Abstract
Reversal of renal dysfunction significantly affects the prognosis of multiple myeloma (MM) with renal impairment (RI). There is no reliable test for predicting reversibility of RI in MM patients. We postulated that MM with high albuminuria may reflect glomerular disease that is difficult to reverse. Here, we examined the impact of urinary albumin excretion. We retrospectively analyzed 279 patients admitted to our hospital from April 2000 to December 2013. Clinical variables and laboratory data that may affect myeloma treatment response were extracted. The results were examined for relationship to renal response by univariate and multivariate analysis. RI (estimated glomerular filtration rate ≦50 ml/min per 1.73 m2) was observed in 116 patients (46%) and renal responses of renal complete response, renal partial response, renal minor response and no response were obtained in 46 (40%), 15 (13%), 13 (11%) and 42 (36%) patients, respectively. Although renal recovery was significantly associated with Durie–Salmon 1 or 2 (P=0.02), myeloma response better than very good partial response (P=0.03), involved free light-chain (iFLC) reduction from baseline 80% at day 12 (P=0.005), ≧95% at day 21 (P<0.001) and urinary albumin ≦25% on admission (P<0.001) on univariate analysis, only reduction of iFLC 95% at day 21 (P=0.015) and urinary albumin ≦25% (P=0.007) remained significant for any renal response. Our observation indicates that increased urinary albumin excretion >25% and reduction of iFLC ≦95% on day 21 were associated with favorable renal recovery in MM patients with RI, and were considered as negative predictors for renal response.
Similar content being viewed by others
Main
Renal impairment (RI) is a major cause of morbidity and mortality in patients with multiple myeloma (MM) and approximately 50 and 20% of patients have RI and acute renal failure depending of its definition.1, 2, 3, 4 The presence of RI limits the use of antimyeloma agents and eligibility for stem cell transplantation, and, therefore, places these patients at higher risk for disease progression and myeloma-related complications. RI is also associated with an increased risk of early death,5,6 although the recent introduction of effective novel agents, such as thalidomide, bortezomib and lenalidomide, has led to the improved survival even in patients with RI.7,8
The most common cause of RI in MM is cast nephropathy, which may be seen in up to 30% of patients;9 other causes of RI include monoclonal immunoglobulin (Ig) deposition disease and amyloidosis. It should be noted that non-paraprotein-associated renal lesions are also seen in 25% of patients. As most patients with MM are elderly, age-related comorbidities such as hypertension and diabetes may also be associated with the decline of renal function.
As the reversibility of renal function may be dependent on the pathogenesis of renal disease,10 correct renal pathology is necessary for successful treatment. Use of bortezomib-based regimens in combination with or without plasma exchange has been reported to yield high rates of renal recovery in patients with cast nephropathy.11, 12, 13, 14 However, reversibility of renal function in cases other than cast nephropathy is largely unknown. Kidney biopsy cannot be performed in all patients with MM and RI because of its various limitations and possible complications. Recently, Nasr et al.9 reported the clinicopathologic correlations in MM patients with kidney biopsy; they reported the highest levels of albuminuria in patients with amyloidosis and lowest levels in those with cast nephropathy.
Despite the heterogeneity of renal pathology, urine albuminuria is thought to reflect glomerular injury, and patients with cast nephropathy usually show tubulointerstitial injury and lack heavy albuminuria. Therefore, we postulated that renal response may be different according to urinary albumin excretion. In this study, we retrospectively analyzed the clinical variables that may affect renal response in 116 MM patients with RI at our hospital. We also examined the predictive capacity of urinary albumin and serum-free light-chain (FLC) reduction on renal recovery of RI patients with MM.
Patients and methods
We retrospectively reviewed the medical records of the Department of Hematology/Oncology at Kameda Medical Center, Kamogawa-shi, Japan, from April 2000 to December 2013. Patients diagnosed as MM complicated with RI were included in the study. Diagnosis of myeloma and evaluation of treatment response were performed according to the International Myeloma Foundation criteria and the treatment response criteria.15 Patients with primary systemic amyloid light-chain (AL) amyloidosis were excluded from this study. RI was defined as an estimated glomerular filtration rate (eGFR) that was measured before treatment ≦50 ml/min per 1.73 m2 by the simplified Modification of Diet in Renal Disease formula.16, 17, 18 Maximal renal response was evaluated during the course of disease according to the recently proposed ‘Criteria for the Definition of Renal Response to Antimyeloma Therapy’ from the International Myeloma Working Group.2 Briefly, renal complete response (CRenal) was defined as a sustained (i.e., lasting for at least 2 months) increase in baseline eGFR to 60 ml/min per 1.73 m2. Renal partial response (PRenal) was defined as an increase of eGFR from 15 to 30–59 ml/min per 1.73 m2 and renal minor response (MRenal) as sustained improvement of baseline eGFR of <15 to 15–29 ml/min per 1.73 m2 or, if baseline eGFR was 15–29 ml/min per 1.73 m2, improvement to 30–59 ml/min per 1.73 m2. If the patient was dependent on dialysis, achievement of dialysis independency was regarded as at least MRenal depending on the recovery of eGFR. Demographic and laboratory data were obtained from electronic records. Patients with pre-existing severe RI (creatinine ≧2.0 mg/dl) owing to causes other than MM were excluded from the study. Extracted clinical data related to myeloma and RI included age, sex, complete blood count, urinalysis, serum protein electrophoresis, serum FLCs, serum albumin, β2-microglobulin, serum creatinine, total urinary protein and urine protein electrophoresis. The percentage of urinary albumin excretion was calculated by protein electrophoresis pattern on admission, and it was considered zero if the protein electrophoresis could not detect any albumin (5 mg/dl). Typical measurement of urine albumin by urine protein electrophoresis was shown in Figure 1. Serum FLCs were measured by nephelometry using the BN II nephelometer (Dade Behring, Deerfield, IL, USA) and Freelite Serum Free Light Chain Kit (The Binding Site, San Diego, CA, USA). Reduction of serum FLC was checked at day 12 and at day 21 after the start of antimyeloma therapy. Baseline serum FLC data were available for 90 patients with RI, as the Freelite assay was not available at our institution until September 2007.
ROC analysis of % of iFLC reduction for obtaining any renal response in patients with RI. (a) ROC analysis of FLC reduction at day 12 from the baseline. The highest sensitivity point of % of iFLC reduction at day 12 was identified as 81.7% with sensitivity 0.931, specificity 0.500 and AUC 0.740 with 95% CI of 0.633–0.850. (b) ROC analysis of FLC reduction at day 21 from the baseline. The highest sensitivity point of % of iFLC reduction at day 12 was identified as 95.5% with sensitivity 0.931, specificity 0.500 and AUC 0.742 with 95% CI of 0.635–0.850.
Approval was obtained by the institutional review board at the Kameda Medical Center in accordance with the Declaration of Helsinki.
Statistical analyses
Baseline characteristics were analyzed for significance of differences between groups by one-way analysis of variance or Student’s t-test for continuous variables and the χ2-test or Fisher’s exact test for categorical variables. Receiver-operating characteristic (ROC) curves were constructed, and an appropriate cutoff value to predict renal response was decided according to the Youden index.19 The results are shown as mean±s.d., numbers (%) and HR with 95% confidence interval (CI). Data analysis was performed with R version 2.14. All statistical test values were two-sided, and P<0.05 was taken to indicate significance in all analyses.
Results
Clinical variables among patients with RI in relation to renal response
A total of 279 patients with myeloma who were admitted to Kameda Medical Center and received at least one course of antimyeloma treatment were included in the study. Among them, 116 patients (41.6%) presented with greater than moderate RI (eGFR ≦50 ml/min per 1.73 m2). Median survival of patients with RI was shorter than that of those without RI (51.3 vs 76.5 months, respectively, P=0.07). Among the patients with RI, the overall survival (OS) of patients with any renal response was longer than those without such response, but the difference was not statistically significant (42.2 months vs 33.5 months, respectively, P=0.16).
Improvement of RI to any degree was seen in 74 patients with RI (63.8%). CRrenal, PRrenal and MRrenal was obtained in 46 (40%), 15 (13%), 13 (11%) patients, respectively. Forty-two patients (36%) did not show any renal response. Nine of the 24 dialysis-dependent patients (37.5%) at presentation became dialysis independent. Seven patients had myeloma and amyloidosis and only two patients received renal biopsy. Among them, five patients did not show renal response and one patient showed MRenal and one showed CRenal. There was no significant association between the quality of renal response and quality of myeloma response. Among the 61 patients with more than PRenal response, 14 (23.0%), 15 (24.6%), 27 (44.3%) and 5 (8.2%) showed myeloma response of CR, very good partial response (VGPR), PR and SD or less, respectively. If the patients’ renal response was limited to those patients with CRenal, myeloma responses of CR, VGPR, PR and SD or less were 9 (19.6%), 12 (26.1%), 21 (45.7%) and 4 (8.7%), respectively. Conversely, among 52 patients with RI who obtained more than VGPR, renal responses of CRenal, PRenal, MRenal and no response were seen in 21 (40.4%), 8 (15.4%), 9 (17.3%) and 14 (26.9%), respectively. There was no difference in median OS between patients with major renal response and those with minor or no response (39.8 vs 43.9 months, P=0.97).
Table 1 shows the clinical and laboratory data for patients with and without any renal response. Data of baseline iFLC were available for 90 patients (77.4%) with RI: 59/74 (79.7%) with renal response and 31/42 (73.8%) without renal response.
Median OS, age, gender, myeloma subtype, hemoglobin, serum albumin, β2-microglobulin, baseline creatinine, baseline iFLC, absolute daily albumin excretion, ISS stage and treatment at presentation were not different between responders and non-responders. However, comparison between the responder with non-responder groups indicated lower median percentage of urinary albumin (7.5% vs 30.0%, P=0.007), and higher prevalence of Durie–Salmon stage 3 (86.4% vs 66.7%, P=0.02) in the former than the latter. Myeloma response ≧VGPR was marginally associated with any renal response (50.0% vs 35.7%, P=0.08).
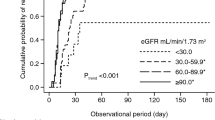
Although baseline iFLC levels were not significantly different among patients with or without renal response, it has been reported that iFLC reduction on days 12 and 21 after treatment is an important determinant for recovery of renal function in dialysis-dependent MM patients.13,20 We next examined the association between subsequent renal response and degree of iFLC reduction on days 12 and 21. ROCs were constructed to determine the best cutoff percentage of iFLC reduction for renal recovery. From the curve, the highest sensitivity point of % of iFLC reduction on day 12 was identified as 81.7% with sensitivity of 0.931, specificity of 0.500 and AUC of 0.740 (Figure 1a). Similarly, 95.5% reduction was identified with sensitivity of 0.931, specificity of 0.500 and AUC of 0.742 on day 21 (Figure 1b). Therefore, reduction of iFLC >80% on day 12 and >95% on day 21 were set for further analysis. When iFLC reduction >80% on day 12 and >95% on day 21 was compared between patients with and without renal recovery, the percentages of responders and non-responders were 35.1% vs 6.0% (P=0.005) and 35.1% vs 3.6% (P<0.001), respectively.
Patients with RI and renal response showed significantly lower percentage of urinary albumin compared with those without renal response (Table 1, P=0.007). The best cutoff value of 24.0% urinary albumin excretion was identified by ROC analysis, which had specificity of 65.8%, sensitivity of 74.0% and AUC of 0.666 with 95% CI of 0.545–0.0.786 (Figure 2). Therefore, we set 25% of urinary albumin as the cutoff value for further analysis. Among the 111 patients with renal response, both any renal response and major renal response (≧PRenal), median iFLC, eGFR and iFLC reduction on days 12 and 21 were associated with less urinary albumin excretion ≦25%. However, median OS was not different between patients with urinary albumin ≦25% and those with urinary albumin >25% (Table 2).
Univariate and multivariate analyses were performed to examine the factors that affect renal response (Tables 3 and 4). Durie–Salmon stage 1 or 2 (P=0.02), myeloma response ≧VGPR (P=0.03), reduction of iFLC ≧80% on day 12 (P=0.005) and ≧95% on day 21 (P<0.001), and baseline urinary albumin ≦25% (P<0.001) were associated with any degree of renal response. However, on multivariate analysis, iFLC reduction ≧95% on day 21 (P=0.015) and urinary albumin ≦25% at baseline (P=0.007) remained significant for prediction of any renal response (Table 3). If the analysis was limited to patients with severe RI (≦30 ml/min per 1.73 m2), similar results were obtained on both univariate and multivariate analyses, although urinary albumin ≦25% at baseline became marginally significant (Tables 4, P=0.06).
Discussion
The underlying mechanisms of pathologic renal injury in MM are diverse21,22 and can be separated into those resulting from monoclonal Ig and other factors independent of monoclonal Ig accumulation, such as dehydration, hypercalcemia, infection, use of contrast media or nephrotoxic drugs, etc.1 Monoclonal Ig-mediated renal injury can be further divided into tubulointerstitial and glomerular injury according to the lesion of RI.1,23 Tubulointerstitial injury is usually seen in cast nephropathy and glomerular injury is seen in amyloidosis.9 Monoclonal Ig deposition disease, which includes light-chain deposition disease, shows a mixed pattern.
Bortezomib with high-dose dexamethasone is considered the standard treatment for MM patients with RI.17,23 However, the reversibility of kidney injury in patients with MM depends both on the effectiveness of chemotherapy and the underlying renal pathology.10 Unfortunately, only kidney biopsy can distinguish the variety of these renal pathologies in RI in MM, but it is difficult to perform in all patients with RI.
The presence of toxic monoclonal FLC has an important role in the pathogenesis of myeloma kidney disease. A decrease in serum iFLC is thought to be critical for recovery from kidney injury in cast nephropathy.12,24,25 Hutchison et al.13 reported a close relationship between any renal recovery and reduction of serum FLC in biopsy-proven severe cast nephropathy using high cutoff hemodialysis. They emphasized that the degree of FLC reduction is important, and that the speed at which reduction occurs is also important. Although FLC reduction from the circulation is closely linked to renal function, it does not always result in reversal of renal function in patients other than those with cast nephropathy. In this study, we included all of the consecutive MM patients with RI except those with a clear history of renal failure unrelated to myeloma. Consistent with the analysis of Hutchison et al.,20 renal response was associated with early reduction of iFLC on days 12 and 21 by univariate analysis, but on multivariate analysis more than 95% of iFLC reduction on day 21 was significantly associated with renal response. Our patients included a variety of renal diseases that may not respond to FLC reduction, while Hutchison et al. included only cases of biopsy-proven cast nephropathy.
Urine analysis is a simple but essential test for patients with renal disease irrespective of its cause, but urine dipstick detects only albumin and is unreliable for detecting myeloma paraprotein. Renal lesions of amyloidosis and monoclonal Ig deposition disease are usually seen in the glomeruli, whereas tubulointerstitial lesions are seen in cast nephropathy.1 Recently, Leung et al.26 reported the association of renal pathology and urine albumin excretion. They found that the % of urinary albumin excretion was highest in patients with amyloid light-chain amyloidosis (70%), followed by light-chain deposition disease (55%), acute tubular necrosis (25%) and lowest in cast nephropathy (7%). Our results validate their observations in the clinical setting. Consistent with their observations, median percentage of urine albumin in patients with and without renal response were 7.5% and 30%, respectively (P=0.007) in our study. Urinary secretion of Bence–Jones protein was not measured in our study because of difficulty in its quantification. As various proteins were often excreted in urine, multiple peaks that prevent measurement of urinary Bence–Jones protein were frequently observed in a subset of patients with RI by urine protein electrophoresis. Dimopoulos et al.7 reported that high levels of urinary Bence–Jones protein (>2 g per day) were not related to renal response in patients treated with novel agents.
Univariate and multivariate analyses also showed the significance of urinary albumin excretion ≧25% as a negative predictive factor for renal recovery. Percentages of serum FLC reduction ≧80% on day 12 and ≧95% on day 21 were also significant in univariate analysis, but only the latter remained significant in multivariate analysis. The present study validates the recent observation reported by Leung et al.26 who found that urinary albumin excretion ≧25% is a negative predictor for biopsy-proven cast nephropathy with sensitivity of 0.98, specificity of 0.94 and negative predictive value of 0.99.
Early reduction of serum iFLC is associated with renal recovery in MM patients with RI. When RI is severe, serum levels of iFLC will remain high even with effective chemotherapy because of reduced renal clearance that may in turn further aggravate renal function. Plasma exchange and high cutoff dialysis have been examined with mixed efficacy.12,27,28 However, with use of urinary albumin excretion pattern, we could further stratify the MM patients with RI who would benefit from aggressive FLC reduction strategy. We speculate that the group of RI patients with low albumin excretion will especially benefit from early institution of aggressive chemotherapy combined with direct removal of FLC by targeting the FLC levels.
Although the positive prognostic value of urine albumin <25% on renal response appeared robust, it is important to recognize that this was a retrospective study and patients were treated heterogeneously. In addition, we did not stratify the patients except for eGFR. Renal pathology data were not available for most of the patients. We recently encountered one patient with vascular limited renal amyloidosis29 who did not show increased percentage of albuminuria despite heavy systemic accumulation of amyloid at autopsy. Although glomerular deposition of amyloid is most common in renal amyloidosis, with an occurrence rate of >80% of cases, vascular or interstitial dominant amyloid deposition may also occur with varied urinary albumin excretion pattern.30 It is possible that more than one type of renal lesion can exist in the same patient,31 which would result in a more complex outcome of renal function.
In conclusion, we retrospectively analyzed the factors that affect the renal recovery of patients with myeloma and RI. Only percentage of urinary albumin ≦25% and reduction of iFLC >95% on day 21 showed positive predictive value for subsequent renal recovery. Although promising as a screening test for renal response, our data should be examined further in larger cohorts of patients in a prospective manner and in patients with biopsy-proven renal pathology.
References
Gaballa MR, Laubach JP, Schlossman RL, Redman K, Noonan K, Mitsiades CS et al. Management of myeloma-associated renal dysfunction in the era of novel therapies. Expert Rev Hematol 2012; 5: 51–66; quiz 58-67.
Dimopoulos MA, Terpos E, Chanan-Khan A, Leung N, Ludwig H, Jagannath S et al. Renal impairment in patients with multiple myeloma: a consensus statement on behalf of the International Myeloma Working Group. J Clin Oncol 2010; 28: 4976–4984.
Kyle RA, Gertz MA, Witzig TE, Lust JA, Lacy MQ, Dispenzieri A et al. Review of 1027 patients with newly diagnosed multiple myeloma. Mayo Clin Proc 2003; 78: 21–33.
Knudsen LM, Hjorth M, Hippe E . Renal failure in multiple myeloma: reversibility and impact on the prognosis. Nordic Myeloma Study Group. Eur J Haematol 2000; 65: 175–181.
Blade J, Kyle RA . Multiple myeloma in young patients: clinical presentation and treatment approach. Leuk Lymphoma 1998; 30: 493–501.
Augustson BM, Begum G, Dunn JA, Barth NJ, Davies F, Morgan G et al. Early mortality after diagnosis of multiple myeloma: analysis of patients entered onto the United kingdom Medical Research Council trials between 1980 and 2002—Medical Research Council Adult Leukaemia Working Party. J Clin Oncol 2005; 23: 9219–9226.
Dimopoulos MA, Roussou M, Gkotzamanidou M, Nikitas N, Psimenou E, Mparmparoussi D et al. The role of novel agents on the reversibility of renal impairment in newly diagnosed symptomatic patients with multiple myeloma. Leukemia 2013; 27: 423–429.
Kastritis E, Zervas K, Symeonidis A, Terpos E, Delimbassi S, Anagnostopoulos N et al. Improved survival of patients with multiple myeloma after the introduction of novel agents and the applicability of the International Staging System (ISS): an analysis of the Greek Myeloma Study Group (GMSG). Leukemia 2009; 23: 1152–1157.
Nasr SH, Valeri AM, Sethi S, Fidler ME, Cornell LD, Gertz MA et al. Clinicopathologic correlations in multiple myeloma: a case series of 190 patients with kidney biopsies. Am J Kidney Dis 2012; 59: 786–794.
Leung N, Gertz MA, Zeldenrust SR, Rajkumar SV, Dispenzieri A, Fervenza FC et al. Improvement of cast nephropathy with plasma exchange depends on the diagnosis and on reduction of serum free light chains. Kidney Int 2008; 73: 1282–1288.
Chanan-Khan AA, Kaufman JL, Mehta J, Richardson PG, Miller KC, Lonial S et al. Activity and safety of bortezomib in multiple myeloma patients with advanced renal failure: a multicenter retrospective study. Blood 2007; 109: 2604–2606.
Burnette BL, Leung N, Rajkumar SV . Renal improvement in myeloma with bortezomib plus plasma exchange. N Engl J Med 2011; 364: 2365–2366.
Hutchison CA, Cockwell P, Stringer S, Bradwell A, Cook M, Gertz MA et al. Early reduction of serum-free light chains associates with renal recovery in myeloma kidney. J Am Soc Nephrol 2011; 22: 1129–1136.
Matsue K, Fujiwara H, Iwama K, Kimura S, Yamakura M, Takeuchi M . Reversal of dialysis-dependent renal failure in patients with advanced multiple myeloma: single institutional experiences over 8 years. Ann Hematol 2010; 89: 291–297.
Durie BG, Harousseau JL, Miguel JS, Blade J, Barlogie B, Anderson K et al. International uniform response criteria for multiple myeloma. Leukemia 2006; 20: 1467–1473.
Levey AS, Eckardt KU, Tsukamoto Y, Levin A, Coresh J, Rossert J et al. Definition and classification of chronic kidney disease: a position statement from Kidney Disease: Improving Global Outcomes (KDIGO). Kidney Int 2005; 67: 2089–2100.
Dimopoulos MA, Richardson PG, Schlag R, Khuageva NK, Shpilberg O, Kastritis E et al. VMP (Bortezomib, Melphalan, and Prednisone) is active and well tolerated in newly diagnosed patients with multiple myeloma with moderately impaired renal function, and results in reversal of renal impairment: cohort analysis of the phase III VISTA study. J Clin Oncol 2009; 27: 6086–6093.
Morabito F, Gentile M, Mazzone C, Rossi D, Di Raimondo F, Bringhen S et al. Safety and efficacy of bortezomib-melphalan-prednisone-thalidomide followed by bortezomib-thalidomide maintenance (VMPT-VT) versus bortezomib-melphalan-prednisone (VMP) in untreated multiple myeloma patients with renal impairment. Blood 2011; 118: 5759–5766.
Schisterman EF, Perkins NJ, Liu A, Bondell H . Optimal cut-point and its corresponding Youden Index to discriminate individuals using pooled blood samples. Epidemiology 2005; 16: 73–81.
Hutchison CA, Heyne N, Airia P, Schindler R, Zickler D, Cook M et al. Immunoglobulin free light chain levels and recovery from myeloma kidney on treatment with chemotherapy and high cut-off haemodialysis. Nephrol Dial Transplant 2012; 27: 3823–3828.
Heher EC, Goes NB, Spitzer TR, Raje NS, Humphreys BD, Anderson KC et al. Kidney disease associated with plasma cell dyscrasias. Blood 2010; 116: 1397–1404.
Fermand JP, Bridoux F, Kyle RA, Kastritis E, Weiss BM, Cook MA et al. How I treat monoclonal gammopathy of renal significance (MGRS). Blood 2013; 122 22: 3583–3590.
Heher EC, Rennke HG, Laubach JP, Richardson PG . Kidney disease and multiple myeloma. Clin J Am Soc Nephrol 2013; 8: 2007–2017.
Hutchison CA, Blade J, Cockwell P, Cook M, Drayson M, Fermand JP et al. Novel approaches for reducing free light chains in patients with myeloma kidney. Nat Rev Nephrol 2012; 8: 234–243.
Davenport A, Merlini G . Myeloma kidney: advances in molecular mechanisms of acute kidney injury open novel therapeutic opportunities. Nephrol Dial Transplant 2012; 27: 3713–3718.
Leung N, Gertz M, Kyle RA, Fervenza FC, Irazabal MV, Eirin A et al. Urinary albumin excretion patterns of patients with cast nephropathy and other monoclonal gammopathy-related kidney diseases. Clin J Am Soc Nephrol 2012; 7: 1964–1968.
Clark WF, Stewart AK, Rock GA, Sternbach M, Sutton DM, Barrett BJ et al. Plasma exchange when myeloma presents as acute renal failure: a randomized, controlled trial. Ann Intern Med 2005; 143: 777–784.
Hutchison CA, Bradwell AR, Cook M, Basnayake K, Basu S, Harding S et al. Treatment of acute renal failure secondary to multiple myeloma with chemotherapy and extended high cut-off hemodialysis. Clin J Am Soc Nephrol 2009; 4: 745–754.
Eirin A, Irazabal MV, Gertz MA, Dispenzieri A, Lacy MQ, Kumar S et al. Clinical features of patients with immunoglobulin light chain amyloidosis (AL) with vascular-limited deposition in the kidney. Nephrol Dial Transplant 2012; 27: 1097–1101.
Hopfer H, Wiech T, Mihatsch MJ . Renal amyloidosis revisited: amyloid distribution, dynamics and biochemical type. Nephrol Dial Transplant 2011; 26: 2877–2884.
Lorenz EC, Sethi S, Poshusta TL, Ramirez-Alvarado M, Kumar S, Lager DJ et al. Renal failure due to combined cast nephropathy, amyloidosis and light-chain deposition disease. Nephrol Dial Transplant 2010; 25: 1340–1343.
Acknowledgements
We thank the patients, nurses, technicians and physicians who contributed on this study. We are especially grateful to those who took care of the patients at our department during the period of this study. We also thank Dr Yuya Matsue, Department of Cardiology Kameda Medical Center, for his critical review of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/4.0/
About this article
Cite this article
Sugihara, H., Chihara, D., Seike, K. et al. Percentage of urinary albumin excretion and serum-free light-chain reduction are important determinants of renal response in myeloma patients with moderate to severe renal impairment. Blood Cancer Journal 4, e235 (2014). https://doi.org/10.1038/bcj.2014.56
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bcj.2014.56
This article is cited by
-
Diagnose und Therapie der Nierenbeteiligung bei Plasmazellerkrankungen
Der Internist (2019)
-
Myeloma light chain cast nephropathy, a review
Journal of Nephrology (2019)