childhood3. Therefore, identifying early-life modifiable exposures that adversely affect cardiovascular health may provide important information to help prevent CVD in later life.
Most research on associations between ambient air pollution and cardiovascular outcomes has focused on particulate matter exposure and consistent evidence from epidemiological and animal studies support a causal relationship1. Oxidant gases, such as ozone (O3) and nitrogen dioxide (NO2), have also been associated with adverse cardiovascular outcomes, although results have been less consistent4,5. Individuals are exposed to both particulate matter and oxidant gases simultaneously, and some evidence suggests these pollutants interact to affect health outcomes. For example, stronger associations between long-term6 and short-term7 fine particulate matter air pollution (PM2.5) and mortality were found when the combined oxidant capacity of NO2 and O3 (using a redox-weighted average, Ox) was higher, highlighting the importance of considering Ox when evaluating PM2.5 health effects.
The microcirculation represents a large component of the circulatory system and microvascular dysfunction is an important predictor of CVD events8. Measuring the structure of the retinal microvasculature through fundus photography can serve as a simple, non-invasive method to evaluate microvascular health9, as the retinal microcirculation is anatomically and physiologically similar to the cerebrovascular10 and coronary11 microcirculation. Of the various parameters that can be estimated with fundus photography, the most common and easily estimated parameters are the diameters of retinal blood vessels. The relationship between air pollution and retinal blood vessel diameter has been examined several times in adults in cross-sectional12 and repeated-measures studies13,14,15, and twice in children in repeated-measures studies16,17. In one study of school-aged children living in an urban centre in Belgium, short-term PM2.5 (measured on the same day as the retinal image and the day before) was associated with narrower retinal arteriolar diameter and wider venular diameter16. In another study of children ages 4–6 years (also living in Belgium), PM2.5 measured during the same day as the retinal image, the day before the retinal image, and the week before the retinal image was associated with both narrower and wider retinal arterial diameter, depending on the exposure lag, while NO2 was not associated with retinal vessel diameter17. Due to the limited number of studies that have explored these associations in children and inconsistent results, these relationships necessitate further exploration.
Another preclinical cardiovascular outcome that may be adversely affected by outdoor air pollution is blood pressure4,5,18, but associations between short-term air pollution and blood pressure have not been extensively studied in children. In a recent meta-analysis of four studies that looked at associations between short-term air pollution (defined as < 30 days) and blood pressure in children, each 10 μg/m3 increase in particulate matter < 10 μm (PM10) was associated with a very small (< 1 mm Hg) increase in systolic blood pressure, while no clear associations were observed between PM10 or PM2.5 and diastolic blood pressure19. An understanding of the relationship between air pollution and blood pressure in children is important because childhood blood pressure tracks into adulthood20 and elevated blood pressure is an important risk factor for the development of cardiovascular disease.
To our knowledge, no studies have explored how the combined oxidant capacity of NO2 and O3 (Ox) affects retinal blood vessel diameter or blood pressure, or whether associations between PM2.5 and these health outcomes are modified by Ox. In addition, no studies have focused specifically on the impact of residential biomass burning-related PM2.5 to changes in the retinal microvasculature or blood pressure. This is an important consideration because residential biomass burning is a major source of PM2.5 in rural Canada21,22 due to the prevalence of wood burning to heat homes, and biomass-burning sources of PM2.5 may be harmful to cardiovascular health22.
To address gaps in our current understanding of air pollution impacts on cardiovascular health of children, we conducted a panel study to examine associations between outdoor PM2.5 and Ox on changes to retinal vessel diameter and blood pressure in children living in a region of Canada known to be impacted by residential biomass burning. We also considered whether the impact of PM2.5 on retinal blood vessel diameter or blood pressure was modified by outdoor concentrations of Ox.
Materials and methods
Study design and population
We conducted a repeated-measures panel study at two elementary schools in the neighbouring communities of Courtenay and Cumberland on the east coast of central Vancouver Island, in the province of British Columbia, Canada. The distance between the two schools is approximately 8 km. This is a rural area of Canada, with a population size of approximately 26,000 in Courtenay and 4,000 in Cumberland in 2016 (the most recent census year). The study took place from September 2018 to June 2019 in Courtenay, and from September 2019-March 2020 in Cumberland (the study was terminated three months early in Cumberland because of school closures due to the COVID-19 pandemic). The study took place over sequential school years (instead of at both schools in the same school year) because study equipment and research staff were limited. This area has elevated outdoor PM2.5 concentrations during the cold season (approximately November–April) because many households rely on wood burning as their primary heating source22. During the warmer season, outdoor PM2.5 concentrations are typically very low (i.e. < 5 μg/m3)22.
Children at each school were eligible to participate if they were 4–12 years of age at enrollment, lived in a non-smoking home, and resided in the community surrounding either school. Recruitment occurred during September of each school year, and health outcome measurements began in October. Exams were scheduled at intervals of approximately one month and were staggered throughout each month (as opposed to measuring everyone on the same day) in order to increase exposure variation and minimize the impact on regular school activities. Exams took place on Thursday and Friday mornings at the school site in Courtenay, and throughout the week in the morning and early afternoon in Cumberland. Oral assent was obtained from children and written informed consent was obtained from their parent/guardian. At baseline, parents/guardians of each participant completed a questionnaire to collect basic sociodemographic and household information. The study was approved by McGill University Research Ethics Board and the Health Canada Research Ethics Board and all methods were performed in accordance with the relevant guidelines and regulations.
Air pollutants and meteorological data
In the first year of the study, daily mean outdoor PM2.5 concentrations in Courtenay were measured using a BAM (Beta-Attenuation Monitor) 1020 instrument located at the provincial air monitoring station situated on the playground of the school. In case there were any problems or gaps in data collection with the government-run monitor, we also set up a Partisol 2025i sequential air sampler at the same location, which collected daily integrated PM2.5 samples that were subsequently sent for gravimetric analysis. However, for this year of the study, we ended up only using PM2.5 measurements from the BAM instrument in our analyses because there were fewer missing data. In the second year of the study in Cumberland, the school was not located at a provincial monitoring station so PM2.5 was only measured using a Partisol 2025i sequential air sampler that we set up on the roof of the school. Although the PM2.5 values used in analysis were from different instruments each year of the study, we observed a strong correlation in duplicate measurements in Courtenay (r2 = 0.94) and both instruments are considered acceptable methods to monitor PM2.5 by the United States Environmental Protection Agency23.
For both years of the study, ozone and nitrogen dioxide were measured at the provincial air monitoring site in Courtenay with an API T400 UV Absorption O3 analyzer and an API T200 chemiluminescence NO/NO2/NOx analyzer, respectively; due to equipment limitations, we were unable to set up our own monitors for O3 and NO2 in Cumberland so relied on measurements from Courtenay as approximations. The combined weighted oxidant capacity (Ox) of NO2 and O3 was calculated as a weighted average of NO2 and O3, with weights equivalent to the respective redox potentials using the formula Ox = [(1.07 × NO2) + (2.075 × O3)]/3.145), as previously described24,25. Indoor air pollution was not measured in this study. Meteorological data, including mean daily temperature, wind speed, precipitation, and humidity were available from a provincial monitoring station located approximately 8 km from the school in Courtenay and 15 km from the school in Cumberland.
In the second year of the study (in Cumberland), there were some days with missing PM2.5 data due to a delay in setting up the PM2.5 monitor at the start of the study and occasional technical issues throughout the study. A model to predict missing PM2.5 was developed, and predicted values were used to impute missing PM2.5. The prediction model regressed log-transformed PM2.5 on several predictors including same-day PM2.5, NO2, temperature, wind speed, and precipitation measured at a nearby provincial monitoring station. Global search regression using the gsreg command in Stata was used to select the final prediction model, considering all possible combinations of interactions and square terms of predictor variables. The best fitting model had a R2 of 0.72. There was a total of 58 days in which PM2.5 was imputed (approximately 12% of PM2.5 values in the time series).
Clinical exams
Clinical exams were conducted by two trained research assistants (one research assistant at each site) and involved imaging the retinal microvasculature and measuring blood pressure, height, and weight. All exams took place in a designated, quiet room in each school.
The fundus of the left and right eye of participants was photographed with a Canon CR2-AF 45° 20.2-megapixel digital nonmydriatic retinal camera in a darkened room. Images were analyzed by one grader (J.K.) using the semi-automatic MONA-REVA software (version 3.0.0, VITO Health, Mol, Belgium). For each participant, images from either the left or right eye were analyzed; the choice of whether to analyze the left or right eye of each participant depended on which eye had the most high quality images (where image quality was judged by how sharp the image was, whether the optic disc was centered, and whether the arterioles and venules were distinguishable from one another). Epidemiological studies have demonstrated a high correlation in retinal vessel diameters between the left and right eye26,27. When analyzing the images, the diameter of the optic disc was first determined, then the width of the retinal arterioles and venules were measured within an area equal to 0.5–1 times the disc diameter from the optic disc margin (Figure S1 in the Supplemental Material). Diameters of the 6 largest arterioles and venules were used in the revised Parr Hubbard formula28 to estimate Central Retinal Arteriolar Equivalent (CRAE) and Central Retinal Venular Equivalent (CRVE), summary measures reflecting average arteriolar and venular diameter. For each participant, the same 6 arterioles and venules were used to calculate CRAE and CRVE in repeated measurements.
Following fundus photography, blood pressure was measured with the SunTech CT40 vital signs device. While sitting upright in a chair with their non-dominant arm resting on a table, an appropriately sized arm cuff was selected based on the circumference of the child’s upper arm, and blood pressure was measured twice with one minute between each reading. If systolic or diastolic blood pressure from the two successive readings were > 10 mm Hg apart, a third reading was done. The average of the two closest readings was calculated and used for analysis.
With shoes and bulky clothing removed, height was measured to the nearest 0.1 cm with the Seca 213 Stadiometer, and weight was measured to the nearest 0.1 kg using the Seca 874 Digital Scale. Measurements were taken in duplicate, and an average was calculated. Body mass index-for-age z-scores were then calculated based on the World Health Organization child growth standards29.
Statistical analyses
Associations between outdoor air pollution and retinal blood vessel diameter
Linear mixed-effect models with a random subject intercept (with a first order autoregressive correlation structure) were used to evaluate associations between PM2.5 (as a continuous variable, in units of μg/m3) or Ox (a continuous variable, in units of ppb) and within-person changes in CRAE or CRVE (continuous variables, in units of μm). We assessed associations between CRAE or CRVE with four different exposure lags: PM2.5 or Ox on the day of the retinal image, 3-day mean (mean of PM2.5 or Ox on the day of the retinal image and two preceding days), 7-day mean, and 21-day mean. These time periods were selected to examine both acute and sub-chronic exposures. For each exposure-outcome relationship, we ran crude models, and models adjusted for an a priori list of potential confounders or predictors of retinal blood vessel diameter, including 7-day mean temperature (degrees Celsius) and humidity (%) (which may be correlated with seasonal differences in air pollution concentrations), body mass index-for-age z-score at the time of the retinal image, sex, age (years), highest level of maternal education (high school or less/ community or technical college/ university), and time of day of outcome assessment (≤ 11:00 AM or > 11:00 AM). We also explored whether associations between PM2.5 and retinal vessel diameter were modified by concentrations of Ox by running models with an interaction term between PM2.5 and Ox (as continuous variables using the same exposure lag for both air pollutants), while adjusting for the same set of covariates identified above. A p-value less than 0.05 for the interaction term was interpreted as evidence of effect modification (on the additive scale). We explored whether including a fixed effect for school was necessary to account for potential clustering within schools, but it did not improve model fit based on the minimum Akaike Information Criterion (AIC) so was not included in the final models. We also explored potential non-linear relationships between continuous covariates and CRAE or CRVE using spline terms, but as splines did not improve model fit (based on the minimum AIC), final models included linear terms for all continuous covariates. Residual plots were generated to verify model assumptions. All estimates are expressed as a change in retinal arteriolar or venular diameter per 5 μg/m3 increase PM2.5 or 10 ppb increase in Ox, which reflect the approximate interquartile ranges of PM2.5 and Ox.
Associations between outdoor air pollution and blood pressure
Linear mixed-effect models with a random subject intercept (and a first order autoregressive correlation structure) were used to evaluate associations between short-term and sub-chronic PM2.5 or Ox (the same exposure lags described above) and systolic and diastolic blood pressure. Similar to analyses for retinal vessel diameter, crude models, adjusted models (including the same set of covariates identified above), and models with an interaction term between PM2.5 and Ox were examined.
Sensitivity analyses
Several sensitivity analyses were conducted. First, analyses were repeated excluding retinal images or blood pressure measurements in which the relevant PM2.5 exposure lags included imputed PM2.5 values. Second, instead of evaluating associations between Ox and retinal blood vessel diameter and blood pressure, we looked at associations with each gas (O3 or NO2) individually. Third, we additionally adjusted our models for season (fall/winter/spring/summer).
All data cleaning and manipulation were conducted using Stata v.15 (StataCorp, College Station, TX), and all modelling was conducted using R (R-project.org).
Results
Study population
A description of the study population is presented in Table 1. A total of 71 children (median age of 8 years) enrolled in the study and high-quality retinal images were available for 64 of these children. Most participants (N = 54, 76%) enrolled during the second year (2019–2020) of the study. The sample was predominantly Caucasian (N = 64, 90%), there were a similar number of boys and girls, and most mothers of participants had some post-secondary education. The majority of participants lived in households that used electricity (N = 46, 65%) or natural gas (N = 21, 30%) as their primary heating source, while few households used wood burning as their primary heating source (N = 3, 4%). The use of woodstoves or wood fireplaces as a secondary source of heating was uncommon in this sample (N = 6, 8%), and 17 participants (24%) lived in households that used an air filter. The average (± standard deviation) body mass index-for age z-score was 0.7 ± 1.3, indicating body mass index of children was slightly higher than the age and sex-specific reference population. Mean (± standard deviation) systolic and diastolic blood pressure at baseline were 106 ± 7 and 63 ± 5 mm Hg, respectively, while mean (± standard deviation) CRAE and CRVE at baseline were 181.51 ± 11.88 and 260.34 ± 15.70 μm.
There was a total of 344 high quality retinal images and 432 blood pressure measurements. The median number of retinal images and blood pressure measurements per child was 6 but some children had as few as three measurements. The maximum number of retinal images was 6 per child, and for blood pressure the maximum number of measurements was 10 per child. Median time between retinal images and blood pressure measurements was 28 days (range 20–63 days).
Exposure characteristics
Distributions of daily mean outdoor PM2.5 and Ox concentrations throughout the study are shown in Fig. 1 and additional exposure characteristics are provided in Table S1 of the Supplemental Material. Overall, mean daily PM2.5 ranged from < 1 μg/m3 to 32 μg/m3 over the entire study period, and was slightly higher and more variable in the first year of the study (mean ± standard deviation: 9 ± 7 μg/m3) than in the second year of the study (mean ± standard deviation: 6 ± 4 μg/m3). Average PM2.5 on the day of the retinal image was the same as the 3-day mean, 7-day mean, and 21-day mean concentrations (7 μg/m3), although the standard deviation was slightly larger on the day of the retinal image (standard deviation: 6 μg/m3) compared to the 3-day and 7-day means (standard deviation of 4 μg/m3 for both lags), and the 21-day mean (standard deviation: 3 μg/m3). Ox ranged from 3 to 27 ppb over the entire study period, and was slightly higher and more variable during the first year of the study (mean ± standard deviation: 14 ± 6 ppb) compared to the second year of the study (mean ± standard deviation: 13 ± 5 ppb). Mean Ox for all exposure lags was 13 ppb, and the standard deviation was slightly larger on the day of the retinal image (6 ppb) compared to the 3-day, 7-day, and 21-day means (5 ppb). There was a moderate inverse correlation between PM2.5 and Ox based on Pearson's correlation coefficient (r2 = − 0.43).
Associations between outdoor PM2.5 or Ox and retinal blood vessel diameter
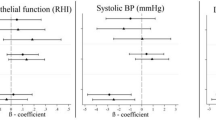
Associations between PM2.5 or Ox from single-pollutant models and retinal arteriolar and venular diameter are presented in Fig. 2 and Tables S2 and S3 of the Supplemental Material. In adjusted models, PM2.5 was associated with a small increase in CRAE but 95% confidence intervals included the null. The strength of this association was largest for the 21-day exposure lag: a 5 μg/m3 increase in 21-day mean PM2.5 was associated with a 1.42 μm increase in CRAE (95% CI − 0.47, 3.32). On the other hand, Ox was consistently associated with a reduction in CRAE and the strongest association was for the 7-day exposure lag: a 10 ppb increase in Ox was associated with a 2.63 μm decrease in CRAE (95% CI − 4.63, − 0.63).
Estimated change (95% confidence interval) in (A) central retinal arteriolar diameter (CRAE, μm); (B) central retinal venular diameter (CRVE, μm); (C) systolic blood pressure (SBP, mm Hg) and; (D) diastolic blood pressure (DBP, mm Hg) per 5 μg/m3 increase in PM2.5 or 10 ppb increase in Ox. Models adjusted for 7-day mean temperature and humidity, body mass index-for-age z-score on the day of the retinal image, sex, age (years), maternal education (high school or less vs. community/technical college vs. university), and time of day of outcome assessment (≤ 11:00 AM vs. > 11:00 AM). aPM2.5 or Ox on the same day as the outcome assessment. bMean PM2.5 or Ox on the day of the outcome assessment and two preceding days. cMean PM2.5 or Ox on the day of the outcome assessment and 6 preceding days. dMean PM2.5 or Ox on the day of the outcome assessment and 20 preceding days.
In general, positive association were observed between PM2.5 and venular diameter and inverse associations were observed between Ox and venular diameter but the strength of these associations was small and 95% confidence intervals included the null in all adjusted models. There were no notable differences in associations between PM2.5 and CRAE or CRVE when analyses excluded retinal images with imputed PM2.5 (Table S4 of the Supplemental Material). In sensitivity analyses, estimated associations between O3 and retinal blood vessel diameter were similar to that of Ox (Table S5 of the Supplemental Material), while NO2 was positively associated with retinal arteriolar and venular diameter, but estimates were imprecise and all confidence intervals included the null (Table S6 of the Supplemental Material). When models were additionally adjusted for season, conclusions remain the same (Table S7 and S8 of the Supplemental Material).
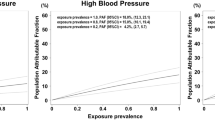
Models including an interaction term between PM2.5 and Ox suggested that Ox modified associations between outdoor PM2.5 and retinal arteriolar diameter (p-values from interaction terms for same-day, 3-day mean, 7-day mean and 21-day mean exposures: 0.10, 0.04, 0.02, and 0.03, respectively). To visualize the associations between PM2.5 and CRAE modified by Ox, we plotted predicted values of CRAE across a range of PM2.5 concentrations (2–16 μg/m3) stratified by Ox concentrations 1 standard deviation above or below the mean (Fig. 3). This figure suggests that when Ox is low there is a weak positive association between PM2.5 and CRAE, while when Ox concentrations are higher there is a weak inverse association between PM2.5 and CRAE. These trends were more pronounced in the 3-day, 7-day, and 21-day lags compared to same-day exposure. Similar figures were generated to visualize how concentrations of PM2.5 modified the associations between Ox and CRAE and suggest that a negative association between Ox and CRAE is only present when concentrations of PM2.5 were high (i.e., 1 standard deviation above the mean) (Figure S2 of the Supplemental Material). There was no evidence of interaction between PM2.5 and Ox for CRVE (p-values from interaction terms for same-day, 3-day mean, 7-day mean, and 21-day mean exposures: 0.52, 0.63, 0.14, and 0.83, respectively).
Predicted values and 95% confidence intervals for central retinal arteriolar equivalent (CRAE) at different concentrations of PM2.5, stratified by Ox (1 standard deviation below and above mean Ox). Plots correspond to (A): Same-day exposure lag; (B): 3-day mean exposure lag; (C): 7-day mean exposure lag; (D): 21-day mean exposure lag.
Associations between outdoor PM2.5 or Ox and blood pressure
Associations between outdoor PM2.5 or Ox concentrations and blood pressure are presented in Fig. 2 and Tables S2 and S3 of the Supplemental Material. In adjusted models, each 5 μg/m3 increase in 3-day mean PM2.5 was associated with a 0.95 mm Hg reduction in systolic blood pressure (95% CI − 1.86, − 0.05), 7-day mean PM2.5 was associated with a 1.11 mm Hg reduction in systolic blood pressure (95% CI − 2.12, − 0.09), and 21-day mean PM2.5 was associated with a 1.70 mm Hg reduction in systolic blood pressure (95% CI − 2.98, − 0.41), but these associations were slightly attenuated and 95% confidence intervals included the null in sensitivity analyses excluding exams where PM2.5 was imputed (Table S4 of the Supplemental Material). Conversely, positive associations were observed between Ox and systolic blood pressure, with the largest association detected for the 21-day exposure lag (estimated change per 10 ppb increase in 21-day mean Ox from an adjusted model: 1.59 (95% CI − 0.06, 3.25)), but confidence intervals included the null for all exposure lags. There were no clear associations between PM2.5 or Ox and diastolic blood pressure. In sensitivity analyses, associations between O3 and blood pressure were similar to those found for Ox and no clear relationship was observed between NO2 and blood pressure (Tables S5 and S6 of the Supplemental Material). When models were additionally adjusted for season, conclusions are similar except the confidence intervals for associations between 3-day and 7-day mean PM2.5 now include the null (Table S7 and S8 of the Supplemental Material).
There was evidence that 7-day mean Ox modified the associations between 7-day mean PM2.5 and systolic blood pressure (p-value from interaction term: 0.04), but there was no evidence of a significant interaction for the same-day, 3-day mean, or 21-day mean exposures (p-values from interaction terms for same-day, 3-day mean, and 21-day mean exposures: 0.63, 0.26, 0.55). Figure S3 in the Supplemental Material suggests that an inverse relationship between 7-day mean PM2.5 and systolic blood pressure is present when 7-day mean Ox concentrations are above average (i.e., 1 standard deviation above the mean), while there is no association when Ox concentrations are lower (i.e., 1 standard deviation below mean). Ox did not modify associations between PM2.5 or diastolic blood pressure for any exposure lags (p-value for interaction term for same-day, 3-day mean, 7-day mean, and 21-day mean exposures: 0.57, 0.46, 0.51 and 0.61).
Discussion
Our findings suggest that outdoor air pollution in a region impacted by residential biomass burning has a measurable impact of the microvasculature of school-age children. Specifically, Ox was consistently associated with retinal arteriolar narrowing in single-pollutant models. Our findings also suggest that an important interaction may exist between outdoor concentrations of oxidant gases and PM2.5, as PM2.5 was only associated with arteriolar narrowing when Ox concentrations were elevated. We also found inverse associations between PM2.5 and systolic blood pressure and evidence of effect modification by Ox for the 7-day exposure lag, while in single-pollutant models there were trends towards positive associations between Ox and systolic blood pressure. No clear associations between PM2.5 or Ox and retinal venular diameter or diastolic blood pressure were observed.
Although this study did not conduct any source apportionment of PM2.5, it is known that residential biomass burning affects air quality in this region of Canada. For example, Hong et al.30 developed an algorithm that was applied to 23 communities in British Columbia, Canada, to identify smoky vs. non-smoky days, and classified 30% of days in Courtenay between 2014–2016 as smoky, making it the second smokiest community of the 23 studied. Moreover, Weichenthal et al.22 identified biomass burning as a major contributor to ambient PM2.5 in Courtenay by measuring daily levoglucosan (a tracer of biomass burning) levels from January 2014–March 2015. Furthermore, traffic-related air pollution is very minimal in this region because it is a rural location on an island with a small population size, and there are no major industries in the area that would affect air quality.
The biological mechanisms underlying air pollution impacts on the microcirculation and blood pressure are thought to be related to oxidative stress, inflammation, and disturbances to the autonomic nervous system1,31. Inhaled particles can stimulate the generation of reactive oxygen species causing both pulmonary and systemic oxidative stress and inflammation which contributes to endothelial dysfunction and vasoconstiction1. Arteriolar narrowing may contribute to elevated blood pressure because arterioles are the main regulators of peripheral blood flow and are essential in the maintenance of blood pressure32. In addition, air pollution exposure may lead to an imbalance of the autonomic nervous system which favours sympathetic pathways, and can contribute to endothelial dysfunction, vasoconstriction, and elevated blood pressure1.
In general, existing evidence from observational studies related to the associations between outdoor air pollution and blood pressure in children is inconsistent. For example, Yang et al.33 found that short-term exposure to PM2.5 was associated with very small increases in both systolic and diastolic blood pressure (< 1 mm Hg increase in systolic and diastolic blood pressure per 10 μg/m3 PM2.5) in a large study of approximately 190,000 children in China, but a smaller study in the Netherlands found no clear associations between short-term PM10, NO2 or O3 and systolic or diastolic blood pressure34. In another study in Belgium, consistent positive associations were detected between ultrafine particles and systolic blood pressure in children, but trends of an inverse association was observed for PM2.535. Inverse associations between systolic blood pressure and short-term particulate matter36,37 and ozone38 have also been observed in adult populations. We are not sure why we observed inverse associations between air pollution and systolic blood pressure because our existing knowledge of physiological responses to air pollution generally would support positive associations1; however, these inconsistent findings highlight uncertainty in our current understanding of air pollution impacts on cardiovascular health. In this study, although we found limited evidence of effect modification by Ox for the associations between PM2.5 and blood pressure, it still is possible that complex interactions between air pollutants exist and contribute to the heterogeneity of results observed between studies.
Regarding the retinal microvasculature, previous evidence in adults12,13 and children16 have observed arteriolar narrowing in response to PM2.5 exposure. For example, Provost et al. found that same-day residential outdoor PM2.5 was associated with a 0.62 μm decrease in retinal arteriolar diameter (95% CI − 1.12, − 0.12) per 10 μg/m3 increase in PM2.5 in school-aged children in Belgium16. However, a second study by Luyten et al. found that the direction of associations between PM2.5 and retinal arteriolar diameter in children was sensitive to the exposure lag that was selected17. Results for retinal venular diameter have been less conclusive but tend to suggest positive associations with air pollution16,17. To our knowledge, no studies to date have examined associations between Ox or O3 and retinal blood vessel diameter but Luyten et al.17 investigated the impact of NO2 and did not find any clear associations.
The most interesting finding in our study is the interaction observed between PM2.5 and Ox in models for retinal arteriolar diameter. Specifically, the direction of the association between PM2.5 and arteriolar diameter was modified by concentrations of Ox, with weak positive associations observed at lower concentrations of Ox and inverse associations observed at higher concentrations of Ox. Similarly, the inverse association between Ox and retinal arteriolar diameter was only observed when concentrations of PM2.5 were high. This modifying role of Ox in PM2.5 health effects has been observed previously for other outcomes. For example, Weichenthal et al.6 found stronger associations between PM2.5 and all-cause, cardiovascular, and respiratory mortality when concentrations of Ox were higher, while Lavigne et al.7 observed similar results with short-term PM2.5 and all-cause and cardiovascular mortality. Together, this evidence highlights the importance of considering Ox when evaluating the health impacts of PM2.5 and also suggests possible co-benefits of regulatory interventions aimed at reducing outdoor air pollution (i.e. reducing Ox may also reduce the health impacts of PM2.5 even if PM2.5 mass concentrations remain unchanged).
Existing evidence suggests several possible mechanisms underlying the observed interaction between PM2.5 and Ox. First, elevated ozone depletes antioxidants in the epithelial lining fluid of the respiratory tract39, and this may lower our defenses against reactive oxygen species produced in response to PM2.5 exposure, contributing to greater oxidative stress. In addition, ozone has been shown to increase the permeability of the lung epithelial barrier40,41,42, which may contribute to greater absorption of particles into the systemic circulation and greater health impacts of PM2.5. Lastly, oxidant gases can increase the toxicity of PM2.5 through photochemical aging processes; for example, exposure to ozone has been shown to increase the oxidative potential of particles from both engine exhaust43,44 and biomass burning45.
There are several strengths of this study, including the repeated measures design that eliminates potential confounding by variables that do not change within individuals over a short time period, exposure information for multiple air pollutants, and the study setting that allowed us to evaluate air pollution primarily from residential biomass burning. However, this study also had limitations. Foremost, this study is subject to non-differential, Berkson-type exposure measurement error because true personal PM2.5 or Ox exposures may differ from outdoor concentrations. The result of Berkson measurement error is a reduction in precision without any systematic bias46. Another limitation is we are evaluating short-term changes in retinal blood vessel diameter but how this may impact future health is not clear. We (and others47) hypothesize that repeated short-term damage to microvascular structure can lead to chronic microvascular changes in later life, but there are no longitudinal studies demonstrating this. In addition, there is likely some classical measurement error in estimating arteriolar and venular diameter, but this is almost certainly non-differential with respect to outdoor air pollution concentrations.
Conclusion
In summary, these results suggest that short-term and sub-chronic exposures to air pollution impact the retinal microvasculature and blood pressure of children, and highlight the importance of considering potential interactions between air pollutants when evaluating cardiovascular health impacts. Given the small number of studies that have investigated the impact of outdoor air pollution on the retinal microvasculature or blood pressure in children, additional work is needed to confirm these findings.
Abbreviations
- AIC:
-
Akaike information criterion
- CI:
-
Confidence interval
- CRAE:
-
Central retinal arteriolar equivalent
- CRVE:
-
Central retinal venular equivalent
- CVD:
-
Cardiovascular disease
- DBP:
-
Diastolic blood pressure
- NO2 :
-
Nitrogen dioxide
- O3 :
-
Ozone
- Ox :
-
The combined redox-weighted oxidant capacity of NO2 and O3
- PM2.5 :
-
Fine particulate matter air pollution
- PM10 :
-
Particulate matter < 10 μm
- SD:
-
Standard deviation
- SBP:
-
Systolic blood pressure
References
Brook, R. D. et al. Particulate matter air pollution and cardiovascular disease: An update to the scientific statement from the American heart association. Circulation https://doi.org/10.1161/CIR.0b013e3181dbece1 (2010).
Mustafić, H. et al. Main air pollutants and myocardial infarction: A systematic review and meta-analysis. JAMA J. Am. Med. Assoc. https://doi.org/10.1001/jama.2012.126 (2012).
National Heart Blood and Lung Institute. Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents: Summary Report. (2012). doi:12-7486A
U.S. Environmental Protection Agency. 2020 Final Report: Integrated Science Assessment for Ozone and Related Photochemical Oxidants (EPA/600/R-20/012). (2020).
U.S. Environmental Protection Agency. 2016 Health Criteria Final Report: Integrated Science Assessment for Oxides of Nitrogen (EPA/600/R-15/068). (2016).
Weichenthal, S., Pinault, L. L. & Burnett, R. T. Impact of oxidant gases on the relationship between outdoor fine particulate air pollution and nonaccidental, cardiovascular, and respiratory mortality. Sci. Rep. https://doi.org/10.1038/s41598-017-16770-y (2017).
Lavigne, E., Burnett, R. T. & Weichenthal, S. Association of short-term exposure to fine particulate air pollution and mortality: effect modification by oxidant gases. Sci. Rep. https://doi.org/10.1038/s41598-018-34599-x (2018).
Gdowski, M. A. et al. Association of isolated coronary microvascular dysfunction with mortality and major adverse cardiac events: A systematic review and meta-analysis of aggregate data. J. Am. Heart Assoc. https://doi.org/10.1161/JAHA.119.014954 (2020).
De Boever, P., Louwies, T., Provost, E., Int Panis, L. & Nawrot, T. S. Fundus photography as a convenient tool to study microvascular responses to cardiovascular disease risk factors in epidemiological studies. J. Vis. Exp. https://doi.org/10.3791/51904 (2014).
Patton, N. et al. Retinal vascular image analysis as a potential screening tool for cerebrovascular disease: A rationale based on homology between cerebral and retinal microvasculatures. J. Anat. https://doi.org/10.1111/j.1469-7580.2005.00395.x (2005).
Flammer, J. et al. The eye and the heart. Eur. Heart J. https://doi.org/10.1093/eurheartj/eht023 (2013).
Adar, S. D. et al. Air pollution and the microvasculature: A cross-sectional assessment of in vivo retinal images in the population-based multi-ethnic study of atherosclerosis (MESA). PLoS Med. 7, 2 (2010).
Louwies, T., Panis, L. I., Kicinski, M., De Boever, P. & Nawrot, T. S. Retinal microvascular responses to short-term changes in particulate air pollution in healthy adults. Environ. Health Perspect. 121, 1011–1016 (2013).
Laeremans, M. et al. Short-term effects of physical activity, air pollution and their interaction on the cardiovascular and respiratory system. Environ. Int. https://doi.org/10.1016/j.envint.2018.04.040 (2018).
Louwies, T. et al. Blood pressure changes in association with black carbon exposure in a panel of healthy adults are independent of retinal microcirculation. Environ. Int. 75, 81–86 (2015).
Provost, E. B. et al. Recent versus chronic fine particulate air pollution exposure as determinant of the retinal microvasculature in school children. Environ. Res. 159, 103–110 (2017).
Luyten, L. et al. Children’s microvascular traits and ambient air pollution exposure during pregnancy and early childhood: Prospective evidence to elucidate the developmental origin of particle-induced diseas. BMC Med. 18, 2. https://doi.org/10.1186/s12916-020-01586-x (2020).
Brook, R. D. & Rajagopalan, S. Particulate matter, air pollution, and blood pressure. J. Am. Soc. Hypertens. https://doi.org/10.1016/j.jash.2009.08.005 (2009).
Huang, M. et al. Effects of ambient air pollution on blood pressure among children and adolescents: A systematic review and meta-analysis. J. Am. Heart Assoc. https://doi.org/10.1161/JAHA.120.017734 (2021).
Chen, X. & Wang, Y. Tracking of blood pressure from childhood to adulthood: A systematic review and meta-regression analysis. Circulation https://doi.org/10.1161/CIRCULATIONAHA.107.730366 (2008).
Meng, J. et al. Source contributions to ambient fine particulate matter for Canada. Env. Sci Technol. 3, 10269–10278 (2019).
Weichenthal, S. et al. Biomass burning as a source of ambient fine particulate air pollution and acute myocardial infarction. Epidemiology 28, 329–337 (2017).
United States Environmetnal Protection Agency. List of Designated Reference and Equivalent Methods. Center for Environmental Measurements and Modeling 1–76 (2020). Available at: https://www.epa.gov/sites/production/files/2019-08/documents/designated_reference_and-equivalent_methods.pdf. (Accessed: 5th May 2021)
Weichenthal, S., Lavigne, E., Evans, G., Pollitt, K. & Burnett, R. T. Ambient PM2.5 and risk of emergency room visits for myocardial infarction: Impact of regional PM2.5 oxidative potential: A case-crossover study. Environ Heal. A Glob. Access Sci. Source https://doi.org/10.1186/s12940-016-0129-9 (2016).
Bratsch, S. G. Standard electrode potentials and temperature coefficients in water at 298.15 K. Vol. 18, No.1, 1–21. (1989).
Couper, D. J. et al. Reliability of retinal photography in the assessment of retinal microvascular characteristics: The Atherosclerosis Risk in Communities Study. Am. J. Ophthalmol. https://doi.org/10.1016/S0002-9394(01)01315-0 (2002).
Leung, H. et al. Computer-assisted retinal vessel measurement in an older population: Correlation between right and left eyes. Clin. Exp. Ophthalmol. https://doi.org/10.1046/j.1442-9071.2003.00661.x (2003).
Knudtson, M. D. et al. Revised formulas for summarizing retinal vessel diameters. Curr. Eye Res. https://doi.org/10.1076/ceyr.27.3.143.16049 (2003).
World Health Organization. WHO child growth standards. Available at: https://www.who.int/childgrowth/standards/bmi_for_age/en/.
Hong, K. Y. et al. Systematic identification and prioritization of communities impacted by residential woodsmoke in British Columbia, Canada. Environ. Pollut. 220, 797–806 (2017).
Stapleton, P. A., Minarchick, V. C., Mccawley, M., Knuckles, T. L. & Nurkiewicz, T. R. Xenobiotic particle exposure and microvascular endpoints: A call to arms. Microcirculation https://doi.org/10.1111/j.1549-8719.2011.00137.x (2012).
Pappano, A. J. & Wier, W. G. Chapter 9: The Peripheral Circulation and Its Control. in Cardiovascular Physiology, 11th edition. Mosby Physiology Monograph Series 155–175 (Elsevier Inc., 2019).
Yang, H. et al. Short-term effects of ambient particulate matter on blood pressure among children and adolescents: A cross-sectional study in a city of Yangtze River delta, China. Chemosphere 2, 2. https://doi.org/10.1016/j.chemosphere.2019.124510 (2019).
Bilenko, N. et al. Traffic-related air pollution and noise and children’s blood pressure: Results from the PIAMA birth cohort study. Eur. J. Prev. Cardiol. https://doi.org/10.1177/2047487313505821 (2015).
Pieters, N. et al. Blood pressure and same-day exposure to air pollution at school: Associations with nano-sized to coarse PM in children. Environ. Health Perspect. https://doi.org/10.1289/ehp.1408121 (2015).
Harrabi, I., Rondeau, V., Dartigues, J. F., Tessier, J. F. & Filleul, L. Effects of particulate air pollution on systolic blood pressure: A population-based approach. Environ. Res. https://doi.org/10.1016/j.envres.2006.01.012 (2006).
Brauer, M. et al. Exposure of chronic obstructive pulmonary disease patients to particles: Respiratory and cardiovascular health effects. J. Expo. Anal. Environ. Epidemiol. https://doi.org/10.1038/sj.jea.7500195 (2001).
Hoffmann, B. et al. Opposing effects of particle pollution, ozone, and ambient temperature on arterial blood pressure. Environ. Health Perspect. https://doi.org/10.1289/ehp.1103647 (2012).
Lakey, P. S. J. et al. Chemical exposure-response relationship between air pollutants and reactive oxygen species in the human respiratory tract. Sci. Rep. https://doi.org/10.1038/srep32916 (2016).
Broeckaert, F. et al. Serum Clara cell protein: A sensitive biomaker of increased lung epithelium permeability caused by ambient ozone. Environ. Health Perspect. https://doi.org/10.1289/ehp.00108533 (2000).
Blomberg, A. et al. Clara cell protein as a biomarker for ozone-induced lung injury in humans. Eur. Respir. J. https://doi.org/10.1183/09031936.03.00048203 (2003).
Chitano, P., Hosselet, J. J., Mapp, C. E. & Fabbri, L. M. Effect of oxidant air pollutants on the respiratory system: Insights from experimental animal research. Eur. Respir. J 8, 1357–1371 (1995).
Li, Q., Wyatt, A. & Kamens, R. M. Oxidant generation and toxicity enhancement of aged-diesel exhaust. Atmos. Environ. https://doi.org/10.1016/j.atmosenv.2008.11.018 (2009).
McWhinney, R. D., Gao, S. S., Zhou, S. & Abbatt, J. P. D. Evaluation of the effects of ozone oxidation on redox-cycling activity of two-stroke engine exhaust particles. Environ. Sci. Technol. https://doi.org/10.1021/es102874d (2011).
Wong, J. P. S. et al. Effects of atmospheric processing on the oxidative potential of biomass burning organic aerosols. Environ. Sci. Technol. https://doi.org/10.1021/acs.est.9b01034 (2019).
Armstrong, B. G. Effect of measurement error on epidemiological studies of environmental and occupational exposures. Occup. Environ. Med. https://doi.org/10.1136/oem.55.10.651 (1998).
Zhang, X. et al. Associations between microvascular function and short-term exposure to traffic-related air pollution and particulate matter oxidative potential. Environ. Heal. A Glob. Access Sci. Source 2, 2. https://doi.org/10.1186/s12940-016-0157-5 (2016).
Acknowledgements
We would like to acknowledge Dr. Sarai Racey for her help as a research assistant, John Burch who collected the PM2.5 filters, Health Canada for providing funding for gravimetric analysis and in-kind use of the retinal camera, and the lab technicians at ALS Canada Ltd who conducted the PM2.5 gravimetric analyses. We would also like to thank Nele Gerrits, Sven Vercauteren and Patrick De Boever at MONA-REVA who provided training and feedback on analysing the retinal images. Lastly, we would also like to thank Dr. Charmaine Enns (Ministry of Health, Government of British Columbia), Earl Plaine (Ministry of the Environment, Government of British Columbia), and the participating families and staff from Courtenay Elementary and Cumberland Community School.
Funding
This work was supported by Health Canada, a Canadian Institute for Health Research Foundation Grant, and J.K. is supported by a Fonds de la recherche en sante du Quebec doctoral scholarship.
Author information
Authors and Affiliations
Contributions
J.K. coordinated the study, analyzed the retinal images, performed statistical analyses and wrote the manuscript. K.L.P. and N.G.P. organized the fieldwork and collected all clinical data. R.K. coordinated the collection and analysis of exposure data. S.W. designed the study, obtained funding, oversaw all aspects of data collection and statistical analyses and provided critical revisions of the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Korsiak, J., Perepeluk, KL., Peterson, N.G. et al. Air pollution and retinal vessel diameter and blood pressure in school-aged children in a region impacted by residential biomass burning. Sci Rep 11, 12790 (2021). https://doi.org/10.1038/s41598-021-92269-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-92269-x
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.