Abstract
Background:
Biliary tract cancers (BTC) are relatively rare malignant tumours with poor prognosis. It is known from other solid neoplasms that antitumour inflammatory response has an impact on tumour behaviour and patient outcome. The aim of this study was to provide a comprehensive characterisation of antitumour inflammatory response in human BTC.
Methods:
Tumour-infiltrating T lymphocytes (CD4+, CD8+, and Foxp3+), natural killer cells (perforin+), B lymphocytes (CD20+), macrophages (CD68+) as well as mast cells (CD117+) were assessed by immunohistochemistry in 375 BTC including extrahepatic (ECC; n=157), intrahepatic (ICC; n=149), and gallbladder (GBAC; n=69) adenocarcinomas. Overall and intraepithelial quantity of tumour-infiltrating immune cells was analysed. Data were correlated with clinicopathological variables and patient survival.
Results:
The most prevalent inflammatory cell type in BTC was the T lymphocyte. Components of the adaptive immune response decreased, whereas innate immune response components increased significantly in the biliary intraepithelial neoplasia – primary carcinoma – metastasis sequence. BTC patients with intraepithelial tumour-infiltrating CD4+, CD8+, and Foxp3+ T lymphocytes showed a significantly longer overall survival. Number of total intraepithelial tumour-infiltrating Foxp3+ regulatory T lymphocytes (HR: 0.492, P=0.002) and CD4+ T lymphocytes (HR: 0.595, P=0.008) were tumour grade- and UICC-stage-independent prognosticators. The subtype-specific evaluation revealed that the tumour-infiltrating lymphocytic infiltrate is a positive outcome predictor in ECC and GBAC but not in ICC.
Conclusion:
Our findings characterise the immune response in cholangiocarcinogenesis and identify inflammatory cell types that influence the outcome of BTC patients. Further, we show that BTC subtypes show relevant differences with respect to density, quality of inflammation, and impact on patient survival.
Similar content being viewed by others
Main
Biliary tract cancers (BTC) are a diverse group of tumours that arise from the biliary tract epithelium. Biliary tract cancers can be divided into three major clinical phenotypes: cholangiocarcinomas (CC) of intrahepatic (ICC) and extrahepatic (ECC) origin and adenocarcinomas of the gallbladder (GBAC). In the United States and Europe, risk factors for BTC include chronic biliary tract diseases, such as primary sclerosing cholangitis, hepatolithiasis, choledochal cysts, and other anatomical malformations of the bile ducts (Blechacz et al, 2011). Non-biliary diseases such as heavy alcohol abuse, obesity, non-alcoholic fatty liver disease, chronic hepatitis C, and cirrhosis are also more prevalent in BTC patients compared with the general population. For BTC patients with locally advanced or metastatic disease, the prognosis is poor with median survival less than 1 year (Hezel et al, 2010). Common therapeutic options include surgery and chemotherapy but as BTC patients often present in an unresectable state, there is an urgent need of novel chemotherapeutic options (Patel, 2011). As some BTC patients are in a general condition insufficient to undergo aggressive systemic treatment, finding better and reliable prognostic markers for BTC is of importance for further stratification of patients for therapeutic trials.
Tumour cells are often surrounded by infiltrating inflammatory cells, particularly lymphocytes and macrophages (Smyth et al, 2006). Tumour antigens drive the development of tumour-specific adaptive immune responses (Boon et al, 1994). CD4+ and CD8+ T lymphocytes are crucial components of tumour-specific cellular adaptive immunity. CD8+ T lymphocytes attack tumour cells presenting tumour-associated antigen peptide with major histocompatibility complex class I (MHC I) on their surface by producing interferon-γ. Interferon-γ-dependent mechanisms of tumour cell cytostasis and killing comprise cell cycle inhibition, apoptosis, angiostasis, and induction of antitumourigenic activity of macrophages (Dunn et al, 2004). Immunohistochemical studies have found that tumour-infiltrating CD8+ T lymphocytes have a favourable effect on patient survival in several malignant tumours including colorectal (Galon et al, 2006), ovarian (Zhang et al, 2003), breast (Mahmoud et al, 2011), and pancreatic (Fukunaga et al, 2004) cancer. In colorectal cancer (CRC), density and location of CD8+ T lymphocytes have a prognostic value superior to and independent of the International Union Against Cancer (UICC) – TNM classification (Mlecnik et al, 2011). Further, density of immune cells at the invasive margin of metastatic CRC is predictive for response to chemotherapy (Halama et al, 2011).
In BTC, sub-populations of immune cells have so far only been studied in parts, using comparably small patient cohorts and without specifying anatomical/histological subtypes (Oshikiri et al, 2003; Takagi et al, 2004). Therefore, our aim was to analyse the influence of density and distribution of tumour-infiltrating immune cells on patient prognosis in a large, well-characterized series of BTC patients with long-time follow-up.
Materials and methods
Clinicopathological characteristics of BTC patients
Tissue samples from 375 patients (median 64.1 years) who underwent bile duct and/or liver surgery at the University Hospital Heidelberg between 1995 and 2010 were included in this study. Only patients with primary adenocarcinomas of the biliary tract and without other known malignancies at the time of diagnosis were included. Biliary tract cancers consisted of 149 ECC (106 perihilar and 43 distal), 157 ICC, and 69 GBAC. Patients who received radiochemotherapy before surgery were excluded. Survival data were available for 335 patients (Table 1). Tumours were restaged according to the seventh TNM classification of malignant tumours and classified after the World Health Organization (WHO) tumour classification system (Bosman et al, 2010). Clinicopathological data of the complete study cohort is given in Supplementary Table 1. The use of the tissues for this study was approved by the institutional ethics committee (206/05).
TMA construction and immunohistochemistry
From all 375 BTC, 3 μm sections were cut and stained with H&E. Representative areas from the tumour centre and invasive margins were marked by pathologists with special expertise in BTC pathology (BG and WW). For each case, tumour tissue cores (1.5 mm diameter) from the selected representative tumour areas were punched out of the sample tissue blocks and embedded into a new paraffin array block using a tissue microarrayer (Beecher Instruments, Woodland, CA, USA). For 92 cases, in addition, high-grade dysplastic lesions (BilIN III) were sampled. In addition, we included 30 metastatic lesions of BTC. For the characterisation of the inflammatory components, vessel density, and proliferative activity, a monoclonal mouse IgG antibody directed against CD4 (1:20, Novocastra, Newcastle upon Tyne, UK), a monoclonal mouse IgG antibody directed against CD8 (1:150, DAKO, Hamburg, Germany), a monoclonal mouse IgG antibody directed against CD20 (1:150, DAKO, Glostrup, Denmark), a monoclonal mouse IgG antibody directed against CD31 (1: 25, DAKO, Denmark), a monoclonal mouse IgG antibody directed against CD68 (1: 8000, DAKO, Denmark), a polyclonal rabbit IgG antibody directed against CD117 (1: 50, DAKO, Denmark), a monoclonal mouse IgG antibody directed against Perforin (1:20, Novocastra), a monoclonal IgG antibody directed against Foxp3 (1:100, clone 236A/E7, Abcam, Cambridge, UK), and a monoclonal mouse IgG antibody directed against Ki-67 (1: 200, clone Mib 1, DAKO, Glostrup, DK) were used. Staining was performed on two automated systems (Foxp3: Bond, Leica, Wetzlar, Germany; all others were obtained from Discovery Ultra, Ventana, Tuscon, AZ, USA) following the manufacturers’ instructions.
Evaluation of TMAs
Immune cell density was assessed quantitatively on tissue microarray (TMA) slides. Immune cells were identified as either T-helper cells (CD4+), regulatory T lymphocytes (Foxp3+, a subset of CD4+ T lymphocytes), cytotoxic T lymphocytes (CD8+), natural killer (NK) cells (perforin+), B lymphocytes (CD20+), macrophages (CD68+), and mast cells (CD117+). The immunostaining was in all instances evaluated in conjunction with morphology to avoid misclassification of immunohistochemically positive cells without matching morphology as immune cells. For CD4, CD8, CD20, CD68, Foxp3, CD31, and Ki-67 the whole set of cases could be evaluated, whereas for perforin and CD117 only a part of the cohort was available. Infiltrating immune cells were numerically evaluated in the category ‘total’ by counting the total number of positive immune cells per TMA dot, regardless of whether these cells were found in the epithelial or in the stromal compartment of the adenocarcinoma (for example, ‘CD4 total’). For statistical analyses, the cases were grouped by using the median as a cutoff. We defined those cases with an inflammatory infiltrate above the median as positive and those cases with an inflammatory infiltrate below the median as negative for the respective infiltrating immune cell type. Overall, NK cell count numbers were very low; therefore, we grouped cases as having none or any number of infiltrating NK cells. In solid tumours, the localisation of inflammatory cells (stroma vs epithelium) has been shown to be of some importance (Galon et al, 2006). Therefore, the number of infiltrating immune cells within a representative area containing 100 carcinoma cells (epithelial compartment of the carcinoma) was evaluated separately (for example, ‘CD4 intraepithelial’). Immune cells observed in lymphoid follicles (aggregates) were excluded from counting; the presence of lymph follicles was evaluated separately. For technical reasons, single TMA dots could not be evaluated with the necessary precision. Therefore, the number of cases included varies between the statistical analyses of the different immune cell types. The number of Ki-67-stained tumour cells out of 100 tumour cells were counted and expressed in percent. The number of CD31+ vessels was counted per TMA dot (1.5 mm diameter).
Statistical analyses
Statistical analyses were performed with the statistical computing environment R version 2.15.1 and IBM SPSS STATISTICS version 19 (SPSS, Chicago, IL, USA). Spearman’s rank order correlation was used to determine whether there was a positive or negative correlation between the degrees of tumour-infiltrating immune cells, vessel density, and proliferative activity. The significance of differences in the density of immune cells for differing tumour stages and other clinicopathological variables was assessed with Mann–Whitney-U-tests, Kruskal–Wallis tests, and χ2-tests, as indicated. Statistically significant trends associated with increasing UICC stages, tumour grades, or T-stages were identified by Jonkheere–Terpstra and Cochran–Armitage trend tests. Univariate survival analysis was performed for overall survival by generation of Kaplan–Meier curves. Significance of differences between the groups was assessed using the log-rank test. For multivariate analysis, concordance regression (Dunkler et al, 2010) was applied, representing a generalisation of Cox proportional hazards regression, which is robust to violations of the proportional hazards assumption. P-values<0.05 were considered significant. All tests were done two sided.
Results
Characteristic distribution of inflammatory infiltrate in BTC
In BTC, T lymphocytes were the most prevalent inflammatory cell type (for exemplary photomicrographs, see Supplementary Figure 1). The majority of T lymphocytes were CD8+ T lymphocytes (64 cells per TMA spot) but CD4+ T lymphocytes were also frequently found (40 cells per spot; Supplementary Table 1). Correspondingly, CD8+ T lymphocytes showed a higher propensity towards infiltration of tumour epithelium (48.4% of cases), whereas only 36.3% of cases had intraepithelial CD4+ T lymphocyte infiltrates (Supplementary Table 2). Of the CD4+ T lymphocytes, only a subset was of the Foxp3+ regulatory T-cell-type (in median 5 out of 40, 12.5%, Supplementary Table 1). B lymphocytes were only infrequently observed. More than half of the tumours did not show any B lymphocyte infiltrate and only 1.4% of BTC showed B lymphocytes within the tumour epithelium (Supplementary Tables 1 and 2).
Macrophages were quite frequently encountered per total TMA dot (median of 72 cells) as well as in the tumour epithelium (77.6% of cases). Mast cells were infrequently seen with more than half of the tumours being completely negative. Within the tumour epithelium, mast cells were infrequent as well (4.3% of cases; Supplementary Tables 1 and 2). Total NK cell count was very low, with only 19.1% of tumours showing any infiltration of this cell type at all (Supplementary Table 2).
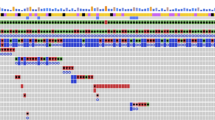
The total count of CD4+ T lymphocytes, CD8+ T lymphocytes, regulatory T lymphocytes, B lymphocytes, and mast cells was high in BilIN III, and showed a stepwise decrease in invasive tumours and their metastases (Figure 1). Similarly, NK cell content also decreased from BilIN III to the primary tumour (Supplementary Figure 2). On the contrary, the number of macrophages was increased in invasive tumours and metastases when compared with BilIN III (Figure 1).
Distribution of inflammatory cell infiltrates in non-invasive precursors (BilIN III), tumour margin, tumour centre, and metastatic lesions of BTC. Total number of CD4+ T lymphocytes (A), Foxp3+ regulatory T lymphocytes (B), CD8+ T lymphocytes (C), CD20+ B lymphocytes (D), CD68+ macrophages (E), CD117+ mast cells (F) in non-invasive precursors (BilIN III), tumour margin, tumour centre, and metastatic lesions of BTC.
The densities of specific immune cell types are correlated with each other and are partly associated with vessel density and proliferative activity
As expected, the total density of specific immune cell types was significantly correlated with the corresponding number of intraepithelial immune cells for all cell types evaluated (Figure 2). However, the statistical strength of correlations varied. Although for CD4+ T lymphocytes, CD8+ T lymphocytes, and macrophages strong correlations showing r-values well above 0.5 were observed, total and intraepithelial Foxp3+ regulatory T lymphocyte counts showed only a moderate association (r=0.41). This association was even weaker for B lymphocytes and mast cells (r=0.20 and r=0.24, respectively). The densities of CD4+ T lymphocytes, CD8+ T lymphocytes, and macrophages was quite strong, positively linked to each other, whereas the density of B lymphocytes, NK cells, and mast cells seemed to be independent. The total density of cytotoxic T cell, regulatory T lymphocytes, and macrophages was positively associated with proliferative capacity. This was also observed for intraepithelial infiltrates of regulatory T lymphocytes. All other inflammatory components did not correlate with the proliferation status. In general, the density of inflammatory cells was higher in tumours with a high microvessel count, but the respective associations of inflammatory cell numbers with vessel density were only weak (Figure 2).
Differences in the density of inflammatory infiltrate with respect to clinicopathological parameters and BTC subtypes
Apart from the total infiltration of regulatory and cytotoxic T lymphocytes, which was higher in older patients, age and sex were not associated with significant differences in the density of inflammatory cells (Supplementary Table 1). Higher UICC stages (specifically stage III) were associated with a modest increase in mast cell infiltrates (Supplementary Table 1). In contrast, NK cell counts decreased by trend in locally more advanced tumours (Supplementary Table 2). Regarding the intraepithelial density of inflammatory cells, a decrease of intraepithelial CD4+ T lymphocyte density with increasing UICC and pT stages (Supplementary Table 2) was observed. Total densities of CD4+ T lymphocytes, CD8+ T lymphocytes as well as B lymphocytes (single cells as well as aggregates) were significantly higher in low-grade than in high-grade tumours (Supplementary Tables 1 and 2; Supplementary Figure 3). Striking differences in the composition of inflammatory cells were noted for BTC subtypes. Although ECC and GBAC showed equal amounts of total CD8+ T lymphocytes (median 88 per TMA dot; Supplementary Table 1), numbers in ICC were significantly reduced (median 40 per TMA dot, P<0.001). Regulatory T lymphocytes were most frequent in GBAC (median 24 per TMA dot), followed by ECC (median 8 per TMA dot), and most infrequent in ICC (median 2 per TMA dot, P<0.001; Supplementary Table 1, Figure 3). In addition, mast cell counts were higher in ECC when compared with GBAC and ICC (median 20 vs 0, and 0 per TMA dot, P<0.001). However, these differences in total density did not translate into differences in the intraepithelial component for all cell types (Supplementary Table 2).
Distribution of inflammatory cell infiltrates in biliary tract cancers (BTC) and subtypes. Total number of CD4+ T lymphocytes (A), CD8+ T lymphocytes (B), Foxp3+ regulatory T lymphocytes (C), CD20+ B lymphocytes (D), CD68+ macrophages (E), and CD117+ mast cells (F) in BTC, extrahepatic cholangiocarcinoma (ECC), adenocarcinoma of the gallbladder (GBAC), and intrahepatic cholangiocarcinoma (ICC).
The number of intraepithelial lymphocytes is an independent predictor of patient survival in BTC
Classical survival prognosticators such as UICC stage and others proved to have high prognostic impact on our BTC cohort (Table 1). The presence of intraepithelial tumour-infiltrating CD4+ T lymphocytes as well as CD8+ T lymphocytes correlated significantly with a longer overall survival in BTC patients (P=0.002 and 0.015, respectively). Patients who had higher total regulatory T lymphocyte counts had a significantly better prognosis when compared with those patients whose tumour tissues showed lower regulatory T-lymphocyte counts (Figure 4F, P=0.018). Intraepithelial B lymphocytes were rarely observed and the few cases with intraepithelial cells did not differ with respect to prognosis. However, presence of total B lymphocytes had a positive prognostic impact (Figure 4H, P=0.032). The presence of B-lymphocyte aggregates, macrophages, or mast cells either total or within the tumour epithelium was not associated with significant differences in overall survival (Figure 4). Multivariate analysis under inclusion of UICC stage and tumour grade revealed a significant independent prognostic impact of the presence of either intraepithelial Foxp3+ regulatory T lymphocytes (HR: 0.492, P=0.002; Supplementary Table 3) or intraepithelial CD4+ T lymphocytes (HR: 0.595, P=0.008; Supplementary Table 4) but not of intraepithelial CD8+ T lymphocytes (HR: 0.840, P=0.363; data not shown) or total B lymphocytes (HR: 0.758, P=0.151; data not shown).
Overall survival probability in BTC patients stratified for inflammatory cell infiltrates. Kaplan–Meier curves depict overall survival probability stratified for either intraepithelial (A, C, E, I, K) or total (B, D, F, G, H, J, L) immune cell infiltrate of CD4+ T lymphocytes (A, B), CD8+ T lymphocytes (C, D), Foxp3+ regulatory T lymphocytes (E, F). CD20+ B lymphocytes (G, H), CD68+ macrophages (I, J), and CD117+ mast cells (K, L). P-values were calculated with a log-rank test.
The role of CD4+ and CD8+ T lymphocytes as a predictor of patient survival is subtype dependent in BTC
We analysed the impact of immune cells on survival regarding the major subtypes of BTC and found that the prognostic significance of the presence of intraepithelial T and B lymphocytes is dependent on the BTC subtype. Our data showed that in ECC and GBAC, the respective associations of lymphocyte infiltration and prognosis were retained for CD4+ T lymphocytes (Supplementary Figure 4), CD8+ T lymphocytes (Supplementary Figure 5), regulatory T lymphocytes (Supplementary Figure 6), and B lymphocytes (Supplementary Figure 7). In contrast to ECC and GBAC, all of these prognostic parameters lost their power in the subgroup of ICC (Supplementary Figures 4–7).
Discussion
In this study, we provide a comprehensive analysis of the inflammatory infiltrate in BTC by evaluating total and intraepithelial tumour-infiltrating CD4+, CD8+, Foxp3+, CD20+ lymphocytes, perforin+ NK cells, CD68+ macrophages, and CD117+ mast cells in a large and well-characterized BTC cohort. We decided not to include granulocytes in the analysis, as tumour infiltration by this cell type is heavily influenced by the presence of tumour cell necrosis and therefore difficult to analyse with respect to its biological relevance in a study design like ours.
We observed that general components of the adaptive immune response (T/B lymphocytes) decreased via the dysplasia – primary carcinoma – metastasis sequence, whereas components of the innate immune response (such as macrophages) increased. This observation is in line with a variety of functional data showing that in the course of carcinogenesis, neoplasms are able to learn how to evade an activation of the adaptive immune response (Dunn et al, 2004; Rabinovich et al, 2007).
In general, we observed that the adaptive immune response is beneficial for BTC patients and its activation is associated with longer overall survival times. In line with these results, some of the inflammatory cell types involved in this type of immune response have previously been linked to a more favourable outcome in other malignancies (Cho et al, 2003; Fukunaga et al, 2004; Galon et al, 2006; Mahmoud et al, 2011; Mlecnik et al, 2011). An explanation for this association is that these inflammatory cells represent a cell-mediated immune response against the tumour. However, the particular tumour-infiltrating immune cell type relevant for patient outcome may vary between different malignancies.
The role of CD8+ T lymphocytes in tumour progression has been examined in a variety of human malignancies (Oshikiri et al, 2003; Fukunaga et al, 2004; Galon et al, 2006; Mahmoud et al, 2011; Mlecnik et al, 2011). Most of these studies reported a beneficial prognostic effect of high intratumoural/intraepithelial CD8+ T lymphocyte counts – a finding, which we were able to expand to BTC in the present study. The role of CD4+ T lymphocytes in immunologic anticancer response is more controversial. It is generally accepted that CD4+ T lymphocytes may suppress tumour growth indirectly through cytokine production (Waldner et al, 2006). However, a low CD4/CD8 ratio has also been reported to be associated with better prognosis of patients in colorectal carcinoma (Diederichsen et al, 2003), suggesting an adverse effect of CD4+ T lymphocytes on the ability of CD8+ T lymphocytes to attack tumours in certain conditions. On the other hand, cooperation between CD4+ and CD8+ T lymphocytes has been described to improve patient outcome (Cho et al, 2003). We found a favourable prognostic impact of both intraepithelial tumour-infiltrating CD4+ and CD8+ T lymphocytes indicating a cooperative antitumour effect of these two T lymphocyte types in BTC.
Tumour cells can suppress immunity either by producing immunosuppressive molecules or by attracting other immune cell types, which in turn are able to suppress the immune reaction against the tumour. The latter mode of action has been suggested to be mediated at least in part by regulatory T lymphocytes (Zou, 2006; Liu et al, 2007). However, infiltration of regulatory T lymphocytes in vivo has been observed to be associated with inconsistent survival probabilities (Siddiqui et al, 2007; Sinicrope et al, 2009; Mathai et al, 2012; Yoon et al, 2012). In this BTC cohort, total tumour-infiltrating regulatory T lymphocytes were associated with a longer patient survival. Therefore, a prognostically relevant immunosuppressive effect of regulatory T lymphocytes is unlikely in BTC.
The functional contribution of B lymphocytes to the inflammatory response of solid tumours is not well understood. Here we present data that showed that the total tumour-infiltrating B lymphocyte count is correlated with a longer overall survival probability in BTC. Whether this observation just reflects an epiphenomenon in the context of immune response activation, or whether it is indicative of a true contribution of B lymphocytes to tumour control by the immune system should be determined in future studies.
Our data revealed that ECC, GBAC, and ICC are different regarding the prognostic importance of the inflammatory infiltrate. Although all three BTC subtypes are traditionally merged in the clinical context and are treated similarly with respect to chemotherapeutic approaches, there is evidence that this viewpoint might be oversimplified concerning the molecular basis of the BTC subtypes (Guedj et al, 2009; Cardinale et al, 2010; Komuta et al, 2012). The here-observed subtype-specific immune responses and their differing associations with patient survival suggest profound differences in the immune system – tumour interaction for the respective BTC subtypes. In this regard, one potentially important mechanism might be tumour immune escape. Immune escape mechanisms of tumour cells have been studied extensively in a variety of human cancers, including breast, prostate, pancreatic, oesophagus, and CRC (Du and Wang, 2011; Scott et al, 2012). However, concerning biliary malignancies and immune escape mechanisms, the number of available studies is limited. One major mechanism of immune escape is the downregulation of MHC I antigen on cancer cells by a number of different molecular alterations (Seliger, 2008; Seliger, 2012). Down-regulation of MHC I expression on cancer cells has been shown in a variety of human malignancies and mostly, but not exclusively, had a negative impact on patient survival (Natali et al, 1989; Facoetti et al, 2005; Meissner et al, 2005; Ogino et al, 2006; Han et al, 2008; Kasajima et al, 2010; Du and Wang, 2011). Further, the correct function of MHC I antigen is dependent on a network of intracellular proteins called the antigen-processing machinery (APM). We could recently demonstrate that besides down-regulation of MHC I, down-regulation of other components of the APM is also linked to the density of tumour-infiltrating lymphocytes and also correlates with poor patient survival in CRC (Kasajima et al, 2010). Such mechanisms might be underlying the failure of antitumour inflammation to improve prognosis in ICC observed in our study. This theory is strengthened by proposed differences for the cell of origin of ICC and ECC/GBAC. Although recently developed concepts of a stem cell phenotype in hepatocellular carcinoma/combined hepatocellular CC show stem cell features that are also encountered in classical ICC, the hilar/distal ECC and GBAC show a different stem cell phenotype originating from biliary tree stem cells (Bosman et al, 2010; Roskams et al, 2010; Komuta et al, 2012). It is known that several normal and cancer stem cells express minimal or no class I and II MHC (Kubota and Reid, 2000; Du and Wang, 2011). This knowledge has specifically been confirmed in human hepatic stem cells (Kubota and Reid, 2000; Rao et al, 2008). This might explain why ICC are able to evade damage induced by tumour immune response, which in turn would explain the missing association of inflammation and ameliorated patient outcome in this tumour subtype. However, further studies are necessary to prove that alterations in MHC-associated mechanisms are actually of importance in BTC. Another potential mechanism of tumour immune escape is Fas-mediated apoptosis of immune cells. Fas ligand (FasL) binding to death receptor Fas triggers apoptosis of Fas-expressing cells including tumour-infiltrating immune cells. Upregulation of FasL has been demonstrated in a variety of human neoplasms and was linked to survival (Du and Wang, 2011). In ICC, one study showed upregulation of FasL at early stages and downregulation of FasL at progressed stages, thereby indicating a potential role of this immune escape mechanism in cholangiocarcinogenesis (Shimonishi et al, 2000). Interestingly, in vitro experiments showed that primary and malignant cholangiocytes undergo CD40-mediated Fas-dependent apoptosis, but are insensitive to direct activation with exogenous FasL (Humphreys et al, 2010).
Recently, immune response modulating targeted drugs have been successfully tested as anticancer agents in a variety of human tumours (Weber et al, 2008; Brahmer et al, 2012; Kirkwood et al, 2012). As the clinical effect of these drugs is now explored in other neoplasias, our data may serve as a rationale to launch future clinical trials in BTC patients.
In conclusion, we report that the presence of both intratumoural T and B lymphocytes is correlated with a longer survival in BTC patients. In addition, we found that BTC subtypes show important differences in the composition and the prognostic relevance of immune cell infiltrate, that is, in ECC and GBAC, prognosis was inflammation linked, whereas in ICC no such association was observed. These data provide a solid basis for a better understanding of the biological role of inflammatory infiltrate in BTC and might therefore encourage future functional and clinical studies exploring the modulation of the inflammatory response for the benefit of BTC patients.
Change history
12 November 2013
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Blechacz B, Komuta M, Roskams T, Gores GJ (2011) Clinical diagnosis and staging of cholangiocarcinoma. Nat Rev Gastroenterol Hepatol 8 (9): 512–522.
Boon T, Cerottini JC, Van den Eynde B, van der Bruggen P, Van Pel A (1994) Tumor antigens recognized by T lymphocytes. Ann Rev Immunol 12: 337–365.
Bosman FT, Carneiro F, Hruban RH, Theise ND (2010) WHO Classification of Tumours of the Digestive System 4th edn International Agency for Research on Cancer (IARC): Lyon, France.
Brahmer JR, Tykodi SS, Chow LQ, Hwu WJ, Topalian SL, Hwu P, Drake CG, Camacho LH, Kauh J, Odunsi K, Pitot HC, Hamid O, Bhatia S, Martins R, Eaton K, Chen S, Salay TM, Alaparthy S, Grosso JF, Korman AJ, Parker SM, Agrawal S, Goldberg SM, Pardoll DM, Gupta A, Wigginton JM (2012) Safety and activity of anti-PD-L1 antibody in patients with advanced cancer. N Engl J Med 366 (26): 2455–2465.
Cardinale V, Semeraro R, Torrice A, Gatto M, Napoli C, Bragazzi MC, Gentile R, Alvaro D (2010) Intra-hepatic and extra-hepatic cholangiocarcinoma: new insight into epidemiology and risk factors. World J Gastrointest Oncol 2 (11): 407–416.
Cho Y, Miyamoto M, Kato K, Fukunaga A, Shichinohe T, Kawarada Y, Hida Y, Oshikiri T, Kurokawa T, Suzuoki M, Nakakubo Y, Hiraoka K, Murakami S, Shinohara T, Itoh T, Okushiba S, Kondo S, Katoh H (2003) CD4+ and CD8+ T cells cooperate to improve prognosis of patients with esophageal squamous cell carcinoma. Cancer Res 63 (7): 1555–1559.
Diederichsen AC, Hjelmborg J, Christensen PB, Zeuthen J, Fenger C (2003) Prognostic value of the CD4+/CD8+ ratio of tumour infiltrating lymphocytes in colorectal cancer and HLA-DR expression on tumour cells. Cancer Immunol Immunother 52 (7): 423–428.
Du C, Wang Y (2011) The immunoregulatory mechanisms of carcinoma for its survival and development. J Exp Clin Cancer Res 30: 12.
Dunkler D, Schemper M, Heinze G (2010) Gene selection in microarray survival studies under possibly non-proportional hazards. Bioinformatics 26 (6): 784–790.
Dunn GP, Old LJ, Schreiber RD (2004) The three Es of cancer immunoediting. Annu Rev Immunol 22: 329–360.
Facoetti A, Nano R, Zelini P, Morbini P, Benericetti E, Ceroni M, Campoli M, Ferrone S (2005) Human leukocyte antigen and antigen processing machinery component defects in astrocytic tumors. Clin Cancer Res 11 (23): 8304–8311.
Fukunaga A, Miyamoto M, Cho Y, Murakami S, Kawarada Y, Oshikiri T, Kato K, Kurokawa T, Suzuoki M, Nakakubo Y, Hiraoka K, Itoh T, Morikawa T, Okushiba S, Kondo S, Katoh H (2004) CD8+ tumor-infiltrating lymphocytes together with CD4+ tumor-infiltrating lymphocytes and dendritic cells improve the prognosis of patients with pancreatic adenocarcinoma. Pancreas 28 (1): e26–e31.
Galon J, Costes A, Sanchez-Cabo F, Kirilovsky A, Mlecnik B, Lagorce-Pages C, Tosolini M, Camus M, Berger A, Wind P, Zinzindohoue F, Bruneval P, Cugnenc PH, Trajanoski Z, Fridman WH, Pages F (2006) Type, density, and location of immune cells within human colorectal tumors predict clinical outcome. Science 313 (5795): 1960–1964.
Guedj N, Zhan Q, Perigny M, Rautou PE, Degos F, Belghiti J, Farges O, Bedossa P, Paradis V (2009) Comparative protein expression profiles of hilar and peripheral hepatic cholangiocarcinomas. J Hepatol 51 (1): 93–101.
Halama N, Michel S, Kloor M, Zoernig I, Benner A, Spille A, Pommerencke T, von Knebel DM, Folprecht G, Luber B, Feyen N, Martens UM, Beckhove P, Gnjatic S, Schirmacher P, Herpel E, Weitz J, Grabe N, Jaeger D (2011) Localization and density of immune cells in the invasive margin of human colorectal cancer liver metastases are prognostic for response to chemotherapy. Cancer Res 71 (17): 5670–5677.
Han LY, Fletcher MS, Urbauer DL, Mueller P, Landen CN, Kamat AA, Lin YG, Merritt WM, Spannuth WA, Deavers MT, De Geest K, Gershenson DM, Lutgendorf SK, Ferrone S, Sood AK (2008) HLA class I antigen processing machinery component expression and intratumoral T-Cell infiltrate as independent prognostic markers in ovarian carcinoma. Clin Cancer Res 14 (11): 3372–3379.
Hezel AF, Deshpande V, Zhu AX (2010) Genetics of biliary tract cancers and emerging targeted therapies. J Clin Oncol 28 (21): 3531–3540.
Humphreys EH, Williams KT, Adams DH, Afford SC (2010) Primary and malignant cholangiocytes undergo CD40 mediated Fas dependent apoptosis, but are insensitive to direct activation with exogenous Fas ligand. PLoS One 5 (11): e14037.
Kasajima A, Sers C, Sasano H, Johrens K, Stenzinger A, Noske A, Buckendahl AC, Darb-Esfahani S, Muller BM, Budczies J, Lehman A, Dietel M, Denkert C, Weichert W (2010) Down-regulation of the antigen processing machinery is linked to a loss of inflammatory response in colorectal cancer. Hum Pathol 41 (12): 1758–1769.
Kirkwood JM, Butterfield LH, Tarhini AA, Zarour H, Kalinski P, Ferrone S (2012) Immunotherapy of cancer in 2012. CA Cancer J Clin 62 (5): 309–335.
Komuta M, Govaere O, Vandecaveye V, Akiba J, Van Steenbergen W, Verslype C, Laleman W, Pirenne J, Aerts R, Yano H, Nevens F, Topal B, Roskams T (2012) Histological diversity in cholangiocellular carcinoma reflects the different cholangiocyte phenotypes. Hepatology 55 (6): 1876–1888.
Kubota H, Reid LM (2000) Clonogenic hepatoblasts, common precursors for hepatocytic and biliary lineages, are lacking classical major histocompatibility complex class I antigen. Proc Natl Acad Sci USA 97 (22): 12132–12137.
Liu VC, Wong LY, Jang T, Shah AH, Park I, Yang X, Zhang Q, Lonning S, Teicher BA, Lee C (2007) Tumor evasion of the immune system by converting CD4+CD25- T cells into CD4+CD25+ T regulatory cells: role of tumor-derived TGF-beta. J Immunol 178 (5): 2883–2892.
Mahmoud SM, Paish EC, Powe DG, Macmillan RD, Grainge MJ, Lee AH, Ellis IO, Green AR (2011) Tumor-infiltrating CD8+ lymphocytes predict clinical outcome in breast cancer. J Clin Oncol 29 (15): 1949–1955.
Mathai AM, Kapadia MJ, Alexander J, Kernochan LE, Swanson PE, Yeh MM (2012) Role of Foxp3-positive tumor-infiltrating lymphocytes in the histologic features and clinical outcomes of hepatocellular carcinoma. Am J Surg Pathol 36 (7): 980–986.
Meissner M, Reichert TE, Kunkel M, Gooding W, Whiteside TL, Ferrone S, Seliger B (2005) Defects in the human leukocyte antigen class I antigen processing machinery in head and neck squamous cell carcinoma: association with clinical outcome. Clin Cancer Res 11 (7): 2552–2560.
Mlecnik B, Tosolini M, Kirilovsky A, Berger A, Bindea G, Meatchi T, Bruneval P, Trajanoski Z, Fridman WH, Pages F, Galon J (2011) Histopathologic-based prognostic factors of colorectal cancers are associated with the state of the local immune reaction. J Clin Oncol 29 (6): 610–618.
Natali PG, Nicotra MR, Bigotti A, Venturo I, Marcenaro L, Giacomini P, Russo C (1989) Selective changes in expression of HLA class I polymorphic determinants in human solid tumors. Proc Natl Acad Sci USA 86 (17): 6719–6723.
Ogino T, Shigyo H, Ishii H, Katayama A, Miyokawa N, Harabuchi Y, Ferrone S (2006) HLA class I antigen down-regulation in primary laryngeal squamous cell carcinoma lesions as a poor prognostic marker. Cancer Res 66 (18): 9281–9289.
Oshikiri T, Miyamoto M, Shichinohe T, Suzuoki M, Hiraoka K, Nakakubo Y, Shinohara T, Itoh T, Kondo S, Katoh H (2003) Prognostic value of intratumoral CD8+ T lymphocyte in extrahepatic bile duct carcinoma as essential immune response. J Surg Oncol 84 (4): 224–228.
Patel T (2011) Cholangiocarcinoma—controversies and challenges. Nat Rev Gastroenterol Hepatol 8 (4): 189–200.
Rabinovich GA, Gabrilovich D, Sotomayor EM (2007) Immunosuppressive strategies that are mediated by tumor cells. Annu Rev Immunol 25: 267–296.
Rao MS, Khan AA, Parveen N, Habeeb MA, Habibullah CM, Pande G (2008) Characterization of hepatic progenitors from human fetal liver during second trimester. World J Gastroenterol 14 (37): 5730–5737.
Roskams T, Katoonizadeh A, Komuta M (2010) Hepatic progenitor cells: an update. Clin Liver Dis 14 (4): 705–718.
Scott AM, Wolchok JD, Old LJ (2012) Antibody therapy of cancer. Nat Rev Cancer 12 (4): 278–287.
Seliger B (2008) Molecular mechanisms of MHC class I abnormalities and APM components in human tumors. Cancer Immunol Immunother 57 (11): 1719–1726.
Seliger B (2012) Novel insights into the molecular mechanisms of HLA class I abnormalities. Cancer Immunol Immunother 61 (2): 249–254.
Shimonishi T, Isse K, Shibata F, Aburatani I, Tsuneyama K, Sabit H, Harada K, Miyazaki K, Nakanuma Y (2000) Up-regulation of fas ligand at early stages and down-regulation of Fas at progressed stages of intrahepatic cholangiocarcinoma reflect evasion from immune surveillance. Hepatology 32 (4 Pt 1): 761–769.
Siddiqui SA, Frigola X, Bonne-Annee S, Mercader M, Kuntz SM, Krambeck AE, Sengupta S, Dong H, Cheville JC, Lohse CM, Krco CJ, Webster WS, Leibovich BC, Blute ML, Knutson KL, Kwon ED (2007) Tumor-infiltrating Foxp3-CD4+CD25+ T cells predict poor survival in renal cell carcinoma. Clin Cancer Res 13 (7): 2075–2081.
Sinicrope FA, Rego RL, Ansell SM, Knutson KL, Foster NR, Sargent DJ (2009) Intraepithelial effector (CD3+)/regulatory (FoxP3+) T-cell ratio predicts a clinical outcome of human colon carcinoma. Gastroenterology 137 (4): 1270–1279.
Smyth MJ, Dunn GP, Schreiber RD (2006) Cancer immunosurveillance and immunoediting: the roles of immunity in suppressing tumor development and shaping tumor immunogenicity. Adv Immunol 90: 1–50.
Takagi S, Miyagawa S, Ichikawa E, Soeda J, Miwa S, Miyagawa Y, Iijima S, Noike T, Kobayashi A, Kawasaki S (2004) Dendritic cells, T-cell infiltration, and Grp94 expression in cholangiocellular carcinoma. Hum Pathol 35 (7): 881–886.
Waldner M, Schimanski CC, Neurath MF (2006) Colon cancer and the immune system: the role of tumor invading T cells. World J Gastroenterol 12 (45): 7233–7238.
Weber JS, O’Day S, Urba W, Powderly J, Nichol G, Yellin M, Snively J, Hersh E (2008) Phase I/II study of ipilimumab for patients with metastatic melanoma. J Clin Oncol 26 (36): 5950–5956.
Yoon HH, Orrock JM, Foster NR, Sargent DJ, Smyrk TC, Sinicrope FA (2012) Prognostic impact of FoxP3+ regulatory T cells in relation to CD8+ T lymphocyte density in human colon carcinomas. PLoS One 7 (8): e42274.
Zhang L, Conejo-Garcia JR, Katsaros D, Gimotty PA, Massobrio M, Regnani G, Makrigiannakis A, Gray H, Schlienger K, Liebman MN, Rubin SC, Coukos G (2003) Intratumoral T cells, recurrence, and survival in epithelial ovarian cancer. N Engl J Med 348 (3): 203–213.
Zou W (2006) Regulatory T cells, tumour immunity and immunotherapy. Nat Rev Immunol 6 (4): 295–307.
Acknowledgements
We thank Andrea Hain and John Moyers (Institute of Pathology, University of Heidelberg) for their excellent technical assistance. We also thank the NCT tissue bank Heidelberg for its support. This work was supported by a grant from the Deutsche Forschungsgemeinschaft (DFG) to P Schirmacher (SFB/TRR77).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
Supplementary Information accompanies this paper on British Journal of Cancer website
Supplementary information
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Goeppert, B., Frauenschuh, L., Zucknick, M. et al. Prognostic impact of tumour-infiltrating immune cells on biliary tract cancer. Br J Cancer 109, 2665–2674 (2013). https://doi.org/10.1038/bjc.2013.610
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2013.610
Keywords
This article is cited by
-
Clinical response to adding pyrotinib to pembrolizumab and lenvatinib for HER2-positive advanced intrahepatic cholangiocarcinoma: a case report
World Journal of Surgical Oncology (2023)
-
PD-L1 expression on immune cells, but not on tumor cells, is a favorable prognostic factor for patients with intrahepatic cholangiocarcinoma
Cancer Immunology, Immunotherapy (2023)
-
The role of tumor-infiltrating lymphocytes in cholangiocarcinoma
Journal of Experimental & Clinical Cancer Research (2022)
-
B cells and tertiary lymphoid structures as determinants of tumour immune contexture and clinical outcome
Nature Reviews Clinical Oncology (2022)