Abstract
Aim:
To compare the effects of cholecalciferol (800 IU/d) and calcitriol (0.25 μg/d) on calcium metabolism and bone turnover in Chinese postmenopausal women with vitamin D insufficiency.
Methods:
One hundred Chinese postmenopausal women aged 63.8±7.0 years and with serum 25-hydroxyvitamin D [25(OH)D] concentration <30 ng/mL were recruited. The subjects were divided into 2 groups based on the age and serum 25(OH)D concentration: 50 subjects (group A) received cholecalciferol (800 IU/d), and 50 subjects (group B) received calcitriol (0.25 μg/d) for 3 months. In addition, all the subjects received Caltrate D (calcium plus 125 IU cholecalciferol) daily in the form of one pill. The markers of calcium metabolism and bone turnover, including the serum levels of calcium, phosphorus, alkaline phosphatase, intact parathyroid hormone, 25(OH)D and β-CrossLaps of type I collagen containing cross-linked C-telopeptide (β-CTX), were measured before and after the intervention.
Results:
After the 3-month intervention, the serum 25(OH)D concentration in group A was significantly increased from 16.01±5.0 to 20.02±4.5 ng/mL, while that in group B had no significant change. The serum calcium levels in both the groups were significantly increased (group A: from 2.36±0.1 to 2.45±0.1 mmol/L; group B: from 2.36±0.1 to 2.44±0.1 mmol/L). The levels of serum intact parathyroid hormone in both the groups were significantly decreased (group A: from 48.56±12.8 to 39.59±12.6 pg/mL; group B: from 53.67±20.0 to 40.32±15.4 pg/mL). The serum levels of β-CTX in both the groups were also significantly decreased (group A: from 373.93±135.3 to 325.04±149.0 ng/L; group B: from 431.00±137.1 to 371.74±185.0 ng/L).
Conclusion:
We concluded that both cholecalciferol (800 IU/d) and calcitriol (0.25 μg/d) plus Caltrate D modifies the serum calcium and bone turnover markers in Chinese postmenopausal women with vitamin D insufficiency. In addition, cholecalciferol (800 IU/d) significantly increased the serum 25(OH)D concentration.
Similar content being viewed by others
Introduction
The vitamin D receptor is found in bone, most tissues and cells in the body. Vitamin D deficiency is a common health problem that increases the risk of many common and serious diseases, including some cancers, type 1 diabetes, cardiovascular disease, and osteoporosis1. Vitamin D is important for maintaining bone health because it stimulates the synthesis of osteopontin and alkaline phosphatase and inhibits osteoblast apoptosis2. Vitamin D status is best evaluated by measuring the serum concentration of 25-hydroxyvitamin D [25(OH)D]3. Most specialties define vitamin D deficiency as 25(OH)D levels below 20 ng/mL4. A level of 25(OH)D of 21–29 ng/mL indicates a vitamin D insufficiency whereas a level of 30 ng/mL or greater indicates vitamin D sufficiency5. The prevalence of atrophic skin changes in older adults is concomitant with an increased probability of lower 25(OH)D levels6. Unlike those of other nutrients, dietary sources of vitamin D are limited. Therefore, most people require supplements such as cholecalciferol (vitamin D3) to meet the recommended intake7. Current guidelines for vitamin D intakes vary around the world. The National Osteoporosis Foundation (NOF) recommends an intake of 800 to 1000 international units (IU) of vitamin D per day for adults 50 years and older8. Hanley et al9 have suggested that adults over 50 years old are at a moderate risk for vitamin D deficiency and recommended the use of a supplement with at least 800–1000 IU of vitamin D3. In an expert roundtable discussion, it was agreed that the daily vitamin D intake should be approximately 800 IU for most postmenopausal women10. One study indicated that serum 25(OH)D increased with cholecalciferol supplementation and nearly plateaued after 3–4 months of intervention11. In elderly people, diminished renal function due to aging leads to a decrease in renal conversion to 1,25(OH)2D312. Calcitriol [1,25(OH)2D3] plays an important role in promoting bone formation, and D-hormone analogs prevent falls to a greater extent than does ordinary vitamin D. Therefore, the use of D-hormone analogs has been advocated for the treatment of osteoporosis in many studies13, 14, 15. Because patients who are treated with 0.5 μg/d or 1.0 μg/d of calcitriol tend to develop hypercalcinuria, serum and urinary calcium levels should be examined regularly, and the calcitriol regime should be examined intermittently. Patients are frequently treated with 0.25 μg/d of calcitriol in China, especially elderly patients with osteoporosis. Hurst et al16 concluded that correcting vitamin D deficiency in older women may suppress the age-induced acceleration in bone turnover and may reduce bone resorption. However, Seemans et al17 observed that despite the stratification of different vitamin D receptor genotypes, cholecalciferol supplementation throughout the winter months did not affect bone turnover markers in young or old people. The aim of the current study was to compare the effects of cholecalciferol at 800 IU per day and calcitriol at 0.25 μg per day on calcium metabolism and bone turnover in Chinese postmenopausal women who are vitamin D insufficient.
Materials and methods
Subjects and study design
This was an open-label, controlled clinical trial. The study was approved by the Ethics Committee of the Shanghai Jiao Tong University Affiliated Sixth People's Hospital.
One hundred healthy, independent, ambulatory, postmenopausal female volunteers were recruited from community centers. All participants were of Han ethnicity and had lived in Shanghai for more than 30 years. Postmenopausal women over 50 years of age were eligible for the study, and the serum 25(OH)D concentrations of all subjects were less than 30 ng/mL. All subjects were given a physical examination and were found to be in good health. No participant was receiving treatment or had medical complications that were known to affect bone metabolism, including hyperthyroidism, diabetes mellitus, primary hyperparathyroidism, renal failure, pituitary diseases, and adrenal diseases. All the women had taken less than 600 mg/day of calcium and less than 600 IU/day of vitamin D within the 3 months prior to enrollment. The subjects were divided into two groups based on age and serum 25(OH)D concentrations. Fifty of the subjects received 800 IU/day of cholecalciferol (Cholecalciferol, Xingsha Pharmaceuticals Co, Xiamen, China), and the other fifty matched subjects received 0.25 μg/day of calcitriol (Calcitriol, Roche Pharmaceuticals Co, Shanghai, China), as group A and group B, respectively. All subjects received 1 pill/day of Caltrate D (containing 600 mg of calcium and 125 IU of vitamin D3, Wyeth Pharmaceuticals, Health Care Products, Suzhou, China). Because the Caltrate D contained 125 IU of vitamin D3, group A was provided 925 IU of cholecalciferol altogether. The study period was from December 2009 to March 2010, which was during the end of winter and the beginning of spring in China.
Laboratory tests
Fasting blood samples were obtained at baseline and at the end of the study. Blood routine, erythrosedimentation, liver function, renal function and fasting blood-glucose were examined to exclude subjects who had other factors that may affect their vitamin D status. Markers of calcium metabolism and bone turnover were assessed before and after the three-month intervention, including serum calcium (Ca), phosphorus (P), alkaline phosphatase (AKP) (using the HITACHI7600-020 automatic biochemistry analyzer), intact parathyroid hormone (normal, 15–65 pg/mL, intact PTH Kit, Roche Diagnostics, Mannheim, Switzerland), concentrations of 25(OH)D (25 hydroxy vitamin D3 Kit, Roche Diagnostics, Mannheim, Switzerland; using a Cobase 6000 electrochemiluminescence analyzer) and β-CrossLaps of type I collagen containing cross-linked C-telopeptide (β-CTX) (β-CrossLaps Kit, Roche Diagnostics, Mannheim, Switzerland). The coefficients of variability (CV) of serum Ca, P, AKP, PTH, 25(OH)D, and β-CTX were 2.4%, 3.3%, 5.1%, 9.5%, 4.0%, and 3.4%, respectively.
Statistical analysis
Data are represented as the mean±standard deviation (SD). Comparisons of the result before and after treatments were calculated using paired Student's t-test for the parametric data of each group. The independent sample t-tests were used to compare the serum parameters before and after the treatments of groups A and B, respectively. The independent sample t-test was used to compare the difference in the change pattern over time between group A and group B, starting at the treatment baseline. All calculations were performed using SPSS ver 11.0 software (SPSS Inc, Chicago, IL, USA). Data were considered statistically significant at a value of P<0.05.
Results
The baseline characteristics of 100 postmenopausal women are shown in Table 1. The mean age of the subjects was 63.8±7.0 years old, the mean menopausal period was 13.7±8.7 years, and the mean 25(OH)D level was 16.84±5.4 ng/mL.
Serum parameters of groups A and B
The baseline characteristics showed no differences between the two groups, except that β-CTX was significantly higher in group B than that in group A (P<0.05) (Table 2).
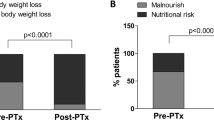
After the 3-month intervention, the mean serum 25(OH)D increased from 16.01±5.0 ng/mL to 20.02±4.5 ng/mL in group A (P<0.01). However, the mean serum 25(OH)D showed no significant difference before and after the intervention performed on group B (P>0.05) (Table 3). In group A, serum 25(OH)D less than 20 ng/mL was detected in 76% of women (34/45), including 18% of women (8/45) with less than 10 ng/mL vitamin D, and 25(OH)D between 20 and 30 ng/mL was indicated in 24% of women (11/45) previous to the intervention. Serum 25(OH)D less than 20 ng/mL was indicated in 49% of group A (22/45), including 2% of women (1/45) with less than 10 ng/mL vitamin D, and 25(OH)D between 20 and 30 ng/mL was indicated in 51% of group A (23/45) after the intervention. In group B, serum 25(OH)D less than 20 ng/mL was indicated in 66% of women (31/47), including 13% of women (6/47) with less than 10 ng/mL vitamin D, and 25(OH)D between 20 and 30 ng/mL was indicated in 34% of women (16/47) before the intervention. Serum 25(OH)D less than 20 ng/mL was indicated in 85% of group B (40/47), including 6% of group B (3/47) with less than 10 ng/mL vitamin D, and vitamin D 25(OH)D between 20 and 30 ng/mL was indicated in 15% of group B (7/47) after the intervention.
After the three-month intervention, both groups showed a significant increase in serum Ca levels (all P<0.01) that were within the normal range. The AKP levels of groups A and B also showed a significant increase (P<0.05 and P<0.01, respectively). The serum PTH and β-CTX levels showed a significant decrease in both groups (all P<0.01 and all P<0.05) (Table 3).
We compared the serum parameters between the two groups after the 3-month intervention and identified significantly higher levels of serum 25(OH)D in group A than those of group B (P<0.01) (Table 4). We compared the difference in the change pattern between the two groups over time starting at treatment baseline and found that only serum 25(OH)D showed a significant difference between group A and group B (Table 5).
Withdrawal from the study and adverse events
Eight participants (5 participants in the group A and 3 participants in the group B) discontinued the study. In the group A, two participants withdrew without providing a reason, two participants were lost during follow-up, and one participant withdrew because of cholelithiasis and shingles that, according to the clinical judgment, were attributed to a severe adverse event but were not related to the use of study medication. In the group B, three participants withdrew without providing a reason. After the 3-month treatment, the concentration of serum Ca, P, and the total AKP activities in the two groups remained within normal ranges.
Discussion
Many studies have shown that 40% to 100% of elderly people in the US and Europe suffer from vitamin D deficiencies18, 19. More than 50% of postmenopausal women had levels of 25-hydroxyvitamin D that were lower than 30 ng per milliliter19. Low levels of 25(OH)D are associated with a significant decrease in the absorption of intestinal calcium and induced secondary hyperparathyroidism18, 20. Secondary hyperparathyroidism may stimulate the transformation of preosteoclasts into mature osteoclasts, causing osteoporosis and increasing the risk of fracture19. Our results show that serum Ca levels increased and serum PTH levels decreased significantly after supplementation with of cholecalciferol (800 IU/d) plus Caltrate D for three months. Kuwabara et al21 discovered that the supplementation of 200 mg of calcium with 800 IU of vitamin D3 daily for one month significantly lowered the serum PTH levels compared with the supplementation of only 200 mg of calcium daily. Seemans et al17 identified that in the winter, the endpoint serum PTH level to be significantly lower in 3 cholecalciferol-supplemented groups (cholecalciferol 200 IU, 400 IU, and 600 IU) compared with the placebo group, though other bone turnover markers were not affected. An increased rate of bone turnover is associated with low bone mass22 and an increased risk of bone fracture23. Higher levels of serum CTX indicate an increase in bone resorption and bone fragility24. Total AKP is primarily a nonspecific marker of bone formation. Our results show that after supplementing with 800 IU per day of cholecalciferol for three months, serum AKP levels increased significantly, and serum β-CTX levels decreased. These results indicate that 800 IU per day of cholecalciferol is effective for stimulating bone formation and reducing bone resorption. Hurst et al16 has shown that vitamin D-deficient women who were administered 4000 IU of cholecalciferol daily for 6 months displayed a suppression of age-induced bone turnover and bone resorption. However, some studies have shown cholecalciferol supplementation have no effect on bone turnover markers17, 21.
Oral vitamin D supplementation increases bone mineral density and appears to reduce the risk of hip and other nonvertebral fractures. Therefore, it is reasonable to supply 800–1000 IU/d of vitamin D to older individuals25. Heaney et al11 found that after supplementing with 1000, 5000, and 10 000 IU of cholecalciferol, the serum 25(OH)D levels of every group plateaued after 3–4 months intervention. Therefore, Hanley et al[9] suggested measuring the serum 25(OH)D after 3–4 months of adequate intervention. In our study, the mean concentration of serum 25(OH)D increased from 16.01 to 20.02 ng/mL after 3 months of supplementation with cholecalciferol. However, 49% of this group was still vitamin D-deficient. The cholecalciferol group in our study was provided with 125 IU of Caltrate D. Therefore, the total cholecalciferol reached 925 IU, and the dose was not sufficient to achieve adequate 25(OH)D concentrations. Similarly, Pignotti et al26 have shown that after supplementation with 400 IU of cholecalciferol and 1200 mg of calcium for 3 months in sunny Brazil, the concentration of serum 25(OH)D increased from 18.7 ng/mL to 23.8 ng/mL. However, 86.2% of the supplemented group did not reach optimal levels (30.0 ng/mL) of 25(OH)D. Kuwabara et al21 discovered that after supplementation with 800 IU of cholecalciferol and 200 mg of calcium for 1 month, serum 25(OH)D levels in old men and women increased from 9.7 ng/mL to 19.3 ng/mL, although 60% of the subjects remained vitamin D-deficient. However, Chapuy et al27 reported that after supplementation with 800 IU of cholecalciferol and 1200 mg of calcium for 6 months, serum 25(OH)D levels increased from 9.2 ng/mL to 30.0 ng/mL. The varied results of these different studies may be associated with the dose of cholecalciferol, the period of study, the intake of calcium and differences associated with the population. Hanley et al9 systematically reviewed 168 potentially relevant vitamin D papers from 1996 to 2008 and concluded that vitamin D was necessary for the prevention of osteoporosis. They recommended an intake of cholecalciferol for high-risk and older adults ranging from 800 to 2000 IU daily. To achieve satisfactory vitamin D status (>30 ng/mL), many individuals may require higher doses. A similar suggestion was made at an expert roundtable discussion. The participants concluded that the intake of vitamin D should be at least 800 IU daily10. In addition, this recommendation was independent of sun exposure, seasonal exposure and additional multivitamin use.
Calcitriol has been used as a therapy for osteoporosis for many years. One study verified that supplementation with calcitriol at 0.5 μg per day for six months may promote bone formation and decrease bone absorption28. Active vitamin D analogs have a larger impact in decreasing bone loss and fracture incidence than standard vitamin D in postmenopausal osteoporosis because vitamin D analogs display a greater effect in reducing numbers of falls29. Calcitriol plays an important role in skeletal system regulation and may have other bone-protective effects independent of its calcium absorption effects30. To prevent hypercalcinuria, patients with osteoporosis or osteopenia in China are frequently treated with 0.25 μg/d of calcitriol13. After 3 months of intervention in our study, no differences were identified in calcium metabolism and bone turnover between the group treated with 0.25 μg of calcitriol daily and the group treated with 800 IU of cholecalciferol daily. Serum calcium and AKP levels were significantly increased in both groups. The serum PTH and β-CTX levels were significantly decreased in both groups. However, the serum 25(OH)D level did not change significantly in the calcitriol group; it showed only a slight decreasing trend. Clements et al31 discovered that after supplementation with 1 μg per day of calcitriol to treat postmenopausal osteoporosis, hypoparathyroidism and hypophosphatemic osteomalacia, the elimination half-time for 25(OH)D in the plasma could be significantly shortened by raising the circulating concentration of 1,25-dihydroxyvitamin D. One explanation for this result is that calcitriol is the activated form of cholecalciferol, and excessive calcitriol decreases serum 25(OH) in a negative feedback system. Halloran et al32 discovered that rats chronically administered calcitriol displayed reduced serum concentrations of 25-OH-D3 and 24,25(OH)2D3 in a dose- and time-dependent fashion. Calcitriol administration increased the metabolic clearance of 25-OH-D but not its production.
After 3 months of intervention, the concentration of serum Ca, P, and the total AKP activities in both groups remained within normal ranges. However, urinary calcium excretions were not observed in either group; this was a limitation of our study. In the United States, the previous NOF guidelines set the safe upper limit for vitamin D intake at 2000 IU per day. However, recent evidence has shown that higher intake is safe and that some older patients need at least this amount to maintain adequate 25(OH)D levels8. Doses of more than 50 000 IU of vitamin D3 per day are associated with hypercalcemia and hyperphosphatemia33. However, Vieth et al34 observed that doses of 10 000 IU of cholecalciferol daily for up to 5 months did not cause toxicity. In a randomized, double-blind trial that tested the efficacy and safety of zoledronic acid (5 mg) that was intravenously supplemented annually in preventing new fractures in women and men who had hip fractures35, all the patients received oral calcium (1000–1500 mg) and vitamin D (800–1200 IU) daily. By the end of the study, none of the patients suffered from hypercalcemia. These results indicate that the current safe upper intake level of 2000 IU of vitamin D per day may be too conservative.
Our current study indicated that that cholecalciferol (800 IU/d) plus Caltrate D increased the mean serum 25(OH)D to 20 ng/mL in most but not all individuals. Both 800 IU/day of cholecalciferol and 0.25 μg/day of calcitriol plus Caltrate D effectively modified calcium and bone turnover markers in postmenopausal women in Shanghai with vitamin D insufficiency. The use cholecalciferol or calcitriol and the doses specified in the study for improving the bone health of postmenopausal women requires further investigation.
Author contribution
Qi-ren HUANG designed this research; Hao ZHANG, Zhen-lin ZHANG, Jie-mei GU, Wei-wei HU, and Yu-juan LIU performed clinical research; Qi-ren HUANG, Jie-mei GU, Yun-qiu HU, and Yu-juan LIU recruited subjects; Hao ZHANG wrote the paper; and Qi-ren HUANG and Zhen-lin ZHANG revised the paper.
References
Holick MF . Vitamin D deficiency. N Engl J Med 2007; 357: 266–81.
Morales O, Samuelsson MK, Lindgren U, Haldosen LA . Effects of 1alpha,25-dihydroxyvitamin D3 and growth hormone on apoptosis and proliferation in UMR 106 osteoblast-like cells. Endocrinology 2004; 145: 87–94.
DeLuca HF . Overview of general physiologic features and functions of vitamin D. Am J Clin Nutr 2004; 80: 1689S–96S.
Thomas MK, Lloyd-Jones DM, Thadhani RI, Shaw AC, Deraska DJ, Kitch BT, et al. Hypovitaminosis D in medical inpatients. N Engl J Med 1998; 338: 777–83.
Dawson-Hughes B, Heaney RP, Holick MF, Lips P, Meunier PJ, Vieth R . Estimates of optimal vitamin D status. Osteoporos Int 2005; 16: 713–6.
Holick MF, Matsuoka LY, Wortsman J . Age, vitamin D, and solar ultraviolet. Lancet 1989; 2: 1104–5.
Weaver CM, Fleet JC . Vitamin D requirements: current and future. Am J Clin Nutr 2004; 80: 1735S–9S.
Foundation NO . Clinician's Guide to Prevention and Treatment of Osteoporosis. Washington, DC: National Osteoporosis Foundation; 2010. Report No: 0029–6643 (Print) 0029–6643 (Linking).
Hanley DA, Cranney A, Jones G, Whiting SJ, Leslie WD . Vitamin D in adult health and disease: a review and guideline statement from Osteoporosis Canada (summary). CMAJ 2010; 182: 1315–9.
Roux C, Bischoff-Ferrari HA, Papapoulos SE, de Papp AE, West JA, Bouillon R . New insights into the role of vitamin D and calcium in osteoporosis management: an expert roundtable discussion. Curr Med Res Opin 2008; 24: 1363–70.
Heaney RP, Davies KM, Chen TC, Holick MF, Barger-Lux MJ . Human serum 25-hydroxycholecalciferol response to extended oral dosing with cholecalciferol. Am J Clin Nutr 2003; 77: 204–10.
Lau KH, Baylink DJ . Vitamin D therapy of osteoporosis: plain vitamin D therapy versus active vitamin D analog (D-hormone) therapy. Calcif Tissue Int 1999; 65: 295–306.
Xia WB, Zhang ZL, Wang HF, Meng XW, Zhang Y, Zhu GY, et al. The efficacy and safety of calcitriol and/or Caltrate D in elderly Chinese women with low bone mass. Acta Pharmacol Sin 2009; 30: 372–8.
Holzherr ML, Retallack RW, Gutteridge DH, Price RI, Faulkner DL, Wilson SG, et al. Calcium absorption in postmenopausal osteoporosis: benefit of HRT plus calcitriol, but not HRT alone, in both malabsorbers and normal absorbers. Osteoporos Int 2000; 11: 43–51.
Richy F, Dukas L, Schacht E . Differential effects of D-hormone analogs and native vitamin D on the risk of falls: a comparative meta-analysis. Calcif Tissue Int 2008; 82: 102–7.
von Hurst PR, Stonehouse W, Kruger MC, Coad J . Vitamin D supplementation suppresses age-induced bone turnover in older women who are vitamin D deficient. J Steroid Biochem Mol Biol 2010; 121: 293–6.
Seamans KM, Hill TR, Wallace JM, Horigan G, Lucey AJ, Barnes MS, et al. Cholecalciferol supplementation throughout winter does not affect markers of bone turnover in healthy young and elderly adults. J Nutr 2010; 140: 454–60.
Holick MF, Siris ES, Binkley N, Beard MK, Khan A, Katzer JT, et al. Prevalence of vitamin D inadequacy among postmenopausal North American women receiving osteoporosis therapy. J Clin Endocrinol Metab 2005; 90: 3215–24.
Lips P, Hosking D, Lippuner K, Norquist JM, Wehren L, Maalouf G, et al. The prevalence of vitamin D inadequacy amongst women with osteoporosis: an international epidemiological investigation. J Intern Med 2006; 260: 245–54.
Heaney RP, Dowell MS, Hale CA, Bendich A . Calcium absorption varies within the reference range for serum 25-hydroxyvitamin D. J Am Coll Nutr 2003; 22: 142–6.
Kuwabara A, Tsugawa N, Tanaka K, Fujii M, Kawai N, Mukae S, et al. Improvement of vitamin D status in Japanese institutionalized elderly by supplementation with 800 IU of vitamin D(3). J Nutr Sci Vitaminol (Tokyo) 2009; 55: 453–8.
Ravn P, Fledelius C, Rosenquist C, Overgaard K, Christiansen C . High bone turnover is associated with low bone mass in both pre- and postmenopausal women. Bone 1996; 19: 291–8.
Seeman E, Delmas PD . Bone quality — the material and structural basis of bone strength and fragility. N Engl J Med 2006; 354: 2250–61.
Eastell R, Hannon RA . Biomarkers of bone health and osteoporosis risk. Proc Nutr Soc 2008; 67: 157–62.
Bischoff-Ferrari HA, Willett WC, Wong JB, Giovannucci E, Dietrich T, Dawson-Hughes B . Fracture prevention with vitamin D supplementation: a meta-analysis of randomized controlled trials. JAMA 2005; 293: 2257–64.
Pignotti GA, Genaro PS, Pinheiro MM, Szejnfeld VL, Martini LA . Is a lower dose of vitamin D supplementation enough to increase 25(OH)D status in a sunny country? Eur J Nutr 2010; 49: 277–83.
Chapuy MC, Pamphile R, Paris E, Kempf C, Schlichting M, Arnaud S, et al. Combined calcium and vitamin D3 supplementation in elderly women: confirmation of reversal of secondary hyperparathyroidism and hip fracture risk: the Decalyos II study. Osteoporos Int 2002; 13: 257–64.
Tsukamoto Y, Watanabe T, Nakagami T, Morishita K . Effect of treatment with oral calcitriol on calcium metabolism and fasting serum 25(OH)- or 1,25(OH)2-vitamin D level in Japanese postmenopausal women. Endocr J 2003; 50: 681–7.
Schacht E, Richy F, Reginster JY . The therapeutic effects of alfacalcidol on bone strength, muscle metabolism and prevention of falls and fractures. J Musculoskelet Neuronal Interact 2005; 5: 273–84.
Richy F, Ethgen O, Bruyere O, Reginster JY . Efficacy of alphacalcidol and calcitriol in primary and corticosteroid-induced osteoporosis: a meta-analysis of their effects on bone mineral density and fracture rate. Osteoporos Int 2004; 15: 301–10.
Clements MR, Davies M, Hayes ME, Hickey CD, Lumb GA, Mawer EB, et al. The role of 1,25-dihydroxyvitamin D in the mechanism of acquired vitamin D deficiency. Clin Endocrinol (Oxf) 1992; 37: 17–27.
Halloran BP, Bikle DD, Levens MJ, Castro ME, Globus RK, Holton E . Chronic 1,25-dihydroxyvitamin D3 administration in the rat reduces the serum concentration of 25-hydroxyvitamin D by increasing metabolic clearance rate. J Clin Invest 1986; 78: 622–8.
Koutkia P, Chen TC, Holick MF . Vitamin D intoxication associated with an over-the-counter supplement. N Engl J Med 2001; 345: 66–7.
Vieth R . Why the optimal requirement for vitamin D3 is probably much higher than what is officially recommended for adults. J Steroid Biochem Mol Biol 2004; 89–90: 575–9.
Lyles KW, Colon-Emeric CS, Magaziner JS, Adachi JD, Pieper CF, Mautalen C, et al. Zoledronic acid and clinical fractures and mortality after hip fracture. N Engl J Med 2007; 357: 1799–809.
Acknowledgements
This study was supported by the National Natural Science Foundation of China (NSFC) (No 30800387, 30771019, 81070692, 81170803), Academic Leaders in Health Sciences in Shanghai (XBR2011014), STCSM10DZ1950100, Science and Technology commission of Shanghai municipality (11ZR1427300) and Shanghai Rising Star Project (No 11QA1404900).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zhang, H., Huang, Qr., Gu, Jm. et al. Comparison of the effects of cholecalciferol and calcitriol on calcium metabolism and bone turnover in Chinese postmenopausal women with vitamin D insufficiency. Acta Pharmacol Sin 33, 490–495 (2012). https://doi.org/10.1038/aps.2011.172
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/aps.2011.172
Keywords
This article is cited by
-
Seasonal variation of serum 25-hydroxyvitamin D level in hemodialysis patients in the northernmost island of Japan
Clinical and Experimental Nephrology (2021)
-
Association between SOST gene polymorphisms and response to alendronate treatment in postmenopausal Chinese women with low bone mineral density
The Pharmacogenomics Journal (2019)
-
Calcitriol treatment in patients with low vitamin D levels
Archives of Osteoporosis (2018)
-
The effects of high-dose calcitriol and individualized exercise on bone metabolism in breast cancer survivors on hormonal therapy: a phase II feasibility trial
Supportive Care in Cancer (2018)
-
The efficacy and safety of weekly 35-mg risedronate dosing regimen for Chinese postmenopausal women with osteoporosis or osteopenia: 1-year data
Acta Pharmacologica Sinica (2015)