Abstract
The pupil is a suitable end organ for studying autonomic function because both sympathetic and parasympathetic nerve activity can be evaluated independently using a light stimulus. Sympathetic response elicited by physical stress is augmented in hypertensive patients compared with normotensive subjects, which increases the risk of cardiovascular events. We used pupillometry to evaluate the effects of the calcium channel blockers azelnidipine (AZ) and amlodipine (AM) on changes in autonomic nervous activity induced by isometric exercise in patients with hypertension. Twenty patients with essential hypertension who were administered AM and 21 who were administered AZ underwent a pupillary function test and blood pressure (BP) and pulse rate (PR) measurements before and after isometric handgrip exercise (IHG). Maximal velocities of pupil constriction (VC) and re-dilation (VD) obtained with light stimulation for 1 s were used as indices of parasympathetic and sympathetic nerve activity, respectively. Increases in systolic BP and PR elicited by IHG were significantly smaller in the AZ group than in the AM group. After IHG, both VC and VD significantly increased in the AM group but not in the AZ group. The low-to-high frequency ratio obtained from analysis of PR variability, another measure of sympathetic activity, also increased in only the AM group. Thus AZ inhibited autonomic activation and suppressed cardiovascular responses to IHG more effectively than AM. The sympathoinhibitory effect of AZ may therefore be beneficial for patients with essential hypertension. In addition, pupillometry was shown to be a useful tool for assessing autonomic function in hypertensive patients.
Similar content being viewed by others
Introduction
An increase in sympathetic nerve activity (SNA) is an important cause of the onset and maintenance of hypertension.1, 2 Psychological and physical stress increase SNA and therefore elevate blood pressure (BP) in healthy individuals3, 4 and in patients with hypertension.5 SNA and BP are more reactive to mental and physical stress in experimental hypertensive animals than in normotensive animals.6 Sympathetic and pressor responses elicited by mental and physical stress are also augmented in hypertensive humans compared with normotensive subjects.7, 8 This sympathetic hyper-reactivity to stress might increase the risk for coronary events.9 Sympathetic activation in hypertensive patients is associated with a decrease in the reactive hyperemia index, a marker of resistance artery endothelial function.10
Calcium channel blockers (CCBs) are used widely in Japan as first-line agents for treating hypertension.11, 12 However, administration of CCBs, in particular short-acting dihydropyridine CCBs, can elicit sympathoexcitation via the baroreceptor unloading induced by their depressor action.13 This reflex sympathoexcitation increases cardiac workload, resulting in cardiac complications such as coronary heart disease.14, 15 Long-acting dihydropyridine CCBs reduce sympathoexcitation more than short-acting dihydropyridine CCBs. Although amlodipine (AM) is a long-acting dihydropyridine CCB used frequently for antihypertensive therapy, it remains controversial as to whether AM produces sympathetic activation. Several reports have shown that administration of AM does not elicit sympathoexcitation in patients with essential hypertension.16, 17, 18 However, others have demonstrated that AM increases SNA and tachycardia in hypertensive patients.19, 20, 21 In contrast, azelnidipine (AZ), another long-acting dihydropyridine CCB, has consistently been reported not to elicit increases in heart rate or SNA in hypertensive model animals22 and hypertensive patients.20, 23, 24, 25 These studies of the relationship between AZ and SNA have compared AZ with other CCBs or compared SNA before and after the administration of AZ. However, the effect of AZ on the acute autonomic responses of hypertensive patients to physical stress such as isometric exercise has yet to be shown.
The pupil is an appropriate end organ for studying autonomic function because sympathetic and parasympathetic nerves innervate the dilator and constrictor pupillae muscles of the iris, respectively. Both SNA and parasympathetic nerve activity can be evaluated quickly and independently by the pupillary function test using light stimulus.26, 27, 28 Since pupillography was developed in 1958,29 it has been used as an effective tool in the analysis of autonomic dysfunction associated with various diseases, such as diabetes,30 heart failure,31 Parkinson’s disease,32 Alzheimer’s disease33 and head injury.34 Pupillometry is a simple, non-invasive and cost-effective method to assess autonomic nerve activity.26, 35 However, to our knowledge, autonomic activity has not been assessed by pupillometry in patients with hypertension, except in our previous study.36
In the present study, we used pupillometry to compare the effects of AM and AZ on the changes in autonomic activity induced by isometric handgrip exercise (IHG) in patients with essential hypertension under the hypothesis that AZ reduces sympathetic activation elicited by IHG compared with AM.
Methods
Participants
We enrolled a total of 41 consecutive outpatients with essential hypertension who had been administered AM (n=20) or AZ (n=21) for at least 6 months at Wakayama Medical University Hospital or a satellite clinic of the university. Patients diagnosed with secondary hypertension, orthostatic hypotension, diabetes, cataract, retinal disorders or other medical issues requiring specific treatment were excluded. Patients administered alpha- and/or beta-adrenergic antagonists were also excluded. Informed consent to the study protocol was obtained in writing from all participants. The study conformed to the principles of the Declaration of Helsinki and was approved by the Ethics Committee of Wakayama Medical University.
Study protocol
The general protocols were described in detail in our previous publication.36 Briefly, all tests were performed between 0900 and 1200 hours in a dim room at a controlled temperature of 25 °C. After resting for 15 min to allow their eyes to adjust to the low light levels, each participant underwent a pupillary function test, and BP, pulse rate (PR) and PR variability were measured within 2 min in a sitting position. IHG was then performed for 1 min. The pupillary function test and BP, PR, and PR variability measurements were performed again within 2 min after completion of IHG.
Isometric handgrip exercise
Maximal voluntary contraction of the right hand was measured using a JAMAR hydraulic hand dynamometer (Patterson Medical Holdings, Bolingbrook, IL, USA) before resting for 15 min in a sitting position. Isometric contraction was maintained for 1 min at 70% of the maximal voluntary contraction. Patients were instructed to breathe naturally during the isometric exercise to avoid a Valsalva maneuver, and their respiratory profiles were observed throughout the exercise.
Measurement parameters
BP and PR were monitored using an autonomic sphygmomanometer (COLIN 203i; OMRON, Tokyo, Japan) on the left radial artery, and parameters of the pupillary light reflex were measured using a pupillograph (Iriscorder Dual C10641; Hamamatsu Photonics, Hamamatsu, Japan) before and after IHG. Figure 1 indicates the indices of pupillary tests obtained from successive changes in pupil diameter elicited by red light stimulating both eyes simultaneously for 1 s. Average values of initial pupil diameter (D1), minimal pupil diameter (D2), contraction ratio (CR) obtained from the formula (D1−D2)/D1 and maximal velocities of pupil constriction (VC) and re-dilation (VD) obtained from each pupil were adopted as parameters of pupillary function. On the basis of previous reports,32, 36 VD was used as an index of SNA, and VC was used as an index of parasympathetic nerve activity.
PR variability
In order to calculate the low-frequency to high-frequency (LF/HF) ratio, an acceleration pulse wave measurement system (Artett C; U-Medica, Osaka, Japan) was used. Variation of the pulse interval, obtained by monitoring the pulse wave in the left middle finger for 1 min, was analyzed with fast Fourier transform. The LF component was calculated as the power within a frequency range of 0.02–0.15 Hz, and the HF component was calculated as that within a frequency range of 0.15–0.50 Hz. The LF/HF ratio was then used as an index of SNA.37
Statistical analysis
Differences between the AM-treated and AZ-treated groups in age, body mass index, maximal voluntary contraction of handgrip and baseline BP and PR were examined with Student’s unpaired t-test. Analysis of covariance with treatment regimen (AM or AZ) and baseline BP and PR measured before IHG as explanatory variables was used to compare the changes in BP and PR elicited by IHG between the two groups. Rates of males and females, smokers, patients with dyslipidemia or hyperuricemia and patients administered angiotensin II receptor antagonists and/or diuretics were compared between the groups by the chi-square test. Student’s paired t-test was used for comparisons of BP, PR, D1, D2, CR, VC, VD and LF/HF ratio before and after IHG within groups. Data are expressed as means±s.e.m., with P<0.05 taken to indicate a significant difference.
Results
Baseline characteristics
The baseline characteristics in the AM and AZ groups are shown in Table 1. There were no significant differences between the AM and AZ groups on any measure. In some patients, CCBs were administered in combination with angiotensin II receptor antagonists and/or diuretics, and the rates of patients administered these drugs in combination with CCBs were not statistically different between the groups.
BP and PR
There were no differences between the AZ and AM groups in baseline systolic BP (SBP), diastolic BP (DBP) or PR measured before IHG. IHG significantly (P<0.01) increased DBP and PR in both the AM and AZ groups (Figures 2b and c). However, IHG did not alter SBP in the AZ group, although it significantly (P<0.001) increased SBP in the AM group (Figure 2a).
Changes in SBP (a), DBP (b) and PR (c) after isometric handgrip exercise in the amlodipine and azelnidipine groups. Values are expressed as means±s.e.m. Aft IHG, after isometric handgrip exercise; AM, amlodipine; AZ, azelnidipine; Bef IHG, before isometric handgrip exercise; DBP, diastolic blood pressure; NS, not significant, PR, pulse rate; SBP, systolic blood pressure. *P<0.05, †P<0.01, ‡P<0.001.
The increase in SBP elicited by IHG was significantly (P<0.05) smaller in the AZ group (3.8±2.6 mm Hg) than in the AM group (11.3±2.9 mm Hg) (Figure 2a). The increase in PR elicited by IHG was also significantly (P<0.01) smaller in the AZ group (2.1±0.5 min−1) than in the AM group (5.1±0.9 min−1) (Figure 2c). The increase in DBP elicited by IHG did not differ between the two groups: increases in DBP in the AZ and AM groups were 4.2±1.4 and 7.7±1.9 mm Hg, respectively (Figure 2b).
Pupillary function
D1 remained unchanged after IHG in both the AM and AZ groups. D1 before and after IHG was 4.54±0.21 and 4.46±0.19 mm, respectively, in the AM group and 4.59±0.23 and 4.42±0.25 mm, respectively, in the AZ group. D2 after light stimulus also remained unaltered by IHG in both groups: D2 before and after IHG was 3.35±0.14 and 3.22±0.16 mm, respectively, in the AM group and 3.34±0.17 and 3.31±0.19 mm, respectively, in the AZ group. There was no significant difference in CR before and after IHG in each group: 0.25±0.03 and 0.28±0.03, respectively, in the AM group and 0.27±0.02 and 0.25±0.02, respectively, in the AZ group.
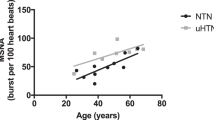
VC increased significantly after IHG in the AM group but not in the AZ group. VC before and after IHG was 3.53±0.26 and 4.52±0.41 mm s−1, respectively, in the AM group (P<0.05) and 3.58±0.18 and 3.64±0.28 mm s−1, respectively, in the AZ group (P>0.05) (Figure 3a). VD also increased significantly after IHG but only in the AM group. VD before and after IHG was 1.82±0.15 and 2.64±0.23 mm s−1, respectively, in the AM group (P<0.01) and 1.73±0.14 and 2.08±0.30 mm s−1, respectively, in the AZ group (P>0.05) (Figure 3b).
Comparison of changes in VC (a) and VD (b) induced by isometric handgrip exercise in the azelnidipine group (filled circles) and amlodipine group (unfilled circles). Values are expressed as means±s.e.m. Significant differences from baseline (resting) values in the amlodipine group: *P<0.05, †P<0.01.
LF/HF ratio
The LF/HF ratio increased significantly after IHG only in the AM group. The LF/HF ratio before and after IHG was 2.17±0.46 and 4.71±1.00 mm s−1, respectively, in the AM group (P<0.05) and 3.54±0.62 and 3.46±0.69 mm s−1, respectively, in the AZ group (P>0.05) (Figure 4).
Comparison of changes in the LF/HF ratio induced by isometric handgrip exercise in the azelnidipine group (filled circles) and amlodipine group (unfilled circles). Values are expressed as means±s.e.m. Significant difference from baseline (resting) values in the amlodipine group: *P<0.05. LF/HF, ratio of low frequency to high frequency.
Discussion
In this study, we found that AZ, but not AM, inhibited the expected increases in SNA, as assessed by pupillometry and analysis of PR variability and elevations of SBP and PR elicited by IHG were significantly reduced in the AZ group compared with the AM group.
In clinical studies, plasma catecholamines, sympathetic skin response and heart rate variability have generally been used for the assessment of SNA. However, measurement of plasma catecholamines is not suitable for this study because repetitive blood sampling elicits pain, which can change the levels of catecholamines, and a time lag exists between the physical loading and elevation of plasma catecholamines. The sympathetic skin response test requires direct electric stimulation of the skin, and the response habituates when stimuli are applied with short intervals.38 Pupillometry using light stimuli is a reproducible and non-invasive method for the assessment of autonomic function.26, 33, 39 Moreover, pupillometry can evaluate sympathetic and parasympathetic function separately in a short time and is not affected by the secretion of catecholamines from the adrenal gland.26, 33 Consequently, we used pupillometry to evaluate autonomic activity in this study.
Sympathetic activation during IHG dilates the pupil.40 It is not clear whether pupillary autonomic activity reflects other autonomic activity contributing to cardiovascular regulation, such as renal SNA. However, because isometric exercise has been also reported to increase renal SNA,41 renal and pupillary sympathetic activity may change in a parallel manner at least during isometric exercise.
The present study showed no significant differences in D1, D2 or CR before and after IHG in either the AM or the AZ group. This finding is in agreement with a previous study that did not find a change in pupil diameter in the recovery phase following exercise.40 However, VC and VD, indices of parasympathetic nerve activity and SNA, respectively, increased in the AM group after IHG. VC and VD may therefore be more sensitive than pupil diameter for the measurement of pupillary autonomic activity. The increases in VC elicited by IHG in the AM group can be explained as a counteraction to sympathetic activation. In contrast, in the AZ group, changes in VC by IHG were completely inhibited and no significant changes in VD were observed. These results suggest that AZ inhibits the sympathetic activation elicited by the exercise and counteractive changes in pupillary parasympathetic activity were not elicited as pupillary SNA was not altered by IHG. In each group, the change in VD induced by IHG was consistent with the change in the LF/HF ratio. Therefore, we were able to validate the VD changes in pupillometry as an excellent indicator of SNA obtained by the LF/HF ratio of heart rate variability. Indeed, pupillary autonomic function has been reported to correlate with cardiac autonomic function assessed by heartbeat interval.42 The inhibitory effect of AZ on sympathetic activation might result in a significant reduction of SBP and PR elevation elicited by IHG compared with AM.
Several reports have shown a sympathoinhibitory effect of AZ. In studies using hypertensive model animals, infusion of AZ did not elicit reflex renal sympathetic activation by its depressor effect, whereas infusion of AM did.22 The reduction of SNA elicited by AZ administration is mediated by its antioxidant effect on the rostral ventrolateral medulla.43 In patients with hypertension, AZ has been reported to reduce serum norepinephrine levels.44 A recent study showed that resting muscle SNA is reduced in hypertensive patients who were given AZ compared with patients who were given AM.45 Although the present study showed that significant increases in VD and the LF/HF ratio after IHG were observed in the AM group, but not in the AZ group, these indices of SNA before IHG were similar between the two groups. The inhibitory effect of AZ on SNA may appear more remarkable after isometric exercise than at rest. It has been reported that baroreflex sensitivity was improved by AZ therapy but not by AM therapy.25 The inhibitory effects of AZ on the acute sympathoexcitation induced by IHG observed in this study may be partly due to the improving effect of AZ on baroreflex sensitivity. In spite of the inhibitory effect of AZ on IHG-induced sympathoexcitation, IHG significantly increased DBP and PR even in the AZ group. The reason for this finding remains unclear but could be explained by adrenal gland activation as a result of IHG.
Calcium channels are classified into several subtypes, including L-type and T-type.46 L-type calcium channels in vascular smooth muscle participate in vascular contraction.47, 48 T-type calcium channels are present in the sinoatrial node in the heart and accelerate pacemaker depolarization.49 AZ, but not AM, blocks T-type calcium channels in addition to L-type channels.50 This pharmacological difference may also explain the smaller elevation of PR in the AZ group compared with the AM group.
A limitation of this study was that only patients treated with antihypertensive drugs were enrolled. The participation of individuals with untreated hypertension was not permitted by our Ethics Committee, because it has been reported that the pressor responses induced by IHG are greater in hypertensive patients than in normotensive subjects,8 and such augmented pressor responses can be a risk for cardiovascular events.
In conclusion, pupillometry is useful for assessing autonomic function in hypertensive patients. Using pupillometry, we found that, compared with AM, AZ inhibited autonomic activation and elevation of SBP and PR elicited by IHG among patients with essential hypertension. These effects of AZ may be beneficial for hypertensive patients.
References
Esler M, Jennings G, Lambert G . Noradrenaline release and the pathophysiology of primary human hypertension. Am J Hypertens 1989; 2: 140–146.
Esler M . The sympathetic system and hypertension. Am J Hypertens 2000; 13 (Suppl 2): 99S–105S.
Lucini D, Norbiato G, Clerici M, Pagani M . Hemodynamic and autonomic adjustments to real life stress conditions in humans. Hypertension 2002; 39: 184–188.
Leuenberger U, Sinoway L, Gubin S, Gaul L, Davis D, Zelis R . Effects of exercise intensity and duration on norepinephrine spillover and clearance in humans. J Appl Physiol (1985) 1993; 75: 668–674.
Victor RG, Leimbach WN Jr, Seals DR, Wallin BG, Mark AL . Effects of the cold pressor test on muscle sympathetic nerve activity in humans. Hypertension 1987; 9: 429–436.
Li SG, Lawler JE, Randall DC, Brown DR . Sympathetic nervous activity and arterial pressure responses during rest and acute behavioral stress in SHR versus WKY rats. J Auton Nerv Syst 1997; 62: 147–154.
Matsukawa T, Gotoh E, Uneda S, Miyajima E, Shionoiri H, Tochikubo O, Ishii M . Augmented sympathetic nerve activity in response to stressors in young borderline hypertensive men. Acta Physiol Scand 1991; 141: 157–165.
Delaney EP, Greaney JL, Edwards DG, Rose WC, Fadel PJ, Farquhar WB . Exaggerated sympathetic and pressor responses to handgrip exercise in older hypertensive humans: role of the muscle metaboreflex. Am J Physiol Heart Circ Physiol 2010; 299: H1318–H1327.
Julius S . Sympathetic hyperactivity and coronary risk in hypertension. Hypertension 1993; 21: 886–893.
Tomiyama H, Yoshida M, Higashi Y, Takase B, Furumoto T, Kario K, Ohya Y, Yamashina A, sub-group study of FMD-J. Autonomic nervous activation triggered during induction of reactive hyperemia exerts a greater influence on the measured reactive hyperemia index by peripheral arterial tonometry than on flow-mediated vasodilatation of the brachial artery in patients with hypertension. Hypertens Res 2014; 37: 914–918.
Kansui Y, Ibaraki A, Goto K, Haga Y, Seki T, Takiguchi T, Ohtsubo T, Kitazono T, Matsumura K . Trends in blood pressure control and medication use during 20 years in a hypertension clinic in Japan. Clin Exp Hypertens 2016; 30: 1–6.
Shimamoto K, Ando K, Fujita T, Hasebe N, Higaki J, Horiuchi M, Imai Y, Imaizumi T, Ishimitsu T, Ito M, Ito S, Itoh H, Iwao H, Kai H, Kario K, Kashihara N, Kawano Y, Kim-Mitsuyama S, Kimura G, Kohara K, Komuro I, Kumagai H, Matsuura H, Miura K, Morishita R, Naruse M, Node K, Ohya Y, Rakugi H, Saito I, Saitoh S, Shimada K, Shimosawa T, Suzuki H, Tamura K, Tanahashi N, Tsuchihashi T, Uchiyama M, Ueda S, Umemura S . Japanese Society of Hypertension Committee for Guidelines for the Management of Hypertension. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2014). Hypertens Res 2014; 37: 253–390.
Rigel DF, Millard RW . Effects of calcium channel antagonists on carotid sinus baroreflex control of arterial pressure and heart rate in anesthetized dogs. Circ Res 1989; 64: 276–286.
Furberg CD, Psaty BM, Meyer JV . Nifedipine: dose-related increase in mortality in patients with coronary heart disease. Circulation 1995; 92: 1326–1331.
Psaty BM, Heckbert SR, Koepsell TD, Siscovick DS, Raghunathan TE, Weiss NS, Rosendaal FR, Lemaitre RN, Smith NL, Wahl PW . The risk of myocardial infarction associated with antihypertensive drug therapies. JAMA 1995; 274: 620–625.
Hamada T, Watanabe M, Kaneda T, Ohtahara A, Kinugawa T, Hisatome I, Fujimoto Y, Yoshida A, Shigemasa C . Evaluation of changes in sympathetic nerve activity and heart rate in essential hypertensive patients induced by amlodipine and nifedipine. J Hypertens 1998; 16: 111–118.
Minami J, Ishimitsu T, Kawano Y, Matsuoka H . Effects of amlodipine and nifedipine retard on autonomic nerve activity in hypertensive patients. Clin Exp Pharmacol Physiol 1998; 25: 572–576.
Binggeli C, Corti R, Sudano I, Luscher TF, Noll G . Effects of chronic calcium channel blockade on sympathetic nerve activity in hypertension. Hypertension 2002; 39: 892–896.
Eguchi K, Kario K, Shimada K . Differential effects of a long-acting angiotensin converting enzyme inhibitor (temocapril) and a long-acting calcium antagonist (amlodipine) on ventricular ectopic beats in older hypertensive patients. Hypertens Res 2002; 25: 329–333.
Kuramoto K, Ichikawa S, Hirai A, Kanada S, Nakachi T, Ogihara T . Azelnidipine and amlodipine: a comparison of their pharmacokinetics and effects on ambulatory blood pressure. Hypertens Res 2003; 26: 201–208.
Lindqvist M, Kahan T, Melcher A, Ekholm M, Hjemdahl P . Long-term calcium antagonist treatment of human hypertension with mibefradil or amlodipine increases sympathetic nerve activity. J Hypertens 2007; 25: 169–175.
Shokoji T, Fujisawa Y, Kiyomoto H, Matlubur R, Guang-Ping S, Yu-Yan F, Kimura S, Kohno M, Abe Y, Nishiyama A . Effects of a new calcium channel blocker, azelnidipine, on systemic hemodynamics and renal sympathetic nerve activity in spontaneously hypertensive rats. Hypertens Res 2005; 28: 1017–1023.
Wellington K, Scott LJ . Azelnidipine. Drugs 2003; 63: 2613–2624.
Yamaguchi T . Efficacy of azelnidipine on home blood pressure and pulse rate in patients with essential hypertension: comparison with amlodipine. Hypertens Res 2006; 29: 767–773.
Eguchi K, Tomizawa H, Ishikawa J, Hoshide S, Fukuda T, Numao T, Shimada K, Kario K . Effects of a new calcium channel blocker, azelnidipine, and amlodipine on baroreflex sensitivity ambulatory blood pressure. J Cardiovasc Pharmacol 2007; 49: 394–400.
Fotiou F, Fountoulakins KN, Goulas A, Alexopoulos L, Palikaras A . Automated standardized pupillometry with optical method for purposes of clinical practice and research. Clin Physiol 2000; 20: 336–347.
Yamaji K, Hirata Y, Usui S . A method for monitoring Autonomous Nervous activity by pupillary flash response. Syst Comput Jpn 2000; 31: 2447–2456.
Barbur JL. Learning from the pupil: studies of basic mechanisms and clinical applications. In: Chalpura LM, Werner JS (eds). The Visual Neurosciences. MIT Press: Cambridge, MA, USA. 2004, pp 641–656.
Lowenstein O, Loewenfeld IE . Electronic pupillography; a new instrument and some clinical applications. AMA Arch Ophthalmol 1958; 59: 352–363.
Pina SJ, Halonen JP . Infrared pupillometry in the assessment of autonomic function. Diabetes Res Clin Pract 1994; 26: 61–66.
Keivanidou A, Fotiou D, Arnaoutoglou C, Arnaoutoglou M, Fotiou F, Karlovasitou A . Evaluation of autonomic imbalance in patients with heart failure: a preliminary study of pupillomotor function. Cardiol J 2010; 17: 65–72.
Jain S, Siegle GJ, Gu C, Moore CG, Ivanco LS, Jennings JR, Steinhauer SR, Studenski S, Greenamyre JT . Autonomic insufficiency in pupillary and cardiovascular systems in Parkinson's disease. Parkinsonism Relat Disord 2011; 17: 119–122.
Fotiou F, Fountoulakins KN, Tsolaki M, Goulas A, Palikaras A . Changes in pupil reaction to light in Alzheimer’s disease patients: a preliminary report. Int J Psychophysiol 2000; 37: 111–120.
Taylor WR, Chen JW, Meltzer H, Gennarelli TA, Kelbch C, Knowlton S, Richardson J, Lutch MJ, Farin A, Hults KN, Marshall LF . Quantitative pupillometry, a new technology: normative data and preliminary observations in patients with acute head injury. J Neurosurg 2003; 98: 205–213.
Granholm E, Steinhauer SR . Pupillometric measures of cognitive and emotional processes. Int J Psychophysiol 2004; 52: 1–6.
Koike Y, Kawabe T, Nishihara K, Iwane N, Hano T . Cilnidipine but not amlodipine suppresses sympathetic activation elicited by isometric exercise in hypertensive patients. Clin Exp Hypertens 2015; 37: 531–535.
Pagani M, Montano N, Porta A, Malliani A, Abboud FM, Birkett C, Somers VK . Relationship between spectral components of cardiovascular variabilities and direct measures of muscle sympathetic nerve activity in humans. Circulation 1997; 95: 1441–1448.
Cariga P, Catley M, Mathias CJ, Ellaway PH . Characteristics of habituation of the sympathetic skin response to repeated electrical stimuli in man. Clin Neurophysiol 2001; 112: 1875–1880.
Zafar SF, Suarez JI . Automated pupillometer for monitoring the critically ill patient: a critical appraisal. J Crit Care 2014; 29: 599–603.
Hayashi N, Someya N . Muscle metaboreflex activation by static exercise dilates pupil in human. Eur J Appl Physiol 2011; 111: 1217–1221.
Matsukawa K, Mitchell JH, Wall PT, Wilson LB . The effect of static exercise on renal sympathetic nerve activity in conscious cats. J Physiol 1991; 434: 453–467.
Neil HAW, Smith SA . A simple clinical test of pupillary autonomic function: correlation with cardiac autonomic function tests in diabetes. Neuroophthalmology 1989; 9: 237–242.
Konno S, Hirooka Y, Araki S, Koga Y, Kishi T, Sunagawa K . Azelnidipine decreases sympathetic nerve activity via antioxidant effect in the rostral ventrolateral medulla of stroke-prone spontaneously hypertensive rats. J Cardiovasc Pharmacol 2008; 52: 555–560.
Nada T, Nomura M, Koshiba K, Kawano T, Mikawa J, Ito S . Clinical study with azelnidipine in patients with essential hypertension. Antiarteriosclerotic and cardiac hypertrophy-inhibitory effects and influence on autonomic nervous activity. Arzneimittelforschung 2007; 57: 698–704.
Inomata J, Murai H, Kaneko S, Hamaoka T, Ikeda T, Kobayashi D, Usui S, Furusho H, Sugiyama Y, Takata S, Takamura M . Differential effects of azelnidipine and amlodipine on sympathetic nerve activity in patients with primary hypertension. J Hypertens 2014; 32: 1898–1904.
Ertel EA, Campbell KP, Harpold MM, Hofmann F, Mori Y, Perez-Reyes E, Schwartz A, Snutch TP, Tanabe T, Birnbaumer L, Tsien RW, Catterall WA . Nomenclature of voltage-gated calcium channels. Neuron 2000; 25: 533–535.
Benham CD, Hess P, Tsien RW . Two types of calcium channels in single smooth muscle cells from rabbit ear artery studied with whole-cell and single-channel recordings. Circ Res 1987; 61: I10–I16.
Fish RD, Sperti G, Colucci WS, Clapham DE . Phorbol ester increases the dihydropyridine-sensitive calcium conductance in a vascular smooth muscle cell line. Circ Res 1988; 62: 1049–1054.
Ono K, Iijima T . Cardiac T-type Ca(2+) channels in the heart. J Mol Cell Cardiol 2010; 48: 65–70.
Hayashi K, Homma K, Wakino S, Tokuyama H, Sugano N, Saruta T, Itoh H . T-type Ca channel blockade as a determinant of kidney protection. Keio J Med 2010; 59: 84–95.
Acknowledgements
This study was supported by a Grant-in-Aid for Scientific Research (C) (no. 26460915) from the Ministry of Education, Culture, Sports, Science, and Technology (MEXT), Japan.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Koike, Y., Kawabe, T., Nishihara, K. et al. Effects of azelnidipine and amlodipine on exercise-induced sympathoexcitation assessed by pupillometry in hypertensive patients. Hypertens Res 39, 863–867 (2016). https://doi.org/10.1038/hr.2016.94
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2016.94
Keywords
This article is cited by
-
Abnormal Systemic and Ocular Responses to the Valsalva Manoeuvre in Primary Open-Angle Glaucoma: A Case for Autonomic Failure?
Current Medical Science (2023)
-
Therapeutic Usefulness of a Novel Calcium Channel Blocker Azelnidipine in the Treatment of Hypertension: A Narrative Review
Cardiology and Therapy (2022)