Abstract
This study investigated the relationship between seasonal variations in blood pressure (BP) and the corresponding changes in meteorological parameters and weather-induced patients’ discomfort. Hypertensives on stable treatment were assessed in winter-1, summer and winter-2 with clinic (CBP), home (HBP) and 24-hour ambulatory BP (ABP). Discomfort indices derived from temperature, humidity and atmospheric pressure that reflected subjects’ discomfort were evaluated. Symptomatic orthostatic hypotension was assessed with a questionnaire. Sixty subjects (mean age 65.1±8.8 [s.d.], 39 men) were analyzed. CBP, HBP and daytime ABP were lower in summer than in winter (P<0.01). Nighttime ABP was unchanged, which resulted in a 55% higher proportion of non-dippers (P<0.001). All the discomfort indices that reflected weather-induced subjects’ discomfort were higher in summer (P<0.05) and systolic daytime ABP was <110 mm Hg in 15 subjects (25%). Seasonal changes in temperature and the discomfort indices were correlated with BP changes (P<0.05). Multivariate analyses revealed that winter BP levels, seasonal differences in temperature, female gender and the use of diuretics predicted the summer BP decline. In conclusion, all aspects of the BP profile, except nighttime ABP, are reduced in summer, resulting in an increased prevalence of non-dippers in summer with unknown consequences. Seasonal BP changes are influenced by changes in meteorological parameters, anthropometric and treatment characteristics. Trials are urgently needed to evaluate the clinical relevance of excessive BP decline in summer and management guidelines for practicing physicians should be developed.
Similar content being viewed by others
Introduction
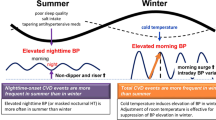
The seasonal variation of blood pressure (BP) is a complex phenomenon that has attracted interest in clinical research and practice.1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16 Several studies, primarily retrospective or cross-sectional, reported lower BP values during summer compared with winter, in both normotensive and hypertensive patients in all age groups.1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16 The elderly have been shown to exert larger seasonal BP variation,7, 11, 15 whereas other factors such as gender, body mass index (BMI) and smoking status may interfere.11, 12, 14 Cardiovascular morbidity and mortality is higher in winter than in summer, especially in the elderly, and higher BP values in winter may contribute to this seasonal pattern.17, 18, 19, 20
In clinical practice, the summer decline in BP, particularly when accompanied by symptoms suggesting orthostasis but also in the absence of symptoms when systolic BP becomes too low, may lead some physicians to down-titrate antihypertensive drug treatment. Moreover, the widespread use of BP self-monitoring at home allows patients to promptly identify the summer decline in BP, which often becomes a reason of concern or causes treatment down-titration by the patients themselves.
Current hypertension guidelines provide detailed recommendations for the identification of uncontrolled hypertension and the optimal strategy for up-titrating treatment to reach optimal BP control.21 However, although down-titration of treatment appears to be a sensible and unavoidable action whenever there is a persistent and excessive decline in BP attributed to any factor (summer decline or other), there are no recommendations to doctors on the optimal management of such cases. Unfortunately current guidelines do not mention seasonal BP changes, although these changes are common and often considerable, demanding action by the practicing physician. This absence probably reflects a lack of interventional studies that provide evidence on when and how intervention in these cases is necessary and beneficial, although the phenomenon has been clearly described in several studies.1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16
This study investigated seasonal BP changes assessed by clinic (CBP), home (HBP) and ambulatory (ABP) measurements and the relationship of these changes to changes in several meteorological parameters and weather-induced patients’ discomfort, in terms of magnitude, predictors and clinical implications.
Subjects and methods
Subjects
This was a prospective study in adults who attended an outpatient hypertension clinic. The following inclusion criteria were used: fully ambulatory subjects, age >40 years, treated for hypertension with stable antihypertensive drug treatment (⩾8 weeks) and well-controlled hypertension (systolic HBP <130 mm Hg; average ⩾12 measurements; validated oscillometric arm device with automated memory). The following exclusion criteria were used: symptomatic heart disease, cardiovascular or cerebrovascular event in the previous 3 months, neurological disorders, serum creatinine >2 mg dl−1 and the use of loop diuretics. The study protocol was approved by the hospital scientific committee and signed informed consent was obtained from all participants.
BP measurements
Participants were evaluated during three consecutive seasonal periods: winter-1 (December 2009–March 2010); summer (June 2010–September 2010) and winter-2 (December 2010–March 2011). CBP, HBP and ABP measurements were assessed during each evaluation in all participants within 2 weeks.
The primary analysis included all participants who had complete data for winter-1 and summer, and whose seasonal assessments were performed under the same antihypertensive drug treatment. Any treatment changes during the summer were performed after the summer BP evaluation, and treatment was restored at least 4 weeks before the winter-2 evaluation.
CBP was evaluated with triplicate measurements in a single study visit (after at least one pre-study visit) after 5 min of sitting rest with at least 1 min between measurements, using a standard mercury sphygmomanometer or a validated professional oscillometric BP monitor (Microlife WatchBP Office)22 (inflatable bladder size according to the individual’s arm circumference) by physicians who fulfilled the British Hypertension Society Protocol criteria for observers’ agreement in BP measurement.23
HBP was monitored on 6 routine workdays within 2 weeks using validated oscillometric arm devices (Microlife WatchBP Home with appropriate cuff size to fit the individual’s arm circumference).24
Participants were trained in the conditions of HBP measurement and device use, and they were instructed to perform duplicate morning (0600–0900 h, before drug intake) and evening (1800–2100 h) measurements after a 5-min sitting rest with 1 min between readings. A form was supplied to the participants to report their HBP values. These data were verified against measurements downloaded from the device memory through a PC link. The average value of all HBP measurements was used in the analyses.
ABP was monitored on a routine workday, before or after the HBP monitoring session (according to the individual patient’s preference and device availability), using validated oscillometric devices (Spacelabs 90207 or 90217, Microlife WatchBP O3 or Meditech ABPM 04 and 05);25, 26, 27, 28 measurements were taken at 15–20 min intervals for 24 h, using a cuff size that fitted the individual’s arm circumference. The same type of ABP monitor was used for each individual throughout the study. Patients were instructed to perform their routine daily activities and remain still with their arm extended and relaxed during each measurement.
Daytime ABP was defined as the average of measurements taken between 1000–1400 h and 1800–2000 h, and nighttime ABP was defined as the average of measurements taken between 0100 and 0600 h. This approach was performed to exclude the potential impact of the afternoon sleep (siesta), which is particularly common in this country.29 Twenty subjects recorded sleeping hours in their diary. Non-dipping was defined as a <10% nighttime fall in systolic and/or diastolic ABP compared with daytime values.
Before each ABP or HBP monitoring session, the accuracy of each device was tested against a standard mercury sphygmomanometer by manual activation (three successive readings; Y connector) to ensure that there was no consistent BP difference >10 mm Hg.
Symptoms suggestive of orthostatic hypotension were assessed simultaneously with each seasonal BP evaluation, using a questionnaire that was a modified version of a validated orthostatic hypotension questionnaire.30 More specifically, subjects were asked to report a frequency score from 0 to 4 (recall period over the previous week) for each one of the following categories of symptoms: (i) generalized weakness and tiredness; (ii) postural dizziness; (iii) weakness in the upright position after awakening; (iv) problems with vision (blurring, seeing spots, etc.); and (v) dizziness and weakness a few hours after the intake of antihypertensive drugs (total score 0–20).
Meteorological parameters—discomfort indices
Data on meteorological parameters such as air temperature ([T], outdoor under shadow), atmospheric pressure (P) and humidity, during each BP monitoring period were obtained from the Hellinikon Meteorological Station of the Hellenic National Meteorological Service in Athens (www.hnms.gr). Three additional ‘discomfort indices’ were calculated using different meteorological parameters that express the level of the individual’s discomfort due to the weather conditions (Table 1). Index 1 includes T, wind velocity (V) and wet bulb temperature (Tw).31 The latter expresses the lowest temperature that can be reached by evaporating water into the air. Less evaporation occurs through perspiration as Tw approaches T. Skin temperature may begin to rise as a result. High V increases evaporation. Index 2 includes T and relative humidity (RH), which is the ratio of the amount of water vapor actually in the air to the maximum amount of water vapor required for saturation at that particular temperature and atmospheric pressure.32 Less water evaporates through perspiration with higher RH. Index 3 includes T, P and dew-point (Td), which represents the temperature to which air would have to be cooled for water saturation of the air to occur.33 The air saturation in water rises as Td approaches T, and less evaporation occurs through perspiration.
Data for each of the above meteorological parameters were retrieved from 3 hourly synoptic observations for the purpose of this study. These parameters were evaluated based on the dates of each BP monitoring session of each individual and separately for each BP measurement method. For CBP measurements, values of all meteorological parameters obtained at 0900, 1200 and 1500 h were averaged on the day of each clinic visit. For HBP monitoring, average values of the meteorological parameters of all monitoring days of each individual were calculated for each seasonal evaluation. For ABP monitoring, the average value of each parameter measured from 0900 to 1800 on the first day (when the ABP monitor was fitted to the participant), and 0600 to 1500 on the next day (when ABP recording was terminated) was calculated to obtain daytime ABP period values. Nighttime ABP parameters were calculated by averaging the data obtained from 2100 h on the first day (when the monitor was fitted to patient) to 0600 h on the next day.
Statistical analysis
The Kolmogorov–Smirnov test was used to assess the normality of the distribution of the study parameters. Normally distributed continuous variables were described as a mean±s.d., and median (interquartile range) values were used for non-parametric values. BP values exhibited a normal distribution; thus, Student’s paired t-test was used for the seasonal comparison of BP measurements in the same subjects, and unpaired t-test was used for comparisons between different groups of participants. Non-parametric tests (Wilcoxon, Mann–Whitney) were used for non-parametric variables. The chi-square test was used to assess differences between categorical variables. Pearson or Spearman bivariate correlation coefficients were used to examine the association of seasonal changes in BP and meteorological parameters/discomfort indices. The following variables were used as independent variables in stepwise multiple regression analysis of seasonal BP changes: gender, age, BMI, diabetes mellitus, cardiovascular disease, number of antihypertensive drugs, diuretic use, winter-1 systolic BP and winter-1 minus summer difference in temperature and discomfort indices. The summer systolic BP decline (%) (clinic, home and ambulatory) was the dependent variable. Normality of the regression residuals and collinearity diagnostics were checked. Statistical analysis was performed using SPSS 21 statistical software (SPSS, Chicago, IL, USA). A probability value of P<0.05 was considered as statistically significant.
Results
Participants’ characteristics
A total of 92 patients were recruited, and 32 patients were excluded (12 without winter-1 HBP measurements, 8 without summer HBP measurements, 2 without summer ABP monitoring, 3 with treatment change before summer evaluation and 7 who dropped out). The primary analysis included 60 subjects with complete BP data in winter-1 and summer. There was no difference in the characteristics of analyzed vs. excluded subjects, except for a trend for a higher percentage of males in the analyzed group (Table 2). Twenty-one subjects underwent treatment changes after the summer evaluation. Four of these patients returned to their initial antihypertensive drug therapy at least 4 weeks before the winter-2 evaluation, and these patients were included in the secondary analysis along with patients without treatment changes. Thirty-seven of the sixty subjects had complete BP data in winter-2, and these patients were included in the secondary analysis. There was no difference in the characteristics of the subjects with data for both winters (n=37) compared with subjects with data only for winter-1 (n=23) (data not shown).
BP levels
Table 3 shows the results of the primary analysis of CBP, HBP, daytime and nighttime ABP in winter-1 compared with summer. Seated CBP was reduced in summer by 7.0/1.9 mm Hg (systolic/diastolic), as well as erect systolic CBP, whereas erect diastolic BP increased (3.6/−3.5 mm Hg, respectively, P<0.05/<0.001). Average HBP was reduced by 4.9/2.9 mm Hg, and daytime ABP was reduced by 6.6/3.5 mm Hg (Table 3). However, there was no significant change in nighttime ABP (−1.2 /−0.3 mm Hg) (Table 3). Heart rate (assessed by radial artery palpation by the physician during clinic visits and automated home and ambulatory BP monitoring during out-of-office assessments) did not differ between seasons. Available data from 20 subjects on exact sleeping time during ABP monitoring revealed a trend toward shorter sleep duration during summer compared with winter-1 (442.5±87 vs. 471.2±96.6 min, respectively, P=0.12).
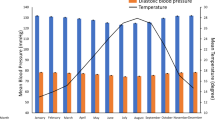
The secondary analysis (n=37) revealed a similar summer BP decline as the primary analysis, with a complete reversal in winter-2 to the same levels as winter-1 (Figure 1). The proportion of subjects classified as non-dippers increased in summer by 55% compared with winter-1 (85 and 55%, respectively, P<0.001, Figure 2).
Seasonal changes in blood pressure and temperature. Subjects with complete data for winter-1, summer and winter-2 were included (n=37). *P<0.05; NS, not significant, all comparisons vs. summer values. CBP, clinic blood pressure; HBP, home blood pressure; dABP, daytime ambulatory blood pressure; nABP, nighttime ambulatory blood pressure; Temp, temperature.
Orthostatic hypotension and weather-induced subjects’ discomfort
Fifteen subjects (25%) exhibited systolic daytime ABP <110 mm Hg in the summer evaluation. Thirteen subjects exhibited an increase in orthostatic symptoms score ⩾3 points, suggestive of orthostatic hypotension. Their absolute summer BP decline (compared with winter-1) was 11.1±11.5 mm Hg compared with 5.3±9.1 mm Hg in the remaining 47 subjects (P=0.06). Orthostatic hypotension symptoms were more frequent in summer compared with winter-1 [2.0 (3.0) vs. 2.0 (6.0), respectively, P<0.01]. Women exhibited more frequent symptoms in the summer evaluation than men [3.0 (7.0) vs. 1.0 (4.5), respectively, P<0.05]. A stepwise multivariate regression analysis with age, BMI, gender, summer systolic CBP, HBP and daytime ABP, history of diabetes or cardiovascular disease and all of the antihypertensive drug categories as independent variables demonstrated that the summer orthostatic hypotension symptoms score was determined (R2=0.22) by female gender (beta coefficient±s.e.: 2.14±0.86) and the intake of alpha-blockers (6.35±2.09). All discomfort indices (1–3) reflective of weather-induced subjects’ discomfort had higher values in summer compared with winter-1 (Table 3).
Subgroup analyses
Supplementary Table 1 presents the differences in CBP and orthostatic hypotension symptoms between winter-1 and summer according to gender, age, BMI and the presence/absence of treatment with diuretics. Women and subjects on diuretics had the largest summer decline in seated systolic CBP, and a similar trend was observed for subjects aged >70 years (Supplementary Table 1). The summer decline in erect systolic CBP was also larger in women and subjects on diuretics (Supplementary Table 1).
BP changes and meteorological parameters
The following average temperatures were recorded in Athens for the months analyzed in the study: 2009: December 14.3; 2010: January 11.0, February 12.9, March 13.9, June 26.1, July 29.6, August 31.0, September 25.1, December 13.8; 2011: January 10.6, February 11.1 and March 12.1 (°C). The seasonal change (winter-1 vs. summer) in systolic/diastolic daytime ABP was inversely correlated with the respective change in temperature (r=−0.34/−0.21), index 1 (−0.36/−0.23), index 2 (−0.36/−0.23) and index 3 (−0.29/−0.20) (all P <0.05). Figure 3 shows the associations for systolic daytime ABP. Multivariate analysis revealed that the summer BP decline was determined by winter-1 BP levels (for daytime ABP, CBP), seasonal differences in temperature (daytime ABP), female gender (HBP) and diuretic use (CBP) (Table 4).
Discussion
This prospective study investigated seasonal BP changes assessed by clinic, home and 24-h ambulatory measurements in treated hypertensives in relation to changes in meteorological parameters and weather-induced patients’ discomfort.
The following primary findings were observed in treated hypertensives: (i) all BP measurements were lower in summer, except nighttime ABP; (ii) these changes resulted in a higher prevalence of non-dippers in summer by 55% compared with winter; (iii) the summer BP decline was closely associated with changes in meteorological parameters reflective of weather-induced patients’ discomfort; (iv) old age, female gender and treatment with diuretics seemed to enhance the seasonal BP changes; and (v) large systolic BP decline during the summer that mandated treatment adjustment was not uncommon.
Although the seasonal BP changes have been recognized and reported in several previous studies,1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16 the present study has several methodological strengths: (i) the same individuals were included in all seasonal assessments; (ii) a second winter evaluation was performed to demonstrate a reversal of the summer changes and the reproducibility of the phenomenon, as well as to exclude an ‘order’ effect; (iii) all participants were treated for hypertension, and the seasonal changes were evaluated under the same antihypertensive drug treatment; (iv) a complete assessment of the BP profile was obtained using CBP, HBP and daytime and nighttime ABP measurements in all subjects; and (v) evaluations of several meteorological parameters and indices of weather-induced patients’ discomfort were performed simultaneously with BP evaluations.
The present study demonstrated seasonal variation in all aspects of the BP profile, with higher values in winter, except nighttime ABP, which remained unchanged. Seasonal BP changes in all BP monitoring methods occurred in a fairly similar range, which is reassuring for the clinical relevance of these findings. Although ABP might be expected to be more suitable method for the identification of seasonal BP changes, both CBP and HBP appear to be able to identify this phenomenon to a similar degree. These results are consistent with reports from previous studies.2, 3
To our knowledge, this is the first study to examine the relationship between seasonal changes in BP and composite discomfort indices other than temperature. Significant associations were observed between the seasonal change in daytime ABP and the change in several discomfort indices, which considered humidity and atmospheric pressure and reflected weather-induced subjects’ discomfort. All of these indices were higher in summer, which confirmed the expected weather-induced discomfort.
The different behavior of nighttime BP compared with all other BP measurements is a rather tricky finding. This result may be explained by the fact that people tend to maintain a more stable in-bed temperature during nighttime sleep that is rather similar in winter and summer (depending on the bed covers used and the body temperature). Discomfort during sleep due to high temperatures in summer leads to more fragmental sleep with more frequent arousals, which may also have a role. Indeed, this study revealed a trend toward shorter sleep duration during summer compared with winter. The decline in daytime, but not nighttime, BP in summer resulted in a more flat diurnal BP pattern with attenuation of the nocturnal dip. The absence of seasonal variability in nighttime ABP contrasts previous studies that demonstrated a rise in nighttime BP during summer.15, 16 However, the cross-sectional design in previous studies using different subjects in different seasons, and the fact that the participants could have used an uncontrolled down-titration of treatment in summer, may partially explain the nighttime BP rise.15, 16 Another prospective study in 50 hypertensives reported no seasonal change in nighttime ABP in winter and summer,2 which is consistent with the present study results. All of the studies agree that summer nighttime BP does not drop, in contrast to daytime BP, which inevitably leads to an increased proportion of non-dippers in summer.
This study demonstrated that large and clinically relevant BP declines during summer (systolic daytime ABP <110 mm Hg) appear to be common (25%) and should not be ignored. The cutoff value of systolic BP <110 mm Hg is somewhat arbitrary, but previous studies have demonstrated that this level is more clinically relevant in defining hypotension and hypoperfusion.34 This cutoff is a practical problem for clinicians, and there are no guidelines for optimal management because of a lack of evidence from relevant interventional studies. However, inferential reasoning suggests that a down-titration of treatment should be considered in summer, at least in subjects with excessive BP decline associated with symptomatic orthostasis. Furthermore, reductions in treatment may be sensible in patients with average systolic daytime ABP <110 mm Hg, despite the absence of relevant guidelines, particularly in the elderly. In other words, a down-titration of treatment should have been considered in as many as 25% of the present study participants, thus presenting a major clinical issue. This issue is timely and becomes even more important considering the recent more conservative hypertension guidelines regarding the BP goal to be achieved with treatment.21 Notably, the current recommendations for treatment-induced BP reduction are even more conservative in the elderly, who appear to have the additional problem of experiencing a larger BP decline in summer than younger hypertensives.21
Although seasonal BP changes have been described in previous studies,1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16 the mechanisms regarding the effects of meteorological parameters are not fully understood. One study in 20 hypertensives suggested that increased sympathetic nervous activity (assessed by norepinephrine excretion and plasma norepinephrine concentration) and increased kidney load of sodium (assessed by urinary sodium) may be contributing factors to the rise in BP in winter in patients with essential hypertension.35
Moreover, the present study suggests that other parameters, beyond meteorological ones, such as anthropometric (female gender, older age) and antihypertensive treatment characteristics (use of diuretics), may predict an exaggerated summer BP decline. However, there was inconsistency in the variables that appeared to influence the seasonal BP difference depending on the BP monitoring method (Table 4). This result may be attributed to the fact that each BP monitoring method is influenced by different parameters and provides different information on the BP profile and behavior. For example, CBP was performed in the morning, which is only a few hours after the morning antihypertensive drug intake, and therefore, it better demonstrates the peak effect of the treatment. HBP was performed under steady indoor conditions across several days, thus providing information of the trough drug effect in the morning and the plateau of the effect in the evening. Daytime ABP incorporates the effects of daily activity, which may be more affected by the outdoor climate conditions. These differences might explain, at least in part, the predictive value of the use of diuretics in the seasonal change of CBP and the higher R2 of the regression model for ABP. Previous studies have also suggested that parameters, such as gender, BMI and smoking status, may interfere with the seasonal BP variation, but these findings have not been consistent.11, 12, 14 It also appears that the seasonal BP variation is a complex phenomenon that is determined not only by environmental parameters but also by personal characteristics of individual subjects. Larger studies with subgroup analyses are required to determine subgroups of the population who are at high risk of clinically important summer BP decline that require intervention.
The present findings should be interpreted in light of some limitations. First, the study sample size was probably small to provide reliable subgroup analyses. Second, indoor temperature and the use of heating or air-conditioning were not taken into account. These results were obtained in a single city in the Mediterranean area, and seasonal changes in other climatic conditions may yield different findings. Previous studies have demonstrated that the correlation between indoor and outdoor temperature in warm climates appears to be higher than in cold climates (for outdoor temperature range 9.8–27.7 °C; r=0.84 and for −3.4–9.7 °C; r=0.28).36 The average temperature for both winter seasons was approximately 12.5 °C in this study compared with 28 °C in the summer. Therefore, it may be argued that the lack of information on indoor temperature in the present study may have not considerably affected the findings. These findings apply to treated hypertensives only, and the results might differ in untreated subjects or subjects of other races or ages. Notably, this study used 4 months as the definition of winter (December–March) and summer (June–September) season. This timeframe allowed for a slight increase in our recruitment, and it was based on meteorological data that exhibited few differences in the average temperature of the ‘additional months’ compared with the respective season.
In conclusion, seasonal variation affected all aspects of the BP profile, except nighttime BP, which was not changed. Therefore, there is a considerable increase in non-dippers in summer, but the consequences of this increase are not known. The seasonal BP changes were affected by changes in meteorological parameters, and anthropometric and antihypertensive treatment characteristics. Excessive BP decline in summer is not uncommon, and this decline deserves further investigation. There is an urgent need for controlled trials to evaluate the clinical relevance of excessive BP decline in summer and the development of management guidelines for practicing physicians on the optimal management of such cases.
References
Giaconi S, Ghione S, Palombo C, Genovesi-Ebert A, Marabotti C, Fommei E, Donato L . Seasonal influences on blood pressure in high normal to mild hypertensive range. Hypertension 1989; 14: 22–27.
Minami J, Kawano Y, Ishimitsu T, Yoshimi H, Takishita S . Seasonal variations in office, home and 24 h ambulatory blood pressure in patients with essential hypertension. J Hypertens 1996; 14: 1421–1425.
Sega R, Cesana G, Bombelli M, Grassi G, Stella ML, Zanchetti A, Mancia G . Seasonal variations in home and ambulatory blood pressure in the PAMELA population. Pressione Arterios Monitorate e Loro Associazioni. J Hypertens 1998; 16: 1585–1592.
Minami J, Ishimitsu T, Kawano Y, Matsuoka H . Seasonal variations in office and home blood pressures in hypertensive patients treated with antihypertensive drugs. Blood Press Monit 1998; 3: 101–106.
Morabito M, Crisci A, Orlandini S, Maracchi G, Gensini GF . A synoptic approach to weather conditions discloses a relationship with ambulatory blood pressure in hypertensives. Am J Hypertens 2008; 21: 748–752.
Hayashi T, Ohshige K, Sawai A, Yamasue K, Tochikubo O . Seasonal influence on blood pressure in elderly normotensive subjects. Hypertens Res 2008; 31: 569–574.
Alperovich A, Lacombe JM, Hanon O, Dartigues JF, Ritchie K, Ducimetiere P, Tzourio C . Relationship between blood pressure and outdoor temperature in a large sample of elderly individuals. The Three-City Study. Arch Intern Med 2009; 169: 75–80.
Kimura T, Senda S, Masugata H, Yamagami A, Okuyama H, Kohno T, Hirao T, Fukunaga M, Okada H, Goda F . Seasonal blood pressure variation and its relationship to environmental temperature in healthy elderly Japanese studied by home measurements. Clin Exp Hypertens 2010; 32: 8–12.
Murikami S, Otsuka K, Kono T, Soyama A, Umeda T, Yamamoto N, Morita H, Yamanaka G, Kitaura Y . Impact of outdoor temperature on prewaking morning surge and nocturnal decline in blood pressure in a Japanese population. Hypertens Res 2011; 34: 70–73.
Hozawa A, Kuriyama S, Shimazu T, Ohmori-Matsuda K, Tsuji I . Seasonal variation in home blood pressure measurements and relation to outside temperature in Japan. Clin Exp Hypertens 2011; 33: 153–158.
Lewington S, Li L, Sherliker P, Guo Y, Millwood I, Bian Z, Whitlock G, Yang L, Collins R, Chen J, Wu X, Wang S, Hu Y, Jiang L, Yang L, Lacey B, Peto R, Chen Z . China Kadoorie Biobank study collaboration. Seasonal variation in blood pressure and its relationship with outdoor temperature in 10 diverse regions of China: the China Kadoorie Biobank. J Hypertens 2012; 30: 1383–1391.
Tu YK, Chien KL, Chiu YW, Ellison GT . Seasonal variation in blood pressure is modulated by gender and age but not by BMI in a large Taiwanese population, 1996-2006. J Am Soc Hypertens 2013; 7: 216–228.
Modesti PA, Morabito M, Massetti L, Rapi S, Orlandini S, Mancia G, Gensini GF, Parati G . Seasonal blood pressure changes: an independent relationship with temperature and daylight hours. Hypertension 2013; 61: 908–914.
Kristal-Boneh E, Harari G, Green MS . Seasonal change in 24- hour blood pressure and heart rate is greater among smokers than nonsmokers. Hypertension 1997; 30: 436–441.
Modesti PA, Morabito M, Bertolozzi I, Massetti L, Panci G, Lumachi C, Giglio A, Bilo G, Caldara G, Lonati L, Orlandini S, Maracchi G, Mancia G, Gensini GF, Parati G . Weather-related changes in 24- hour blood pressure profile: effects of age and implications for hypertension management. Hypertension 2006; 47: 155–161.
Fedecostante M, Barbatelli P, Guerra F, Espinosa E, Dessì-Fulgheri P, Sarzani R . Summer does not always mean lower: seasonality of 24 h, daytime, and nighttime blood pressure. J Hypertens 2012; 30: 1392–1398.
van Rossum CT, Shipley MJ, Hemingway H, Grobbee DE, Mackenbach JP, Marmot MG . Seasonal variation in cause-specific mortality: are there high-risk groups? 25-year follow-up of civil servants from the first Whitehall study. Int J Epidemiol 2001; 30: 1109–1116.
Sheth T, Nair C, Muller J, Yusuf S . Increased winter mortality from acute myocardial infarction and stroke: the effect of age. J Am Coll Cardiol 1999; 33: 1916–1919.
Analitis A, Katsouyanni K, Biggeri A, Baccini M, Forsberg B, Bisanti L, Kirchmayer U, Ballester F, Cadum E, Goodman PG, Hojs A, Sunyer J, Tiittanen P, Michelozzi P . Effects of cold weather on mortality: results from 15 European cities within the PHEWE project. Am J Epidemiol 2008; 168: 1397–1408.
Kamezaki F, Sonoda S, Nakata S, Muraoka Y, Okazaki M, Tamura M, Abe H, Tekeuchi M, Otsuji Y . Association of seasonal variation in the prevalence of metabolic syndrome with insulin resistance. Hypertens Res 2013; 36: 398–402.
Mancia G, Fagard R, Narkiewicz K, Redón J, Zanchetti A, Böhm M, Christiaens T, Cifkova R, De Backer G, Dominiczak A, Galderisi M, Grobbee DE, Jaarsma T, Kirchhof P, Kjeldsen SE, Laurent S, Manolis AJ, Nilsson PM, Ruilope LM, Schmieder RE, Sirnes PA, Sleight P, Viigimaa M, Waeber B, Zannad F, Task Force Members. 2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens 2013; 31: 1281–1357.
Stergiou GS, Lin CW, Lin CM, Chang SL, Protogerou AD, Tzamouranis D, Nasothimiou E, Tan TM . Automated device that complies with current guidelines for office blood pressure measurement: design and pilot application study of the Microlife WatchBP Office device. Blood Press Monit 2008; 13: 231–235.
O'Brien E, Petrie J, Littler W, de Swiet M, Padfield PL, Altman DG, Bland M, Coats A, Atkins N . An outline of the revised British Hypertension Society protocol for the evaluation of blood pressure measuring devices. J Hypertens 1993; 11: 677–679.
Stergiou GS, Giovas PP, Gkinos CP, Patouras JD . Validation of the Microlife WatchBP Home device for self home blood pressure measurement according to the International Protocol. Blood Press Monit 2007; 12: 185–188.
O'Brien E, Mee F, Atkins N, O'Malley K . Accuracy of the Spacelabs 90207 determined by to the British Hypertension Society Protocol. J Hypertens 1991; 9 (Suppl 5): S25–S31.
Baumgart P, Kamp J . Accuracy of the Spacelabs Medical 90217 ambulatory blood pressure monitor. Blood Press Monit 1998; 3: 303–307.
Ragazzo F, Saladini F, Palatini P . Validation of the Microlife WatchBP O3 device for clinic, home, and ambulatory blood pressure measurement, according to the International Protocol. Blood Press Monit 2010; 15: 59–62.
Barna I, Keszei A, Dunai A . Evaluation of Meditech ABPM-04 ambulatory blood pressure measuring device according to the British Hypertension Society protocol. Blood Press Monit 1998; 3: 363–368.
Stergiou GS, Malakos JS, Zourbaki AS, Achimastos AD, Mountokalakis TD . Blood pressure during siesta: effect on 24- h ambulatory blood pressure profiles analysis. J Hum Hypertens. 1997; 11: 125–131.
Kaufmann H, Malamut R, Norcliffe-Kaufmann L, Rosa K, Freeman R . The Orthostatic Hypotension Questionnaire (OHQ): validation of a novel symptom assessment scale. Clin Auton Res 2012; 22: 79–90.
Thom EC . The discomfort index. Weatherwise 1959; 12: 57–60.
Zambakas JD . General Climatology, 1st edn. Athina: Athens, Greece. 1981 pp 322–329.
Hufty A . Introduction à la climatologie, 1st edn. Presses Universitaires de France: Paris, France. 1976 p 225.
Eastridge BJ, Salinas J, McManus JG, Blackburn L, Bugler EM, Cooke WH, Convertino VA, Wade CE, Holcomb JB . Hypotension begins at 110 mm Hg: redefining "hypotension" with data. J Trauma. 2007; 6: 291–297.
Hata T, Ogihara T, Maruyama A, Mikami H, Nakamaru M, Naka T, Kumahara Y, Nugent CA . The seasonal variation of blood pressure in patients with essential hypertension. Clin Exp Hypertens A 1982; 4: 341–354.
Saeki K, Obayashi K, Iwamoto J, Tone N, Okamoto N, Tomioka K, Kurumatani N . The relationship between indoor, outdoor and ambient temperatures and morning BP surges from inter-seasonally repeated measurements. J Hum Hypertens 2014; 28: 482–488.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on Hypertension Research website
Supplementary information
Rights and permissions
About this article
Cite this article
Stergiou, G., Myrsilidi, A., Kollias, A. et al. Seasonal variation in meteorological parameters and office, ambulatory and home blood pressure: predicting factors and clinical implications. Hypertens Res 38, 869–875 (2015). https://doi.org/10.1038/hr.2015.96
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2015.96
Keywords
This article is cited by
-
Seasonal variation in blood pressure and its impact on target organ damage and cardiovascular disease incidence
Hypertension Research (2023)
-
Seasonal variation in the effect of antihypertensive treatment with the irbesartan/hydrochlorothiazide combination
Hypertension Research (2023)
-
Gender-specific effect of outdoor temperature and seasonal variation on blood pressure components: a cross-sectional study on Iranian adults from 2015 to 2018
Environmental Science and Pollution Research (2023)
-
Novel insights into the association between seasonal variations, blood pressure, and blood pressure variability in patients with new-onset essential hypertension
BMC Cardiovascular Disorders (2022)
-
The accuracy of 8-hour ambulatory blood pressure monitoring, adjusted to seasons
Journal of Human Hypertension (2022)