Abstract
Study design:
Case series from a prospectively acquired database and phone survey.
Objectives:
To assess the efficacy of upper limb reanimation (ULR) protocols on acquisition of intermittent self-catheterization (ISC) in C5–C7 ASIA tetraplegic patients.
Setting:
University Hospital, Paris, France.
Methods:
A prospectively acquired database of 152 tetraplegic patients followed in ULR consultation between 1997 and 2008 in a rehabilitation unit was studied. A total of 20 patients met the inclusion criteria, which mainly were traumatic C5–C7 tetraplegic adult patients who were unable to perform ISC, and who benefited from ULR with the objectives of improving hand abilities and of ISC acquisition, through urethral orifice for males or via a continent urinary stoma for females. The main outcome measure was ISC acquisition (ISC+) proportion. Population characteristics and secondary outcome measures: ISC+/ISC− patients were compared regarding epidemiological and surgical data, key-grip strength, patient global improvement score, activities of daily living and quality of life (PGI-I, Wuolle questionnaire, verbal rating scale).
Results:
ISC+ was 75%. It depended on key-grip strength (P<0.05) and led to a statistically significant improvement of urinary status compared with ISC− patients (P<0.01). ULR improved patients’ abilities and QoL in both ISC+ and ISC− patients.
Conclusion:
ULR protocols allow ISC in most C5–C7 tetraplegic patients. Multidisciplinary care with surgeons and PRM physicians improves patients’ vital and functional prognosis by changing their urological-management method.
Similar content being viewed by others
Introduction
Spinal cord injuries lead to motor and urinary impairments, with functional and vital prognosis. Urological complications, in relation to detrusor hyperactivity and detrusor-sphincter dyssynergia, are the first causes of morbidity and mortality in this population,1 and the priority of management self-reported by the patients.2 The aims of urological management include improvements in continence and prevention of kidney complications. Intermittent self-catheterization (ISC) introduced by Lapides et al.3 in 1972, combined with detrusor hyperactivity treatment, enables patients to achieve these two goals.4, 5 Among patients with spinal cord injuries, those with tetraplegia have several deficiencies that limit their ability to perform ISC. This task depends mainly on the ability to use the hand and on the independent access to the urethral meatus while in a wheelchair, especially for female patients. The problem of urethral access can be resolved by formation of a continent urinary stoma (CUS) (or diversion) through various surgical techniques, which are performed after an ISC simulation test in rehabilitation units.6, 7
Studies have shown that C6 ASIA injury level is the highest level to enable ISC, but in a very low proportion of patients. The overall success for ISC ranges from 20 to 30% in the whole tetraplegic population.8 In contrast, the majority of C8 level patients can perform ISC with active pinch and grasp holds.9 Hand function can be improved by upper limb reanimation (ULR) protocols consisting of reconstructive surgery10, 11 (tendon transfers, tenodeses and arthrodeses) combined with specific rehabilitation procedures (tasked motor training, biofeedback and new muscle-function integration).12 These protocols improve hand abilities, activities of daily living (ADL) and quality of life (QoL).13, 14
To our knowledge, the contribution of ULR to the acquisition of ISC has not been specifically addressed in the literature in traumatic tetraplegics.9, 15 The objective of our study was to assess the efficacy of ULR protocols on acquisition of ISC in tetraplegic C5–C7 ASIA patients.
Materials and methods
Design
Monocentric case series using a prospectively acquired patient file database and phone surveys.
Participants and inclusion criteria
The study population consisted of 152 patients with tetraplegia seen for ULR visit between 1997 and 2008 in a physical and rehabilitation medicine unit at a university hospital.
Strict inclusion criteria were defined: traumatic tetraplegic adult patients, later than 1 year after injury, with ASIA16 level from C5 to C7, Giens17 level from 1 to 7 (for example, starting level for ULR but without active pinch or grasp holds), unable to manage fully-independent ISC. This was verified by physiatrists and occupational therapists during pre-surgical ecological assessments through urethral orifice for males or via CUS simulation testing using a phantom mimicking stoma orifice on the abdominal wall for females.18 ULR procedures were systematically performed before CUS surgery, which consisted of Monti or Mitrofanoff derivations associated with augmentation ileo-cystoplasty.7 Pre-surgical ULR clinical visit was composed of standardized assessments and time for education and questions. Patient objectives for ULR procedure consisted of improvement in hand function and ISC acquisition through the native urethra for males and via CUS for females. Patients needed to benefit from at least one hand reanimation surgery to be included, and patients undergoing elbow reanimation only were excluded.
Evaluation criteria
The main outcome measure was independent ISC acquisition proportion. ‘Independent ISC’ criteria were assessed through patient files and phone surveys to ensure accuracy. We analysed the relationship of this main outcome measure with population characteristics such as gender, age, ASIA and Giens level, post-traumatic delay at the end of the programme, follow-up duration, upper limb surgical procedures, CUS-associated surgery, surgical morbidity, total hospitalization duration, and with secondary outcomes including key-grip strength, time taken for ISC, impression of improvement or change (Patient Global Impression of Improvement (PGI-I), Patient Clinical Global Impression of Change in Physical Frailty (PGIC-PF)), patient's global satisfaction and QoL (Wuolle questionnaire, verbal rating scale).
All file data were recorded during the initial assessment visit, hospitalization and follow-up visit. Key-grip strength for each hand was assessed on average 6 months after the last surgery, using three measures of the ‘Pinch dynamometer-Jauge de pincement’ (Kinetec, Charleville-Mezieres, France). The maximum value was recorded. Phone survey data were recorded between January and March 2009 with a single telephone call to each patient. Time taken for ISC was self-reported by patients.
The PGI-I 19 and PGIC-PF20 exact question was ‘Check the one number that best describes how your urinary tract condition (or hand abilities for PGIC-PF) is now, compared with how it was before treatment.’ The PGI-I scale ranges from 1 (‘very much better’) to 7 (‘very much worse’). The PGIC-PF scale ranges from −7 (‘a very great deal worse’) to 7 (‘a very great deal better’). The Wuolle questionnaire 14 consists of several questions with binary (yes/no) responses about ADL (‘I can perform more activities’), QoL (‘The surgery has improved the quality of my life’) and global satisfaction (‘I would have the surgery again’). When a positive response to the QoL question was received, a QoL verbal rating scale was used: ‘What is the percentage of improvement of your QoL, from 1 to 100, since ULR?’
Statistical analysis
Statistical analyses were conducted by the Clinical Investigation and Technological Innovation Center. Means and s.d.'s were calculated for each variable. Qualitative data from the two groups (ISC+ and ISC−) were compared with a Fisher's exact test, and P<0.05 was considered statistically significant. Continuous (strength) and discrete (patient global improvement score, verbal rating scale) data were compared using a Wilcoxon test (with P<0.05 considered statistically significant). The statistical analyses software used was R statistical programming language (2.9.2 version), R foundation (Vienna, Austria).
Approval by an institutional human research review board was not relevant in this current care study.
Results
From 152 patients on file, 20 met the inclusion criteria.
Primary outcome measure
Patients who independently acquired ISC were labelled ISC+ and consisted of 75% (n=15) of the study group. Mean ISC duration was 8.7±5 min. The mean number of ISC procedures per day was 4.8±0.5. The remaining patients were labelled ISC−; those unable to perform ISC (n=2) were categorized ‘ISC− primary failure’, and patients for whom ISC was possible but not used (n=3) were categorized ‘ISC− secondary failure’.
Statistically significant secondary outcome measures: key-grip strength and PGI-I
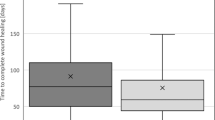
Post-ULR key-grip strength was statistically different between ISC+ and ISC− groups (17.7 N versus 10.1 N, P<0.05, Figure 1).
ISC+ patients had improved urinary status compared with ISC− patients, which was statistically significant (P<0.01, Figure 2).
Population characteristics and other secondary outcome measures
All files were complete for the 20 study subjects, except for the phone survey, which was available for 90% of patients (18/20 cases). One patient died 4 years after the end of the ULR protocol from a pulmonary embolism and another patient was lost to follow-up 1 year after the end of the ULR program.
Mean age±s.d. at the end of the program was 35±7. The patient ASIA levels were as follows: C5 (n=2), C6 (n=15) and C7 (n=3). The main characteristics of this patient population are shown in Table 1. Main surgical data are shown in Table 2. Cases of ULR morbidity consisted of infection (abscess, one case) and mechanical failure of tendon transfer (four cases): suture distension (three cases), and elbow flessum (one case). All cases were revised successfully except one mechanical failure. There was one case of CUS morbidity that consisted of stoma orifice stenosis, which was later revised with success. The average delay between the end of ULR procedure and CUS was 31 months±30 months (range 8–52).
Despite a 100% ISC+ proportion for C7 patients (n=3) and for those with CUS (female) (n=4), no statistically significant differences were seen for all other secondary outcome variables except key-grip strength and PGI-I between the two groups (ISC+/ISC−).
Activities of daily living, QoL and global satisfaction assessed by phone survey are shown in Table 3.
Discussion
Study limitations
The primary limitation of this study is that there is currently no simple, validated and specific functional assessment scale to measure the outcome after ULR. Some are simple but lack satisfactory metrological properties; others are too long to be used frequently or lack urinary activities assessment. A phone survey was thus added to the prospective-reviewed data in order to assess urinary management and global satisfaction.
Another limitation of this study was the small sample size. As only 20 patients were included, the conclusions drawn here cannot be extrapolated to the general spinal cord injury population. On the other hand, strict inclusion criteria were chosen in order to obtain accurate results, which led to this small sample.
ISC acquisition: possible predictive factors
The study of the reasons for success or failure showed that several factors seemed to be relevant.
Giens level. It was a clinically relevant variable that nearly achieved statistical significance (P=0.07). Furthermore, it represented the first parameter to determine the feasibility of active reanimation, leading to high key-grip strength.
Key-grip strength. Other authors have already found that patients need a strong key grip to perform ISC themselves.15 We have found a statistical difference between the two groups for this outcome measure. None of the ‘ISC– primary failure’ patients could reach a key-grip value after an ULR of 0.5 kg (mean value being 0.28 kg), whereas 0.5 kg was the lowest score achieved in the ISC+ group (mean 1.8 kg). The positive predictive value of this parameter (key grip ⩾0.5 kg) for ISC+ status was 86% in this study. This could be the threshold to enable independent ISC, but it has to be confirmed by appropriate studies.
Bilateral/unilateral ULR. Bilateral ULR could be another predictive factor for ISC status. That confirms the results of Hashizume:15 the eight ISC+ patients in this study had undergone bilateral ULR. In our study, most of the ISC+ patients had undergone bilateral ULR, whereas the two ISC– ‘primary failure’ patients had had unilateral surgery. Here also, sample size was insufficient to achieve statistical difference.
Motivation, pre-existent urological-management method and propitious family. ISC failure could be explained either by medical complications (n=2, one surgical complication and revision failure and one myasthenia after ULR) or by motivational difficulties (n=3). Lack of motivation applied either for the pursuit of a long rehabilitation program or for performing ISC. Beyond self-motivation, two other well-known parameters seemed to determine failure for these three patients: the first was the existence of a safe and comfortable urological-management method before ULR (for example: non-continent urethral stenting or Bricker stoma), with high bladder pressure control and no kidney complications. If continence was no priority, the constraints of ISC could have explained the choice of these alternative techniques. The second one was the presence of an available and compliant family and/or attendant to perform assisted intermittent catheterization, which led to ISC advantages (continence and kidney preservation) without its manipulation constraints, but induced dependence. Patients’ motivation and its relation to ISC acquisition were not assessed, but it could have been a main predictive criterion of success.
CUS-associated surgery. Despite a 100% success (n=4), the sample size and the initial choice to perform CUS only on females probably limited the statistical significance. This technique allows ISC for people with high-level injuries through an easier access to the urethral meatus, which releases one hand from the perineum (the one spotting the meatus and spreading the labia for females or holding the penis for males) and allows bimanual holds to handle the material and catheterize the urethra. If the simulation test is positive, this surgery could be the priority solution for female patients who cannot catheterize through the urethra in a wheelchair and for whom the main objective is ISC, rather than improvement of global hand abilities through a long surgical program, and an alternative surgery for male patients with ULR failure.
The evaluation of predictive values for all these negative or positive parameters for ISC could be an interesting goal for an appropriate prospective study.
Conclusion
ULR protocols allow ISC acquisition for most of the C5–C7 tetraplegic patients, with a significant improvement in urinary status. Effective use of independent ISC after ULR depends mainly on hand abilities, especially key-grip strength. Multidisciplinary care with surgeons and PRM physicians leads to an improvement in vital and functional prognosis in these patients by changing their urological-management method. Even when ISC acquisition fails, ULR improves hand impairments and consequently the activity and participation of this severely disabled population.
References
Cardenas DD, Hoffman JM, Kirshblum S, McKinley W . Etiology and incidence of rehospitalization after traumatic spinal cord injury: a multicenter analysis. Arch Phys Med Rehabil 2004; 85: 1757–1763.
Snoek GJ, Ijzerman MJ, Hermens HJ, Maxwell D, Biering-Sorensen F . Survey of the needs of patients with spinal cord injury: impact and priority for improvement in hand function in tetraplegics. Spinal Cord 2004; 42: 526–532.
Lapides J, Diokno AC, Silber SJ, Lowe BS . Clean, intermittent self-catheterization in the treatment of urinary tract disease. J Urol 1972; 107: 458–461.
Weld KJ, Dmochowski RR . Effect of bladder management on urological complications in spinal cord injured patients. J Urol 2000; 163: 768–772.
Killorin W, Gray M, Bennett JK, Green BG . The value of urodynamics and bladder management in predicting upper urinary tract complications in male spinal cord injury patients. Paraplegia 1992; 30: 437–441.
Zommick JN, Simoneau AR, Skinner DG, Ginsberg DA . Continent lower urinary tract reconstruction in the cervical spinal cord injured population. J Urol 2003; 169: 2184–2187.
Karsenty G, Chartier-Kastler E, Mozer P, Even-Schneider A, Denys P, Richard F . A novel technique to achieve cutaneous continent urinary diversion in spinal cord-injured patients unable to catheterize through native urethra. Spinal Cord 2008; 46: 305–310.
Asayama K, Kihara K, Shidoh T, Shigaki M, Ikeda T . The functional limitations of tetraplegic hands for intermittent clean self-catheterisation. Paraplegia 1995; 33: 30–33.
Kiyono Y, Hashizume C, Ohtsuka K, Igawa Y . Improvement of urological-management abilities in individuals with tetraplegia by reconstructive hand surgery. Spinal Cord 2000; 38: 541–545.
Moberg E . Surgical treatment for absent single-hand grip and elbow extension in quadriplegia. Principles and preliminary experience. J Bone Joint Surg Am 1975; 57: 196–206.
Revol M, Cormerais A, Laffont I, Pedelucq JP, Dizien O, Servant JM . Tendon transfers as applied to tetraplegia. Hand Clin 2002; 18: 423–439.
Vaynman S, Gomez-Pinilla F . License to run: exercise impacts functional plasticity in the intact and injured central nervous system by using neurotrophins. Neurorehabil Neural Repair 2005; 19: 283–295.
Mohammed KD, Rothwell AG, Sinclair SW, Willems SM, Bean AR . Upper-limb surgery for tetraplegia. J Bone Joint Surg Br 1992; 74: 873–879.
Wuolle KS, Bryden AM, Peckham PH, Murray PK, Keith M . Satisfaction with upper-extremity surgery in individuals with tetraplegia. Arch Phys Med Rehabil 2003; 84: 1145–1149.
Hashizume C, Fukui J . Improvement of upper limb function with respect to urination techniques in quadriplegia. Paraplegia 1994; 32: 354–357.
Maynard Jr FM, Bracken MB, Creasey G, Ditunno Jr JF, Donovan WH, Ducker TB et al. International Standards for Neurological and Functional Classification of Spinal Cord Injury. American Spinal Injury Association. Spinal Cord 1997; 35: 266–274.
McDowell CL, Moberg EA, Smith AG . International conference on surgical rehabilitation of the upper limb in tetraplegia. J Hand Surg Am 1979; 4: 387–390.
Boirel E, Vaultier S . Experience of an evaluation tool in occupational therapy for the choice of an urinary diversion. Ergotherapies 2008; 29: 57–64.
Yalcin I, Bump RC . Validation of two global impression questionnaires for incontinence. Am J Obstet Gynecol 2003; 189: 98–101.
Studenski S, Hayes RP, Leibowitz RQ, Bode R, Lavery L, Walston J et al. Clinical Global Impression of Change in Physical Frailty: development of a measure based on clinical judgment. J Am Geriatr Soc 2004; 52: 1560–1566.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Bernuz, B., Guinet, A., Rech, C. et al. Self-catheterization acquisition after hand reanimation protocols in C5–C7 tetraplegic patients. Spinal Cord 49, 313–317 (2011). https://doi.org/10.1038/sc.2010.120
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2010.120
Keywords
This article is cited by
-
How many spinal cord injury patients can catheterize their own bladder? The epidemiology of upper extremity function as it affects bladder management
Spinal Cord (2016)
-
Clean Intermittent Catheterization in the Elderly
Current Bladder Dysfunction Reports (2015)
-
Intermittent self-catheterization in tetraplegic patients: a 6-year experience gained in the spinal cord unit in Prague
Spinal Cord (2014)