Abstract
To elucidate the association between medial meniscus extrusion measured on ultrasonography (MMEUS) and the prevalence of medial meniscus posterior root tear detected on magnetic resonance imaging (MMPRTMRI). We recruited 127 patients (135 knees; 90 females; mean age: 64.4 ± 8.7 years old; mean BMI: 25.5 ± 3.4 kg/m2) in this cross-sectional study. All participants had medial knee pain without a knee trauma or surgery history. Knee osteoarthritis (KOA) severity was evaluated using Kellgren-Lawrence grade (KLG) scores. Patients with KLG scores 0–1 and ≥ 2 were classified in non-radiographic (non-ROA) and radiographic KOA (ROA) groups, respectively. MMEUS was measured with patients in the supine position. Based on fat-suppressed T2-weighted images, MMPRTMRI was defined as the presence of “Ghost meniscus sign” and “Cleft/truncation sign”, indicating an abnormal high signal intensity of a completely disrupted posterior root. MMEUS was compared between MMPRT+ and MMPRT– patients using a non-paired t-test. Receiver operating characteristic (ROC) curves were used to determine the optimal cut-off MMEUS to predict MMPRT+. The prevalence of MMPRT+ was 31.3% (25/80 knees) and 29.1% (16/55 knees) in the non-ROA and ROA groups. The MMEUS of MMPRT+ patients were significantly greater than that of MMPRT– patients in both the non-ROA (5.9 ± 1.4 mm vs. 4.4 ± 1.0 mm, P < 0.001) and ROA (7.8 ± 1.3 mm vs. 6.3 ± 1.3 mm, P < 0.001) groups. ROC curves demonstrated that 5-mm and 7-mm MMEUS were the optimal cut-off values in non-ROA (adjusted odds ratio: 6.280; area under the curve [AUC]: 0.809; P < 0.001) and ROA (adjusted odds ratio: 15.003; AUC: 0.797; P = 0.001) groups. In both early non-radiographic and established radiographic KOA stages, a greater MMEUS was associated with a higher MMPRTMRI prevalence.
Similar content being viewed by others
Introduction
The anterior and posterior meniscal roots are essential structures for anchoring the menisci to the tibial plateau and maintaining the meniscal function of articular cartilage protection. These bony attachments of the menisci allow the circumferential collagen fibers in the meniscal body to disperse axial loads into hoop stresses that redistribute the forces applied to the knee joint during daily activities1,2. Specifically, the posterior root of the medial meniscus is rigidly attached to the tibia, thereby rendering the meniscal body less mobile compared to the other roots. Therefore, the posterior root of the medial meniscus is more vulnerable to not only traumatic damage such as hyperflexion or squatting but also degenerative changes, resulting from a higher incidence of root tears3,4. Medial meniscus posterior root tear (MMPRT), defined as an avulsion injury or radial tear occurring within 10 mm from a bony attachment, has gained the attention of clinicians and surgeons to deal with knee symptom management5,6,7. MMPRT substantially disrupts the ability of medial meniscus to anchor the stretching of circumferential collagen fibers in a radial direction; the medial meniscus radially extrudes toward the outside of the knee joint during the allocation of axial loading force3. Consequently, MMPRT not only alters loading stress distribution to increase peak contact pressure and decrease contact area in the medial compartment of the tibiofemoral joint3,5,8, but also influences joint arthrokinematics by increasing the level of lateral tibial translation and medial compartment excursion9. Intra-articular derangement derived from MMPRT eventually leads to a rapid progression of osteoarthritis (OA) or spontaneous osteonecrosis in the affected knee joint5,10,11,12. More recently, the concept of early knee OA has drawn the interest of clinicians and researchers in the early diagnosis of knee OA to prevent the progression of OA changes13,14. Accordingly, the early diagnosis of MMPRT prior to definitive knee OA development significantly contributes to the improvement of patient quality of life in terms of locomotive function. Due to the lack of highly sensitive or specific history and physical findings3, the use of magnetic resonance imaging (MRI) has been valuable in MMPRT detection based on the presence of a linear defect around the posterior bony insertion of meniscal roots on axial or coronal view15,16,17. Moreover, other important findings are observed on sagittal view, such as the “Ghost meniscus sign”, which indicates the complete absence of an identifiable triangular meniscal body as a high signal replacing the normal dark meniscal signal; a normal meniscus is seen on the immediately adjacent images3,5,15,17,18,19. Nevertheless, MRI has limitations such as increased cost and an increased duration of examination. Therefore, the use of a more convenient alternative examination modality to validate the risk of MMPRT would be helpful in the outpatient room, for instance. Ultrasonography (US) has several advantages over MRI; US provides physicians with an inexpensive, non-invasive, quick, and real-time assessment of the knee joint20,21,22. Several studies have reported that US demonstrates a relatively high sensitivity and specificity in meniscal pathology detection20,23,24. On the other hand, the presence of artifacts which originate from adjacent bone surface makes the examiners have difficulty to detect the inner meniscal margins25. Therefore, the available US data on the direct detection of posterior root rupture in the medial joint space are scarce. Limited previous studies have reported that US could indirectly detect greater medial meniscus extrusion (MME) in a knee joint with MMPRT in the biomechanical26 or clinical setting27. More recent cohort study reported that a knee joint with a greater MME measured by US (MMEUS) had a higher risk of knee OA development or aggravation regardless of MMPRT occurrence22. Thereafter, MMEUS has the potential to indirectly reveal the presence of MMPRT in patients having knee symptoms with a predisposition for knee OA development or aggravation. Unfortunately, it is difficult to validate the sensitivity of MMEUS to indicate the presence of MMPRT due to a lack of previous data. Thus, we aimed to cross-sectionally evaluate how the value of MMEUS can indicate the presence of MMPRT on MRI (MMPRTMRI), dividing the patients who have medial knee joint pain into non-radiographic knee OA and radiographic knee OA. We hypothesized that the greater value of non-weight bearing MMEUS with patients in the supine position would be associated with a higher prevalence of MMPRTMRI.
Methods
Study participants
The current study was approved by the ethical committee of Hirosaki Memorial Hospital (IRB No. 2020-13). Informed consent was obtained from all participants. All methods were performed in accordance with the relevant guidelines and regulations (Declaration of Helsinki). Study participants visited our hospital from December 2019 to December 2020 presenting with medial knee joint pain during daily activities such as walking, climbing and descending stairs, and sitting and standing. During this period, 186 patients visited our outpatient clinic. We excluded the patients without MRI or US data, and those with a history of other rheumatic disease such as rheumatoid arthritis and that of previous knee trauma (i.e., ligament injury or fracture) or surgery. Finally, we recruited 127 patients (135 knees; 90 females; mean age: 64.4 ± 8.7 years old; mean BMI: 25.5 ± 3.4 kg/m2) for the current study.
Weight bearing anteroposterior knee radiographs were acquired with film-focus distance of 100 cm, 68 kV, and 20 mAs. Plain radiographs of the affected knee were taken in an orthostatic position with the knee semi-flexed, corresponding to Rosenberg view. According to the Kellgren-Lawrence grade (KLG)28, single orthopaedic surgeon (DC, 12-year experience) assigned participants to the non-radiographic knee OA (Non-ROA: KLG 0–1) or radiographic knee OA (ROA: KLG 2–4) group. The intra-rater reliability (k) for determining KLG was 0.821 for the right knee and 0.805 for the left knee29.
Ultrasonographic measurement of MME
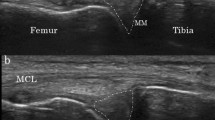
All participants underwent measurement of non-weight bearing MMEUS in the supine position. The ultrasound probe (12 MHz, ARIETTA Prologue, Hitachi Aloka Medical, Tokyo, Japan) was placed at the center of the medial knee joint space, with the knee joint fully extended and in neutral rotation. MMEUS was measured on ultrasonographic image where the medial meniscus was displayed with a hypoechoic band of the medial collateral ligament30 and the downslope of the medial femoral epicondyle (Fig. 1). First, a line was drawn connecting the cortex of both the femur and tibia (Line A); thereafter, a line perpendicular to Line A was drawn from the bottom of Line A to the most medially extruded part of the medial meniscus (Line B, Fig. 1). Finally, the length of Line B was measured as the MMEUS. Regarding the technique used to draw Line A, we ignored the existence of osteophytes and drew Line A through the osteophyte bases to avoid the bony interference of osteophytes for Line B. Additionally, on the femoral side of Line A, this line should trace the femoral cortex at the bottom of the medial femoral epicondyle (Fig. 1). In the outpatient room, single orthopaedic surgeon (DC) acquired US image and measured MMEUS before the patients underwent the plain radiographs of affected knee. Regarding the intra-rater reliability of DC, intraclass correlation coefficient [ICC] (1.1) was 0.977 (95% CI 0.942–0.991)22. Based on total of 18 knee-OA patients, ICC (1.1) was measured by reading the US images twice to wait one-week interval between first and second measurement of MME.
Ultrasonographic evaluation of medial meniscus extrusion. *Osteophyte, **Medial meniscus, ***Medial femoral epicondyle. Line A was drawn to connect the cortex of both the femur and tibia, thereby tracing the femoral cortex at the bottom of the medial femoral epicondyle. Line B was drawn perpendicularly from the bottom of Line A to the most medially extruded part of the medial meniscus. Line A was drawn through the osteophyte bases to avoid the bony interference of osteophytes throughout the length of Line B. Finally, the length of Line B (mm) was measured as the medial meniscus extrusion.
MRI evaluation of medial meniscus tear
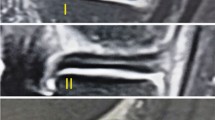
All participants underwent 1.5-T MRI for the affected knee joint (Optima MR360, GE Healthcare). The knee joint was kept immobilized by customized frame during examination with 10° knee flexion and externally rotated at 10–15°. A T2-weighted image with fat-suppressed sequence was used to evaluate MMPRT31,32,33,34,35 with the following imaging sequence: coronal T2 with fat suppression (TR/TE[ms]: 2200/90, field of view: 200 × 200 mm, Matrix 320 × 224, Layer thickness: 4.0 mm, Gap: 1.0 mm) and sagittal T2 with fat suppression (TR/TE[ms]: 2000/32, field of view: 200 × 200 mm, Matrix 320 × 256, Layer thickness: 4.0 mm, Gap: 1.0 mm) Based on the sagittal images, the presence of MMPRT was defined using the ghost meniscus sign, which indicates the complete absence of an identifiable triangular meniscal body as a high signal replacing the normal dark meniscal signal seen on the immediately adjacent images (Fig. 2a)5,17,19. Furthermore, on coronal MRI, cleft/truncation sign (vertical linear defect) was defined as the other reference of MMPRT (Fig. 2b). If the current subjects had both ghost meniscus and cleft/truncation signs, they were defined as having MMPRT. Regarding the diagnostic performance of MMPRT, both ghost meniscus (96.7–100%) and cleft/truncation sign (90–100%) have been reported to demonstrate a high sensitivity16,17. Radiologist in our hospital finally diagnosed the presence of MMPRTMRI, blinded to the clinical information of current subjects. Regarding the other forms of medial meniscus tear, further classification was performed as longitudinal, radial, horizontal, oblique, or complex tear36. Moreover, the severity of meniscal tears was determined by WORMS Score: 0 = intact; 1 = minor radial tear or parrot-beak tear; 2 = non-displaced tear; 3 = displaced tear; 4 = complete maceration/destruction37.
Ghost meniscus sign on a fat-suppressed T2-weighted sagittal image. (a) Sagittal view showing ghost meniscus sign, (b) coronal view showing a defect of the medial meniscus posterior root. An abnormally high signal, indicating the absence of an identifiable meniscal body, is detected in place of the normal dark meniscal signal at the posterior horn of the medial meniscus (arrow).
Statistical analysis
All statistical analyses were conducted using SPSS version 24 (SPSS Inc., Chicago, IL, USA). Continuous variables of demographic data and MMEUS between patients with and without the MMPRTMRI were compared by non-paired t-test. A receiver operating characteristic (ROC) curve was drawn to determine the optimal cut-off to predict the prevalence of the MMPRTMRI in each of non-ROA or ROA group, respectively. Using the optimal cut-off of MMEUS, a logistic regression analysis was conducted with the prevalence of the MMPRTMRI as the dependent variable, and with the optimal cut-off of MMEUS as the independent variable, adjusted for age, sex, and body mass index. A P-value < 0.05 was considered statistically significant.
Results
The prevalence of positive MMPRT (MMPRT+) was 31.3% (25/80 knees) and 29.1% (16/55 knees) in the non-ROA and ROA groups, respectively. The prevalence of MMPRT+ was not significantly different between the groups. In the non-ROA group, the mean age of patients in the MMPRT+ group was significantly higher than that of patients in the negative MMPRT (MMPRT−) group (Table 1). MMEUS in MMPRT+ patients were significantly greater than that in MMPRT– patients in both the non-ROA (5.9 ± 1.4 mm vs. 4.4 ± 1.0 mm, P < 0.001) and the ROA groups (7.8 ± 1.3 mm vs. 6.3 ± 1.3 mm, P < 0.001, Table 1). Regarding the other form of medial meniscus tear, 116 knees (91.3%) had degenerative complex tear pattern including a component with horizontal pattern often communicating with the inferior meniscus surface on at least two image slices38. Twenty-four (20.7%) out of 116 knees having degenerative meniscus tear showed severe meniscal maceration. Only one case had definitive flap tear which was arthroscopically resected. All MMPRT+ patients had the comorbidity of degenerative medial meniscus tear around its central to posterior portion. Ten knees (7.9%) showed no medial meniscus tear.
Overall, the ROC curve demonstrated that the MMEUS value could significantly predict the prevalence of MMPRT+ (AUC: 0.736; 95%CI: 0.647 to 0.824; P < 0.001). In addition, the ROC curve consistently demonstrated that the MMEUS value could significantly predict the prevalence of MMPRT+ in both the non-ROA (AUC: 0.809; 95%CI: 0.710 to 0.907; P < 0.001) and the ROA (AUC: 0.797; 95%CI: 0.669 to 0.925; P = 0.001) group, respectively. Based on the ROC curve, the optimal cut-offs of MMEUS in the non-ROA and ROA groups were 5 mm (Sensitivity: 76.0%; 95%CI: 66.6% to 85.4% and Specificity: 73.6%; 95%CI: 63.9% to 83.3%) and 7 mm (Sensitivity: 81.3%; 95%CI: 71.0% to 91.6% and Specificity: 74.4%; 95%CI: 62.9% to 85.9%), respectively (Fig. 3).
Multiple logistic regression analysis showed that a 5-mm MMEUS was significantly associated with the prevalence of MMPRT+ in the non-ROA group (adjusted odds ratio: 6.280; 95%CI: 1.854 to 21.277; P = 0.003). Similarly, a 7-mm MMEUS was associated with the prevalence of MMPRT+ in the ROA group (adjusted odds ratio: 15.003; 95%CI: 3.923 to 69.205; P = 0.001, Table 2).
Discussion
The most important finding of the current study is that a greater MMEUS was associated with a higher prevalence of MMPRTMRI based on a positive finding of the ghost meniscus and cleft/truncation signs, which corresponds to the complete rupture of the posterior root of the medial meniscus on sagittal and coronal fat-suppressed T2-weighted MRI. Notably, the current finding was consistently significant in patients with medial knee pain both with and without definitive radiographic OA changes defined by the KLG. Moreover, the cut-off value of MMEUS differed according to the stage of radiographic knee OA.
The prevalence of MMPRT in the current study was 31.3% (25/80 knees) and 29.1% (16/55 knees) in the non-ROA and ROA groups. This prevalence of MMPRT was higher than the previous epidemiological data, ranged from 10.1 to 27.8%39,40,41. Interestingly, Bin et al.39 and Hwang et al.41 from Korea reported relatively similar prevalence of MMPRT with the current study. Asian people are more likely to experience MMPRT due to their lifestyle of frequent squatting and sitting on the floor with the legs deeply folded5. A greater MMEUS was consistently associated with a higher prevalence of MMPRTMRI, thereby verifying our study hypothesis. In accordance with the significant loss of meniscal function resulting from MMPRT, some previous cohort studies reported that patients with medial meniscus posterior root injury on MRI42,43 demonstrate a greater MME on the corresponding MRI. In line with these previous cohort study findings, our study findings showed that the use of US is compatible with that of MRI in terms of measuring MME for MMPRT prevalence determination. Furthermore, US is likely to be clinically relevant for the easily validation of the risk of MMPRT in patients with medial knee joint pain in the outpatient clinic.
However, there is insufficient evidence to connect the relationship between MMEUS and the prevalence of MMPRT at this point. A cadaveric biomechanical study reported that the resection of the posterior root of the lateral meniscus affected the degree of MMEUS26. For knees with a total resection of the posterior root, a greater MMEUS was observed in comparison to that of knees with a partial resection. Specifically, when an axial load was applied, MMEUS was significantly greater than when a non-axial load was applied; the latter was simulated as non-weight bearing condition26. Karpinski et al. conducted a study with a similar design to that of the current study to elucidate the relationship between the prevalence of MMPRTMRI and the values of MME measured by both US and MRI27. They observed a greater MME value in participants who had MMPRT in the knee OA population with a relatively early stage of KLG 0–2. This study27 also evaluated the alterations between the weight and non-weight bearing conditions of MMEUS. Interestingly, the results of Karpinski et al. conflicted with those of Rowland et al.26 wherein weight bearing condition did not change the value of MMEUS27. Based on these limited US data, there remains a controversy with regard to the relationship between the value of MMEUS and the prevalence of MMPRT. The biomechanical effect of MMPRT on MMEUS would change in accordance with the severity of cartilage degeneration44,45, lateral or medial meniscus involvement, and weight or non-weight bearing condition. Moreover, to improve inter-rater reliability, future studies should be conducted to determine a consistent method of MMEUS measurements.
The most important limitation of previous US studies26,27 is the small sample size; the reliability of MMEUS was not high enough to determine the prevalence of MMRPT. Thus, the lack of evidence makes it difficult for musculoskeletal healthcare providers to consider the values of MMEUS that validate the prevalence of MMPRT at various stages of knee OA. Based on our study data, with a relatively large sample size, we can progress in the further discussion of applying the optimal cut-off of MMEUS to determine the prevalence of MMPRT. In the current non-radiographic OA population with KLG 0–1, a 5-mm MMEUS is the optimal cut-off to detect MMPRT on fat-suppressed T2-weighted sagittal and coronal MRI. In contrast, a 7-mm MMEUS cut-off is optimal for detecting MMPRT in the definitive radiographic OA population with KLG ≥ 2. Compared to the findings of Karpinski et al., the current cut-off values are greater; notably, the upper error bar of the supine position MMEUS was between 5 and 6 mm in the study by Karpinski et al.27 In other words, further discussion would be needed to conclude which MMEUS value is best to detect the prevalence of MMPRT, and future large-sample studies will shed light on the detailed mechanism of the effect of meniscus root rupture on the deterioration of meniscal function.
Our study had several limitations. First, we could not validate whether the current study participants had grossly visible MMPRT using arthroscopy. Second, the US evaluation was performed only in the supine position with a non-weight bearing condition. Therefore, we did not discuss how the weight bearing condition affects MMEUS based on the current data. Third, the sample size of the advanced knee OA stage (KLG 3–4, N = 20 knees) was relatively small. Finally, the design of the current study was cross-sectional, and therefore we could not establish a cause-effect relationship between MMEUS value and MMPRT development or aggravation. Despite these limitations, the current study emphasizes the clinical relevance of MMEUS in detecting the prevalence of MMPRT by healthcare providers. The use of US can potentially aid in the evaluation of posterior root meniscus rupture in an outpatient room.
Conclusion
The current cross-sectional study elucidated the association between MMEUS and the prevalence of MMPRT. For the patients having medial knee joint pain, a greater MMEUS was associated with a higher prevalence of MMPRT on fat-suppressed T2-weighted MRI. MMEUS ≥ 5 mm can be a risk factor for MMPRT in the patients with non-radiographic knee OA and MMEUS ≥ 7 mm can be a risk factor for MMPRT in the patients with definitive radiographic knee OA.
References
Chung, K. S., Ha, J. K., Ra, H. J., Nam, G. W. & Kim, J. G. Pullout fixation of posterior medial meniscus root tears: Correlation between meniscus extrusion and midterm clinical results. Am. J. Sports Med. 45, 42–49 (2016).
LaPrade, R. F., Matheny, L. M., Moulton, S. G., James, E. W. & Dean, C. S. Posterior meniscal root repairs: outcomes of an anatomic transtibial pull-out technique. Am. J. Sports Med. 45, 884–891 (2017).
Bhatia, S., LaPrade, C. M., Ellman, M. B. & LaPrade, R. F. Meniscal root tears. Am. J. Sports Med. 42, 3016–3030 (2014).
Kodama, Y. et al. Transtibial pullout repair of medial meniscus posterior root tears: effects on the meniscus healing score and ICRS grade among patients with mild osteoarthritis of the knee. Knee Surg. Sports Traumatol. Arthrosc. 29, 3001–3009 (2021).
Petersen, W. et al. Posterior root tear of the medial and lateral meniscus. Arch. Orthop. Trauma Surg. 134, 237–255 (2013).
Chung, K. S., Ha, J. K., Ra, H. J. & Kim, J. G. A meta-analysis of clinical and radiographic outcomes of posterior horn medial meniscus root repairs. Knee Surg. Sports Traumatol. Arthrosc. 24, 1455–1468 (2015).
Chahla, J. & LaPrade, R. F. Meniscal root tears. Arthroscopy 35, 1304–1305 (2019).
Allaire, R., Muriuki, M., Gilbertson, L. & Harner, C. D. Biomechanical consequences of a tear of the posterior root of the medial meniscus. J. Bone Jt. Surg. Am. 90, 1922–1931 (2008).
Marsh, C. A., Martin, D. E., Harner, C. D. & Tashman, S. Effect of posterior horn medial meniscus root tear on in vivo knee kinematics. Orthop. J. Sports Med. 2, 2325967114541220 (2014).
Yamagami, R., Taketomi, S., Inui, H., Tahara, K. & Tanaka, S. The role of medial meniscus posterior root tear and proximal tibial morphology in the development of spontaneous osteonecrosis and osteoarthritis of the knee. Knee 24, 390–395 (2017).
Park, J.-Y., Kim, B. H., Ro, D. H., Lee, M. C. & Han, H.-S. Characteristic location and rapid progression of medial femoral condylar chondral lesions accompanying medial meniscus posterior root tear. Knee 26, 673–678 (2019).
Kamatsuki, Y. et al. Placement of an anatomic tibial tunnel significantly improves the medial meniscus posterior extrusion at 90° of knee flexion following medial meniscus posterior root pullout repair. Knee Surg. Sports Traumatol. Arthrosc. 29, 1025–1034 (2021).
Sasaki, E. et al. Early knee osteoarthritis prevalence is highest among middle-aged adult females with obesity based on new set of diagnostic criteria from a large sample cohort study in the Japanese general population. Knee Surg. Sports Traumatol. Arthrosc. 28, 984–994 (2020).
Luyten, F. P. et al. Toward classification criteria for early osteoarthritis of the knee. Semin. Arthritis Rheum. 47, 457–463 (2018).
Kim, S. B. et al. Medial meniscus root tear refixation: Comparison of clinical, radiologic, and arthroscopic findings with medial meniscectomy. Arthroscopy 27, 346–354 (2011).
Lee, Y. G. et al. Magnetic resonance imaging findings of surgically proven medial meniscus root tear. J. Comput. Assist. Tomogr. 32, 452–457 (2008).
Choi, S.-H., Bae, S., Ji, S. K. & Chang, M. J. The MRI findings of meniscal root tear of the medial meniscus: Emphasis on coronal, sagittal and axial images. Knee Surg. Sports Traumatol. Arthrosc. 20, 2098–2103 (2011).
Lerer, D. B., Umans, H. R., Hu, M. X. & Jones, M. H. The role of meniscal root pathology and radial meniscal tear in medial meniscal extrusion. Skelet. Radiol. 33, 569–574 (2004).
Harper, K. W., Helms, C. A., Lambert, H. S. & Higgins, L. D. Radial meniscal tears: Significance, incidence, and MR appearance. Am. J. Roentgenol. 185, 1429–1434 (2005).
Friedman, L., Finlay, K. & Jurriaans, E. Ultrasound of the knee. Skelet. Radiol. 30, 361–377 (2001).
Razek, A. A. K. A., Fouda, N. S., Elmetwaley, N. & Elbogdady, E. Sonography of the knee joint. J. Ultrasound 12, 53–60 (2009).
Chiba, D. et al. US detection of medial meniscus extrusion can predict the risk of developing radiographic knee osteoarthritis: a 5-year cohort study. Eur. Radiol. 30, 3996–4004 (2020).
Park, G.-Y., Kim, J.-M., Lee, S.-M. & Lee, M. Y. The value of ultrasonography in the detection of meniscal tears diagnosed by magnetic resonance imaging. Am. J. Phys. Med. Rehabil. 87, 14–20 (2008).
Wareluk, P. & Szopinski, K. T. Value of modern sonography in the assessment of meniscal lesions. Eur. J. Radiol. 81, 2366–2369 (2012).
Lee, D. & Bouffard, J. A. Ultrasound of the knee. Eur. J. Ultrasound 14, 57–71 (2001).
Rowland, G., Mar, D., McIff, T. & Nelson, J. Evaluation of meniscal extrusion with posterior root disruption and repair using ultrasound. Knee 23, 627–630 (2016).
Karpinski, K. et al. No dynamic extrusion of the medial meniscus in ultrasound examination in patients with confirmed root tear lesion. Knee Surg. Sports Traumatol. Arthrosc. 27, 3311–3317 (2019).
Kellgren, J. H. & Lawrence, J. S. Radiological assessment of osteo-arthrosis. Ann. Rheum. Dis. 16, 494–502 (1957).
Chiba, D. et al. Low prevalence of knee chondrocalcinosis and its catabolic association with serum matrix metalloproteinase 3: A rural Japanese population study. Int. J. Rheum. Dis. 21, 2011–2018 (2018).
Kawaguchi, K., Enokida, M., Otsuki, R. & Teshima, R. Ultrasonographic evaluation of medial radial displacement of the medial meniscus in knee osteoarthritis. Arthritis Rheum. 64, 173–180 (2012).
Kaplan, D. J. et al. Increased extrusion and ICRS grades at 2-year follow-up following transtibial medial meniscal root repair evaluated by MRI. Knee Surg. Sports Traumatol. Arthrosc. 26, 2826–2834 (2017).
Kaplan, D. J. et al. ICRS scores worsen between 2-year short term and 5-year mid-term follow-up after transtibial medial meniscus root repair despite maintained functional outcomes. Knee Surg. Sports Traumatol. Arthrosc. https://doi.org/10.1007/s00167-021-06747-w (2021).
Umans, H., Morrison, W., DiFelice, G. S., Vaidya, N. & Winalski, C. S. Posterior horn medial meniscal root tear: The prequel. Skelet. Radiol. 43, 775–780 (2014).
Koenig, J. H., Ranawat, A. S., Umans, H. R. & DiFelice, G. S. Meniscal root tears: Diagnosis and treatment. Arthroscopy 25, 1025–1032 (2009).
LaPrade, R. F. et al. Diagnostic accuracy of 3.0 T magnetic resonance imaging for the detection of meniscus posterior root pathology. Knee Surg. Sports Traumatol. Arthrosc. 23, 152–157 (2014).
Jee, W.-H. et al. Meniscal tear configurations: categorization with MR imaging. Am. J. Roentgenol. 180, 93–97 (2003).
Peterfy, C. G. et al. Whole-Organ Magnetic Resonance Imaging Score (WORMS) of the knee in osteoarthritis. Osteoarthr. Cartil. 12, 177–190 (2004).
Beaufils, P. et al. Surgical management of degenerative meniscus lesions: The 2016 ESSKA meniscus consensus. Knee Surg. Sports Traumatol. Arthrosc 25, 335–346 (2017).
Bin, S.-I., Kim, J.-M. & Shin, S.-J. Radial tears of the posterior horn of the medial meniscus. Arthroscopy 20, 373–378 (2004).
Ozkoc, G. et al. Radial tears in the root of the posterior horn of the medial meniscus. Knee Surg. Sports Traumatol. Arthrosc. 16, 849–854 (2008).
Hwang, B.-Y. et al. Risk factors for medial meniscus posterior root tear. Am. J. Sports Med. 40, 1606–1610 (2012).
Choi, C.-J., Choi, Y.-J., Lee, J.-J. & Choi, C.-H. Magnetic resonance imaging evidence of meniscal extrusion in medial meniscus posterior root tear. Arthroscopy 26, 1602–1606 (2010).
Magee, T. MR findings of meniscal extrusion correlated with arthroscopy. J. Magn. Reson. Imaging 28, 466–470 (2008).
Svensson, F. et al. Scrutinizing the cut-off for “pathological” meniscal body extrusion on knee MRI. Eur. Radiol. 29, 2616–2623 (2019).
Aoki, H. et al. Relationship between medial meniscus extrusion and cartilage measurements in the knee by fully automatic three-dimensional MRI analysis. BMC Musculoskelet. Disord. 21, 742 (2020).
Acknowledgements
We would like to thank Editage (https://www.editage.jp) for English language editing.
Author information
Authors and Affiliations
Contributions
D.C. wrote the main manuscript and designed the current study. T.S. approved the current study design and contribute to the data collection. Y.I. revised the main manuscript and approved the current study design.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chiba, D., Sasaki, T. & Ishibashi, Y. Greater medial meniscus extrusion seen on ultrasonography indicates the risk of MRI-detected complete medial meniscus posterior root tear in a Japanese population with knee pain. Sci Rep 12, 4756 (2022). https://doi.org/10.1038/s41598-022-08604-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-08604-3
This article is cited by
-
The Role of Ultrasound in the Diagnosis and Treatment of Meniscal Injuries
Current Reviews in Musculoskeletal Medicine (2024)
-
Risk factors of incomplete healing following medial meniscus posterior root tear repair with gracilis tendon
Scientific Reports (2023)
-
Younger patients, lower BMI, complete meniscus root healing, lower HKA degree and shorter preoperative symptom duration were the independent risk factors correlated with the good correction of MME in patients with repaired MMPRTs
Knee Surgery, Sports Traumatology, Arthroscopy (2023)
-
Ultrasonographic diagnosis of medial meniscus posterior root tear in early knee osteoarthritis: a comparative study
Archives of Orthopaedic and Trauma Surgery (2023)
-
The ultrasound assessment of osteoarthritis: the current status
Skeletal Radiology (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.