Abstract
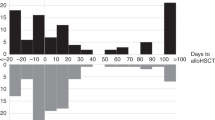
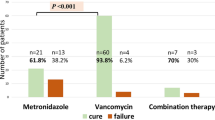
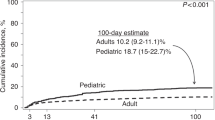
Clostridium difficile infection (CDI) is one of the leading causes of hospital-acquired infections in recent times. Hematopoietic stem cell transplantation (HSCT) confers increased risk for CDI because of prolonged hospital stay, immunosuppression, the need to use broad-spectrum antibiotics and a complex interplay of preparative regimen and GvHD-induced gut mucosal damage. Our study evaluated risk factors (RF) for recurrent CDI in HSCT recipients given the ubiquity of traditional RF for CDI in this population. Of the 499 allogeneic HSCT recipients transplanted between 2005 and 2012, 61 (12%) developed CDI within 6 months before transplant or 2 years after transplant and were included in the analysis. Recurrent CDI occurred in 20 (33%) patients. One year incidence of CDI recurrence was 31%. Multivariable analyses identified the number of antecedent antibiotics other than those used to treat CDI as the only significant RF for recurrence (hazard ratio 1.96, 95% confidence interval 1.09–3.52, P=0.025). Most recurrences occurred within 6 months of the first CDI, and the recurrence of CDI was associated with a trend for increased risk of mortality. This prompts the need for further investigation into secondary prophylaxis to prevent recurrent CDI.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Alonso CD, Treadway SB, Hanna DB, Huff CA, Neofytos D, Carroll KC et al. Epidemiology and outcomes of Clostridium difficile infections in hematopoietic stem cell transplant recipients. Clin Infect Dis 2012; 54: 1053–1063.
Alonso CD, Dufresne SF, Hanna DB, Labbe AC, Treadway SB, Neofytos D et al. Clostridium difficile infection after adult autologous stem cell transplantation: a multicenter study of epidemiology and risk factors. Biol Blood Marrow Transplant 2013; 19: 1502–1508.
Willems L, Porcher R, Lafaurie M, Casin I, Robin M, Xhaard A et al. Clostridium difficile infection after allogeneic hematopoietic stem cell transplantation: incidence, risk factors, and outcome. Biol Blood Marrow Transplant 2012; 18: 1295–1301.
Arango JI, Restrepo A, Schneider DL, Callander NS, Ochoa-Bayona JL, Restrepo MI et al. Incidence of Clostridium difficile-associated diarrhea before and after autologous peripheral blood stem cell transplantation for lymphoma and multiple myeloma. Bone Marrow Transplant 2006; 37: 517–521.
Chopra T, Chandrasekar P, Salimnia H, Heilbrun LK, Smith D, Alangaden GJ . Recent epidemiology of Clostridium difficile infection during hematopoietic stem cell transplantation. Clin Transplant 2011; 25: E82–E87.
Dubberke ER, Reske KA, Srivastava A, Sadhu J, Gatti R, Young RM et al. Clostridium difficile-associated disease in allogeneic hematopoietic stem-cell transplant recipients: risk associations, protective associations, and outcomes. Clin Transplant 2010; 24: 192–198.
Chakrabarti S, Lees A, Jones SG, Milligan DW . Clostridium difficile infection in allogeneic stem cell transplant recipients is associated with severe graft-versus-host disease and non-relapse mortality. Bone Marrow Transplant 2000; 26: 871–876.
Trifilio SM, Pi J, Mehta J . Changing epidemiology of Clostridium difficile-associated disease during stem cell transplantation. Biol Blood Marrow Transplant 2013; 19: 405–409.
Johnson S . Recurrent Clostridium difficile infection: a review of risk factors, treatments, and outcomes. J Infect 2009; 58: 403–410.
Garey KW, Sethi S, Yadav Y, DuPont HL . Meta-analysis to assess risk factors for recurrent Clostridium difficile infection. J Hosp Infect 2008; 70: 298–304.
Cadena J, Thompson GR 3rd, Patterson JE, Nakashima B, Owens A, Echevarria K et al. Clinical predictors and risk factors for relapsing Clostridium difficile infection. Am J Med Sci 2010; 339: 350–355.
Eyre DW, Walker AS, Wyllie D, Dingle KE, Griffiths D, Finney J et al. Predictors of first recurrence of Clostridium difficile infection: implications for initial management. Clin Infect Dis 2012; 55: S77–S87.
Cohen SH, Gerding DN, Johnson S, Kelly CP, Loo VG, McDonald LC et al. Clinical practice guidelines for Clostridium difficile infection in adults: 2010 update by the society for healthcare epidemiology of America (SHEA) and the infectious diseases society of America (IDSA). Infect Control Hosp Epidemiol 2010; 31: 431–455.
Kamboj M, Son C, Cantu S, Chemaly RF, Dickman J, Dubberke E et al. Hospital-onset Clostridium difficile infection rates in persons with cancer or hematopoietic stem cell transplant: a C3IC network report. Infect Control Hosp Epidemiol 2012; 33: 1162–1165.
Rowlings PA, Przepiorka D, Klein JP, Gale RP, Passweg JR, Henslee-Downey PJ et al. IBMTR Severity Index for grading acute graft-versus-host disease: retrospective comparison with Glucksberg grade. Br J Haematol 1997; 97: 855–864.
Fine JP, Gray RJ . A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc 1999; 94: 496–509.
Huang AM, Marini BL, Frame D, Aronoff DM, Nagel JL . Risk factors for recurrent Clostridium difficile infection in hematopoietic stem cell transplant recipients. Transpl Infect Dis 2014; 16: 744–750.
Khanna S, Pardi DS, Aronson SL, Kammer PP, Orenstein R, St Sauver JL et al. The epidemiology of community-acquired Clostridium difficile infection: a population-based study. Am J Gastroenterol 2012; 107: 89–95.
Stevens V, Dumyati G, Fine LS, Fisher SG, van Wijngaarden E . Cumulative antibiotic exposures over time and the risk of Clostridium difficile infection. Clin Infect Dis 2011; 53: 42–48.
Hensgens MP, Goorhuis A, Dekkers OM, Kuijper EJ . Time interval of increased risk for Clostridium difficile infection after exposure to antibiotics. J Antimicrob Chemother 2012; 67: 742–748.
Hosokawa K, Takami A, Tsuji M, Araoka H, Ishiwata K, Takagi S et al. Relative incidences and outcomes of Clostridium difficile infection following transplantation of unrelated cord blood, unrelated bone marrow, and related peripheral blood in adult patients: a single institute study. Transpl Infect Dis 2014; 16: 412–420.
Hunt JJ, Ballard JD . Variations in virulence and molecular biology among emerging strains of Clostridium difficile. Microbiol Mol Biol Rev 2013; 77: 567–581.
Swale A, Miyajima F, Kolamunnage-Dona R, Roberts P, Little M, Beeching NJ et al. Serum mannose-binding lectin concentration, but not genotype, is associated with Clostridium difficile infection recurrence: a prospective cohort study. Clin Infect Dis 2014; 59: 1429–1436.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
SBM is the principal investigator of a multicenter study sponsored by Merck Pharmaceuticals, manufacturer of Fidaxomicin. The remaining authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Mani, S., Rybicki, L., Jagadeesh, D. et al. Risk factors for recurrent Clostridium difficile infection in allogeneic hematopoietic cell transplant recipients. Bone Marrow Transplant 51, 713–717 (2016). https://doi.org/10.1038/bmt.2015.311
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bmt.2015.311