Abstract
The clinical value of the combination of amlodipine and eplerenone is unclear. This study was undertaken to test whether eplerenone potentiates the protective effects of amlodipine against hypertensive cardiovascular injury. Salt-loaded Dahl salt-sensitive hypertensive rats (DS rats) were given (1) vehicle, (2) an antihypertensive dose of amlodipine, (3) a non-antihypertensive dose of eplerenone or (4) combined amlodipine and eplerenone for 6 weeks, and the effects on cardiovascular injuries were compared. There was no significant difference among the four groups regarding plasma aldosterone, urine volume or urinary electrolytes. A subpressor dose of eplerenone markedly ameliorated vascular endothelial dysfunction, cardiac inflammation and fibrosis in DS rats to a similar degree as an antihypertensive dose of amlodipine. Addition of eplerenone to amlodipine, without affecting blood pressure, enhanced the improvement by amlodipine of vascular endothelial function, cardiac inflammation, fibrosis and diastolic dysfunction in DS rats. Additive beneficial effects of eplerenone were attributed to additive potentiation of eNOS and Akt phosphorylation and additive reduction of oxidative stress. Eplerenone significantly attenuated cardiovascular NADPH oxidase activity by reducing gp91phox upregulation and attenuated the upregulation of cardiovascular AT1 receptor, but amlodipine failed to affect them. Thus, the normalization by eplerenone of gp91phox and AT1 receptor upregulation seems to be at least partially responsible for the additive benefits of eplerenone in the prevention of hypertensive cardiovascular injury. The combination of amlodipine and eplerenone may be a promising therapeutic strategy for cardiovascular disease in salt-sensitive hypertension.
Similar content being viewed by others
Introduction
Accumulating experimental1, 2, 3, 4, 5, 6, 7, 8 and clinical evidence9, 10 indicate that mineralocorticoid receptor (MR) activation has a key role in the pathophysiology of cardiovascular injury as well as hypertension. The RALES10 study showed that spironolactone, an MR antagonist, added to an angiotensin-converting enzyme (ACE) inhibitor in patients with severe congestive heart failure, reduces overall mortality. The EPHESUS9 study showed that eplerenone, a selective MR antagonist, added to ACE inhibitor or angiotensin AT1 receptor blocker, decreases cardiovascular events and death in patients with left ventricular (LV) dysfunction following myocardial infarction. In addition to the beneficial effects of MR antagonism on heart failure and myocardial infarction, MR antagonism is as effective for treating hypertension as a calcium channel blocker11 or an AT1 receptor blocker.12 However, the value of MR antagonism in preventing cardiovascular diseases in hypertensive patients remains to be defined.
Calcium channel blockers, such as amlodipine, are effective for hypertension, and blood pressure lowering by calcium channel blockers reduces cardiovascular morbidity and mortality in hypertensive patients.13, 14, 15 However, it remains to be determined whether antihypertensive therapy with calcium channel blockers, in combination with MR antagonists, is useful for the prevention and the treatment of hypertensive cardiovascular injury.
Dahl salt-sensitive hypertensive (DS) rats fed a high-salt diet are characterized by significant cardiac hypertrophy and remodeling, subsequent heart failure and significant vascular endothelial dysfunction. Therefore, salt-loaded Dahl rats are a useful model to examine the protective effects of various drugs against cardiovascular injury. In the present study, we hypothesized that the addition of an MR antagonist to amlodipine may exert additive beneficial effects on cardiovascular injury in salt-sensitive hypertension, independently of blood pressure. To test this hypothesis using salt-loaded DS rats, we compared the effects of a subpressor dose of eplerenone, an antihypertensive dose of amlodipine, and their combination on cardiovascular injury in salt-sensitive hypertensive rats. We obtained the first evidence that MR antagonism with eplerenone potentiates the protective effect of amlodipine-induced blood pressure lowering against cardiovascular injury in salt-sensitive hypertensive rats, independently of blood pressure.
Methods
Animals
All procedures were performed in accordance with institutional guidelines for the care and use of laboratory animals approved by Kumamoto University Graduate School of Medical Sciences. Male DS rats were obtained from Japan SLC (Shizuoka, Japan).
Experimental protocol
DS rats, fed an 8% NaCl diet from 7 weeks of age, were randomized into four groups at 11 weeks of age. They were orally given vehicle, eplerenone (1.25 mg g−1 chow: 100 mg kg−1 per day), or amlodipine (10 mg kg−1 per day in drinking water) alone or in combination with eplerenone (1.25 mg g−1 chow: 100 mg kg−1 per day) for 6 weeks (from 11 to 17 weeks of age). The above-mentioned dose of eplerenone used in this study was a non-antihypertensive dose in DS rats.5 Control DS rats were fed a normal-sodium diet containing 0.3% NaCl throughout the experiments.
Systolic blood pressure was measured by tail-cuff plethysmography (BP-98ASoftron, Tokyo, Japan) every week. Transthoracic echocardiography was performed to estimate cardiac function. At 17 weeks of age, DS rats were anesthetized with ether, arterial blood was immediately collected by cardiac puncture, and plasma was collected by centrifugation and stored at −80 °C until use. After perfusion with phosphate-buffered saline, the carotid artery, thoracic aorta and heart were immediately excised to measure various parameters, as described below.
Arterial ring preparation and tension recording
After removal of the carotid artery from DS rats, the vessel was cut into 5 mm rings, with special care to preserve the endothelium, and mounted in organ baths filled with modified Tyrode's buffer as described.16
Western blot analysis
Our detailed method has been described previously.16 Antibodies used were as follows: anti-phospho eNOS (Ser1177) (1:2000 dilution, BD Transduction Laboratories, Lexington, KY, USA), anti-phospho Akt (1:2000, Cell signaling Technology, Tokyo, Japan), anti-α-tubulin (1:5000, Oncogene, Merck KGaA, Darmstadt, Germany), anti-gp91phox (1:2000, BD Transduction Laboratories), anti-AT1 receptor (1:2000, Santa Cruz Biotechnology, Santa Cruz, CA, USA) and anti-ACE (1:5000, Abcam, Tokyo, Japan). The intensity of the bands was quantified using NIH Image analysis software v1.61 (National Institutes of Health, Bethesda, MD, USA). In individual samples, each value was normalized to α-tubulin.
Measurement of tissue superoxide
The carotid artery and the cardiac tissue removed from DS rats were immediately frozen in Tissue-Tek O.C.T embedding medium (Sakura Finetek, Tokyo, Japan). Dihydroethidium was used to evaluate the levels of cardiac and vascular superoxide in situ as described previously.17
NADPH oxidase activity
The thoracic aorta and the left ventricle were homogenized with a POLYTRON homogenizer PT1200E (KINEMATICA AG, Bohemia, NY, USA) and centrifuged, and NADPH oxidase activity in each resulting supernatant was measured by lucigenin chemiluminescence in the presence of 10 μM NADPH and 10 μM lucigenin as electron acceptor, as described previously.18 Protein concentrations were measured by the Bradford method.
Echocardiography
In vivo cardiac morphology was assessed by transthoracic echocardiography (12-MHz echocardiographic probe, PHILIPS SONOS-4500, CardioVascular Sales, Aliso Viejo, CA, USA), as previously described.17 Rats were anesthetized with a mixture of ketamine HCl (50 mg kg−1 i.p.) and xylazine HCl (5 mg kg−1 i.p.). M-mode LV end-systolic and end-diastolic diameters were averaged from 3–5 beats. LV percent FS and LV mass were calculated as described previously. LV mass=1.04 × ((LVDd+PWd+LVPw)3−LVDd3). Studies and analysis were performed by investigators in a blinded fashion.
Plasma NO2/NO3
Plasma NO2/NO3 was measured with an NO2/NO3 Assay Kit-FX (Dojindo, Kumamoto, Japan).
Histological analysis and immunohistochemistry
The hearts were fixed with 4% formalin overnight, embedded in paraffin, cut into 4 μm thick coronal sections, and stained with Sirius Red F3BA (0.5% in saturated aqueous picric acid, Aldrich Chemical Company, Milwaukee, WI, USA) to assess cardiac interstitial fibrosis. The positive area of fibrosis per field area was assessed by examining at least 10 fields per rat using Lumina Vision version 2.2 analysis software (Mitani Corporation, Tokyo, Japan).
To assess cardiac interstitial macrophage infiltration, the frozen heart sections were immunostained with anti-ED-1 antibody (BMA Biomedicals, Augst, Switzerland) (working dilution 1:500) to identify monocytes/macrophages, as described previously.16 The number of cardiac ED-1–positive cells per field area (mm2) was counted in a blinded manner by examining more than 10 fields per section using a microscope with × 200 magnification; the average ED-1-positive cell number was obtained in each rat.
Reverse transcriptase PCR
Total RNA was prepared using TRIzol reagent (Invitrogen, Carlsbad, CA, USA) from LV tissue. Complementary DNAs were synthesizes by standard techniques using a QuantiTect Reverse Transcription Kit (QIAGEN, Hilden, Germany). Real-time PCR was performed, recorded, and analyzed using a Thermal Cycler Dice Real Time System (TaKaRa Bio, Shiga, Japan) with SYBR Green I detection as described previously.19 The cDNA was amplified using a SYBR Premix Ex Taq (Perfect Real Time) PCR kit (TaKaRa Bio) with specific primers (MCP-1, forward: 5′-CCTCCACCACTATGCAGGTCTC-3′; reverse: 5′-GCACGTGGATGCTACAGGC-3′; transforming growth factor-β1 (TGF-β1), forward: 5′-TGCGCCTGCAGATTCAAG-3′; reverse: 5′-AGGTAACGCCAGGAATTGTTGCTA-3′; gylceraldehyde-3-phosphate dehydrogenase (GAPDH), forward: 5′-GGCACAGTCAAGGCTGAGAATG-3′; reverse: 5′-ATGGTGGTGAAGACGCCAGTA-3′). To confirm the specificity of the PCR, products from each primer pair were subjected to a melting curve analysis.
Statistical analysis
The results are expressed as mean±s.e.m. Statistical significance was determined by one-way analysis of variance, followed by Fisher's PLSD test, using StatView for Windows (SAS Institute Inc., Cary, NC, USA). In all tests, differences were considered statistically significant at the value of P less than 0.05.
Results
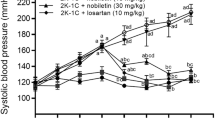
Effects of eplerenone, amlodipine, and their combination on blood pressure
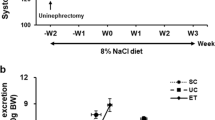
As shown in Figure 1a, amlodipine monotherapy at the dose used in this study moderately but significantly reduced blood pressure in DS rats throughout the treatment, but blood pressure in the amlodipine-treated group was higher than in control DS rats fed a low-salt diet. However, eplerenone monotherapy at the dose used in this study did not significantly lower blood pressure in DS rats. The combination of eplerenone and amlodipine significantly lowered blood pressure throughout the treatment, to a comparable degree to amlodipine monotherapy.
Effect of eplerenone, amlodipine and their combination on blood pressure (a), acetylcholine-induced endothelium-dependent vascular relaxation (b), vascular eNOS phosphorylation (c) and Akt phosphorylation (d). Upper panels in (c) and (d) indicate representative western blots of phospho-eNOS and phosphor-Akt, respectively. Am, amlodipine-treated DS rats fed a high-salt diet; Com, combined eplerenone and amlodipine-treated DS rats fed a high-salt diet; Ep, eplerenone-treated DS rats fed a high-salt diet; L, Dahl salt-sensitive (DS) rats fed a low-salt diet throughout the experiment; Ve, vehicle-treated DS rats fed a high-salt diet. Values are means±s.e.m. (n=4 in L, n=7–8 in Ve, Ep, Am and Com). *P<0.05, **P<0.01.
Effects of eplerenone, amlodipine, and their combination on urinary and plasma variables
High-salt-fed DS rats showed greater water intake, greater urinary volume, lower urinary osmolality and larger urinary sodium excretion than DS rats fed a low-salt diet (Supplementary Table 1). Monotherapy with eplerenone or amlodipine or their combination did not affect urine volume, urinary osmolality or sodium excretion in DS rats.
As shown in Supplementary Table 2, plasma renin activity and aldosterone concentrations in high-salt-loaded DS rats were significantly lower than DS rats fed a low-salt diet. There was no significant difference between these two groups regarding plasma sodium, potassium, or chloride concentrations or plasma osmolality. Plasma renin activity was significantly reduced by amlodipine monotherapy but not by eplerenone monotherapy. Plasma aldosterone was not affected by either monotherapy or their combination.
Effects of eplerenone, amlodipine, and their combination on body weight and organ weight
As shown in Supplementary Table 3, high-salt-loaded DS rats exhibited larger LV weight than low-salt–fed DS rats. Amlodipine monotherapy, but not eplerenone monotherapy, significantly reduced LV weight in DS rats. Add-on eplerenone tended to enhance the reduction of LV weight by amlodipine in DS rats, but the difference did not reach statistical significance.
Effects of eplerenone, amlodipine, and their combination on vascular endothelial function, eNOS, Akt and plasma NOx in DS rats
Vascular endothelial function in salt-loaded DS rats was significantly impaired compared with DS rats fed a low-salt diet (Figure 1b).The eNOS phosphorylation (Figure 1c), Akt phosphorylation (Figure 1d), and plasma NOx (Figure 2a) in salt-loaded DS rats were significantly lower than in low-salt-fed DS rats. Monotherapy with eplerenone or amlodipine comparably improved vascular endothelial function, attenuated the decreases in the phosphorylation of eNOS and Akt, and attenuated the decrease in plasma NOx. However, the combination of eplerenone and amlodipine improved all of these parameters more than either monotherapy.
Effect of eplerenone, amlodipine and their combination on plasma NOx (a), aortic superoxide (b), NADPH oxidase activity (c) and gp91phox protein levels (d) of Dahl salt-sensitive rats. Upper panels in (b) and (d) indicate representative photomicrographs of dihydroethidium-stained aortic sections and western blots, respectively. Abbreviations used are the same as in Figure 1. Values are means±s.e.m. (n=4 in L, n=7–8 in Ve, Ep, Am and Com). Bar=100 μm. * P<0.05, ** P<0.01.
Effects of eplerenone, amlodipine, and their combination on vascular superoxide, NADPH oxidase activity, and gp91phox in DS rats
As shown in Figure 2, salt-loaded DS rats had greater vascular superoxide level, NADPH oxidase activity, and gp91phox protein level than DS rats fed a low-salt diet. Eplerenone or amlodipine alone reduced vascular superoxide to a similar extent (Figure 2b). Combined eplerenone and amlodipine reduced vascular superoxide to a greater extent than either monotherapy. Eplerenone monotherapy and the combination of amlodipine with eplerenone significantly and similarly reduced vascular NADPH oxidase activity (Figure 2c) and gp91phox protein (Figure 2d). In contrast, amlodipine alone did not significantly reduce NADPH oxidase activity or gp91phox in DS rats.
Effects of eplerenone, amlodipine, and their combination on vascular AT1 receptor and ACE expression in DS rats
Vascular AT1 receptor level in salt-loaded DS rats was greater than in DS rats fed a low-salt diet (Figure 3a). Eplerenone monotherapy and the combination of amlodipine with eplerenone significantly and comparably attenuated the increase in vascular AT1 receptor protein expression in DS rats. By contrast, amlodipine alone failed to reduce it. Vascular ACE protein level was similar among all groups of DS rats (Figure 3b).
Effect of eplerenone, amlodipine and their combination on aortic AT1 receptor (a) and ACE protein levels (b) of Dahl salt-sensitive rats. Upper panels in (a) and (b) indicate representative western blots. Abbreviations used are the same as in Figure 1. Values are means±s.e.m. (n=4 in L, n=7–8 in Ve, Ep, Am and Com). *P<0.05, **P<0.01.
Effects of eplerenone, amlodipine and their combination on cardiac diastolic function, lung weight and lung water content in DS rats
Figure 4a shows that salt-loaded DS rats displayed impaired cardiac diastolic function compared with DS rats fed a low-salt diet, as shown by the higher E/A ratio in salt-loaded DS rats than control DS rats. Monotherapy with eplerenone or amlodipine tended to reduce the E/A ratio in DS rats, but the difference did not reach statistical significance. However, the combination of amlodipine with eplerenone significantly reduced the E/A ratio in DS rats (P<0.01). As shown in Figure 4b and c, wet lung weight and lung water content, which was the difference between the weights of wet lung and dry lung, in salt-loaded DS rats were greater than those in DS rats fed a low-salt diet, and they tended to be reduced by monotherapy with eplerenone or amlodipine, but the difference did not reach statistical significance. However, the combination of amlodipine and eplerenone significantly attenuated the increases in wet lung weight (P<0.05) and lung water content (P<0.05) in DS rats.
Effect of eplerenone, amlodipine and their combination on E/A ratio (a), wet lung weight (b) and lung water content (c) of Dahl salt-sensitive rats. Upper panels in (a) indicate representative M-mode and pulsed Doppler tracings by echocardiography. Abbreviations used are the same as in Figure 1. Values are means±s.e.m. (n=4 in L, n=7–8 in Ve, Ep, Am, and Com). *P<0.05, **P<0.01.
As shown in Supplementary Table 4, the increases in LV mass index, IVSd, IVPw, IVDd and LVDs in salt-loaded DS rats were significantly attenuated by amlodipine, but not by eplerenone. Add-on eplerenone tended to potentiate the attenuation of these parameters by amlodipine, although this was not statistically significant. There was no significant difference in FS among groups.
Effects of eplerenone, amlodipine and their combination on cardiac macrophage infiltration, MCP-1 mRNA expression, cardiac interstitial fibrosis and TGF-β1 mRNA expression in DS rats
As shown in Figure 5, cardiac macrophage infiltration, MCP-1 expression, cardiac interstitial fibrosis and cardiac TGF-β1 expression in salt-loaded DS rats were greater than those in DS rats fed a low-salt diet. Monotherapy with amlodipine or eplerenone significantly reduced all these parameters. However, the combination of these drugs reduced all these parameters more than either monotherapy.
Effect of eplerenone, amlodipine and their combination on cardiac ED1-positive cells (a), MCP-1 mRNA (b), cardiac fibrosis (c) and transforming growth factor-β1 (TGF-β1) mRNA (d) of Dahl salt-sensitive rats. Upper panels in (a) and (c) indicate representative photomicrographs of cardiac sections stained with ED1 and Sirius red, respectively. Abbreviations used are the same as in Figure 1. Values are means±s.e.m. (n=4 in L, n=7–8 in Ve, Ep, Am and Com). Bar=100 μm. *P<0.05, **P<0.01.
Effects of eplerenone, amlodipine and their combination on cardiac superoxide, NADPH oxidase, and gp91phox in DS rats
As shown in Figure 6, cardiac superoxide level, NADPH oxidase activity, and gp91phox protein level in salt-loaded DS rats were greater than those in low-salt-fed DS rats. Eplerenone or amlodipine alone significantly attenuated the increase in cardiac superoxide in DS rats, and their combination reduced it more than either monotherapy (Figure 6a). Eplerenone alone or the combination of amlodipine with eplerenone significantly and comparably decreased cardiac NADPH oxidase activity and gp91phox whereas amlodipine alone did not significantly decrease them (Figures 6b and c).
Effect of eplerenone, amlodipine and their combination on cardiac superoxide (a), NADPH oxidase activity (b) and gp91phox protein levels (c) of Dahl salt-sensitive rats. Upper panels in (a) and (c) indicate representative photomicrographs of dihydroethidium-stained cardiac sections and western blots, respectively. Abbreviations used are the same as in Figure 1. Values are means±s.e.m. (n=4 in L, n=7–8 in Ve, Ep, Am and Com). Bar=100 μm. **P<0.01.
Effects of eplerenone, amlodipine and their combination on cardiac AT1 receptor and ACE protein expression in DS rats
As shown in Figure 7a, cardiac AT1 receptor protein level in salt-loaded DS rats was greater than in DS rats fed a low-salt diet (P<0.01). Eplerenone alone or the combination of amlodipine with eplerenone (P<0.05) significantly and similarly reduced cardiac AT1 receptor upregulation in DS rats, whereas amlodipine alone failed to reduce it. There was no significant difference among all groups in cardiac ACE protein level (Figure 7b).
Effect of eplerenone, amlodipine and their combination on cardiac AT1 receptor (a) and angiotensin-converting enzyme (ACE) protein levels (b) of Dahl salt-sensitive rats. Upper panels in (a) and (b) indicate representative western blots. Abbreviations used are the same as in Figure 1. Values are means±s.e.m. (n=4 in L, n=7–8 in Ve, Ep, Am and Com). *P<0.05, **P<0.01.
Discussion
The major findings of this study are that a subpressor dose of eplerenone prevented cardiovascular injury in DS rats, through different mechanisms from an antihypertensive dose of amlodipine, and that addition of eplerenone to amlodipine potentiated the improvement by amlodipine of vascular endothelial function, cardiac inflammation, fibrosis and diastolic function independently of blood pressure in DS rats (Figure 8). Thus, our present work highlights the combination of eplerenone and amlodipine as a promising therapeutic strategy for cardiovascular injury in salt-sensitive hypertension.
In the present study, the dose of eplerenone used was non-antihypertensive, to examine the direct role of MR in cardiovascular injury in the presence of salt-sensitive hypertension. Notably, a non-antihypertensive dose of eplerenone increased the phosphorylation of Akt and eNOS and prevented the impairment of vascular endothelial function to similar extents as an antihypertensive dose of amlodipine. These results show that MR is directly involved in the impairment of vascular endothelial function in DS rats. Of note are the observations that the addition of eplerenone to amlodipine increased the improvement of vascular endothelial function in DS rats, which was associated with additive enhancement of eNOS and Akt phosphorylation and plasma NOx. These results provide the first evidence that the addition of eplerenone to antihypertensive doses of amlodipine augments the beneficial effects on vascular endothelial function.
It is well established that salt-loaded DS rats develop cardiac remodeling followed by diastolic heart failure.20, 21 Interestingly, the combination of amlodipine with eplerenone exerted additive beneficial effects on diastolic dysfunction in DS rats. Furthermore, the addition of eplerenone to amlodipine strengthened the prevention of lung edema, as shown by a greater attenuation of wet lung weight and lung water content by the combination compared with either monotherapy. These results support the notion that the combination of amlodipine with eplerenone may be useful for treating hypertensive diastolic heart failure. Furthermore, eplerenone added to amlodipine suppressed cardiac macrophage infiltration, the upregulation of MCP-1, a proinflammatory chemokine, cardiac fibrosis and the upregulation of TGF-β1 expression, a profibrotic growth factor, more than monotherapy in DS rats. These results show that add-on eplerenone potentiated the prevention by amlodipine of cardiac inflammation and fibrosis in DS rats through greater inhibition of the upregulation of MCP-1 and TGF-β1, respectively. Thus, the additive beneficial effects of add-on eplerenone on cardiac diastolic dysfunction in DS rats seem to be mediated by additive preventive effects on cardiac inflammation and fibrosis.
We have previously reported that either oxidative stress or angiotensin II has a causative role in the development of cardiovascular injury in DS rats.17, 18, 21 Previous work investigating the effects of aldosterone infusion or MR antagonists indicate that MR activation is involved in the increase in cardiovascular NADPH oxidase subunits19, 22, 23 and renin-angiotensin system components24, 25, 26, 27, 28 Therefore, in this study, we also compared the effects of eplerenone, amlodipine and their combination on these parameters in DS rats. Notably, eplerenone alone or in combination with amlodipine significantly attenuated the increase in vascular and cardiac NADPH oxidase activity and its subunit gp91phox in DS rats. However, in spite of a significant reduction of blood pressure, amlodipine alone did not affect NADPH oxidase activity or gp91phox in DS rats. These results show that eplerenone attenuates vascular and cardiac superoxide via a different mechanism from that of amlodipine, which appears to partially explain the reason for the additive attenuation of vascular and cardiac superoxide by the combination of these drugs. Another important finding of this study is that eplerenone alone or combined with amlodipine significantly prevented the upregulation of vascular and cardiac AT1 receptor in DS rats. Taken together with the fact that cardiovascular AT1 receptor has a key role in the development of vascular endothelial dysfunction and cardiac remodeling and dysfunction in DS rats17, 18, 21 our results show that the suppression of cardiovascular AT1 receptor upregulation by eplerenone is involved in the additive beneficial effects of eplerenone on cardiovascular injury in DS rats.
Study limitation
The present study did not allow us to elucidate the precise mechanism underlying the protective effects of eplerenone added to amlodipine against cardiovascular injury in salt-loaded DS rats with low plasma aldosterone. High salt in Dahl rats significantly activates Rac1, and Rac1 in turn activates MR independently of aldosterone.29, 30 Furthermore, Rac1-mediated MR activation is involved in tissue injury.29, 30 Therefore, aldosterone is not always necessary for MR activation. Furthermore, very recently, MR antagonists were found to have protective inverse agonist activity at low concentrations.31 Therefore, the above-mentioned mechanisms might have been involved in the protective effects of eplerenone against cardiovascular injury in the present study.
Although salt-loaded DS rats are characterized by low plasma aldosterone, a marked rise in urinary sodium excretion due to a high-salt diet is accompanied by marked excretory loss of Ca2+ and consequent plasma-ionized hypocalcemia, leading to secondary hyperparathyroidism. Parathyroid hormone may induce intracellular Ca2+ overloading and, subsequently, oxidative stress.32, 33 Moreover, recent experimental work on myocardially infarcted rats shows that under conditions of cardiac tissue damage, physiologic glucocorticoids can activate MR, and subsequently aldosterone becomes a minor player under such conditions. Further research is needed to elucidate the precise mechanism underlying the protective effects of eplerenone in salt-loaded Dahl rats with low plasma aldosterone.
In conclusion, in our present work, we examined for the first time whether the addition of eplerenone to amlodipine can augment the prevention of cardiovascular injury in DS rats. Our work provides the first evidence that eplerenone, combined with an antihypertensive dose of amlodipine, exerts greater beneficial effects on cardiovascular injury in salt-sensitive hypertensive rats than either monotherapy. These beneficial effects of add-on eplerenone appear to be partially mediated by the inhibition of gp91phox-related NADPH oxidase and AT1 receptor upregulation in cardiovascular tissues.
References
Brilla CG, Pick R, Tan LB, Janicki JS, Weber KT . Remodeling of the rat right and left ventricles in experimental hypertension. Circ Res 1990; 67: 1355–1364.
Brown NJ . Aldosterone and vascular inflammation. Hypertension 2008; 51: 161–167.
Funder J . Mineralocorticoids and cardiac fibrosis: the decade in review. Clin Exp Pharmacol Physiol 2001; 28: 1002–1006.
Kobayashi N, Yoshida K, Nakano S, Ohno T, Honda T, Tsubokou Y, Matsuoka H . Cardioprotective mechanisms of eplerenone on cardiac performance and remodeling in failing rat hearts. Hypertension 2006; 47: 671–679.
Nagata K, Obata K, Xu J, Ichihara S, Noda A, Kimata H, Kato T, Izawa H, Murohara T, Yokota M . Mineralocorticoid receptor antagonism attenuates cardiac hypertrophy and failure in low-aldosterone hypertensive rats. Hypertension 2006; 47: 656–664.
Rocha R, Rudolph AE, Frierdich GE, Nachowiak DA, Kekec BK, Blomme EA, McMahon EG, Delyani JA . Aldosterone induces a vascular inflammatory phenotype in the rat heart. Am J Physiol Heart Circ Physiol 2002; 283: H1802–H1810.
Schiffrin EL . Effects of aldosterone on the vasculature. Hypertension 2006; 47: 312–318.
Sun Y, Zhang J, Lu L, Chen SS, Quinn MT, Weber KT . Aldosterone-induced inflammation in the rat heart : role of oxidative stress. Am J Pathol 2002; 161: 1773–1781.
Pitt B, Remme W, Zannad F, Neaton J, Martinez F, Roniker B, Bittman R, Hurley S, Kleiman J, Gatlin M . Eplerenone, a selective aldosterone blocker, in patients with left ventricular dysfunction after myocardial infarction. N Engl J Med 2003; 348: 1309–1321.
Pitt B, Zannad F, Remme WJ, Cody R, Castaigne A, Perez A, Palensky J, Wittes J . The effect of spironolactone on morbidity and mortality in patients with severe heart failure. Randomized aldactone evaluation study investigators. N Engl J Med 1999; 341: 709–717.
White WB, Duprez D, St Hillaire R, Krause S, Roniker B, Kuse-Hamilton J, Weber MA . Effects of the selective aldosterone blocker eplerenone versus the calcium antagonist amlodipine in systolic hypertension. Hypertension 2003; 41: 1021–1026.
Flack JM, Oparil S, Pratt JH, Roniker B, Garthwaite S, Kleiman JH, Yang Y, Krause SL, Workman D, Saunders E . Efficacy and tolerability of eplerenone and losartan in hypertensive black and white patients. J Am Coll Cardiol 2003; 41: 1148–1155.
Julius S, Kjeldsen SE, Weber M, Brunner HR, Ekman S, Hansson L, Hua T, Laragh J, McInnes GT, Mitchell L, Plat F, Schork A, Smith B, Zanchetti A . Outcomes in hypertensive patients at high cardiovascular risk treated with regimens based on valsartan or amlodipine: the value randomised trial. Lancet 2004; 363: 2022–2031.
Liu L, Wang JG, Gong L, Liu G, Staessen JA . Comparison of active treatment and placebo in older chinese patients with isolated systolic hypertension. Systolic hypertension in china (syst-china) collaborative group. J Hypertens 1998; 16: 1823–1829.
Staessen JA, Fagard R, Thijs L, Celis H, Arabidze GG, Birkenhager WH, Bulpitt CJ, de Leeuw PW, Dollery CT, Fletcher AE, Forette F, Leonetti G, Nachev C, O′Brien ET, Rosenfeld J, Rodicio JL, Tuomilehto J, Zanchetti A . Randomised double-blind comparison of placebo and active treatment for older patients with isolated systolic hypertension. The systolic hypertension in europe (syst-eur) trial investigators. Lancet 1997; 350: 757–764.
Nakamura T, Yamamoto E, Kataoka K, Yamashita T, Tokutomi Y, Dong YF, Matsuba S, Ogawa H, Kim-Mitsuyama S . Beneficial effects of pioglitazone on hypertensive cardiovascular injury are enhanced by combination with candesartan. Hypertension 2008; 51: 296–301.
Yamamoto E, Kataoka K, Shintaku H, Yamashita T, Tokutomi Y, Dong YF, Matsuba S, Ichijo H, Ogawa H, Kim-Mitsuyama S . Novel mechanism and role of angiotensin ii induced vascular endothelial injury in hypertensive diastolic heart failure. Arterioscler Thromb Vasc Biol 2007; 27: 2569–2575.
Yamamoto E, Kataoka K, Yamashita T, Tokutomi Y, Dong YF, Matsuba S, Ogawa H, Kim-Mitsuyama S . Role of xanthine oxidoreductase in the reversal of diastolic heart failure by candesartan in the salt-sensitive hypertensive rat. Hypertension 2007; 50: 657–662.
Nakamura T, Kataoka K, Fukuda M, Nako H, Tokutomi Y, Dong YF, Ichijo H, Ogawa H, Kim-Mitsuyama S . Critical role of apoptosis signal-regulating kinase 1 in aldosterone/salt-induced cardiac inflammation and fibrosis. Hypertension 2009; 54: 544–551.
Doi R, Masuyama T, Yamamoto K, Doi Y, Mano T, Sakata Y, Ono K, Kuzuya T, Hirota S, Koyama T, Miwa T, Hori M . Development of different phenotypes of hypertensive heart failure: systolic versus diastolic failure in dahl salt-sensitive rats. J Hypertens 2000; 18: 111–120.
Kim S, Yoshiyama M, Izumi Y, Kawano H, Kimoto M, Zhan Y, Iwao H . Effects of combination of ace inhibitor and angiotensin receptor blocker on cardiac remodeling, cardiac function, and survival in rat heart failure. Circulation 2001; 103: 148–154.
Johar S, Cave AC, Narayanapanicker A, Grieve DJ, Shah AM . Aldosterone mediates angiotensin ii-induced interstitial cardiac fibrosis via a nox2-containing nadph oxidase. Faseb J 2006; 20: 1546–1548.
Keidar S, Kaplan M, Pavlotzky E, Coleman R, Hayek T, Hamoud S, Aviram M . Aldosterone administration to mice stimulates macrophage nadph oxidase and increases atherosclerosis development: a possible role for angiotensin-converting enzyme and the receptors for angiotensin ii and aldosterone. Circulation 2004; 109: 2213–2220.
Di Zhang A, Cat AN, Soukaseum C, Escoubet B, Cherfa A, Messaoudi S, Delcayre C, Samuel JL, Jaisser F . Cross-talk between mineralocorticoid and angiotensin ii signaling for cardiac remodeling. Hypertension 2008; 52: 1060–1067.
Lemarie CA, Paradis P, Schiffrin EL . New insights on signaling cascades induced by cross-talk between angiotensin ii and aldosterone. J Mol Med 2008; 86: 673–678.
Robert V, Heymes C, Silvestre JS, Sabri A, Swynghedauw B, Delcayre C . Angiotensin at1 receptor subtype as a cardiac target of aldosterone: role in aldosterone-salt-induced fibrosis. Hypertension 1999; 33: 981–986.
Schiffrin EL, Franks DJ, Gutkowska J . Effect of aldosterone on vascular angiotensin ii receptors in the rat. Can J Physiol Pharmacol 1985; 63: 1522–1527.
Ullian ME, Schelling JR, Linas SL . Aldosterone enhances angiotensin ii receptor binding and inositol phosphate responses. Hypertension 1992; 20: 67–73.
Fujita T . Mineralocorticoid receptors, salt-sensitive hypertension, and metabolic syndrome. Hypertension 2010; 55: 813–818.
Shibata S, Nagase M, Yoshida S, Kawarazaki W, Kurihara H, Tanaka H, Miyoshi J, Takai Y, Fujita T . Modification of mineralocorticoid receptor function by rac1 gtpase: implication in proteinuric kidney disease. Nat Med 2008; 14: 1370–1376.
Mihailidou AS, Loan Le TY, Mardini M, Funder JW . Glucocorticoids activate cardiac mineralocorticoid receptors during experimental myocardial infarction. Hypertension 2009; 54: 1306–1312.
Vidal A, Sun Y, Bhattacharya SK, Ahokas RA, Gerling IC, Weber KT . Calcium paradox of aldosteronism and the role of the parathyroid glands. Am J Physiol Heart Circ Physiol 2006; 290: H286–H294.
Zia AA, Kamalov G, Newman KP, McGee JE, Bhattacharya SK, Ahokas RA, Sun Y, Gerling IC, Weber KT . From aldosteronism to oxidative stress: the role of excessive intracellular calcium accumulation. Hypertens Res 2010; 33: 1091–1101.
Acknowledgements
This work was supported in part by Grants-in-Aid for Scientific Research from the Ministry of Education, Culture, Sports, Science, and Technology-Japan.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on Hypertension Research website
Rights and permissions
About this article
Cite this article
Nakamura, T., Fukuda, M., Kataoka, K. et al. Eplerenone potentiates protective effects of amlodipine against cardiovascular injury in salt-sensitive hypertensive rats. Hypertens Res 34, 817–824 (2011). https://doi.org/10.1038/hr.2011.35
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2011.35
Keywords
This article is cited by
-
Comparison of eplerenone and spironolactone for the treatment of primary aldosteronism
Hypertension Research (2016)
-
DPP-4 inhibitor linagliptin ameliorates cardiovascular injury in salt-sensitive hypertensive rats independently of blood glucose and blood pressure
Cardiovascular Diabetology (2014)
-
Mineralocorticoid Receptors in Vascular Disease: Connecting Molecular Pathways to Clinical Implications
Current Atherosclerosis Reports (2013)
-
Activation of mineralocorticoid receptors in the rostral ventrolateral medulla is involved in hypertensive mechanisms in stroke-prone spontaneously hypertensive rats
Hypertension Research (2012)
-
Eplerenone, amlodipine and experimental hypertension: one plus one equals three
Hypertension Research (2011)