Abstract
Study design:
A case–control evaluating seminal citrate in patients with spinal cord injury (SCI).
Objective:
Several studies have shown neurological prostatic dysfunction in patients with SCI, as confirmed by low levels of seminal prostate-specific antigen (PSA), which is used as a parameter of gland activity. However, seminal citrate, produced almost exclusively by the prostate, could also be used as a marker of prostate function. Thus, the objective of this study was to determine whether SCI causes any changes in seminal citrate concentration and to compare the results obtained for patients and healthy men (controls).
Setting:
The study was carried out in Brazil.
Methods:
We studied 30 men with SCI aged on average 37.77±10.04 years and 30 controls aged on average 38.03±10.06 years. Blood and semen samples were collected after 3 days of abstinence from ejaculation. Fifteen minutes after collection, semen was stored in liquid nitrogen and the samples were submitted to 1H nuclear magnetic resonance (1H NMR). Serum was stored at a controlled temperature of −70 to −79 °C and later used for the determination of testosterone, prolactin and total PSA using an AxSYM instrument and Abbott reagents.
Results:
The median concentration of seminal citrate was significantly lower in patients than in controls (521.65 versus 858.30 mg per 100 ml, P<0.001).
Conclusions:
Patients with SCI have a significant reduction of seminal citrate as a consequence of neurological dysfunction of the prostate.
Similar content being viewed by others
Introduction
Men with spinal cord injury (SCI) have neurological dysfunction of the prostate1 and seminal vesicle.2 The lack of autonomic control and prostate dysfunction are not clearly understood, but the low level of seminal prostate-specific antigen (PSA) is secondary to these disorders and reflects the magnitude of the effect of SCI on the prostatic function of these individuals.3 Seminal PSA is secreted by the prostate and minimally secreted by periurethral glands,4 but is decreased in the presence of prostatitis.5 In humans, seminal citrate is also almost exclusively produced by the prostate,6 and can be precisely quantified by semen spectroscopy7 and, in contrast to seminal PSA, has not been properly studied in patients with SCI. However, seminal citrate is believed to be a more reliable marker for the evaluation of prostate function in these patients.
Thus, assuming that, in addition to seminal PSA, other substances of interest for prostate metabolism may be affected in these patients, the objective of this study was to determine whether SCI causes any changes in the concentration of seminal citrate and to compare these values between patients and controls.
Materials and methods
A total of 30 patients and 30 controls were studied. The patients were from the multidisciplinary outpatient clinic for patients with SCI and the controls were from the family planning outpatient clinic of our university hospital. The mean age of patient was 37.77±10.04 years and that of control was 38.03±10.06 years. Patients and controls were matched for age. All participants included in the study declared themselves as white and were classified as such.
The level and the degree of SCI were determined according to the classification of the American Spinal Injury Association (ASIA).8 Five patients had cervical injuries, 24 thoracic injuries and 1 had a lumbar injury. Twenty patients had SCI at T7 or above and ten had SCI below T7. Regarding the ASIA degree of injury, 27 patients were type A (complete), 2 were type C (incomplete) and 1 was type D (incomplete). All patients had suffered SCI more than 6 months before the study. Patients and controls had normal serum prolactin and testosterone. None of the participants had PSA levels or a digital rectal examination, raising a suspicion of cancer of the prostate, nor did they have a history of treatment of acute prostatitis during the last 3 months, of chronic prostatitis or previous prostate surgery. None of them had signs or symptoms compatible with a current urinary infection.
Blood and semen samples were collected from all participants after at least 3 days of abstinence from ejaculation, with blood being always collected immediately before seminal fluid. The controls collected semen by masturbation, whereas 26 patients collected it by electroejaculation, 3 by masturbation and 1 by vibroejaculation. The semen samples of the patients were obtained after full bladder emptying with a no. 12 urethral catheter.
A 2-ml serum aliquot from each participant was stored in a freezer at a controlled temperature of −70 to −79 °C. According to the volume obtained, semen was divided into 0.5-ml aliquots placed in polypropylene tubes and placed into polypropilene bags, sealed and stored in liquid nitrogen 15 min after collection at room temperature. The semen samples were later lyophilized and stored in a freezer until the time for 1H nuclear magnetic resonance (1H NMR).
For citrate quantitation, the lyophilized samples were rehydrated with 1 ml of 5.93 mM 3-trimethylsilylpropionic-2,2,3,3-d, acid salt (TSP) in D2O and then transferred to 5 mm NMR tubes. A citrate calibration curve in D2O was constructed at a concentration range of 20–200 mM citrate in the presence of 5.93 mM TSP. 1H NMR spectra were obtained using a Varian, Mercury plus BB spectrometer (Palo Alto, CA, USA) operating at 300.059 MHz for 1H and equipped with a 5-mm inverse detection probe at 28 °C. The spectra were referenced in relation to internal standard TSP (δ 0.00 ppm). For each sample, 64 free induction decays were collected into 28 450 data points (np), with spectral width (sw) of 3908 Hz and 45° pulses. A relaxation delay (d1) of 10 s between radio frequency pulses was used to allow a complete return to equilibrium magnetization for the metabolites after each pulse. Time-domain data were apodized with 1.0 Hz exponential function (lb) to improve the signal-to-noise ratio before Fourier transformation. For quantification of citrate level, the spectral baselines were corrected and the resonanses from citrate (four each) and the internal standard TSP were integrated. To facilitate comparison with the literature data, citrate levels are reported as mg per 100 ml. For this purpose, the spectroscopy results obtained in mM per liter were converted to mg per 100 ml by multiplying by a conversion factor of 19.21.
Blood samples were tested for testosterone, prolactin and total PSA using microparticle enzyme immunoassay. The analytical system used was from Abbott Laboratórios do Brasil (São Paulo, SP, Brazil), and consisted of the AxSYM System and the AxSYM testosterone, AxSYM prolactin and AxSYM total PSA reagents.
Data are reported as mean±s.d., median and range. The groups were compared by the Mann–Whitney or Kruskal–Wallis test,9 and multiple comparisons were carried out by the Dunn test.10 Spearman's correlation was used to determine the correlation between time since SCI and seminal citrate level.9 Data were analyzed statistically using the SAS software version 8.2 (SAS Institute Inc, Cary, NC, USA). The results were considered to be statistically significant when P⩽0.05.
The study was approved by the Bioethics Committee of the Universidade Estadual de Londrina and all volunteers gave written informed consent to participate.
Results
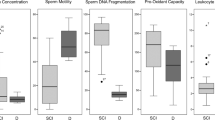
Mean seminal citrate levels were 559.59±359.71 mg per 100 ml (range: 0.0–1369.67, median: 521.65) for patients and 830.06±248.85 mg per 100 ml (range: 408.98–1363.33, median: 858.30) for the controls, with a significant difference (P<0.001) between groups (Figure 1). This lower citrate concentration in patients was observed regardless of whether the injury was at T7 or above or below T7 (P<0.05). Time since the accident ranged from 0.6 to 23.5 years and was not significantly correlated with seminal citrate (P=0.333).
Discussion
Animal studies have shown that SCI causes atrophy of the prostate,11 although sympathectomy reduces the DNA and the proteins on the atrophied side of the gland.12 In humans, the severity of paralysis is associated with a low prostate weight13 and the neurological prostatic dysfunction caused by SCI can be confirmed by a marked fall in seminal PSA.1, 3 Nevertheless, there are also reports showing that prostatitis can contribute to a reduction of seminal PSA,5 although there are no studies showing that this may occur with citrate. As human seminal citrate is almost exclusively produced by the prostate,6 it may be a reliable marker of prostatic secretory activity in patients with SCI. On this basis, this study was carried out to compare seminal citrate between patients with SCI and controls.
In this study, the seminal citrate levels of the patients were significantly lower than control (P<0.001), regardless of the level or time of injury or of patient age. The lower seminal citrate levels of these patients may have been the result of atrophy and lack of neurological control of the prostate, which affect the concentration of this marker.
A recent study in which seminal citrate was determined by 1H NMR established mean citrate levels of 2539.56 mg per 100 ml for individuals without cancer of the prostate aged on average 59 years.14 However, Dondero et al.,15 using a colorimetric methodology, found citrate values of 510 mg per 100 ml (range: 180–835) In this study we obtained a mean value of citrate of 830.06 mg per 100 ml for controls aged on average 38.03 years. This finding may possibly be explained by the fact that older men have prostates of larger volume. In this respect, Kurhanewic et al.16 detected higher tissue citrate levels in prostates with benign hyperplasia.
In this study, lower seminal citrate levels were detected in patients, a finding that may be explained by several possibilities. Most patients had severe paralysis, with ASIA A, a fact that, according to Frisbie et al.,13 might induce a more marked degree of prostate atrophy. In animals, the loss of neurological control of the prostate causes atrophy, with a reduction of gland weight and a reduction of DNA and of protein content in its cells.12 By extrapolating this situation to humans with SCI, we may propose that there may be dysfunction of the mitochondrial system due to the lack of mitochondrial DNA itself. Another explanation is that the neuroendocrine cells of the prostate, which are related to prostate growth and hyperplasia,17 would be less affected by stimuli from the autonomic nervous system because of the lack of neurologic control caused by SCI. Thus, it is possible that all of these factors contribute to the atrophy and lack of neurological control of the prostate, with reduced citrate production and consequent decreased citrate concentration in the seminal fluid.
The production and secretion of citrate by prostatic epithelial cells is regulated by testosterone and prolactin.18 Patients with cervical SCI have a significant fall in testosterone during the first 2 months after injury, with a return to normal levels up to 9 months after the injury.19 In this study, the 5 patients with cervical SCI also had a time of injury of >8 years. These hormones were normal in all the participants studied, ruling out the possibility of a reduction of seminal citrate due to to hormonal disorders. Among the two groups, only five patients had a PSA level slightly above 2.5 ng ml–1, and after a new collection only two of them continued to have levels above this value. Treatment with ciprofloxacin for 3 weeks caused a reduction of PSA in these patients.
In this study, seminal spectroscopy did not detect citrate in three patients, whereas four paradoxically presented concentrations above 1000 mg per 100 ml, values that were much higher than the mean of 559.59 mg per 100 ml. The same methodology was used for all participants and the spectroscopy tests were repeated and confirmed. Perhaps studies correlating prostatic volume with citrate levels may better explain these findings.
The severity of paralysis is related to SCI at T10 or above, and ASIA A, B or C and, the greater the severity of paralysis, the greater the degree of prostatic atrophy.13 In this study, 27 patients had ASIA A, with injuries at T10 or above, and therefore had severe paralysis according to this concept. Although in this study citrate levels were low regardless of the level and time of injury, we may perhaps infer that the severity of paralysis contributed to the low seminal citrate levels. However, what could we say about the four patients with high seminal citrate concentrations with severe paralysis. Frisbie et al.13 detected different degrees of prostatic atrophy and different prostate sizes in patients with severe paralysis.
We believe that the neurological dysfunction of the prostate is related to some factors, such as degree of prostatic atrophy, interrupted control of neuroendocrine cells, low testosterone levels during the first months of SCI and individual susceptibility. Thus, we think that the impact caused by SCI may lead to neurological dysfunction of the prostate of different magnitude among patients. To better elucidate this question, parameters such as seminal PSA and seminal citrate could be evaluated in patients with different degrees of severity of paralysis and correlated with the results of transrectal ultrasonopgraphy of the prostate.
Neoplastic epithelial cells of the prostate lose the ability to produce and secrete citrate, with a consequent intracellular depletion of this marker.20 The use of prostate spectroscopy by NMR with a rectal bobbin has been well documented in the literature for the detection of cancer of the prostate by identification of tissue areas with low citrate levels.16 Kline et al.14 showed that seminal citrate determined by NMR spectroscopy is significantly reduced in patients with prostate cancer and indicated it as a new marker for the detection of this cancer, with greater accuracy compared with PSA. Thus, if indeed seminal citrate should be used as a marker of prostate cancer in the future, it is important to remember that patients with SCI may have lower seminal citrate levels than healthy men.
Conclusions
Patients with SCI have a significant reduction in seminal citrate level in comparison to healthy controls.
References
Lynne CM, Aballa TC, Wang TJ, Rittenhouse HG, Ferrell SM, Brackett NL . Serum and semen prostate specific antigen concentrations are different in young spinal cord injured men compared to normal controls. J Urol 1999; 162: 89–91.
Green JT, Aballa TC, Lynne CM, Brackett NL . Seminal fructose is decreased in ejaculates from men with spinal cord injury. Fertil Steril 1998; 70 (Suppl 1): 200s.
Alexandrino AP, Rodrigues MAF, Matsuo T . Evaluation of serum and seminal levels of prostate specific antigen in men with spinal cord injury. J Urol 2004; 171: 2230–2232.
Iwakiri J, Grandbois K, Wehner N, Graves HC, Stamey T . An analysis of urinary prostate specific antigen before and after radical prostatectomy: evidence for secretion of prostate specific antigen by the periurethral glands. J Urol 1993; 149: 783–786.
Shortliffe LMD, Sellers RG, Schachter J . The characterization of nonbacterial prostatites: search for an etiology. J Urol 1992; 148: 1461–1466.
Mann T . Fructose, polyols, and organic acids. In: Mann T (ed). The Biochemistry of Semen and of the Male Reproductive Tract. Methuen: London, 1964, pp 237–264.
Tomlins AM, Foxall PJD, Lynch MJ, Parkinson J, Everett JR, Nicholson JK . High resolution H NMR spectroscopic studies on dynamic biochemical processes in incubated human seminal fluid samples. Biochim Biophys Acta 1998; 1379: 367–380.
Maynard Jr FM, Bracken MB, Creasey G, Ditunno Jr JF, Donovan WH, Ducker TB et al. International standard for neurological and functional classification of spinal cord injury. Spinal Cord 1997; 35: 266–274.
Daniel WW . Biostatistics: a Foundation for Analysis in the Health Sciences, 2nd edn. John Wiley: New York, NY, 1995.
Dunn OJ . Multiple comparisons using rank sums. Technometrics 1964; 6: 241–252.
Huang HF, Li MT, Linsenmeyer TA, OttenWeller JE, Pogach L M, Irwin RJ . The effects of spinal cord injury on status of messenger ribonucleic acid for TRPM 2 and androgen receptor in the prostate of rat. J Androl 1997; 18: 250–256.
Mcvary RT, Razzaq A, Lee C, Venegas MF, Rademaker A, Mckenna KE . Growth of the rat prostate gland is facilitated by the autonomic nervous system. Biol Reprod 1994; 51: 99–104.
Frisbie JH, Kumar S, Aguilera EJ, Yalla S . prostate atrophy and spinal cord lesions. Spinal Cord 2006; 44: 24–27.
Kline EE, Treat EG, Averna TA, Davis MS, Smith AY, Sillerud LO . Citrate concentrations in human seminal fluid and expressed prostatic fluid determined via 1H nuclear magnetic resonance spectroscopy outperform prostate specific antigen in prostate cancer detection. J Urol 2006; 176: 2274–2279.
Dondero F, Sciarra F, Isidori A . Evaluation of relationship between plasma testosterone and human seminal citric acid. Fertil Steril 1972; 23: 168–171.
Kurhanewicz J, Vigneron DB, Nelson SJ, Hricak H, Macdonald JM, Konety B et al. Citrate as an in vivo marker to discriminate prostate cancer from benign prostatic hyperplasia and normal prostate peripheral zone: detection via localized proton spectroscopy. Urology 1995; 45: 459–466.
Abrahamsson PA, Wadstrrom LB, Alumets J, Falkmer S, Grimelius L . Peptide-hormone and serotonin-immunoreactive cells in normal and hyperplastic prostate glands. Pathol Res Pract 1986; 181: 675–683.
Costello LC, Franklin RB . Concepts of citrate production and secretion by prostate: 2 hormonal relationships in normal and neoplastic prostate. Prostate 1991; 19: 181–205.
Claus-walker J, Scurry M, Carter RE, Campos RJ . Steady state hormonal secretion in traumatic quadriplegia. J Clin Endocrinol Metab 1977; 44: 530–535.
Costello LC, Franklin RB . The clinical relevance of the metabolism of prostate cancer; zinc and tumor suppression: connecting the dots. Mol Cancer, [serial online] 2006 May [cited 5 November 2006] 5: 5–17. Available from: URL: http://www.molecular-cancer.com/content/pdf:1476-4598-5-17.pdf.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Alexandrino, A., Rodrigues, M., Matsuo, T. et al. Evaluation of seminal citrate level by 1H nuclear magnetic resonance spectroscopy in men with spinal cord injury. Spinal Cord 47, 878–881 (2009). https://doi.org/10.1038/sc.2009.62
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2009.62
Keywords
This article is cited by
-
Identification of biochemical differences between different forms of male infertility by nuclear magnetic resonance (NMR) spectroscopy
Journal of Assisted Reproduction and Genetics (2014)