Abstract
Background/objectives:
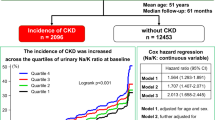
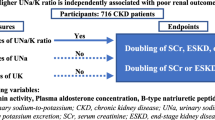
An increased risk of mortality and cardiovascular disease (CVD) is observed in people with chronic kidney disease (CKD) even in early stages. Dietary sodium intake has been associated with important CVD and CKD progression risk factors such as hypertension and proteinuria in this population. We aimed to investigate the relationship between sodium intake and CVD or CKD progression risk factors in a large cohort of patients with CKD stage 3 recruited from primary care.
Subjects/methods:
A total of 1733 patients with previous estimated glomerular filtration rate (eGFR) of 30–59 ml/min/1.73m2, with a mean age 72.9±9.0 years, were recruited from 32 general practices in primary care in England. Medical history was obtained and participants underwent clinical assessment, urine and serum biochemistry testing. Sodium intake was estimated from three early-morning urine specimens using an equation validated for this study population.
Results:
Sixty percent of participants who had estimated sodium intake above recommendation (>100 mmol/day or 6 g salt/day) also had higher diastolic blood pressure, mean arterial pressure (MAP), urinary albumin-to-creatinine ratio, high-sensitive C-reactive protein and uric acid and used a greater number of anti-hypertensive drugs. In multivariable regression analysis, excessive sodium intake was an independent predictor of MAP (B=1.57, 95% confidence interval (CI) 0.41–2.72; P=0.008) and albuminuria (B=1.35, 95% CI 1.02–1.79; P=0.03).
Conclusions:
High sodium intake was associated with CVD and CKD progression risk factors in patients with predominantly early stages of CKD followed up in primary care. This suggests that dietary sodium intake could afffect CVD risk even in early or mild CKD. Intervention studies are warranted to investigate the potential benefit of dietary advice to reduce sodium intake in this population.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Go AS, Chertow GM, Fan DJ, McCulloch CE, Hsu CY . Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med 2004; 351: 1296–1305.
Matsushita K, van der Velde M, Astor BC, Woodward M, Levey AS, De Jong PE et al. Chronic Kidney Disease Prognosis Consortium. Association of estimated glomerular filtration rate and albuminuria with all-cause and cardiovascular mortality in general population cohorts: a collaborative meta-analysis. Lancet 2010; 375: 2073–2081.
Vanholder R, Massy Z, Argiles A, Spasovski G, Verbeke F, Lameire N . European Uremic Toxin Work Group: chronic kidney disease as cause of cardiovascular morbidity and mortality. Nephrol Dial Transplant 2005; 20: 1048–1056.
Rein P, Saely CH, Vonbank A, Boehnel C, Drexel H . Usefulness of serial decline of kidney function to predict mortality and cardiovascular events in patients undergoing coronary angiography. Am J Cardiol 2014; 113: 215–221.
Basile JN . Recognizing the link between CKD and CVD in the primarycare setting: Accurate and early diagnosis for timely and appropriate intervention. South Med J 2007; 100: 499–505.
Lambers Heerspink HJ, de Borst MH, Bakker SJ, Navis GJ . Improving the efficacy of RAAS blockade in patients with chronic kidney disease. Nat Rev Nephrol 2013; 9: 112–121.
McMahon EJ, Bauer JD, Hawley CM, Isbel NM, Stowasser M, Johnson DW et al. A randomized trial of dietary sodium restriction in CKD. J Am Soc Nephrol. 2013; 24: 2096–2103.
Graudal NA, Hubeck-Graudal T, Jürgens G . Effects of low-sodium diet vs. high-sodium diet on blood pressure, renin, aldosterone, catecholamines, cholesterol, and triglyceride (Cochrane Review). Am J Hypertens 2012; 25: 1–15.
Al-Solaiman Y, Jesri A, Zhao Y, Morrow JD, Egan BM . Low-sodium DASH reduces oxidative stress and improves vascular function in saltsensitive humans. J Hum Hypertens 2009; 23: 826–835.
Kitiyakara C, Chabrashvili T, Chen Y, Blau J, Karber A, Aslam S et al. Salt intake, oxidative stress, and renal expression of NADPH oxidase and superoxide dismutase. J Am Soc Nephrol. 2003; 14: 2775–2782.
Sanders PW . Dietary salt intake, salt sensitivity, and cardiovascular health. Hypertension 2009; 53: 442–445.
Vegter S, Perna A, Postma MJ, Navis G, Remuzzi G, Ruggenenti P . Sodium intake, ACE inhibition, and progression to ESRD. J Am Soc Nephrol. 2012; 23: 165–173.
Kidney Disease Outcomes Quality Initiative (K/DOQI). K/DOQI clinical practice guidelines on hypertension and antihypertensive agents in chronic kidney disease. Am J Kidney Dis 2004; 43: S1–290.
MacGregor MS, Taal MW . Renal Association Clinical Practice Guideline on detection, monitoring and management of patients with CKD. Nephron Clin Pract 2011; 118 (Suppl 1): c71–c100.
Yu W, Luying S, Haiyan W, Xiaomei L . Importance and benefits of dietary sodium restriction in the management of chronic kidney disease patients: experience from a single Chinese center. Int Urol Nephrol 2012; 44: 549–556.
Ogura M, Kimura A, Takane K, Nakao M, Hamaguchi A, Terawaki H et al. Estimation of salt intake from spot urine samples in patients with chronic kidney disease. BMC Nephrol 2012; 13: 36–42.
Kutlugün AA, Arici M, Yildirim T, Turgut D, Yılmaz R, Altındal M et al. Daily sodium intake in chronic kidney disease patients during nephrology clinic follow-up: an observational study with 24-hour urine sodium measurement. Nephron Clin Pract 2011; 118: c361–c366.
McIntyre NJ, Fluck RJ, McIntyre CW, Taal MW . Risk profile in chronic kidney disease stage 3: older versus younger patients. Nephron Clin Pract. 2011; 119: c269–c276.
Andrassy KM . 2012 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease. Kidney Int Suppl 2013; 3: 1–150.
McIntyre NJ, Fluck RJ, McIntyre CW, Taal MW . Skin autofluorescence and the association with renal and cardiovascular risk factors in Chronic Kidney Disease stage 3. Clin J Am Soc Nephrol 2011; 6: 2356–2363.
World Health Organisation Global Database on Body Mass Index: 2013 [http://apps.who.int/bmi/index.jsp?introPage=intro_3.html]. Accessed on 20 October 2013.
World Health Organization. The Definition and Diagnosis of Diabetes Mellitus and Intermediate Glycaemia. WHO: Geneva, Switzerland, 2006.
Nerbass FB, Pecoits-Filho R, McIntyre NJ, McIntyre CW, Taal MW . Development of a formula for estimation of sodium intake from spot urine in people with chronic kidney disease. Nephron Clin Pract 2014 (in press).
Nerbass FB, Pecoits-Filho R, McIntyre NJ, McIntyre CW, Willingham FC, Taal MW . Demographic associations of high estimated sodium intake and frequency of consumption of high sodium foods in people with CKD stage 3 in England. J Ren Nutr 2014; 24: 236–242.
Lambers-Heerspink HJ, Holtkamp FA, Parving HH, Navis GJ, Lewis JB, Ritz E et al. Moderation of dietary sodium potentiates the renal and cardiovascular protective effects of angiotensin receptor blockers. Kidney Int 2012; 82: 330–337.
Elliott P, Stamler J, Nichols R, Stamler R, Kesteloot H, Marmot M . INTERSALT revisited: further analyses of 24 h urinary sodium excretion and blood pressure within and across populations INTERSALT Cooperative Research Group. Br Med J 1996; 312: 1249–1253.
Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N Engl J Med 2001; 344: 3–10.
Koomans HA, Roos JC, Boer P, Geyskes GG, Mees EJ . Salt sensitivity of blood pressure in chronic renal failure. Hypertension 1982; 4: 190–197.
Luther JM . Sodium intake, ACE inhibition, and progression to ESRD. J Am Soc Nephrol 2012; 23: 10–12.
Vogt L, Waanders F, Boomsma F . de Zeeuw D, Navis G. Effects of dietary sodium and hydrochlorothiazide on the antiproteinuric efficacy of losartan. J Am Soc Nephrol. 2008 May; 19: 999–1007.
Heran BS, Wong MM, Heran IK, Wright JM . Blood pressure lowering efficacy of angiotensin converting enzyme (ACE) inhibitors for primary hypertension. Cochrane Database Syst Rev 2008, CD003823.
Yilmaz R1, Akoglu H, Altun B, Yildirim T, Arici M, Erdem Y . Dietary salt intake is related to inflammation and albuminuria in primary hypertensive patients. Eur J Clin Nutr 2012; 66: 1214–1218.
The GISEN Group (Gruppo Italiano di Studi Epidemiologici in Nefrologia). Randomised placebo-controlled trial of effect of ramipril on decline in glomerular filtration rate and risk of terminal renal failure in proteinuric, non-diabetic nephropathy. Lancet 1997; 349: 1857–1863.
Ruggenenti P, Perna A, Remuzzi G . GISEN GroupInvestigators. Retarding progression of chronic renal disease: The neglected issue of residual proteinuria. Kidney Int 2003; 63: 2254–2261.
Ekinci EI, Thomas G, Thomas D, Johnson C, Macisaac RJ, Houlihan CA et al. Effects of salt supplementation on the albuminuric response to telmisartan with or without hydrochlorothiazide therapy in hypertensive patients with type 2 diabetes are modulated by habitual dietary salt intake. Diabetes Care 2009; 32: 1398–1403.
Krikken JA, Laverman GD, Navis G . Benefits of dietary sodium restrictionin the management of chronic kidney disease. Curr Opin Nephrol Hypertens 2009; 18: 531–538.
Fogarty AW, Lewis SA, McKeever TM, Britton JR . Is higher sodium intake associated with elevated systemic inflammation? A population-based study. Am J Clin Nutr 2009; 89: 1901–1904.
Forman JP, Scheven L, de Jong PE, Bakker SJ, Curhan GC, Gansevoort RT . Association between sodium intake and change in uric acid, urine albumin excretion, and the risk of developing hypertension. Circulation 2012; 125: 3108–3116.
Acknowledgements
This study was supported by a fellowship a grants from Kidney Research UK and British Renal Society (awarded to NJM) and the CAPES Foundation - Ministry of Education of Brazil (awarded to FN), as well as an unrestricted educational grant from Roche Products plc. This collaboration was facilitated by the Sister Renal Centers Program of the International Society of Nephrology.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Nerbass, F., Pecoits-Filho, R., McIntyre, N. et al. High sodium intake is associated with important risk factors in a large cohort of chronic kidney disease patients. Eur J Clin Nutr 69, 786–790 (2015). https://doi.org/10.1038/ejcn.2014.215
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2014.215
This article is cited by
-
Efficacy of comprehensive group-based education in lowering body weight, uric acid levels, and diuretic use in patients with chronic kidney disease: a retrospective study
BMC Nephrology (2023)
-
Association between urinary salt excretion and albuminuria in Japanese patients with chronic kidney disease: the Fukuoka kidney disease registry study
Clinical and Experimental Nephrology (2021)
-
Is socio-demographic status, body mass index, and consumption of food away from home associated with high sodium intake among adults in Malaysia?: findings from the Malaysian Community Salt Survey (MyCoSS)
Journal of Health, Population and Nutrition (2021)
-
International consensus statement on the diagnosis and management of autosomal dominant polycystic kidney disease in children and young people
Nature Reviews Nephrology (2019)
-
Dietary sources of energy and nutrient intake among children and adolescents with chronic kidney disease
Pediatric Nephrology (2017)