Abstract
Background/Objectives:
Iodine nutritional status and its influence on thyroid function have been thoroughly investigated in many places in China, but little is known about Xinjiang province, where multiple minorities are living in a special geographical location and have different lifestyles compared with people from other parts of China. The aim of this study was to evaluate iodine status and thyroid disorders in two major ethnic groups living in the Xinjiang region of China.
Subjects/Methods:
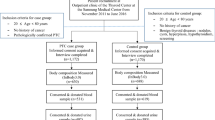
A total of 2253 residents over the age of 18 years who had lived in Xinjiang for more than 3 years were enrolled. Urinary iodine concentration (UIC), serum thyroid hormone concentrations and thyroid autoantibodies were measured, and thyroid ultrasonography was performed.
Results:
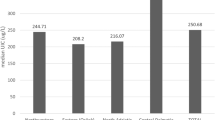
The median UIC was 130.7 μg/l in adults. Among the subjects, those with deficient UIC levels were 34.4%. The prevalence of overt hyper- and hypothyroidism in the iodine-deficient group was higher than in the iodine-sufficient group (1.3% vs 0%, χ2=3.891, P=0.049; 4.8% vs 2.8%, χ2=8.715, P=0.003, respectively), and subclinical hypothyroidism was more frequent in the iodine-deficient group than in the iodine-excess group (19.6% vs 12.5%, χ2=4.529, P=0.033).
Conclusions:
One-third of the population is still iodine deficient in Xinjiang. Uyghur females are more susceptible to hypothyroidism and thyroid autoimmune diseases. Thyroid disorders, especially hyper/hypothyroidism and subclinical hypothyroidism, are more likely to be prevalent in an iodine-deficient population.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Teng W, Shan Z, Teng X, Guan H, Li Y, Teng D et al. Effect of iodine intake on thyroid diseases in China. N Engl J Med 2006; 354: 2783–2793.
Du Y, Gao Y, Meng F, Liu S, Fan Z, Wu J et al. Iodine deficiency and excess coexist in china and induce thyroid dysfunction and disease: a cross-sectional study. PLoS One 2014; 9: e111937.
Pearce EN, Andersson M, Zimmermann MB . Global iodine nutrition: where do we stand in 2013? Thyroid 2013; 23: 523–528.
Jin J (ed). Xinjiang Uyghur Autonomous Region Bureau of Statistics, Xinjiang Statistical Yearbook. China Statistics Press: Beijing, China. 2010 p, 640.
Wang F, Zhang L, Aihete A, Pinjiang M, Shaniya Y et al. Effect of iodine deficiency disease control and disease prediction from 1995 to 2011. Chin J Endemiol 2014; 33: 33.
Xin S, Shan Z, Teng W . Effects of increased iodine intake on thyroid disorders. Endocrinol Metab 2014; 29: 240–247.
Sang Z, Wang PP, Yao Z, Shen J, Halfyard B, Tan L et al. Exploration of the safe upper level of iodine intake in euthyroid Chinese adults: a randomized double-blind trial. Am J Clin Nutr 2012; 95: 367–373.
The guideline for diagnosis and management of thyroid disease of China. The Society of Endocrinology, Chinese Medical Association, 2008. Available at: http://www.cma.org.cn accessed 27 November 2008.
World Health Organization United Nations Children’s Fund, and International Council for the Control of Iodine Deficiency Disorders Assessment of Iodine Deficiency Disorders and Monitoring Their Elimination: A Guide for Programme Managers. World Health Organization: Geneva, Switzerland, 2007, pp 32–34.
Lu Z, Lu Z, Zhu Y, Yan Z, Liu X, Yan W et al. Enhanced hypertension prevalence in non-Han Chinese minorities from Xinjiang Province, China. Hypertens Res 2009; 32: 1097–1103.
The China Salt Substitute Study Collaborative Group. Salt substitution: a low-cost strategy for blood pressure control among rural Chinese. A randomized, controlled trial. J Hypertens 2007; 25: 2011–2018.
Teng X, Hu F, Teng W, Wang H, Shong S, Shan Z et al. The study of thyroid disease in a community not using iodized salt. Chin J Prev Med 2002; 3: 176–179.
Meng F, Zhao R, Liu P, Liu L, Liu S . Assessment of iodine status in children, adults, pregnant women and lactating women in iodine-replete areas of China. PLoS One 2013; 8: e81294.
Teng W, Xing XP, Tong NW et al. An epidemiological survey of thyroid disease of China cities [J]. Proceedings of the Ninth National Conference of Endocinology of Chinese Medical Association 2010, Dalian, Liaoning, PL-07.
Lockshin MD . Sex differences in autoimmune disease. Lupus 2006; 15: 753–756.
Chagnon P, Provost S, Belisle C, Bolduc V, Gingras M, Busque L . Age-associated skewing of X-inactivation ratios of blood cells in normal females: a candidate-gene analysis approach. Exp Hematol 2005; 33: 1209–1214.
Hernández-Molina G, Svyryd Y, Sánchez-Guerrero J, Mutchinick OM . The role of the X-chromosome in immunity and autoimmunity. Autoimmun Rev 2007; 6: 218–222.
Jacobson EM, Hubera A, Tomer Y . The HLA gene complex in thyroid autoimmunity: from epidemiology to etiology. J Autoimmun 2008; 30: 58–62.
Laurberg P, Jorgensen T, Perrild H, Ovesen L, Knudsen N, Pedersen IB et al. The Danish investigation on iodine intake and thyroid disease, DanThyr: status and perspectives. Eur J Endocrinol 2006; 155: 219–228.
Bülow Pedersen I, Laurberg P, Knudsen N, Jorgensen T, Perrild H, Ovesen L et al. A population study of the association between thyroid autoantibodies in serum and abnormalities in thyroid function and structure. Clin Endocrinol (Oxf) 2005; 62: 713–720.
Szabolcs I, Podoba J, Feldkamp J, Dohan O, Farkas I, Sajgo M et al. Comparative screening for thyroid disorders in old age in areas of iodine deficiency, long-term iodine prophylaxis and abundant iodine intake. Clin Endocrinol (Oxf) 1997; 47: 87–92.
Mostbeck A, Galvan G, Bauer P, Eber O, Atefie K, Dam K et al. The incidence of hyperthyroidism in Austria from 1987 to 1995 before and after an increase in salt iodization in 1990. Eur J Nucl Med 1998; 25: 367–374.
Mingchen Z, Zhang L, Fan Y, Zeng X, Zhu Y, Abulikemu Z et al. Relationship between iodine intake and the prevalence of thyroid disease in Urumqi, Xinjiang. Chin J Endocrinol Metab 2011; 27: 972–974.
Malinowski JR, Denny JC, Bielinski SJ, Basford MA, Bradford Y, Peissig PL et al. Genetic variants associated with serum thyroid stimulating hormone (TSH) levels in European Americans andAfrican Americans from the eMERGE Network. PLoS One 2014; 9: e111301.
Hollowell JG, Staehling NW, Flanders WD, Hannon WH, Gunter EW, Spencer CA et al. Serum TSH, T(4), and thyroid antibodies in the United States population (1988 to 1994): National Health and Nutrition Examination Survey (NHANES III). J Clin Endocrinol Metab 2002; 87: 489–499.
Zois C, Stavrou I, Kalogera C, Svarna E, Dimoliatis I, Seferiadis K et al. High prevalence of autoimmune thyroiditis in schoolchildren after elimination of iodine deficiency in northwestern Greece. Thyroid 2003; 13: 485–489.
Chen Z, Xu W, Huang Y, Jin X, Deng J, Zhu S et al. Associations of noniodized salt and thyroid nodule among the Chinese population: a large cross-sectional study. Am J Clin Nutr 2013; 98: 684–692.
Acknowledgements
We thank all the participants in this survey. This study was supported by ‘Natural Science Foundation of Xinjiang Uyghur Autonomous Region’ (2013211A105).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Guo, Y., Zynat, J., Xu, Z. et al. Iodine nutrition status and thyroid disorders: a cross-sectional study from the Xinjiang Autonomous Region of China. Eur J Clin Nutr 70, 1332–1336 (2016). https://doi.org/10.1038/ejcn.2016.82
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2016.82
This article is cited by
-
Effects of long-term excessive iodine intake on blood lipids in Chinese adults: a cross-sectional study
European Journal of Clinical Nutrition (2021)
-
Identifying potential metabolic tissue biomarkers for papillary thyroid cancer in different iodine nutrient regions
Endocrine (2021)
-
Iodine Nutrition and the Prevalence Status of Thyroid Nodules in the Population: a Cross-sectional Survey in Heilongjiang Province, China
Biological Trace Element Research (2021)
-
Effects of Excessive Iodine Intake on Blood Glucose, Blood Pressure, and Blood Lipids in Adults
Biological Trace Element Research (2019)