Abstract
Aim:
The aim of the study was to investigate the potential role of BMP6 in TGF-β1-mediated changes in HK-2 cells.
Methods:
BMP6 was purified via heparin affinity and reverse phase liquid chromatography. The purity, specificity, and bioactivity of BMP6 were determined by SDS-PAGE, Western blot assays, and the induction of alkaline phosphatase (ALP) activity, respectively. Cell proliferation, morphology, and expression levels of α-SMA and E-cadherin were assessed by cell viability, microscopy, and Western blot assays, respectively. In addition, cell adhesion abilities were determined by counting the number of attached cells. The expression of fibronectin, collagen IV, matrix metalloproteinases 2 (MMP-2), and tissue inhibitors of matrix metalloproteinases 2 (TIMP-2) were analyzed using RT-PCR. MMP-2 activity was analyzed by zymography, whereas the activation of the MAPKs and Smad signaling were analyzed using Western blot assays and a reporter gene assay, respectively.
Results:
Our results indicated that recombinant BMP6 induced ALP activity in a dose-dependent and time-course-dependent manner. Treatment with TGF-β1 reduced both the cell proliferation and the expression of E-cadherin, induced a morphological transformation, decreased the expression and activity of MMP-2, and increased the expression levels of α-SMA, fibronectin, and TIMP-2 in HK-2 cells. All of these effects were inhibited when cells were treated with TGF-β1 in combination with rhBMP6, whereas rhBMP6 alone demonstrated no such effect. Treatment with TGF-β1, rhBMP6, or a combination of both had no effect on the expression of collagen IV. In addition, the administration of rhBMP6 prevented the enhanced adhesion behavior triggered by TGF-β1. Furthermore, the addition of rhBMP6 abrogated the JNK and Smad2/3 signaling that was activated by TGF-β1.
Conclusion:
BMP6 ameliorated the TGF-β1-induced changes in HK-2 cells. The suppression of TGF-β1-mediated JNK and Smad2/3 signaling activation were implicated in these effects.
Similar content being viewed by others
Introduction
Renal tubulointerstitial fibrosis (TIF) is the most common pathological pathway that leads to end-stage renal failure. Regardless of the initial cause, renal fibrosis is characterized by interstitial fibroblast activation, which is believed to play a central role in the pathogenesis of TIF1. Although the precise origins of these myofibroblasts remain unresolved, emerging evidence suggests that they may be derived from tubular epithelial cells via an epithelial-to-mesenchymal transition (EMT) process under pathological conditions2.
Tubular EMT is a process in which renal tubular cells lose their epithelial phenotype and acquire new characteristic features similar to those of mesenchymal cells. This phenotypic conversion involves de novo synthesis of α-smooth muscle actin (α-SMA), a downregulation of E-cadherin, the acquisition of a spindle-like morphology, a disruption of the tubular basement membrane, the production of matrix proteins, and an enhanced cell migration and invasion capacity3. Transforming growth factor β1 (TGF-β1) plays a crucial role in the initiation and progression of renal fibrosis4. In response to TGF-β1, tubular epithelial cells can transdifferentiate into myofibroblasts via an EMT process. Whereas numerous factors with positive influence on renal fibrosis have been described, relatively little is known about factors that are capable of suppressing this process.
Bone morphogenetic proteins (BMPs) belong to the TGF-β1 superfamily and regulate proliferation, differentiation, and apoptosis in a variety of cell types5. Multiple BMPs have been verified to act in embryonic development and to function in the postnatal kidney6. Among these BMPs, extensive studies have demonstrated that BMP7 functions as an antifibrogenic factor that is responsible for the maintenance of kidney homeostasis7, 8, 9. Although BMP6 and BMP7 are structurally similar10, there are few reports that have probed a possible role for BMP6 in the kidney. BMP6 is expressed in the kidney only toward late gestation11, 12. Interestingly, the downregulation of BMP6 in the late gestation period of intrauterine growth-restricted newborns may predispose individuals to tubulointerstitial fibrosis in their postnatal life13. The expression of BMP6 was also observed to decrease in diabetes-derived myofibroblast progenitor cells (MFPCs) and revealed a significant inverse correlation with the number of MFPCs14. These data suggest that BMP6 may have a role in the repair and regeneration of the kidney. However, it is unclear whether BMP6 has direct effects on renal cells. Specifically, there is no information regarding the role of BMP6 in renal proximal tubular epithelial cells. In the study presented herein, we investigated the potential role of BMP6 in TGF-β1-induced changes in cultured renal tubular cells and also determined the molecular mechanisms involved in these changes.
Materials and methods
Reagents and antibodies
The cell counting kit-8 (CCK-8) containing Dojindo's tetrazolium salt (WST-8) was purchased from Dojindo Laboratories (Kumamoto, Japan). The protease inhibitor cocktail and p-nitrophenylphosphate were both obtained from Amresco (Solon, OH). The BCA assay kit was purchased from Pierce (Rockford, IL). The chromatography medium (Heparin CL-6B) and Source 15 RPC, the ECL reagent, and the autoradiography film were all purchased from Amersham Biosciences (Piscataway, NJ). The recombinant human TGF-β1 and BMP6 were purchased from R & D Systems (Minneapolis, MN). The antibodies against α-SMA and E-cadherin were obtained from Santa Cruz (Santa Cruz, CA), the β-actin antibody was obtained from Sigma (St Louis, MO), and the anti-BMP6, horseradish peroxidase (HRP)-conjugated goat anti-mouse and anti-rabbit IgG were purchased from Promega (Madison, WI). In addition, antibodies against total MAPKs and phosphorylated MAPKs were purchased from BD Bioscience (Franklin Lakes, NJ). The TRIzol RNA isolation reagent, Lipofectamine 2000, and cell culture ingredients were obtained from Invitrogen (Grand Island, NY), whereas the reverse transcription kit and Dual Luciferase Assay System were purchased from Promega (Madison, WI).
Recombinant human BMP6
Recombinant human BMP6 (rhBMP6) was expressed in Chinese hamster ovary cells (CHO) as previously described15 and purified using a combination of heparin affinity chromatography and reverse phase chromatography from a CHO-conditioned medium. The conditioned medium was diluted with 2 volumes of 50 mmol/L sodium citric acid (pH 5.5) and 9 mol/L urea. Subsequently, the protein was loaded onto a heparin CL-6B packed column pre-equilibrated with 50 mmol/L sodium citric acid and 6 mol/L urea (pH 5.5). RhBMP6 was eluted at a conductivity of 45 mS/cm using 50 mmol/L sodium citric acid, 6 mol/L urea and 1 mol/L NaCl (pH 5.5). Fractions containing rhBMP6 were dialyzed extensively with 30% acetonitrile and 0.1% trifluoroacetic acid and finally subjected to a Source 15 RPC packed column. The retained material was eluted using a linear gradient of 30% to 60% of a buffer consisting of 90% acetonitrile and 0.08% trifluoroacetic acid. The resulting fractions containing rhBMP6 were determined using Western blot assays, after which the samples were pooled and lyophilized.
Cell culture
HK-2 cells (Cell Culture Center, Beijing, China) were grown in a DMEM/F12 medium supplemented with 10% FBS and antibiotics (100 U/mL of penicillin G, 100 μg/mL of streptomycin). With the exception of the cells used for transfection, cells were growth-arrested in serum-free medium for 24 h prior to starting the experiments. Myoblast cells (C2C12) were grown in DMEM medium supplemented with 10% FBS. In the experimental protocols, cells were incubated in medium supplemented with 5% FBS. The cells were subsequently maintained at 37 °C under 5% CO2 in a humidified incubator.
Bioactivity of the rhBMP6 assays
The bioactivity of rhBMP6 was assayed by induction of alkaline phosphatase (ALP) activity in the mouse myoblast cell line C2C12. Briefly, C2C12 cells were treated with BMP6 at the indicated concentration for the indicated period of time. Viable cell numbers were determined using the CCK-8 kit, followed by an assay of ALP activity in a buffer containing p-nitrophenylphosphate as the substrate. The ALP specific activity was normalized with the viable cell number.
Cell proliferation and morphology assays
Cell proliferation was determined using the CCK-8 kit. CCK-8 (10 μL/well, 96-well plate) was added to the medium and the cells were incubated for 2 h at 37 °C. The absorbance was determined at 450 nm with an enzyme-linked immunosorbent assay analyzer. Cell morphology was imaged using a camera mounted on a microscope and processed using Adobe Photoshop software.
Reverse transcription-PCR
Total RNA was extracted using the TRIzol reagent. Reverse transcription reactions were performed using 2 μg of total RNA and were subsequently processed using a reverse transcription kit. PCR was performed under standard conditions using sense and antisense primers designed to recognize human sequences (Table 1). PCR products were then separated electrophoretically in a 1.2% agarose gel and stained with ethidium bromide for analysis with a UVitec Bioimaging System. The PCR cycle number for each primer pair was optimized for a linear increase in the densitometric band intensity measurements with increasing PCR cycles. Semiquantitative analysis of mRNA expression was accomplished by comparing the ratio of the band density of the mRNA's of interest with that of GAPDH (a housekeeping gene) from the same sample.
SDS-PAGE and Western blot assays
Cells were lysed with a lysis buffer [20 mmol/L Tris, pH 7.4, 50 mmol/L NaCl, 5 mmol/L EDTA, 1% (v/v) Triton X-100, 0.1% (w/v) SDS, 1 mmol/L phenylmethylsulfonylfluoride, 0.5 mg/L leupeptin and 0.5 mg/L aprotinin], incubated on ice for 30 min, and centrifuged at 15 000×g for 30 min at 4 °C. The desired protein in the resulting supernatant was detected using a BCA assay and separated on a 12% SDS-PAGE gel. Following gel electrophoresis, proteins were electrotransferred to a nitrocellulose membrane. Any nonspecific binding to the membrane was blocked by the addition of 3% nonfat milk in a Tris-buffered saline-0.05% Tween 20 solution overnight at 4 °C. The membrane was then incubated with primary antibodies and subsequently with the appropriate secondary antibody. Signals were visualized using an ECL reagent after exposure to X-ray film. The intensities of the immunoblots were quantified with a scanner coupled to a personal computer using the UVIband software (UVItec, Cambridge, UK).
Gelatin zymography
Equal volumes of conditioned medium were electrophoresed via 10% SDS-PAGE containing 0.1% (w/v) gelatin. The gels were then renaturated at room temperature for 30 min in a buffer containing 50 mmol/L Tris-HCl, pH 7.2, 5 mmol/L CaCl2, 1 mmol/L ZnCl2 and 2.5% Triton X-100 and then incubated overnight at 37°C in the same sample buffer containing 1% Triton X-100. The gels were then stained with Coomassie blue and destained. Gelatinolytic activity was visualized as a clear band on a blue background.
Cell adhesion assay
A cell adhesion assay was performed as described previously16. The cells were trypsinized and resuspended in DMEM/F12 containing 10% FBS. Subsequently, approximately 5×104 cells were added per well to a 96-well tissue culture plate and allowed to adhere at 37 °C for 1 h. After incubation, non-adherent cells were removed, plated in a second well, and incubated for an additional 1 h. The ability to adhere or not adhere was determined using the CCK-8 kit.
Luciferase reporter gene assay
The reporter construct SBE-Luc, which contained a specific Smad2/3 binding element coupled to a luciferase reporter, has been described previously17. HK-2 cells were plated in 24-well plates at a density of 6×104 cells/well and transfected on the following day. SBE-Luc (0.9 μg), together with pRL-TK (0.1 μg) for normalizing the transfection efficiency, was transfected using Lipofectamine 2000. After a 24-h period of transfection, the cells were incubated with the indicated cytokines for an additional 24 h and subjected to the luciferase assay. The luciferase assay was performed using the Dual Luciferase Assay System kit according to the manufacturer's protocols. All of the experiments were performed in triplicate and the relative luciferase activities were given.
Statistical analyses
The results are presented as the mean±SEM. Statistical analyses were performed using Student's t-test and the analysis of variance was characterized by P<0.05 as the minimal level of significance. Unless indicated, the results are derived from three independent experiments with similar results. The bars indicate the standard deviation.
Results
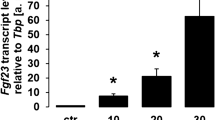
Recombinant BMP6 induces ALP activity
The purity of rhBMP6 was probed using SDS-PAGE and shown to be nearly homogeneous (Figure 1A). The disulfide-linked homodimer of rhBMP6 could be separated into its monomeric form under reducing conditions and was then able to react with anti-human BMP6 antibodies (Figure 1B). The purified rhBMP6 induced ALP activity in a dose-dependent (Figure 1C) and time-course-dependent manner (Figure 1D) with a noticeable effect observed at 25 ng/mL and a maximal effect observed at 400 ng/mL after at least 3 days of incubation.
The expression, purification, and bioactivity of rhBMP6. The purity of rhBMP6 was determined using SDS-PAGE coupled with silver staining (A). The protein bands also reacted with the anti-BMP6 antibody (B). rhBMP6 induced ALP activity in C2C12 cells in a dose-dependent (C) and time-course-dependent manner (D). Commercially available BMP6 (R&D Systems, Minneapolis, MN) was used as a positive control. M, molecular weight markers; NR, nonreducing conditions; R, reducing conditions. ALP, alkaline phosphatase. bP<0.05 vs negative control (n=6).
rhBMP6 prevents TGF-β1-mediated proliferation inhibition of HK-2 cells
TGF-β1 is a well-characterized inducer of EMT in renal tubular epithelial cells. The EMT induced by TGF-β1 appeared to be associated with a reduced cell proliferation rate18. Therefore, we tested the inhibition effect of TGF-β1 on cell proliferation in the presence and absence of rhBMP6. The cell proliferation was determined using a cell viability assay. The proliferation of HK-2 tended to be reduced upon treatment with TGF-β1, whereas administration of TGF-β1 in the presence of rhBMP6 significantly prevented the TGF-β1-induced inhibition of cell proliferation. The administration of rhBMP6 alone had only a slight effect on cell proliferation (Figure 2A and 2B).
rhBMP6 prevents the inhibition of cell proliferation by TGFβ-1. (A) HK-2 cells were treated with TGF-β1, rhBMP6, or a combination of both for 72 h at the indicated concentrations. Cell viability was then detected using the CCK-8 kit. (B) HK-2 cells were treated with TGF-β1 (10 ng/mL), rhBMP6 (200 ng/mL), or a combination of both. Cell viability of these cells was detected at the indicated time point. bP<0.05 vs control group, eP<0.05 vs TGF-β1 treatment (n=6).
rhBMP6 blocks the phenotypical transformation and morphological changes induced by TGF-β1 in HK-2 cells
The induction of EMT by TGF-β1 in numerous types of epithelial cells is accompanied by the activation of α-smooth muscle actin (α-SMA) and the downregulation of E-cadherin19. The effect of rhBMP6 on the TGF-β1-mediated induction of EMT was further analyzed using Western blot analyses of α-SMA and E-cadherin. Interestingly, α-SMA protein expression in HK-2 cells was detected at a low level in the basal state and was significantly induced by TGF-β1. Remarkably, the addition of rhBMP6 inhibited α-SMA expression in a dose-dependent and time-course-dependent manner. Furthermore, rhBMP6 prevented the downregulation of E-cadherin induced by TGF-β1 through the same mechanism (Figure 3A and 3B). To test the role of rhBMP6 in the TGF-β1-mediated induction of EMT, we further monitored the morphological changes in HK-2 cells treated with TGF-β1 alone or in combination with rhBMP6. HK-2 cells without treatment showed a typical epithelial cuboidal shape with a cobblestone morphology. Treatment with TGF-β1 alone caused the cells to appear elongated and adopt a spindle-like shape. Moreover, treatment with TGF-β1 in the presence of rhBMP6 blocked the TGF-β1-induced changes in morphology, whereas those cells that were treated with rhBMP6 alone did not undergo a change in morphology (Figure 3C).
BMP6 prevents α-SMA expression, E-cadherin depression, and cell morphology changes triggered by the addition of TGF-β1. (A) HK-2 cells were exposed to TGF-β1, rhBMP6, or a combination of both at the indicated concentrations for 72 h. (B) HK-2 cells were exposed to TGF-β1 or a combination of TGF-β1 and rhBMP6 for the indicated period of time. The total protein was then isolated and analyzed via Western blot, which was performed for α-SMA and E-cadherin protein expression assay. Equal loading of proteins was verified with β-actin. (C) HK-2 cells were treated as indicated for 72 h before imaging. The original magnification was 400×. bP<0.05 vs control group (n=3), eP<0.05 vs TGF-β1 treatment group (n=3).
rhBMP6 prevents TGF-β1-induced expression and the assembly of extracellular matrix proteins in HK-2 cells
Besides probing the induction of the changes characteristic to EMT, we further examined the gene expression of fibrosis markers such as fibronectin, collagen IV, MMP-2, and TIMP-2. Treatment of HK-2 cells with TGF-β1 increased the levels of fibronectin (0.90±0.03 vs 0.79±0.02 from the control group, n=3, P<0.01) and TIMP-2 mRNA expression (0.89±0.04 vs 0.75±0.05 of the control group, n=3, P<0.05) and decreased the expression of MMP-2 (0.73±0.05 vs 0.92±0.03 of the control group, n=3, P<0.01). In addition, the coincubation of TGF-β1 with rhBMP6 reduced the mRNA expression levels of fibronectin (0.76±0.05 vs 0.90±0.03 of the TGF-β1 treatment group, n=3, P<0.05) and the TIMP-2 mRNA expression levels (0.76±0.06 vs 0.89±0.04 of the TGF-β1 treatment group, n=3, P<0.05) in addition to increasing the mRNA levels of MMP-2 (0.87±0.05 vs 0.73±0.05 of TGF-β1 treatment group, n=3, P<0.05). Interestingly, the increase in the expression of collagen IV (COL4A1) was not increased upon TGF-β1 treatment and accordingly, no effect on rhBMP6 was observed (Figure 4A). Similar results were observed for the level of MMP-2 activity as detected by gelatin zymography (Figure 4B).
rhBMP6 prevents TGF-β1-induced ECM protein deposition. (A) HK-2 cells were exposed to TGF-β1, rhBMP6, or a combination of both for 72 h. RT-PCR was then used to check for ECM gene expression. The optimized PCR cycle number for collagen IV (COL4A1), fibronectin, TIMP-2, MMP-2 and GAPDH was 28, 26, 35, 35, and 28 cycles at an annealing temperature of 60 °C, respectively. (B) Zymography performed to test the activity of MMP-2. ECM, extracellular matrix protein.
rhBMP6 inhibits the enhanced adhesion of HK-2 cells induced by TGF-β1
TGF-β1 treatment also results in behavioral changes in HK-2 cells, including an increase in cell motility and invasion capabilities20. Cell migration typically involves discrete phases of adhesion and de-adhesion20. Therefore, we subsequently examined whether rhBMP6 treatment affected the adhesion of cells to the culture plates. In this experiment, cells that were treated with TGF-β1 showed increased adhesion. In contrast, cells that had been treated with rhBMP6 together with TGF-β1 showed reduced adhesion (Figure 5).
rhBMP6 decreases the enhanced adhesion of HK-2 cells induced by TGFβ-1. HK-2 cells were treated with TGF- β1 (10 ng/mL), rhBMP6 (200 ng/mL) or a combination of both for a 72-h period. The cells were then trypsinized, after which the adhesion and nonadhesion abilities of the treated cells were determined. bP<0.05 vs control group, eP<0.05 vs TGF-β1 treatment (n=6).
rhBMP6 suppresses the JNK and Smad signaling activated by TGF-β1
Activation of the Smad2/3 protein and the MAPKs occurs through well-characterized intracellular signaling pathways that are activated by TGF-β121. Western blot assays indicated that TGF-β1 significantly increased the phosphorylation of JNK within 1 h after the addition of TGF-β1. TGF-β1 also induced the phosphorylation of p38 to a lesser extent, with a peak phosphorylation observed after 1 h of treatment. Interestingly, our results demonstrated that phosphorylation was no longer observed 6 h after treatment. In contrast, the addition of rhBMP6 concomitantly with TGF-β1 suppressed the increased phosphorylation of JNK and p38 that was induced by TGF-β1. Unexpectedly, the combination of BMP6 and TGF-β1 induced the phosphorylation of p38 after 6 h of treatment (Figure 6A). In addition, the activation of Smad signaling was determined by the readout of the luciferase activity in the HK-2 cells transfected with a specific Smad2/3 binding element construct coupled to a luciferase reporter. The luciferase activity was induced by the addition of TGF-β1. However, co-incubation of rhBMP6 with TGF-β1 inhibited the effect of TGF-β1 in a concentration-dependent manner (Figure 6B). Additional studies with JNK inhibitors and Smad2/3 silencing confirmed that the activation of these pathways was involved in the TGF-β1 induced biological changes of HK-2 cells (unpublished observation).
rhBMP6 suppresses JNK and Smad signaling activation induced by TGF-β1. (A) HK-2 cells were treated with TGF- β1 (10 ng/mL) or a combination of TGF-β1 and rhBMP6 (200 ng/mL) for the indicated times. Western blot assays determined the total MAPKs and phospho-MAPKs. β-actin was used to ensure equal amounts of protein were loaded into each lane. (B) HK-2 cells were transiently transfected with a Smad2/3 binding element reporter plasmid SRE-Luc together with pRL-TK. After a 24-h period of transfection, the cells were incubated with the indicated concentration of TGF-β1, rhBMP6, or a combination of both for an additional 24-h period. The luciferase activity was presented as Firefly/Renilla. bP<0.05 vs non-treatment group, eP<0.05 vs TGF-β1 treatment (n=3).
Discussion
Renal interstitial fibrosis (TIF) is a feature of most progressive renal diseases that causes renal failure. The proximal renal tubular epithelial cells (PTECs) are the predominant cell type within the tubulointerstitium of the renal cortex. In addition to the transport of fluid and electrolytes, PTECs have emerged as a critical contributor to the pathogenesis of TIF. Of the many regulatory factors involved in the development of TIF, TGF-β1 plays a fundamental role in inducing epithelial cell transformation, increasing gene expression, and reducing the degradation of extracellular protein, thereby increasing the progressive extracellular deposition of matrix proteins. The HK-2 cells were derived from immortalized primary human proximal tubular cells and thus retained the phenotypic expression and functional characteristics of the cells of the human proximal tubules22. We used HK-2 cells exposed to TGF-β1 as an in vitro model to mimic the profibrogenic effect of TGF-β1, a method that is in general agreement with a previous observation. Exposure of HK-2 cells to TGF-β1 induced a complete conversion of the epithelial cells to myofibroblasts as well as other profibrogenic events23. Knowledge regarding the regulatory mechanism of these processes may lead to the development of effective therapies that halt the progression of TIF.
BMPs are members of the TGF-β1 superfamily. Among these proteins, BMP7 has received much attention as a renoprotective factor, but few reports are available for BMP67. The specific role of BMP6 in renal epithelial cells is also unclear. We tested the effect of BMP6 on the TGF-β1-induced profibrogenic changes of HK-2 in the present study. The requirement of large quantities of the BMP6 protein for research and possible applications has prompted us to produce this growth factor through recombinant DNA technology. Unlike other BMPs, the BMP6 protein can only be produced in mammalian cells because of an N-glycosylation motif of BMP6 that is essential for recognition by the type I receptor10. However, protein yields are very low and multi-step purification procedures performed in an expensive facility are usually required when purifying from the mammalian system24. We previously expressed rhBMP6 in CHO cells at a high level and developed a simplified purification procedure. The purified rhBMP6 was fully functional because the level of activity was comparable to that of the commercially available BMP6.
Incubation with rhBMP6 alone had no obvious effect on the phenotype of the HK-2 cells, whereas rhBMP6 substantially inhibited the TGF-β1-mediated EMT change, as well as the incremental deposition of matrix protein and enhanced adhesion behavior. We demonstrated here for the first time that, like BMP7, BMP6 antagonized the profibrogenic effect of TGF-β1. Several studies using different cell types have indicated clearly that the activation of MAPKs and Smad signaling is required in the TGF-β1-mediated pathway25, 26. Moreover, the addition of rhBMP6 in combination with TGF-β1 suppressed the JNK and Smad signaling activated by TGF-β1. Therefore, our data suggest that the inhibition of Smad2/3 and JNK activation induced by TGF-β1 and by the modulation of p38 activation may be a major mechanism for the antifibrotic effect of rhBMP6.
In summary, the expression and purification procedures described herein yielded a reasonably pure sample of rhBMP6. The nearly homogeneous rhBMP6 sample exhibited a remarkable ability to inhibit the profibrogenic effects of TGF-β1 in PTECs and should be useful for further investigation of rhBMP6 in the therapeutic treatment of renal interstitial fibrosis.
Author contribution
Ji-dong YAN performed the research and wrote the entire manuscript; Shuang YANG contributed new reagents; Jie ZHANG analyzed the data; Tian-hui ZHU designed the research and had final approval of the version to be published.
References
Liu Y . Renal fibrosis: new insights into the pathogenesis and therapeutics. Kidney Int 2006; 69: 213–7.
Iwano M, Plieth D, Danoff TM, Xue C, Okada H, Neilson EG . Evidence that fibroblasts derive from epithelium during tissue fibrosis. J Clin Invest 2002; 110: 341–50.
Li MX, Liu BC . Epithelial to mesenchymal transition in the progression of tubulointerstitial fibrosis. Chin Med J (Engl) 2007; 120: 1925–30.
Bani-Hani AH, Campbell MT, Meldrum DR, Meldrum KK . Cytokines in epithelial-mesenchymal transition: a new insight into obstructive nephropathy. J Urol 2008; 180: 461–8.
Chen D, Zhao M, Mundy GR . Bone morphogenetic proteins. Growth Factors 2004; 22: 233–41.
Godin RE, Robertson EJ, Dudley AT . Role of BMP family members during kidney development. Int J Dev Biol 1999; 43: 405–11.
Patel SR, Dressler GR . BMP7 signaling in renal development and disease. Trends Mol Med 2005; 11: 512–8.
Wang S, de Caestecker M, Kopp J, Mitu G, Lapage J, Hirschberg R . Renal bone morphogenetic protein-7 protects against diabetic nephropathy. J Am Soc Nephrol 2006; 17: 2504–12.
Vukicevic S, Basic V, Rogic D, Basic N, Shih MS, Shepard A, et al. Osteogenic protein-1 (bone morphogenetic protein-7) reduces severity of injury after ischemic acute renal failure in rat. J Clin Invest 1998; 102: 202–14.
Saremba S, Nickel J, Seher A, Kotzsch A, Sebald W, Mueller TD . Type I receptor binding of bone morphogenetic protein 6 is dependent on N-glycosylation of the ligand. FEBS J 2008; 275: 172–83.
Lyons K, Graycar JL, Lee A, Hashmi S, Lindquist PB, Chen EY, et al. Vgr-1, a mammalian gene related to Xenopus Vg-1, is a member of the transforming growth factor beta gene superfamily. Proc Nat Acad Sci USA 1989; 86: 4554–8.
Dudley AT, Robertson EJ . Overlapping expression domains of bone morphogenetic protein family members potentially account for limited tissue defects in BMP7 deficient embryos. Dev Dyn 1997; 208: 349–62.
Bursztyn M, Gross ML, Goltser-Dubner T, Koleganova N, Birman T, Smith Y, et al. Adult hypertension in intrauterine growth-restricted offspring of hyperinsulinemic rats: evidence of subtle renal damage. Hypertension 2006; 48: 717–23.
Nguyen TQ, Chon H, van Nieuwenhoven FA, Braam B, Verhaar MC, Goldschmeding R . Myofibroblast progenitor cells are increased in number in patients with type 1 diabetes and express less bone morphogenetic protein 6: a novel clue to adverse tissue remodelling? Diabetologia 2006; 49: 1039–48.
Yan JD, Yang S, Lü SJ, Lei RY, Zhu TH . Expression of recombinant human BMP6 in CHO cells by fused to the signal peptide and propeptide of another homologue protein. Chin J Biotech 2007; 23: 413–7.
Lamouille S, Derynck R . Cell size and invasion in TGF-beta-induced epithelial to mesenchymal transition is regulated by activation of the mTOR pathway. J Cell Biol 2007; 178: 437–51.
Dennler S, Itoh S, Vivien D, ten Dijke P, Huet S, Gauthier JM . Direct binding of Smad3 and Smad4 to critical TGF beta-inducible elements in the promoter of human plasminogen activator inhibitor-type 1 gene. EMBO J 1998; 17: 3091–100.
Moore LD, Isayeva T, Siegal GP, Ponnazhagan S . Silencing of transforming growth factor-beta1 in situ by RNA interference for breast cancer: implications for proliferation and migration in vitro and metastasis in vivo. Clin Cancer Res 2008; 14: 4961–70.
Liu Y . Epithelial to mesenchymal transition in renal fibrogenesis: pathologic significance, molecular mechanism, and therapeutic intervention. J Am Soc Nephrol 2004; 15: 1–12.
Angers-Loustau A, Côté JF, Tremblay ML . Roles of protein tyrosine phosphatases in cell migration and adhesion. Biochem Cell Biol 1999; 77: 493–505.
Derynck R, Zhang YE . Smad-dependent and Smad-independent pathways in TGF-beta family signalling. Nature 2003; 425: 577–84.
Ryan MJ, Johnson G, Kirk J, Fuerstenberg SM, Zager RA, Torok-Storb B . HK-2: an immortalized proximal tubule epithelial cell line from normal adult human kidney. Kidney Int 1994; 45: 48–57.
Slattery C, Campbell E, McMorrow T, Ryan MP . Cyclosporine A-induced renal fibrosis: a role for epithelial-mesenchymal transition. Am J Pathol 2005; 167: 395–407.
Sampath TK, Maliakal JC, Hauschka PV, Jones WK, Sasak H, Tucker RF, et al. Recombinant human osteogenic protein-1 (hOP-1) induces new bone formation in vivo with a specific activity comparable with natural bovine osteogenic protein and stimulates osteoblast proliferation and differentiation in vitro. J Biol Chem 1992; 267: 20352–62.
Levy L, Hill CS . Smad4 dependency defines two classes of transforming growth factor β (TGF-β) target genes and distinguishes TGF-β-induced epithelial-mesenchymal transition from its antiproliferative and migratory responses. Mol Cell Biol 2005; 25: 8108–25.
Zhang M, Fraser D, Phillips A . ERK, p38, and Smad signaling pathways differentially regulate transforming growth factor-beta1 autoinduction in proximal tubular epithelial cells. Am J Pathol 2006; 169: 1282–93.
Acknowledgements
This work was supported by a grant from the Tianjin Natural Science Foundation (No 05YFJMJC01800).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yan, Jd., Yang, S., Zhang, J. et al. BMP6 reverses TGF-β1-induced changes in HK-2 cells: implications for the treatment of renal fibrosis. Acta Pharmacol Sin 30, 994–1000 (2009). https://doi.org/10.1038/aps.2009.56
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/aps.2009.56
Keywords
This article is cited by
-
Bone morphogenetic protein 6 (BMP6) antagonises experimental proliferative vitreoretinopathy established by TGF-β2 stimulation in retinal pigment epithelial cells through modulation of the p38 and JNK MAPK pathways
Cell and Tissue Research (2024)
-
Candidate rejuvenating factor GDF11 and tissue fibrosis: friend or foe?
GeroScience (2020)
-
The role of extracellular vesicles in renal fibrosis
Cell Death & Disease (2019)
-
Involvement of collagen-binding heat shock protein 47 in scleroderma-associated fibrosis
Protein & Cell (2015)
-
Recent advances in renal interstitial fibrosis and tubular atrophy after kidney transplantation
Fibrogenesis & Tissue Repair (2014)