Abstract
Objectives:
To evaluate follow-up treatments used after treatment of detrusor–sphincter dyssynergia (DSD) by a temporary urethral sphincter stent.
Materials and methods:
Between February 1994 and June 2003, 147 men with a mean age of 41.3±14.4 years were treated by temporary urethral stent inserted across the external sphincter for DSD. The underlying neurologic disease was quadriplegia in 85 cases, multiple sclerosis in 24 cases and paraplegia in 21 cases. A Nissenkorn (Bard) stent was used in 130 cases and a Diabolo (Porgès) stent was used in 17 cases. All patients were either unable to or they refused to perform intermittent self-catheterization. DSD was demonstrated by urodynamic studies in every case.
Results:
The mean duration of temporary stenting was 10.15±16.07 months. After temporary stenting, 92 patients were treated by permanent stent (Ultraflex, Boston Scientifics), 7 started intermittent self-catheterization, 12 had repeated changes of the temporary stent, 4 had an indwelling catheter, 3 underwent cystectomy with non-continent diversion, 2 were treated by endoscopic sphincterotomy, 1 was treated by bladder neck incision, 1 was treated by neuromodulation and 1 was treated by cystostomy. Fifteen patients were lost to follow-up. Two patients died during follow-up (not related to DSD).
Conclusion:
After treatment of DSD by a temporary urethral sphincter stent, 70.7% of patients subsequently require a permanent urethral sphincter stent. This period allows selection of patients unlikely to benefit from permanent urethral sphincter stent.
Similar content being viewed by others
Introduction
Traumatic, inflammatory, neoplastic, vascular or congenital suprasacral spinal cord lesions are responsible for voiding disorders due to detrusor overactivity and detrusor–sphincter dyssynergia (DSD).1, 2, 3 The functional obstruction induced by these disorders results in a high-pressure system that can be responsible for genitourinary tract complications.4 In this setting, the best voiding method consists of pharmacologically controlling the overactive bladder combined with clean intermittent catheterization.5 However, some patients are unable to or they refuse to perform intermittent catheterization. A voiding method allowing low-pressure bladder emptying as complete as possible should be proposed for these patients. The only alternative is to lower resistance distal to the bladder, that is, external urethral sphincter resistance. As bladder emptying is usually a reflex mechanism in this setting, this technique requires the use of a urine collection device and can therefore only be envisaged in men fitted with a condom catheter.
Several treatment options can be proposed to decrease functional obstruction secondary to DSD: drugs such as α-blockers or β-mimetics, intrasphincteric injections of botulinum toxin, endoscopic sphincterotomy, balloon dilatation of the striated sphincter and urethral sphincter stent.6, 7, 8, 9, 10 The use of urethral sphincter stents to treat patients with DSD was reported for the first time in 1990.10 The majority of published studies concern permanent urethral sphincter stents.11, 12, 13 However, increasingly frequently, patients request conservative and reversible management. In some cases, the impossibility or refusal of clean intermittent catheterization may be only transient and a temporary urethral sphincter stent can be placed in these situations.
The objective of this retrospective study was to evaluate the follow-up treatments used after treatment of DSD by temporary urethral sphincter stent.
Methods
Population
Between February 1994 and June 2003, 147 men with a mean age of 41.3±14.4 years underwent temporary urethral sphincter stent placement for neurogenic DSD. The patient distribution according to neurologic disease is presented in Table 1. All patients were either unable to or they refused to perform intermittent self-catheterization. Their preoperative voiding method was third-party intermittent catheterization in 43 (30.0%) cases, indwelling catheter in 36 (24.9%) cases, reflex voiding with incontinence in 24 (17.1%) cases, suprapubic percussion associated with incontinence in 21 (14.8%) cases, suprapubic catheter in 8 (5.7%) cases, clean intermittent self-catheterization in 6 (4.3%) cases, cystostomy in 2 (1.7%) cases and abdominal straining in 2 (1.7%) cases. The patients voiding with clean intermittent self-catheterization refused to continue this voiding method in all cases. Another treatment for DSD had been performed unsuccessfully in 14 cases: botulinum toxin injection in 7 cases and endoscopic sphincterotomy in 7 cases.
Preoperative assessment
Renal and bladder ultrasound, determination of creatinine clearance, urodynamic studies with electromyographic recording (EMG), retrograde and voiding cystourethrography and cystoscopy were performed in each case. Preoperative findings are presented in Table 2. The DSD was diagnosed by EMG and by urodynamics in all cases.
Operation
A Nissenkorn (Bard) stent was used in 130 cases and a Diabolo (Porgès) stent was used in 17 cases. Diabolo (Porgès) stents were used from 2002 onwards. The stent was placed under endoscopic guidance in each case and under local anesthesia in 121 cases (lidocaine jelly), general anesthesia in 17 cases and neuroleptanalgesia in 9 cases. To decrease bladder neck tone, all patients received tamsulosin 0.4 mg morning and evening.
Postoperative follow-up and parameters studied
Patients were reviewed 1 month and 3 months after stent placement and every 3 months thereafter. The following parameters were studied: intraoperative and postoperative complications, the number of episodes of symptomatic urinary tract infection before and after stent placement, the presence of signs of autonomic hyperreflexia before and after stent placement, residual urine before and after stent placement, difficulties related to the use of condom catheters, the duration of temporary stenting, difficulties at the time of stent removal and outcome after removal of the temporary stent. Early postoperative complications were defined as all complications occurring during the first 30 postoperative days. Late postoperative complications were defined as all complications occurring after the 30th postoperative day.
Statistical analysis
The results of quantitative variables are expressed as mean±s.d. These values were compared by Student's t-test (parametric test for unpaired series) and proportions were compared by the χ2 test using GraphPad Prism 3.02 software (GraphPad Software Inc., California, USA). The limit of significance for all comparisons was P<0.05.
Results
The mean hospital stay for stent placement was 3.33±1.75 days. An intraoperative complication was observed in seven (4.7%) cases: hypertensive crisis due to autonomic hyperreflexia in six cases and urethral bleeding in one case. An early postoperative complication was observed in 21 (14.3%) cases: symptomatic urinary tract infection in 14 (9.5%) cases associated with fever in 10 cases, acute urinary retention in 7 (4.8%) cases treated by suprapubic catheterization in 5 cases, macroscopic hematuria in 5 (3.4%) cases, hypertensive crisis secondary to autonomic hyperreflexia in 4 (2.7%) cases complicated by hemorrhagic stroke and death in 1 case and bradycardia associated with resuscitated cardiac arrest in 1 case, bronchial congestion requiring endoscopic aspiration in 1 case, heel pressure ulcer in 1 case and expulsion of the prosthesis in 1 case.
A late postoperative complication, consisting of symptomatic urinary tract infection, was observed in 11 (7.5%) cases. Difficulties related to the use of condom catheters were reported in 10 (6.8%) cases and stent migration was observed in 43 (29%) cases. Stent migration was suspected in case of recurrence of symptoms of autonomic hyperreflexia, of symptomatic urinary tract infections and in case of acute urinary retention. De novo autonomic hyperreflexia was observed in two (1.4%) cases.
The mean post-voiding residual volume was statistically significantly lower after stent placement than before stent placement (298.41±207.08 vs 81.06±112.17 ml, P<0.0001). The number of patients with symptoms of autonomic hyperreflexia was statistically significantly lower after stent placement than before stent placement (4 vs 20, P=0.0003). The mean number of episodes of symptomatic urinary tract infection per month was statistically significantly lower after stent placement than before stent placement (0.26±0.26 vs 0.037±0.13, P<0.0001).
The number of patients with renal dilatation and vesicoureteral reflux was statistically significantly lower after stent placement than before stent placement (3 vs 12, P=0.03 and 5 vs 16, P=0.02, respectively. Renal function remained stable after temporary stent placement in all cases.
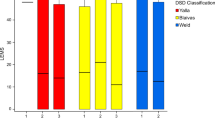
The results after stent placement according to detrusor function are summarized Table 3.
The mean duration of temporary urethral sphincter stenting was 10.2±16.1 months: 8.82±8.07 months for the Nissenkorn (Bard) stent and 12.75±7.41 months for the Diabolo (Porgès) stent. No difference between the two types of stent used was noted in terms of outcome. Problems with the condom catheter were noted in seven (4.7%) cases. It was related to penile retraction in four cases, penile pain in two cases and reflex erections in one case. No erectile dysfunction has been noted after temporary stent placement.
On removal of the stent, incrustation of the stent was observed in 5 (3.4%) cases and granulation tissue in contact with the stent was observed in 15 (10.2%) cases, exclusively when a Nissenkorn (Bard) stent was used. No problem was noted during the removal of the stent in all cases. No problems were noted with subsequent management related to the temporary stent.
In this series of 147 patients, a permanent urethral sphincter stent was placed in 92 (62.6%) cases after the removal of the temporary stent. It was placed during the same procedure in all cases. In all cases, the patients had to be satisfied with this voiding method and the temporary stent placement had to be associated with a significant decrease in urinary complications and in post void residual volume. Twelve (8.1%) patients preferred to be treated by repeated changes of the temporary stent. Seven (4.7%) patients were able to start intermittent self-catheterization. An indwelling catheter was inserted in four (2.7%) cases at the patient's request. Three (2.0%) patients were treated by cystectomy with non-continent diversion, two (1.4%) were treated by endoscopic sphincterotomy, one (0.7%) was treated by bladder neck incision, one (0.7%) was treated by posterior sacral nerve root neuromodulation and one (0.7%) was treated by surgical cystostomy. Fifteen (10.2%) patients were lost to follow-up, corresponding to spinal cord injury patients in 66.7% of cases. Two (1.4%) patients died during follow-up from a cause unrelated to the stent.
Discussion
Endoscopic sphincterotomy was developed for the treatment of DSD in the 1950s by Ross.14 It has been demonstrated to be effective for both the treatment and the prevention of genitourinary complications of DSD.15 However, this technique is associated with a failure rate of 15–50%, erectile dysfunction in 4–40% of cases, perioperative complications such as septicemia and hemorrhage in 5% of cases and is irreversible.15, 16 In view of these high complication and failure rates, α-blocker and β-mimetic drugs were proposed but without success.6 Balloon dilatation of the striated sphincter was also proposed, but subsequently abandoned owing to the high failure rate.7 Urethral sphincter stents were therefore developed.11
This study shows that temporary urethral sphincter stent placement ensures effective bladder emptying and prevents autonomic and infectious complications, as by ensuring better bladder emptying, the urethral sphincter stent significantly decreases the rate of infectious, autonomic and renal functional complications.17 It has also been recently demonstrated that this improved bladder emptying is associated with reduction of bladder voiding pressures, which also decreases urologic and nephrologic complications.11
Urethral sphincter stent was associated with low morbidity in our series. Autonomic hyperreflexia was less frequent than previously reported (1.4%),12 which is related to the position of the stent. In our series, all stents were placed within the sphincter, distal to the veru montanum. In contrast, the Memokath stent used by Hamid also passed through the bladder neck, thereby creating a source of intravesical irritation that may be responsible for dysreflexia.
The stent migration rate was 29% in our series. This rate may appear to be high, but it is nevertheless comparable to rates reported previously.12, 18 In our experience, it was frequently associated with a severe spasticity.
In this series, the voiding method after temporary urethral sphincter stent consisted of urethral sphincter stent associated with a condom catheter in 70.7% of patients. In 4.7% of cases, patients were able to start intermittent self-catheterization; these patients were spinal cord injury patients in whom a temporary stent was placed early (during the 6 months following the injury) while waiting for recovery or rehabilitation of the upper limbs, subsequently enabling intermittent self-catheterization. This voiding method ensures a lower nosocomial urinary tract infection rate in the rehabilitation unit by reducing caregiver intermittent self-catheterization and it also reduces the nursing workload.19 In 7.5% of cases, patients did not start self-catheterization and did not undergo permanent stent placement. In these patients, temporary urethral sphincter stent placement constituted a therapeutic test. This type of test is now facilitated by the Diabolo temporary stent, specifically developed for the external sphincter.20 The objectives of this test are to ensure adequate application of the condom catheter,20 verify the absence of autonomic hyperreflexia induced by the stent,12 assess acceptability of the voiding method, verify the efficacy on bladder emptying, study bladder emptying in the sitting position, improve the patient's independence and give the patient time to think about the possibilities of semen preservation, problems of fertility and sex life. After the trial period with a temporary stent, the patient can then choose the preferred voiding method, that is, return to the former method or opt for a temporary stent or a permanent stent.
The percentage of patients in our series not choosing a stent as the preferred voiding method or in whom the stent did not provide the expected results was comparable to the percentage of patients requiring removal of the permanent stent reported in the North American multicenter study.13 Owing to the absence of reliable predictive factors of the results of urethral sphincter stent, a temporary stent must constitute the first step of any change of voiding method to permanent urethral sphincter stent.
This technique is limited by the lack of material on the market specifically designed and evaluated for urethral sphincter stenting. The Nissenkorn stent has been withdrawn from the market while this study was performed and it was not specifically designed for this purpose. The only stent currently under evaluation in this indication is the Diabolo stent. Hopefully manufacturers will take advantage of progress in biomaterials in this indication to prolong the use of stents for the treatment of DSD due to their ease of placement (local anesthesia) and the fact that they can be used early in the course after spinal cord injury.19
Conclusion
Temporary urethral sphincter stent ensures effective bladder emptying and prevents infectious and autonomic complications, especially in patients with a detrusor overactivity. After temporary stenting, most patients were subsequently treated by permanent urethral sphincter stent, while several patients treated by stent soon after spinal cord injury were able to start intermittent self-catheterization.
The patients with underactive detrusor urethral stent seem to be less adapted or not indicated.
References
Weld KJ, Graney MJ, Dmochowski RR . Clinical significance of detrusor–sphincter dyssynergia type in patients with post-traumatic spinal cord injury. Urology 2000; 56: 565–568.
Schmidt RD, Markovchick V . Nontraumatic spinal cord compression. J Emerg Med 1992; 10: 189–199.
Dawson DM, Potts F . Acute nontraumatic myelopathies. Neurol Clin 1991; 9: 585–603.
Hackler RH . A 25-year prospective mortality study in the spinal cord injured patient: comparison with the long-term living paraplegic. J Urol 1977; 117: 486–488.
Weld KJ, Dmochowski RR . Effect of bladder management on urological complications in spinal cord injured patients. J Urol 2000; 163: 768–772.
Chancellor MB, Erhard MJ, Rivas DA . Clinical effect of alpha-1 antagonism by terazosin on external and internal urinary sphincter function. J Am Paraplegia Soc 1993; 16: 207–214.
McFarlane JP, Foley SJ, Shah PJ . Balloon dilatation of the external urethral sphincter in the treatment of detrusor–sphincter dyssynergia. Spinal Cord 1997; 35: 96–98.
Parratte B, Bonniaud V, Tatu L, Metton G, Michel F, Cosson A et al. Dyssynergie vésico-sphinctérienne et toxine botulique. Ann Readapt Med Phys 2003; 46: 319–325.
Ross JC, Gibbon NO, Damanski M . Division of the external urethral sphincter in the treatment of the paraplegic bladder: a preliminary report on a new procedure. Paraplegia 1987; 25: 185–195.
Shaw PJ, Milroy EJ, Timoney AG, el Din A, Mitchell N . Permanent external striated sphincter stents in patients with spinal injuries. Br J Urol 1990; 66: 297–302.
Denys P, Thiry-Escudie I, Ayoub N, Even-Schneider A, Benyahya S, Chartier-Kastler E . Urethral stent for the treatment of detrusor–sphincter dyssynergia: evaluation of the clinical, urodynamic, endoscopic and radiological efficacy after more than 1 year. J Urol 2004; 172: 605–607.
Hamid R, Arya M, Wood S, Patel HR, Shah PJ . The use of the Memokath stent in the treatment of detrusor–sphincter dyssynergia in spinal cord injury patients: a single-centre seven-year experience. Eur Urol 2003; 43: 539–543.
Gajewski JB, Chancellor MB, Ackman CF, Appell RA, Bennett J, Binard J et al. Removal of UroLume endoprosthesis: experience of the North American Study Group for detrusor–sphincter dyssynergia application. J Urol 2000; 163: 773–776.
Ross JC, Damanski M, Gibbon N . Resection of the external urethral sphincter in the paraplegic – preliminary report. J Urol 1958; 79: 742.
Fontaine E, Hajri M, Rhein F, Fakacs C, Le Mouel MA, Beurton D . Reappraisal of endoscopic sphincterotomy for post-traumatic neurogenic bladder: a prospective study. J Urol 1996; 155: 277–280.
Noll F, Sauerwein D, Stohrer M . Transurethral sphincterotomy in quadriplegic patients: long-term-follow-up. Neurourol Urodyn 1995; 14: 351–358.
Chancellor MB, Rivas DA, Abdill CK, Staas Jr WE, Bennett CJ, Finocchiaro MV et al. Management of sphincter dyssynergia using the sphincter stent prosthesis in chronically catheterized SCI men. J Spinal Cord Med 1995; 18: 88–94.
Mehta SS, Tophill PR . Memokath stents for the treatment of detrusor–sphincter dyssynergia (DSD) in men with spinal cord injury: the Princess Royal Spinal Injuries Unit 10-year experience. Spinal Cord 2006; 44: 1–6.
Chartier-Kastler EJ, Thomas L, Bussel B, Chancellor MB, Richard F, Denys P . Feasibility of a temporary urethral stent through the striated sphincter in patients in the early phase (6 months) of spinal cord injury. Eur Urol 2001; 39: 326–331.
Chartier-Kastler E, De Petriconi R, Bussel B, Richard F, Denys P . Etude de faisabilité de la prothèse endouréthrale transsphinctérienne striée Diabolo® dans le traitement de la dyssynergie vésico-sphinctérienne striée. Prog Urol 2002; 12: 59A.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gamé, X., Chartier-Kastler, E., Ayoub, N. et al. Outcome after treatment of detrusor–sphincter dyssynergia by temporary stent. Spinal Cord 46, 74–77 (2008). https://doi.org/10.1038/sj.sc.3102069
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3102069
Keywords
This article is cited by
-
Overactive bladder and multiple sclerosis in the University Hospital of Oujda
African Journal of Urology (2023)
-
Contemporary Treatment of Detrusor Sphincter Dyssynergia: a Systematic Review
Current Bladder Dysfunction Reports (2018)
-
Predictors of outcome for urethral injection of botulinum toxin to treat detrusor sphincter dyssynergia in men with spinal cord injury
Spinal Cord (2016)
-
Management of the Detrusor Sphincter Dyssynergia
Current Bladder Dysfunction Reports (2013)
-
Bladder Neck Dysfunction in Spinal Cord Injury
Current Bladder Dysfunction Reports (2011)