Abstract
The present study investigated cardiovascular calcification, peripheral bone mineral density (BMD), and lab indices in hypertensive patients aged 55–74 years without severe kidney dysfunction. Cardiovascular calcification was investigated by ultrasound examinations at eight sites: aortic valve, left and right common carotid artery, left and right carotid artery bifurcation, left and right internal carotid artery, and abdominal aorta. The presence/absence of calcification at each site was coded as 1/0, respectively, for the calculation of a cumulative score. Peripheral bone mineral density was assessed by forearm quantitative computed tomography (pQCT) and was defined as low if the T-score was <−1. Lab work-up included plasma creatinine, calcium, phosphorus, parathyroid hormone and 25-(OH) vitamin D measurements. Ninety-one patients were studied. The range was 2–8 for the calcification score and 229–492 mg cm−3 for bone mineral density. The prevalence of low bone densitometry was 83.5%. The calcification score and bone densitometry were inversely correlated in a non-adjusted analysis (R=−0.297, P=0.004) and in multivariable regression (beta=−0.335, P=0.003). The association was significant for subcortical bone (beta=−0.302, P=0.007) but not for cortical bone or trabecular bone (P⩾0.194 in both cases). The calcification score was associated with a low prevalence of bone densitometry in the non-adjusted analysis (odds ratio=2.53, 95% CI=1.41/4.54, P=0.002) and in the multivariable logistic regression (odds ratio=2.46, 95% CI=1.25/4.81, P=0.009). Cardiovascular calcification was independently associated with peripheral bone densitometry in hypertensive patients. The data support the hypothesis that vascular calcification and low bone densitometry share some determinants in hypertensive patients.
Similar content being viewed by others
Introduction
Atherosclerosis, cardiac valve sclerosis and bone demineralization are important risk factors for the development of cardiovascular disease and fractures.1, 2, 3 Advanced atherosclerosis includes the presence of vascular calcification,4 which was associated with spinal or femoral (axial) bone demineralization in some studies.5, 6, 7, 8, 9 Low kidney function is considered a key factor in the association between vascular calcification and bone demineralization via the effects of kidney dysfunction on mineral homeostasis and parathyroid gland activity.10, 11 In addition to kidney dysfunction, vascular calcification and bone demineralization can also share other pathogenic factors. Hypertension could be one of these factors because it is associated with both vascular calcification12 and low bone mineralization in rat experimental models and in women.13, 14, 15 To further our understanding of the association between vascular calcification and bone mineralization in hypertension, the present study investigated several vascular sites together with peripheral bone mineral density in hypertensive patients without severe kidney dysfunction.
Methods
This study adhered to the principles of the Declaration of Helsinki and was approved by the local institutional ethics committee (Hospital Ethics Committee, prot. n. 589). The study required the written informed consent of the participants and was registered in the public registries of the Italian Drug Agency (Agenzia Italiana del Farmaco, ID n. 654) and the Authority for Privacy of the Italian Parliament (Garante della Privacy, n. 102400183803). All procedures were in accordance with institutional guidelines.
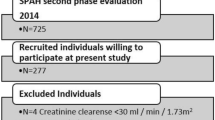
Target patients were hypertensive patients who were aged 55–74 years and who had been referred to the outpatient clinic of the AO dei Colli, Monaldi HospitalNaples, Italy Patients were defined has having hypertension if their systolic pressure was ⩾140 mm Hg and their diastolic pressure was ⩾90 mm Hg, or if they were taking regular drug treatment for hypertension. The exclusion criteria were reports of diagnoses or treatments that could be associated with altered bone densitometry, such as diseases of the bone, thyroid gland or parathyroid glands, and treatment with sex hormones, steroids, diphosphonates, teriparatide, calcium-mimetic drugs, calcium salts, vitamin D or vitamin D analogs. Selected patients underwent an early morning withdrawal of venous blood under fasting conditions for the assessment of plasma concentrations of creatinine, calcium, albumin, phosphorus, parathyroid hormone and 25-(OH) vitamin D. Kidney function was assessed by the estimated glomerular filtration rate (eGFR) and was defined as low if the eGFR was <60 ml min−1 × 1.73 m2 (chronic kidney disease G3–G5).16 Low kidney function was used as an exclusion criterion to reduce the effects of altered mineral homeostasis and parathyroid hyperactivity secondary to kidney dysfunction.17 Patients were deemed to have hypercholesterolemia if their plasma total cholesterol was ⩾240 mg per 100 ml or if they were taking regular treatment for hypercholesterolemia; and to have diabetes if their plasma glucose was ⩾126 mg per 100 ml or they were taking regular treatment for diabetes.
Ultrasound imaging was used for the assessment of vascular calcification because it is non-invasive, does not involve X-ray exposure and is highly specific.18 Patients fulfilling the selection criteria and not falling under the exclusion criteria underwent a set of ultrasound examinations that included the following: standard 2D color Doppler echocardiography for the assessment of aortic valve calcification, high-resolution B-mode ultrasonography of the left and right carotid artery for the assessment of carotid calcification, and ultrasonography of the abdominal aorta for the assessment of aortic calcification. All the ultrasound examinations were performed by a single certified examiner (CC). Standard Doppler echocardiography was performed using Vivid 7 (GE Healthcare, Milwaukee, WI, USA) with the patient in the left semi-recumbent position and in accordance with standardized protocols.19 Calcification of the aortic valve was evaluated along the long and short parasternal axes.20 Ultrasound examination of the carotid arteries was performed with the patient in the supine position combining B-mode and the color Doppler/pulsed-wave mode using an ultrasound scanner equipped with a linear array 8–12.5 MHz transducer (Aloka Prosound Alpha 10 Ultrasound System, Hitachi Aloka Medical America, Inc. Wallingford, CT, USA). The presence of calcification in the common carotid artery, carotid bifurcation, and internal carotid arteries was defined by the evidence of type IV or type V plaques.21 Ultrasonography of the abdominal aorta and iliac bifurcation was performed with the patient in the supine position using both a cardiac 3 MHz transducer and a Convex Probe (Vivid 7, GE Healthcare, Milwaukee, WI, USA), and the abdominal aorta was scanned from the origin of the renal arteries down to the iliac carrefour.22 Patients were excluded from the study if they had poor echographic windows at one or more of the sites listed above. Two independent blind observers confirmed the readings (FN and CC). Overall, the presence or absence of calcification was determined for the following eight sites: aortic valve, left common carotid artery, left external carotid artery, left internal carotid artery, right common carotid artery, right external carotid artery, right internal carotid artery and abdominal aorta.
Patients with a complete set of ultrasound examinations were included in the study cohort and underwent forearm peripheral quantitative computed tomography (pQCT) for the assessment of peripheral BMD QCT was selected for bone densitometry analysis because it is associated with the lowest X-ray exposure in radiologic imaging for osteoporosis (<0.01 mSv) while allowing for the detailed definition of bone architecture with separate analyses for cortical, subcortical, and trabecular bone.23, 24, 25 The forearm site was preferred to the leg site to exclude the confounding effects of leg BMD variability resulting from interindividual differences in habitual walking/standing time.26, 27 A single trained examiner performed all the pQCT exams (GB). The examiner was blind to the results of the ultrasound examinations. pQCT was performed in the non-dominant forearm using an XCT 2000 (Stratec Medizintechnik, Pforzheim, Germany) with software version 6.2 and default parameter settings.27, 28, 29, 30 Briefly, in accordance with standard procedures, scout views were generated in the frontal plane to identify the radiocarpal clefts to position the reference line. The radial length was measured from the distal end of the styloid to the tip of the olecranon. Sectional images were then obtained at 4 and 66% of the radial length (at the distal epiphysis and diaphysis, respectively). Total, subcortical and trabecular BMD were measured at the 4% site, while cortical BMD was measured at the 66% site.
Serum creatinine was measured by and IDMS-traceable colorimetric kinetic assay and used for calculation of eGFR by the Chronic Kidney Disease—Epidemiologic collaborative group.31, 32 Plasma levels of creatinine, calcium, albumin, phosphorus, parathyroid hormone and 25(OH) vitamin D were measured by automated biochemistry with the use of commercially available kits. To reduce the confounding of low plasma calcium due to low plasma albumin, plasma calcium was expressed with normalization to 40 g l−1 plasma albumin.
Calculations and statistics
The results of the ultrasound examination at each arterial site were coded as 1 (one) if calcification was detected or as 0 (zero) if calcification was not detected. The number of sites with calcification was used as a quantitative score for the assessment of the extent of vascular calcification. The score could range from 0 to 8, corresponding to a range from no calcification in any of the eight sites (0) to evidence of calcification in all eight sites.8 Total BMD was expressed either as absolute BMD (numerical variable, mg cm−3) or as the presence or absence of low BMD (categorical variable: presence=1 and absence=0). BMD was defined as low when the T-score was ⩽1 (total BMD <375 mg cm−3 in men and <325 mg cm−3 in women regardless of the patient’s age). Cortical, subcortical and trabecular BMD were expressed as absolute BMD only (mg cm−3). Correlation, χ2, ANOVA, linear regression and logistic regression were used for statistical analyses. ANOVA with adjustments for covariates and multivariable regression was used to verify whether the association between cardiovascular calcification and BMD was statistically independent from the other variables in the analyses. P<0.05 was considered statistically significant.
Results
Descriptive statistics
Table 1 reports the descriptive data for the study cohort. All patients were Caucasian, and as per the inclusion criteria, they were all hypertensive with an eGFR ⩾60 ml min−1 × 1.73 m2. With regard to vascular calcification, the carotid bifurcation was the most prevalent site of calcification, whereas the common carotid artery was the least prevalent. The cumulative score of vascular calcification ranged from 2 to 8, indicating that all patients had at least two arterial sites with evidence of calcification and that some patients had evidence of calcification at all eight arterial sites. With regard to bone densitometry, most of the patients had a low value of total BMD, and the mean BMD was progressively lower from the cortical to the subcortical bone as well as to the trabecular bone. In terms of antihypertensive drug treatment, inhibitors/blockers of the renin–angiotensin system were the most used drugs, whereas thiazide diuretics were the least used drugs.
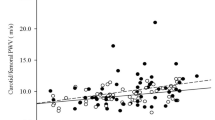
Vascular calcification and absolute BMD
The score for vascular calcification was inversely correlated with absolute values of total BMD; in other words, a greater number of sites with vascular calcification was associated with a lower total BMD (Figure 1). The correlation coefficient was significant or borderline significant in stratified analyses for men (n=63, R=−0.382, P=0.002) and for women (n=28, R=−0.414, P=0.028). Separate analyses for cortical, subcortical, and trabecular bone indicated that an association was present only for subcortical BMD (Figure 2). The correlation coefficient between the score of vascular calcification and subcortical BMD was significant in stratified analyses for men (n=63, R=−0.359, P=0.004) and for women (n=28, R=−0.383, P=0.044). In the multivariable linear regression analysis controlling for sex, age and other variables, the standardized regression coefficient between the score for vascular calcification and total BMD was stable and significant for total BMD and for subcortical BMD (Table 2). For the other variables, male gender was independently associated with higher BMD, whereas plasma phosphorus concentrations were directly associated with only cortical and subcortical BMD (Table 3).
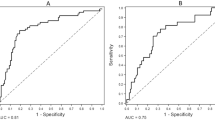
Vascular calcification and low BMD
A higher calcification score was significantly associated with the progressively higher prevalence of low BMD (Figure 3). The odds ratio of low BMD was 2.53 for a calcification score one point higher in the non-adjusted logistic regression (95% CI=1.41/4.54, P=0.002) and was similarly increased when other variables were controlled for. None of the other variables was independently associated with the prevalence of low total BMD. In the analyses of single cardiovascular sites, the odds ratio of low total BMD was significant for calcification at the internal carotid arteries and abdominal aorta (odds ratio ⩾4.07, P⩽0.047) but was weak and non-significant for calcification at other sites (odds ratio ⩽1.37, P⩾0.702).
Hypertensive patients with low total BMD had higher calcification scores compared with hypertensive patients without low BMD by non-adjusted ANOVA (with low BMD and without low BMD: n=76 and 15, mean score=4.20 and 2.67, respectively; P<0.001). With regard to the other variables, differences between hypertensive patients with or without low BMD were significant for plasma parathyroid hormone concentrations (45.2 and 38.1 pg ml−1, respectively; P=0.027) but were not significant for sex distribution, prevalence of hypercholesterolemia, smoking, history of cardiovascular disease, diabetes and eGFR as well as normalized plasma levels of total calcium, plasma phosphorus and plasma 25-(OH) vitamin D (P⩾0.160). Hypertensive patients with low BMD had higher calcification scores compared with hypertensive patients without low BMD when the ANOVA adjusted for sex, age and other variables (mean score=4.11 and 3.09, P=0.018).
Discussion
The current study reported an independent cross-sectional association between a quantitative index of the extent of cardiovascular calcification and peripheral densitometry of the subcortical bone of hypertensive patients. The novelty of the results is based on three points: the target cohort of hypertensive patients without low kidney function, the use of an ultrasound-based multisite score for the assessment of the extent of cardiovascular calcification and the use of forearm pQCT for BMD evaluation.
In general, the present results were consistent with all previous studies reporting an association between cardiovascular calcification and low BMD.5, 6, 7 However, a true comparison between the present results and previous results was difficult because the present study was the first to use multisite echography for the assessment of the extent of cardiovascular calcification and of forearm BMD in high-risk hypertensive patients without severe kidney dysfunction. A large set of the recent data from the Framingham study indicated that calcification of the abdominal aorta is more strongly associated with low BMD when compared with other arteries and that this association does not involve the cortical bone.7 The present results were consistent with that observation and extended the evidence of the association between low BMD and cardiovascular calcification to other large arteries and peripheral bone.
Theoretically, several non-alternative mechanisms could explain an independent cross-sectional association between cardiovascular calcification and low BMD. First, the two disorders could have common determinants. Hypertension and smoking are two reasonable candidates in this regard because both induce atherosclerosis and are associated with low BMD.12, 13, 14, 15, 33, 34 Thus, the association of cardiovascular calcification and low BMD would reflect the parallel development of vascular damage and bone demineralization resulting from the duration and/or severity of exposure to hypertension and smoking. A similar mechanism could be hypothesized for high salt intake because it favors not only hypertension, but also osteoporosis, likely increasing urinary calcium loss.35, 36, 37 A second mechanism could be a detrimental effect on bone metabolism and bone formation because of inadequate circulation resulting from vascular diseases.11 In this view, low BMD could be another complication that is secondary to vascular disease. A third mechanism could involve the renin–angiotensin system, which is expressed within the vascular wall and in the local milieu of bone and, thus, could promote not only vascular damage, but also low BMD.38 The last mechanism, or the last set of mechanisms, could occur at the molecular level, given that the downregulation of osteoprotegerin and/or other proteins can cause both vascular calcification and low BMD.39, 40, 41 However, other mechanisms cannot be excluded at this time.
The available data for the different cardiovascular sites and for different bone sections indicated that there was a strong association between the calcification of either the carotid arteries or the aorta and the low BMD of the subcortical bone, whereas such an association was weak or absent between the other cardiovascular sites and the cortical or trabecular bone. Although the reasons underlying the patchy distribution of the associations are unknown, the data from the Framingham study and from the present study both indicated the large arteries and subcortical bone to be sites of crosstalk between vascular damage and bone demineralization.7 The selection of patients without low kidney function proved that the association between cardiovascular calcification and low BMD is independent of and can occur largely before perturbations in mineral homeostasis and parathyroid gland activity resulting from severely reduced kidney function. The results of multivariable analyses indicated that the association was independent of not only sex, age and kidney dysfunction, but also other cardiovascular risk factors. Finally, the mild increase in plasma parathyroid hormone levels observed in hypertensive patients with low BMD suggested that parathyroid overactivity has a role in the association between BMD and cardiovascular calcification, although this possibility was not supported by the results of the multivariable regression analyses.
The main limitations of the present study were the number of patients, the lack of data for other ethnic groups, the lack of accurate imaging for the assessment of cardiovascular calcification and BMD, and the lack of data for non-hypertensive persons. The limited number of patients and the lack of data for various ethnic groups indicate the need for further studies. The use of state-of-the-art imaging methods for the assessment of cardiovascular calcification or bone densitometry would have improved the quality of the study, but it would have also raised ethical concerns and limited the practical implications because accurate imaging techniques require higher radiation exposure and higher costs. Finally, the lack of data for non-hypertensive persons precluded the ability to prove that the association between cardiovascular calcification and BMD depended on the presence of hypertension.
The practical implications of the results are that, an assessment of BMD may be advisable in hypertensive patients with or at risk of cardiovascular calcification because low BMD was prevalent in these patients and was associated with vascular calcification, particularly with signs of more severe vascular damage. By contrast, the same results suggested that vascular imaging is advisable in hypertensive patients with low BMD because of the possible co-existence of widespread vascular calcification. In this view, the use of pQCT and multisite echo may be preferable because of the absence of significant radiation exposure and because of the limited costs. Moreover, in accordance with the Japanese Society of Hypertension Guidelines for the Management of Hypertension42 and with the protective effects of thiazide diuretics on fracture risk in older hypertensive patients,43 the results of the present study support the idea that antihypertensive drugs that antagonize bone demineralization may be preferable in hypertensive patients with low BMD. Given the cross-sectional design of the analysis, it was impossible to assess whether the lack of association between treatment with thiazide diuretics and BMD reflected the pretreatment of BMD rather than the effects of the treatment on BMD. Finally, the association of low BMD with vascular calcification and the possible association between vascular calcification and arterial stiffness suggest that low BMD is also associated with arterial stiffness and related disorders.44, 45, 46, 47
In summary, the study showed that a greater number of sites with cardiovascular calcification were independently associated with lower forearm BMD in hypertensive patients without low kidney function. The association was stronger between the calcification of the carotid artery or of the abdominal aorta and subcortical bone. The results support the hypothesis that vascular calcification and low BMD share some determinants. Moreover, the results suggest the need not only for BMD assessments in hypertensive patients with vascular calcification, but also to evaluate hypertensive patients with low BMD for vascular calcification.
References
Fifth Joint Task Force of the European Society of Cardiology, European Association of Echocardiography, European Association of Percutaneous Cardiovascular Interventions, European Heart Rhythm Association, Heart Failure Association, European Association for Cardiovascular Prevention and Rehabilitation, European Atherosclerosis Society, International Society of Behavioural Medicine, European Stroke Organisation, European Society of Hypertension, European Association for the Study of Diabetes, European Society of General Practice/Family Medicine, International Diabetes Federation Europe, European Heart Network.. European Guidelines on cardiovascular disease prevention in clinical practice (version 2012): the Fifth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of nine societies and by invited experts). Eur J Prev Cardiol 2012; 19: 585–667.
James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, Lackland DT, LeFevre ML, MacKenzie TD, Ogedegbe O, Smith SC Jr, Svetkey LP, Taler SJ, Townsend RR, Wright JT Jr, Narva AS, Ortiz E . Evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 2014; 311: 507–520.
Kanis JA, McCloskey EV, Johansson H, Strom O, Borgstrom F, Oden A The National Osteoporosis Guideline Group. Case finding for the management of osteoporosis with FRA. Assessment and intervention thresholds for the UK. Osteoporos Int 2008; 19: 1395–1408.
Ruiz JL, Hutcheson JD, Aikawa E . Cardiovascular calcification: current controversies and novel concepts. Cardiovasc Pathol 2015; 24: 207–212.
Chue CD, Wall NA, Crabtree NJ, Zehnder D, Moody WE, Edwards NC, Steeds RP, Townend JN, Ferro CJ . Aortic calcification and femoral bone density are independently associated with left ventricular mass in patients with chronic kidney disease. PLoS ONE 2012; 7: e39241.
Zulc P, Samelson EJ, Sornay-Rendu E, Chapurlat R, Kiel DP . Severity of aortic calcification is positively associated with vertebral fracture in older men—a densitometry study in the STRAMBO cohort. Osteoporos Int 2013; 24: 1177–1184.
Chan JJ, Cupples LA, Kiel DP, O'Donnell CJ, Hoffmann U, Samelson EJ . QCT volumetric bone mineral density and vascular and valvular calcification: the Framingham Study. J Bone Miner Res 2015; 30: 1767–1774.
Shavit L, Girfoglio D, Vijay V, Goldsmith D, Ferraro PM, Moochhala SH, Unwin R . Vascular calcification and bone mineral density in recurrent kidney stone formers. Clin J Am Soc Nephrol 2015; 10: 278–285.
Nasser EJ, Iglésias ER, Ferreira JA, Fernandes CE, Pompei LM . Association of breast vascular calcifications with low bone mass in postmenopausal women. Climacteric 2014; 17: 486–491.
Tomlinson J, Cunningham J . Soft bones and hard arteries-can we reverse the trend in CKD? J Ren Care 2009; 35 (Suppl 1): 28–33.
Thompson B, Towler DA . Arterial calcification and bone physiology: role of the bone-vascular axis. Nat Rev Endocrinol 2012; 8: 529–543.
Kalra SS, Shanahan CM . Vascular calcification and hypertension: cause and effect. Ann Med 2012; 44 (Suppl 1): S85–S92.
Lucas PA, Brown RC, Drüeke T, Lacour B, Metz JA, McCarron DA . Abnormal vitamin D metabolism, intestinal calcium transport, and bone calcium status in the spontaneously hypertensive rat compared with its genetic control. J Clin Invest 1986; 78: 221–227.
Cirillo M, Galletti F, Strazzullo P, Torielli L, Melloni MC . On the pathogenetic mechanism of hypercalciuria in genetically hypertensive rats of the Milan strain. Am J Hypertens 1989; 2: 741–746.
Yang S, Nguyen ND, Center JR, Eisman JA, Nguyen TV . Association between hypertension and fragility fracture: a longitudinal study. Osteoporos Int 2014; 25: 97–103.
Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int 2013; 3 (Suppl): 1–150.
Kidney Disease: Improving Global Outcomes (KDIGO) CKD-MBD Work Group. KDIGO clinical practice guideline for the diagnosis, evaluation, prevention, and treatment of Chronic Kidney Disease-Mineral and Bone Disorder (CKD-MBD). Kidney Int 2009; 76: S1–S130.
Karohl C, D'Marco Gascón L, Raggi P . Noninvasive imaging for assessment of calcification in chronic kidney disease. Nat Rev Nephrol 2011; 7: 567–577.
Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, Flachskampf FA, Foster E, Goldstein SA, Kuznetsova T, Lancellotti P, Muraru D, Picard MH, Rietzschel ER, Rudski L, Spencer KT, Tsang W, Voigt JU . Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging 2015; 16: 233–270.
Nightingale AK, Horowitz JD . Aortic sclerosis: not an innocent murmur but a marker of increased cardiovascular risk. Heart 2005; 91: 1389–1393.
Gray-Weale A, Graham J, Burnett J, Byrne K, Lusby R . Carotid artery atheroma: comparison of preoperative B-mode ultrasound appearance with carotid endarterectomy specimen pathology. J Cardiovasc Surg 1988; 29: 676–681.
Mohler ER, Gornik HL, Gerhard-Herman M, Misra S, Olin JW, Zierler RE . 2012 Appropriate use criteria for peripheral vascular ultrasound and physiological testing Part I: arterial ultrasound and physiological testing: a report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, American College of Radiology, American Institute of Ultrasound in Medicine, American Society of Echocardiography, American Society of Nephrology, Intersocietal Commission for the Accreditation of Vascular Laboratories, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, Society for Interventional Radiology, Society for Vascular Medicine, and Society for Vascular Surgery. J Am Coll Cardiol 2012; 60: 242–276.
Engelke K, Adams JE, Armbrecht G, Augat P, Bogado CE, Bouxsein ML, Felsenberg D, Ito M, Prevrhal S, Hans DB, Lewiecki ME . Clinical Use of quantitative computed tomography and peripheral quantitative computed tomography in the management of osteoporosis in adults: the 2007 ISCD official positions. J Clin Densitom 2008; 11: 123–162.
Damilakis J, Adams JE, Guglielmi G, Link TM . Radiation exposure in X-ray-based imaging techniques used in osteoporosis. Eur Radiol 2010; 20: 2707–2714.
Adams JE . Quantitative computed tomography. Eur J Radiol 2009; 71: 415–424.
Boyer KA, Kiratli BJ, Andriacchi TP, Beaupre GS . Maintaining femoral bone density in adults: how many steps per day are enough? Osteoporos Int 2011; 22: 2981–2988.
Rittweger J, Simunic B, Bilancio G, De Santo NG, Cirillo M, Biolo G, Pisot R, Eiken O, Mekjavic IB, Narici M . Bone loss in the lower leg during 35 days of bed rest is predominantly from the cortical compartment. Bone 2009; 44: 612–618.
Conway JL, Yurkowski E, Glazier J, Gentles Q, Walter A, Bowering G, Curtis S, Schellenberg D, Halperin R, Lapointe V, Beckham W, Olivotto IA, Olson RA . Comparison of patient-reported outcomes with single versus multiple fraction palliative radiotherapy for bone metastasis in a population-based cohort. Radiother Oncol 2016; 119: 202–207.
Edwards MH, Gregson CL, Patel HP, Jameson KA, Harvey NC, Aihie Sayer A, Dennison EM, Cooper C . Muscle size, strength, and physical performance and their associations with bone structure in the Hertfordshire Cohort Study. J Bone Miner Metab 2013; 28: 2295–2304.
Belavý DL, Armbrecht G, Blenk T, Bock O, Börst H, Kocakaya E, Luhn F, Rantalainen T, Rawer R, Tomasius F, Willnecker J, Felsenberg D . Greater association of peak neuromuscular performance with cortical bone geometry, bone mass and bone strength than bone density: a study in 417 older women. Bone 2016; 83: 119–126.
Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF, Feldman HI, Kusek JW, Eggers P, Van Lente F, Greene T, Coresh J CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration). A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009; 150: 604–612.
Cirillo M, Lombardi C, Luciano MG, Bilancio G, Anastasio P, De Santo NG . Estimation of GFR: a comparison of new and established equations. Am J Kidney Dis 2010; 56: 802–804.
Herrington W, Lacey B, Sherliker P, Armitage J, Lewington S . Epidemiology of atherosclerosis and the potential to reduce the global burden of atherothrombotic disease. Circ Res 2016; 118: 535–546.
Cusano NE . Skeletal effects of smoking. Curr Osteopor Rep 2015; 13: 302–309.
He FJ, Li J, MacGregor GA . Effect of longer term modest salt reduction on blood pressure: Cochrane systematic review and meta-analysis of randomised trials. BMJ 2013; 346: f1325.
Heaney RP . Role of dietary sodium in osteoporosis. J Am Coll Nutr 2006; 25 (3 Suppl): 271S–276S.
Cirillo M, Ciacci C, Laurenzi M, Mellone M, Mazzacca G, De Santo NG . Salt intake, urinary sodium, and hypercalciuria. Miner Electrolyte Metab 1997; 23: 265–268.
Tamargo J, Caballero R, Delpón E . The Renin–angiotensin system and bone. Clinic Rev Bone Miner Metab 2015; 13: 125.
Bucay N, Sarosi I, Dunstan CR, Morony S, Tarpley J, Capparelli C, Scully S, Lin Tan H, Xu W, Lacey DL, Boyle WJ, Simonet WS . Osteoprotegerin-deficient mice develop early onset osteoporosis and arterial calcification. Genes Dev 1998; 12: 1260–1268.
Luo G, Ducy P, McKee M, Pinero GJ, Loyer E, Behringer RR, Karsenty G . Spontaneous calcification of arteries and cartilage in mice lacking matrix GLA protein. Nature 1997; 386: 78–81.
van Campenhout A, Golledge J . Osteoprotegerin, vascular calcification and atherosclerosis. Atherosclerosis 2009; 204: 321–329.
Shimamoto K, Ando K, Fujita T, Hasebe N, Higaki J, Horiuchi M, Imai Y, Imaizumi T, Ishimitsu T, Ito M, Ito S, Itoh H, Iwao H, Kai H, Kario K, Kashihara N, Kawano Y, Kim-Mitsuyama S, Kimura G, Kohara K, Komuro I, Kumagai H, Matsuura H, Miura K, Morishita R, Naruse M, Node K, Ohya Y, Rakugi H, Saito I, Saitoh S, Shimada K, Shimosawa T, Suzuki H, Tamura K, Tanahashi N, Tsuchihashi T, Uchiyama M, Ueda S, Umemura S on behalf of The Japanese Society of Hypertension Committee for Guidelines for the Management of Hypertension. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2014). Hypertens Res 2014; 37: 253–392.
Puttnam R, Davis BR, Pressel SL, Whelton PK, Cushman WC, Louis GT, Margolis KL, Oparil S, Williamson J, Ghosh A, Einhorn PT, Barzilay JI Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT) Collaborative Research Group. Association of 3 different antihypertensive medications with hip and pelvic fracture risk in older adults: secondary analysis of a randomized clinical trial. JAMA Intern Med 2017; 177: 67–76.
László A, Reusz G, Nemcsik J . Ambulatory arterial stiffness in chronic kidney disease: a methodological review. Hypertens Res 2016;39: 1928.
Kollias A, Rarra V, Karpettas N, Roussias L, O'Brien E, Stergiou GS . Treatment-induced changes in ambulatory arterial stiffness index: one-year prospective study and meta-analysis of evidence. Hypertens Res 2015;38: 62731.
Peng F, Pan H, Wang B, Lin J, Niu W . The impact of angiotensin receptor blockers on arterial stiffness: a meta-analysis. Hypertens Res 2015;38: 61320.
Zagura M, Kals J, Kilk K, Serg M, Kampus P, Eha J, Soomets U, Zilmer M . Metabolomic signature of arterial stiffness in male patients with peripheral arterial disease. Hypertens Res 2015;38: 8406.
Acknowledgements
This work was supported by grant from the Agenzia Spaziale Italiana (ASI, contract No 2013-093-R.0).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Cirillo, C., Bilancio, G., Natale, F. et al. Cardiovascular calcification and subcortical bone demineralization in hypertension. Hypertens Res 40, 825–830 (2017). https://doi.org/10.1038/hr.2017.44
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2017.44
Keywords
This article is cited by
-
Diabetes and Abdominal Aortic Calcification—a Systematic Review
Current Osteoporosis Reports (2018)