Abstract
Arterial stiffness exemplified by the ambulatory arterial stiffness index (AASI) and pulse pressure (PP) predicts cardiovascular morbidity and mortality. The present cross-sectional study assessed the association of renal function with AASI and 24-h PP in hypertensive inpatients. Subjects included 948 hypertensive inpatients with drug treatment (mean age, 53.3 years; male, 67.1%). The AASI was defined as 1 minus the regression slope of diastolic over systolic blood pressure readings obtained from 24-h recordings. Renal function was evaluated by serum creatinine and urinary albumin excretion was expressed by the urinary albumin-to-urinary creatinine ratio (ACR), and estimated glomerular filtration rate (eGFR) was calculated by the modification of diet in renal disease formula and chronic kidney disease-epidemiology collaboration formula. As AASI and 24-h PP increased, serum creatinine concentrations and ACR increased, and eGFR decreased. Multiple linear regression showed that AASI and 24-h PP were associated with eGFR-EPI (B=−12.00, P=0.001 vs. B=−0.14, P=0.002) and ACR (B=0.56, P=0.004 vs. B=0.01, P=0.017) independent of other cardiovascular risk factors. After additional adjustment for 24-h PP, the association of AASI with eGFR-EPI had borderline significance (P=0.053), whereas the significant associations of 24-h PP with serum creatinine and ACR persisted (P=0.009 and P=0.006) after adjusting for confounding factors and AASI. Multiple logistic regression analysis showed that each s.d. increase in 24-h PP (that is, 13 mm Hg) was associated with a higher risk of suffering from microalbuminuria (MA) by 39% (P=0.038) after additional adjustment for AASI. In conclusion, AASI is more closely associated with eGFR compared with 24-h PP in hypertensive inpatients. However, for MA 24-h PP is a better predictor.
Similar content being viewed by others
Introduction
Arterial stiffness is a strong predictor of cardiovascular morbidity and mortality in patients with hypertension.1, 2 Pulse pressure (PP), a traditional marker of arterial stiffness, has been shown to be associated with cardiovascular mortality.3, 4, 5 In 2006, Li et al.6 proposed a novel, easy-to-obtain index of arterial stiffness, called the ambulatory arterial stiffness index (AASI). The AASI is defined as 1 minus the regression slope of diastolic blood pressure (DBP) plotted against systolic blood pressure (SBP) obtained from individual 24-h blood pressure (BP) recordings. AASI is correlated with classical measurements of arterial stiffness and predicts cardiovascular mortality in hypertensive patients and in the general population.6, 7, 8
Generally, renal insufficiency is one of the important target organ damage (TOD) in hypertensive patients. Cardiovascular events progressively increase as renal function declines in patients, even in cases of mild renal insufficiency.9 Alteration of arterial stiffness, a subclinical sign of TOD in hypertension, has been reported to be correlated with renal function within the normal range10 or in renal dysfunction.11, 12, 13, 14, 15, 16, 17 As a surrogate index of arterial stiffness, PP is correlated with early signs of renal dysfunction.18, 19 Similar to PP, AASI is also associated with TOD20 and renal abnormalities21, 22 in untreated patients with primary hypertension. However, clinically most hypertensive patients receive state-of-the-art anti-hypertensive therapy, which may have a protective role for arterial and renal function.23, 24, 25, 26 Therefore, it is largely unknown whether AASI and PP are indicators for renal function in these treated inpatients. Therefore, the present study aimed to determine the association of indices of renal function, such as serum creatinine, estimated glomerular filtration rate (eGFR) and microalbuminuria (MA) with AASI and PP in a large group of primary hypertensive inpatients with drug treatment, and to determine which index is more closely correlated with renal damage.
Methods
Study population
From January 2006 to December 2008, 1660 consecutive inpatients with antihypertensive treatment from the Department of Hypertension, Shanghai Ruijin Hospital were included in the present study. Exclusion criteria included life-threatening disease, secondary hypertension, atrial fibrillation and other arrhythmias. We excluded 712 patients for the following reasons: blood measurements were not available at baseline (n=567); ambulatory blood pressure readings were <10 times during daytime or <5 times during nighttime or <20 times during 24 h (n=11); not all of the cardiovascular risk factors had been recorded (n=114) and the patient’s age was <18 years or >90 years (n=20). Therefore, the total number of patients included in the present analysis was 948. T2DM was diagnosed using the following criteria: (i) fasting plasma glucose levels ⩾7.0 mmol l−1 on two occasions; (ii) two 2-h postprandial plasma glucose readings ⩾11.1 mmol l−1 after a glucose load of 75 g; (iii) two casual glucose readings ⩾11.1 mmol l−1 or (iv) treatment with oral hypoglycemic drugs or parenteral insulin. The study protocol was approved by the ethics committee of Ruijin Hospital, and written informed consent was obtained from all participants.
Ambulatory BP and AASI
Ambulatory BP was recorded using an oscillometric SpaceLabs 90217 (SpaceLabs Inc., Redmond, WA, USA) monitor that obtained blood pressure readings at 20-min intervals from 0600 hours to 2200 hours and at 30-min intervals from 2200 hours to 00600 hours. From 24-h BP readings, we computed the regression slope of DBP on SBP. AASI was 1 minus the regression slope. We did not force the slope through the origin.
Glomerular filtration rate and urinary albumin excretion
Glomerular filtration rate was estimated by the modification of diet in renal disease (MDRD) formula27 and chronic kidney disease-epidemiology collaboration (CKD-EPI) formula.28 Urinary albumin excretion was assessed from a morning fasting spot urine sample by the urinary albumin-to-urinary creatinine ratio (ACR). Urinary creatinine concentration was measured by an automatic biochemistry analyzer (Beckman CX7, Chaska, MN, USA) and urinary albumin concentration was measured by means of particle-enhanced turbidimetric immunoassay (Beckman CX7). MA was defined as an albumin–creatinine ratio ⩾22 (males) or ⩾31 (females) mg per g creatinine.29
Statistical analysis
Data are expressed as either mean±s.d. or median (interquartile range) for skewed variables. The ACR was log transformed. One-way analysis of variance was used to analyze differences among the quartiles of AASI and 24-h PP distribution. Comparisons of proportions were performed using the χ2-test. In multivariate analyses, we used linear regression models to study the association of indices of renal function with AASI and 24-h PP. Odds ratios (ORs) and 95% confidence intervals (CIs) were calculated by exponentiation of logistic regression coefficients. Statistical significance was defined as P<0.05. All statistical analyses were performed using SPSS Version 11.5 (SPSS, Chicago, IL, USA).
Results
Clinical characteristics of the inpatients
Of the 948 inpatients, whose mean age was 53.3±13.9 years, 67.1% were men, 30.6% were smokers and 24.0% had diabetes mellitus. The mean AASI was 0.43±0.15 and 24-h PP was 49.1±12.9 mm Hg. All participants were taking oral antihypertensive agents, including diuretics (10.1%), β-blockers (20.7%), vasodilators (calcium channel blockers and α-blockers; 89.8%), and inhibitors of the renin–angiotensin–aldosterone system (angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers, 36.7%). Univariate analysis showed that AASI was positively related to age (r=0.415, P<0.001) and 24-h mean blood pressure (MBP; r=0.158, P<0.001), and negatively related to height (r=−0.151, P<0.001) and pulse rate (r=−0.111, P=0.001).
The main clinical characteristics of the study population across the quartiles of AASI and 24-h PP distribution are shown in Tables 1 and 2. Patients with a higher AASI were older, had higher 24-h SBP and MBP, higher prevalence of diabetes (all P<0.001), and a lower 24-h pulse rate (P<0.001) and 24-h DBP (P=0.018). Moreover, serum creatinine concentration (P=0.029), ACR (P<0.001), the prevalence of eGFR <90 ml min−1 per 1.73 m2 (both P<0.001) and MA (P=0.001) were increased with AASI, whereas the value of eGFR (P<0.001) was decreased with AASI. As the patients we studied were all being treated, we analyzed the use of antihypertensive medications in the quartiles of AASI groups and found a significant difference only in the use of vasodilators (P=0.042, Table 1). The results of the above parameters among the quartiles groups divided by 24-h PP were similar with those grouped by AASI, except for the use of inhibitors of the renin–angiotensin–aldosterone system (Table 2).
Correlation between serum creatinine, eGFR, ACR and risk factors
As shown in Table 3, stepwise multiple regression analysis showed that serum creatinine concentrations were negatively correlated with sex and positively correlated with age, 24-h MBP and the use of diuretics. eGFR calculated by the MDRD formula was related to age (B=−0.60), sex (B=3.59), 24-h MBP (B=−0.34) and diuretics (B=−7.25). However, eGFR measured by the CKD-EPI formula was associated with age (B=−0.83), 24-h MBP (B=−0.25), diuretics (B=−5.70) and the use of inhibitors of the renin–angiotensin–aldosterone system (B=−2.31). Log-transformed ACR was positively correlated with sex, 24-h MBP, total to HDL cholesterol ratio, diabetes, diuretics and the use of inhibitors of the rennin–angiotensin–aldosterone system.
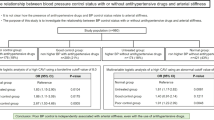
Association of renal indices with AASI and 24-h PP
Multiple linear regression analysis was performed to evaluate the relationship of renal indices such as serum creatinine, eGFR and urinary albumin excretion with AASI and 24-h PP (Table 4). In unadjusted analysis, both AASI and 24-h PP were related to serum creatinine concentration, eGFR and urinary albumin excretion. In the adjusted models shown in Table 4, we found that serum creatinine (B=16.58, P=0.005 vs. B=0.27, P<0.001), urinary albumin excretion (B=0.56, P=0.004 vs. B=0.01, P=0.017) and eGFR-EPI (B=−12.00, P=0.001 vs. B=−0.14, P=0.002) were independently correlated with AASI and 24-h PP after adjusting for several potentially confounding variables. However, when eGFR was assessed by the MDRD formula, the association between eGFR and 24-h PP was weakened (P=0.101). Furthermore, in the fully adjusted model, that is, adjusting for AASI, 24-h PP and other confounding variables, AASI had a borderline statistical significance with eGFR-EPI (P=0.053), whereas 24-h PP remained associated with serum creatinine (P=0.009) and urinary albumin excretion (P=0.006). Additionally, in the subgroup of 24-h SBP <130 mm Hg, the association of AASI with eGFR-EPI, and the relationship between 24-h PP and urinary albumin excretion still persisted (Supplementary Table 1).
Multiple logistic regression analysis showed that each s.d. increase in AASI (that is, 0.15) and 24-h PP (that is, 13 mm Hg) entailed a higher risk of suffering from eGFR-EPI <90 ml min−1 per 1.73 m2 by 80% (OR=1.80; 95% CI: 1.55−2.08) and 79% (OR=1.79; 95% CI: 1.54−2.07) in the unadjusted model (Table 5). When we adjusted for some confounders in the model, both AASI and 24-h PP lost their statistical significance for eGFR-EPI <90 ml min−1 per 1.73 m2 (P=0.073 and P=0.337). However, 24-h PP maintained its prognostic value for MA after additional adjustment for AASI (P=0.038). Each s.d. increase in 24-h PP was associated with a higher risk of suffering from MA by 39% (OR=1.39; 95% CI: 1.02−1.90) after adjusting for several potentially confounding factors.
Discussion
The present study investigated the association of renal function with the novel indices AASI and 24-h PP in a large hypertensive inpatient cohort. Our results indicated that both AASI and 24-h PP were associated with eGFR and urinary albumin excretion. AASI is more strongly correlated with eGFR than 24-h PP, and 24-h PP might be superior to AASI as a marker for MA.
Stiffening of the arteries has an important role in the pathogenesis of cardiovascular events and it is a classic feature in individuals with renal dysfunction. Arterial enlargement and increased stiffness have been observed in the early stages of (CKD),14, 15, 16 suggesting that arterial remodeling occurs early in the course of renal diseases. Moreover, recent studies have suggested an association between impaired renal function and decreased arterial stiffness in essential hypertensive patients.11, 12, 13, 20, 21
In the present study, AASI and 24-h PP were inversely correlated with eGFR-MDRD and eGFR-EPI, independent of other cardiovascular risk factors, such as MBP. However, after adjusting for all the potential confounders, including AASI, 24-h PP and other risk factors, AASI (P=0.053), but not 24-h PP (P=0.081), was independently related to eGFR-EPI. These findings are in agreement with the observations of Mulè et al.22 that increased AASI was associated with GFR in 143 untreated hypertensive patients, which was independent of traditional cardiovascular risk factors, including 24-h MBP and 24-h PP. However, in contrast to the previous studies, we assessed GFR by the CKD-EPI and MDRD formulas, which are noninvasive and easily achieved methods, rather than by a radioisotopic technique. Some studies have shown that the CKD-EPI formula is more accurate than the MDRD equation and it can replace it for routine clinical use.28, 30, 31 Our results showed that the value of eGFR measured by the MDRD formula was lower than that estimated with the CKD-EPI formula. In a study by Ratto et al.21 the risk of a mild reduction in eGFR increased almost twofold for each s.d. increase in AASI. However, in our study, multivariate logistic regression analysis showed that neither AASI nor 24-h PP was related to the presence of mild renal insufficiency (eGFR <90 ml min−1 per 1.73 m2) after adjusting for potential confounders. In addition, we found that AASI was correlated with eGFR-EPI (P=0.051) in the subgroup of 24-h SBP <130 mm Hg, whereas 24-h PP was more closely associated with eGFR-MDRD (P=0.026) and eGFR-EPI (P=0.003) in the subgroup of 24-h SBP ⩾130 mm Hg. These findings suggest that AASI might be an indicator of arterial dysfunction at the early stage and 24-h PP better reflects the advanced stage of vascular lesions.
Our study showed that although AASI and 24-h PP were also associated with urinary albumin excretion, 24-h PP might be a better predictor of MA than AASI. This finding is different from the results of Leoncini et al.20 and Ratto et al.21 The reasons for this discrepancy between studies might be that the objective population we included was from a specific hypertensive ward, it had more cardiovascular complications and all patients were treated with antihypertensive agents. Numerous studies have shown a decrease in arterial stiffness with various pharmacological classes of antihypertensive agents.24, 31, 32, 33 Moreover protecting the kidneys by reducing BP, antihypertensive drugs can also have direct effects on intrarenal mechanisms of damage, such as increased glomerular pressure and proteinuria.26, 34, 35 Additionally, the use of hypertensive agents might affect the degree of nocturnal BP fall, which is considered as an important factor for AASI in hypertensive patients.36 In fact, our study showed that the association of AASI with eGFR and urinary albumin excretion was weakened after adjusting for the same confounders and night-to-day ratio of SBP. However, some studies have reported that 24-h PP outperformed AASI in assessing arterial stiffness37 and in predicting renal damage.18, 19
Arterial stiffness is a common feature of aging and is exacerbated by several disorders such as hypertension, diabetes and renal disease. Mean 24-h PP is an estimate of arterial stiffness at a single point on the pressure stiffness curve, and it is critically dependent on the average distending pressure over the 24 h of measurement. In contrast, AASI is based on the concept that the average distending pressure varies during the day and that the relation between DBP and SBP, with this changing distending pressure, largely depends on the structural and functional characteristics of the large arteries.6 Therefore, AASI and PP reflect different characteristics of the arterial system and may provide different information. It is noteworthy that we demonstrated a different relationship of renal function with AASI and 24-h PP, and confirmed that AASI and 24-h PP could also assess the cardiovascular–renal risk, even in patients with antihypertensive medications.
Some limitations of this study should be noted. First, the cross-sectional design meant that the potential predictive variables and outcome variables were obtained nearly simultaneously, and the information about causality could not be provided. Second, the population of our research was treated inpatients; although we adjusted for some confounders, the complicated effect of antihypertensive agents could not be avoided.
In conclusion, this study provided evidence that the indices of arterial stiffness, AASI and 24-h PP are associated with renal function, such as eGFR and urinary albumin excretion. AASI might more closely correlate with eGFR, and 24-h PP might be superior to AASI in assessing MA in a large group of primary hypertensive inpatients.
References
Blacher J, Asmar R, Djane S, London GM, Safar ME . Aortic pulse wave velocity as a marker of cardiovascular risk in hypertensive patients. Hypertension 1999; 33: 1111–1117.
Laurent S, Boutouyrie P, Asmar R, Gautier I, Laloux B, Guize L, Ducimetiere P, Benetos A . Aortic stiffness is an independent predictor of all-cause and cardiovascular mortality in hypertensive patients. Hypertension 2001; 37: 1236–1241.
Darne B, Girerd X, Safar M, Cambien F, Guize L . Pulsatile versus steady component of blood pressure: a cross-sectional analysis and a prospective analysis on cardiovascular mortality. Hypertension 1989; 13: 392–400.
Franklin SS, Khan SA, Wong ND, Larson MG, Levy D . Is pulse pressure useful in predicting risk for coronary heart disease? The Framingham Heart Study. Circulation 1999; 100: 354–360.
Domanski M, Norman J, Wolz M, Mitchell G, Pfeffer M . Cardiovascular risk assessment using pulse pressure in the first national health and nutrition examination survey (NHANES I). Hypertension 2001; 38: 793–797.
Li Y, Wang JG, Dolan E, Gao PJ, Guo HF, Nawrot T, Stanton AV, Zhu DL, O’Brien E, Staessen JA . Ambulatory arterial stiffness index derived from 24-hour ambulatory blood pressure monitoring. Hypertension 2006; 47: 359–364.
Dolan E, Thijs L, Li Y, Atkins N, McCormack P, McClory S, O’Brien E, Staessen JA, Stanton AV . Ambulatory arterial stiffness index. Hypertension 2006; 47: 365–370.
Kikuya M, Staessen JA, Ohkubo T, Thijs L, Metoki H, Asayama K, Obara T, Inoue R, Li Y, Dolan E, Hoshi H, Hashimoto J, Totsune K, Satoh H, Wang JG, O’Brien E, Imai Y . Ambulatory arterial stiffness index and 24-hour ambulatory pulse pressure as predictors of mortality in Ohasama, Japan. Stroke 2007; 38: 1161–1166.
Culleton BF, Larson MG, Wilson PW, Evans JC, Parfrey PS, Levy D . Cardiovascular disease and mortality in a community-based cohort with mild renal insufficiency. Kidney Int 1999; 56: 2214–2219.
Schillaci G, Pirro M, Mannarino MR, Pucci G, Savarese G, Franklin SS, Mannarino E . Relation between renal function within the normal range and central and peripheral arterial stiffness in hypertension. Hypertension 2006; 48: 616–621.
Gosse P, Safar ME . Arterial stiffness and plasma creatinine in untreated hypertensive patients. Am J Hypertens 2005; 18: 1140–1145.
Mule G, Cottone S, Vadala A, Volpe V, Mezzatesta G, Mongiovi R, Piazza G, Nardi E, Andronico G, Cerasola G . Relationship between albumin excretion rate and aortic stiffness in untreated essential hypertensive patients. J Intern Med 2004; 256: 22–29.
Mourad JJ, Pannier B, Blacher J, Rudnichi A, Benetos A, London GM, Safar ME . Creatinine clearance, pulse wave velocity, carotid compliance and essential hypertension. Kidney Int 2001; 59: 1834–1841.
Briet M, Bozec E, Laurent S, Fassot C, London GM, Jacquot C, Froissart M, Houillier P, Boutouyrie P . Arterial stiffness and enlargement in mild-to-moderate chronic kidney disease. Kidney Int 2006; 69: 350–357.
Wang MC, Tsai WC, Chen JY, Huang JJ . Stepwise increase in arterial stiffness corresponding with the stages of chronic kidney disease. Am J Kidney Dis 2005; 45: 494–501.
Taal MW, Sigrist MK, Fakis A, Fluck RJ, McIntyre CW . Markers of arterial stiffness are risk factors for progression to end-stage renal disease among patients with chronic kidney disease stages 4 and 5. Nephron Clin Pract 2007; 107: c177–c181.
Safar ME, London GM, Plante GE . Arterial stiffness and kidney function. Hypertension 2004; 43: 163–168.
Palmas W, Pickering T, Eimicke JP, Moran A, Teresi J, Schwartz JE, Field L, Weinstock RS, Shea S . Value of ambulatory arterial stiffness index and 24-h pulse pressure to predict progression of albuminuria in elderly people with diabetes mellitus. Am J Hypertens 2007; 20: 493–500.
Laugesen E, Hansen KW, Knudsen ST, Erlandsen M, Ebbehoj E, Mogensen CE, Poulsen PL . Increased ambulatory arterial stiffness index and pulse pressure in microalbuminuric patients with type 1 diabetes. Am J Hypertens 2009; 22: 513–519.
Leoncini G, Ratto E, Viazzi F, Vaccaro V, Parodi A, Falqui V, Conti N, Tomolillo C, Deferrari G, Pontremoli R . Increased ambulatory arterial stiffness index is associated with target organ damage in primary hypertension. Hypertension 2006; 48: 397–403.
Ratto E, Leoncini G, Viazzi F, Vaccaro V, Falqui V, Parodi A, Conti N, Tomolillo C, Deferrari G, Pontremoli R . Ambulatory arterial stiffness index and renal abnormalities in primary hypertension. J Hypertens 2006; 24: 2033–2038.
Mule G, Cottone S, Cusimano P, Incalcaterra F, Giandalia M, Costanzo M, Nardi E, Palermo A, Geraci C, Costa R, Cerasola G . Inverse relationship between ambulatory arterial stiffness index and glomerular filtration rate in arterial hypertension. Am J Hypertens 2008; 21: 35–40.
Van Bortel LM, Struijker-Boudier HA, Safar ME . Pulse pressure, arterial stiffness, and drug treatment of hypertension. Hypertension 2001; 38: 914–921.
Laurent S . Drugs and arterial stiffness in hypertensive patients]. Drugs 2003; 63: 1–8.
Asmar R . Effect of antihypertensive agents on arterial stiffness as evaluated by pulse wave velocity: clinical implications. Am J Cardiovasc Drugs 2001; 1: 387–397.
Wenzel RR . Renal protection in hypertensive patients: selection of antihypertensive therapy. Drugs 2005; 65 (Suppl 2): 29–39.
Levey AS, Greene T, Kusek JW, Beck GJ . A simplified equation to predict glomerular filtration rate from serum creatinine [Abstract]. J Am Soc Nephrol 2000; 11: A0828.
Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro 3rd AF, Feldman HI, Kusek JW, Eggers P, Van Lente F, Greene T, Coresh J . A new equation to estimate glomerular filtration rate. Ann Intern Med 2009; 150: 604–612.
Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G, Grassi G, Heagerty AM, Kjeldsen SE, Laurent S, Narkiewicz K, Ruilope L, Rynkiewicz A, Schmieder RE, Struijker Boudier HA, Zanchetti A, Vahanian A, Camm J, De Caterina R, Dean V, Dickstein K, Filippatos G, Funck-Brentano C, Hellemans I, Kristensen SD, McGregor K, Sechtem U, Silber S, Tendera M, Widimsky P, Zamorano JL, Erdine S, Kiowski W, Agabiti-Rosei E, Ambrosioni E, Lindholm LH, Manolis A, Nilsson PM, Redon J, Struijker-Boudier HA, Viigimaa M, Adamopoulos S, Bertomeu V, Clement D, Farsang C, Gaita D, Lip G, Mallion JM, Manolis AJ, O’Brien E, Ponikowski P, Ruschitzka F, Tamargo J, van Zwieten P, Waeber B, Williams B, The Task Force for the Management of Arterial Hypertension of the European Society of H, the Task Force for the Management of Arterial Hypertension of the EUROPEAN Society of C. 2007 Guidelines for the management of arterial hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J 2007; 28: 1462–1536.
Cirillo M . Evaluation of glomerular filtration rate and of albuminuria/proteinuria. J Nephrol 2010; 23: 125–132.
Ishimitsu T, Numabe A, Masuda T, Akabane T, Okamura A, Minami J, Matsuoka H . Angiotensin-II receptor antagonist combined with calcium channel blocker or diuretic for essential hypertension. Hypertens Res 2009; 32: 962–968.
Payne RA, Wilkinson IB, Webb DJ . Arterial stiffness and hypertension: emerging concepts. Hypertension 2010; 55: 9–14.
Agabiti-Rosei E, Porteri E, Rizzoni D . Arterial stiffness, hypertension, and rational use of nebivolol. Vasc Health Risk Manag 2009; 5: 353–360.
Wright Jr JT, Bakris G, Greene T, Agodoa LY, Appel LJ, Charleston J, Cheek D, Douglas-Baltimore JG, Gassman J, Glassock R, Hebert L, Jamerson K, Lewis J, Phillips RA, Toto RD, Middleton JP, Rostand SG . Effect of blood pressure lowering and antihypertensive drug class on progression of hypertensive kidney disease: results from the AASK trial. JAMA 2002; 288: 2421–2431.
Nakamura T, Inoue T, Suzuki T, Kawagoe Y, Ueda Y, Koide H, Node K . Comparison of renal and vascular protective effects between telmisartan and amlodipine in hypertensive patients with chronic kidney disease with mild renal insufficiency. Hypertens Res 2008; 31: 841–850.
Schillaci G, Parati G, Pirro M, Pucci G, Mannarino MR, Sperandini L, Mannarino E . Ambulatory arterial stiffness index is not a specific marker of reduced arterial compliance. Hypertension 2007; 49: 986–991.
Muxfeldt ES, Fiszman R, Castelpoggi CH, Salles GF . Ambulatory arterial stiffness index or pulse pressure: which correlates better with arterial stiffness in resistant hypertension? Hypertens Res 2008; 31: 607–613.
Acknowledgements
This study was supported by the National Natural Science Foundation of China (81070261 and 30871085), the National Basic Research Program of China (2011CB503905, 2009CB521905), and grants from the Shanghai Health Bureau (2008078) and the Shanghai Science and Technology Committee (09540704600). We gratefully acknowledge the recommendations and modifications from Dr Jan A Staessen (Studies Coordinating Centre, Laboratory of Hypertension, University of Leuven).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on Hypertension Research website
Supplementary information
Rights and permissions
About this article
Cite this article
Wang, Y., Hu, Y., Li, Y. et al. Association of renal function with the ambulatory arterial stiffness index and pulse pressure in hypertensive patients. Hypertens Res 35, 201–206 (2012). https://doi.org/10.1038/hr.2011.167
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2011.167
Keywords
This article is cited by
-
Clinical features of and risk factors for normoalbuminuric diabetic kidney disease in hospitalized patients with type 2 diabetes mellitus: a retrospective cross-sectional study
BMC Endocrine Disorders (2021)
-
Estimated glomerular filtration rate and arterial stiffness in Japanese population: a secondary analysis based on a cross-sectional study
Lipids in Health and Disease (2019)
-
Macro- and microvascular alterations in patients with metabolic syndrome: sugar makes the difference
Hypertension Research (2014)
-
The ambulatory arterial stiffness index and target-organ damage in Chinese patients with chronic kidney disease
BMC Nephrology (2013)