Abstract
In patients with insufficient blood pressure (BP) control, despite using a combination regimen containing an angiotensin receptor blocker and a calcium channel blocker (CCB), whether a greater dose of CCB or adding a diuretic is more effective at lowering BP remains unclear. We conducted a multicenter randomized clinical trial to compare the efficacy of switching from the daily administration of a single-pill fixed-dose combination of irbesartan (100 mg) and amlodipine (5 mg) to irbesartan (100 mg) with an increased dose of amlodipine (10 mg) (HD group, n=62) or irbesartan (100 mg) and amlodipine (5 mg) with 1 mg of indapamide (D group, n=63) in patients with poorly controlled hypertension. BP measured at home was monitored by a physician using a telemonitoring system. Between the HD and D groups, no significant differences were observed in morning home BP changes (mean reduction of systolic/diastolic BP, 1.7/0.9 mmHg; 95% confidence intervals, −2.4 to 5.7/−1.4 to 3.2; P=0.19/0.37), achievement rate of target BP (45.2% vs. 42.9%, P=0.80), BP variability independent of the mean (P⩾0.74), other variability indices (P⩾0.55) and time to stabilization, which was calculated using a fitted analysis (13.1 days vs. 11.4 days, P=0.99). Although a significant increase in serum uric acid was observed in the D group (P<0.0001), neither clinically relevant abnormal laboratory test results nor critical BP changes were observed throughout the trial period. Both antihypertensive drug combination strategies were effective treatment options. Further investigation is required to determine the appropriate use of both therapies based on the various pathologies associated with hypertension.
Similar content being viewed by others
Introduction
Intensive blood pressure control is important in reducing the risk of cardiovascular diseases.1, 2, 3 However, the rate of achievement of target blood pressure level in daily practice has been 30–40% or less,4, 5 and that rate is even lower based on self-measured home blood pressure.5 When blood pressure control is insufficient by monotherapy, therapy with a combination of antihypertensive drug classes is more effective compared with increasing the dose of the single drug.6, 7 In particular, the combined use of a renin–angiotensin system inhibitor (that is, angiotensin converting enzyme inhibitors or angiotensin 2 receptor blockers) and a long-acting calcium channel blocker is superior to that of β blockers and diuretics for the reduction of cardiovascular morbidly8, 9 and mortality.9 Although the above-mentioned combination therapy is recommended,10 the mean number of antihypertensive drugs was <2 even among patients allocated to tight blood pressure control groups in a previous randomized trial11 and an observational study.12
Although challenges in managing the accuracy of home blood pressure measurements13 and the reliability of self-recording systems14 remain, transferring blood pressure data from a home device to a central server has become feasible.11 A large-scale remote blood pressure monitoring system enables us to improve therapeutic efficacy in the patient population.15 However, as Rothwell et al.16 reported, there have been no reports on whether increasing the dose of the calcium channel blocker, which has dose-dependent effects, or adding diuretics to the conventional combination therapy is the more effective option for lowering home and clinic blood pressure or on which one has a larger impact on blood pressure variability in patients with insufficient blood pressure control. We therefore aimed to compare the effects of a dose increase of amlodipine with that of adding indapamide to treat patients with insufficient home and clinic blood pressure control under a fixed low-to-moderate dose combination regimen of irbesartan and amlodipine.
Methods
Study design
This study is a multicenter, randomized, open-label study on blood pressure reduction in patients aged 20–79 years with essential hypertension. The study was approved by the Institutional Review Board at each institution and complies with the Declaration of Helsinki for the investigation of human subjects;17 this study is also registered with the UMIN Clinical Trial Registry (http://www.umin.ac.jp/ctr) as number UMIN000011328. All study participants gave their written informed consent.
Eligible patients were those who regularly visited an outpatient clinic and were treated with a combination of 100 mg per day irbesartan and 5 mg per day amlodipine but did not achieve the target blood pressure level in consideration of the Japanese Society of Hypertension Guidelines 2009;18 as follows: (1) clinic blood pressure <140/<90 mmHg and home blood pressure <135/<85 mmHg without diabetes or chronic kidney disease or (2) clinic and home blood pressure <130/<80 mmHg with diabetes or chronic kidney disease. We compared the efficacy of switching from their initial combination regimen to that with the same dose of irbesartan but a higher dose of amlodipine (10 mg per day) or to that including 1 mg of indapamide with the initial combination regimen. The combinations of 100 mg of irbesartan and 5 mg of amlodipine as well as 100 mg of irbesartan and 10 mg of amlodipine were supplied as a combination tablet (Aimix LD and Aimix HD, respectively) that is marketed in Japan.
The exclusion criteria were as follows: (1) patients with secondary hypertension or malignant hypertension or those who had a myocardial infarction, percutaneous coronary angioplasty or coronary artery bypass within 6 months prior to obtaining informed consent; (2) patients with contraindications for treatment with increased doses of amlodipine or administration of indapamide; (3) patients receiving angiotensin converting enzyme inhibitors, direct renin inhibitors and/or diuretics; (4) patients who would not visit the clinic regularly or were suspected to have insufficient drug adherence; (5) shift workers who had daytime and nighttime shifts; and (6) patients on hemodialysis.
Study procedures
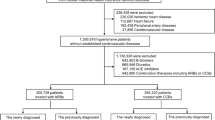
After informed consent was given, physicians sent a registration form indicating study participation to the research secretariat at the Nihon University School of Medicine via fax. As shown in Figure 1, the administration of 100 mg per day irbesartan and 5 mg per day amlodipine (Aimix LD) started at visit 0, and patients visited the study center of the outpatient clinic every month. Clinic blood pressure was measured at each visit, whereas home blood pressure was measured over 2 months during the study period. No other antihypertensive drug was prescribed during this period. If either the home or clinic blood pressure of the study participants did not reach the aforementioned target blood pressure level at visit 2, patients were randomized to two treatment groups that were treated with either the Aimix HD (HD group) or the combination of Aimix LD and 1 mg of indapamide (D group) based on a minimization algorithm that considered sex, age and the systolic and diastolic clinic blood pressure levels. Randomization was stratified by age, sex and clinic blood pressure at visit 2. After the randomization, changes in home and clinic blood pressure were observed for 3 months at visits 3–5. No other concomitant drugs were changed and/or added during the study period. The primary end point was the change in home and clinic blood pressure and the rate of achievement of target blood pressure. The secondary end points were blood pressure and heart rate variability and the time required to stabilize the antihypertensive effects (stabilizing time).
Trial profile. Patients visited each trial site every month (visits 0–5). At visit 2, patients allocated to the HD group were prescribed the combination therapy of 100 mg per day irbesartan and 10 mg of amlodipine, and those allocated to the D group were prescribed the combination therapy of 100 mg per day irbesartan, 5 mg per day amlodipine and 1 mg of indapamide.
Blood pressure measurement and telemonitoring
At each visit, after the patients had rested in the sitting position for 2 min, physicians obtained two consecutive measurements of blood pressure and heart rate by any device at the clinic that was validated and approved by the Ministry of Health, Labour and Welfare of Japan. The mean of the two office measurements was considered as the clinic measurement.
Patients were instructed to measure home blood pressure after 2 min of rest in the sitting position every morning during the study duration. Patients had to obtain these measurements within 1 h of awakening before breakfast and before taking their antihypertensive medication. They were asked to measure their blood pressure twice per occasion, and the mean of these two measurements taken was considered as the home blood pressure. These measurement conditions were based on the Japanese Society of Hypertension Guidelines 2014.10 A validated Omron HEM-7251G (Omron Colin, Tokyo, Japan)19 device equipped with communication capabilities via a mobile phone line was lent to the study patients for use. Blood pressure, heart rate, time of measurement and room temperature were shown on the terminal at the physicians’ office, and the study was managed by the internet-based telemonitoring system (MedicalLINK) using serial numbers embedded in the HEM-7251G and the random numbers that were automatically assigned to each patient at registration to prevent sending personal information externally.
Laboratory data
Diabetes was defined as fasting plasma glucose concentrations ⩾7.0 mmol l−1 (⩾126 mg dl−1), HbA1c ⩾6.5% or current treatment with anti-diabetic agents. Dyslipidemia was defined as low-density lipoprotein cholesterol of 3.62 mmol l−1 (140 mg dl−1) or higher, triglycerides of 1.69 mmol l−1 (150 mg dl−1) or higher, high-density lipoprotein cholesterol less than 1.03 mmol l−1 (40 mg dl−1) or current treatment with lipid-lowering agents. Smoking was defined as current smoking or smoking cessation within 1 year prior to the start of the study. The estimated glomerular filtration rate was calculated with the Japanese Equation as follows:20 estimated glomerular filtration rate (ml min−1 per 1.73 m2)=194 × serum creatinine−1.094 × age−0.287 (× 0.739 if women), and chronic kidney disease was defined as estimated glomerular filtration rate <60 ml min−1 per 1.73 m2 or proteinuria diagnosed by a protein reading on a dip-stick test of 1+ or more. Angiographically confirmed coronary artery disease was defined as a history of documented myocardial infarction, prior coronary revascularization intervention (coronary artery bypass graft surgery or percutaneous coronary intervention) or the presence of ⩾50% stenosis in one or more coronary arteries during cardiac catheterization. Diagnoses of chronic heart failure were made using the Framingham criteria.21
Statistical analysis
Statistical analyses were performed using the SAS software version 9.4 (SAS Institute, Cary, NC, USA). We expressed data as the mean±s.d. for continuous variables and as percentages for categorical variables, while continuous data that did not follow a normal distribution were expressed as the median (interquartile range). According to the type of variables, Student’s t-test, Mann–Whitney’s U test, and the χ2-test were appropriately used to compare variables between the groups, and paired t-test and Wilcoxon’s signed-rank test were appropriately used to compare variables within the same group.
Data regarding home blood pressure values for the 5 days prior to randomization at visit 2 and for the final 5 days prior to visit 5 were used for the calculation of level and variability at baseline and during follow-up, respectively. We computed the home blood pressure variability from the s.d., coefficient of variation and maximum minus minimum blood pressure.22, 23, 24 The within-patient blood pressure variability was further represented by variability independent of the mean index, which is s.d. divided by the mean of the power x.16, 22, 24 Power x is modeled by the following equation: s.d.=a × meanx and was derived by nonlinear regression analysis using the PROC NLIN procedure of the SAS package. We also used average real variability, which was calculated as the average of the absolute differences between blood pressure measurements from consecutive days.24, 25, 26 The blood-pressure-lowering effect after drug initiation was evaluated as the time required to stabilize blood pressure level after randomization at visit 2 using exponential decay data and the least squares fitting method.7, 27, 28 The exponential function is as follows: Y=A × e−kT+C, where Y and T are home blood pressure level and days since randomization, respectively; A denotes the extent of the blood-pressure-lowering effect; C reflects the final blood pressure level; and k reflects the time constant for blood pressure decay (day−1). We fitted an intercept of a curve (A+C) to the baseline home blood pressure level as the average of the 5 days prior to randomization. We defined stabilization time as the computed T when the blood pressure reduction reached 95% of the maximum degree, which was calculated as 3.0 k−1 and was derived by the PROC NLMIXED procedure of the SAS package. We used home blood pressure data until 28 days after the randomization, while outlying blood pressure values defined as±2 s.d. of each day were excluded from the analysis.
Results
The study started on 4 June 2013, and 200 patients were recruited by 16 January 2016, from nine trial sites (Figure 1). Of those, 23 achieved the target blood pressure level under the initial drug treatment before randomization, and eight patients were discontinued from the study. The remaining 169 patients met the eligibility criteria and were randomly allocated to either the HD treatment group (n=83) or the D (n=86) treatment group. Of the 83 patients in the HD group and the 86 in the D group, 21 (15 had incomplete blood pressure measurements, 5 withdrew from the trial and 1 moved) and 23 (15 had incomplete measurements, 5 withdrew and 2 moved) patients, respectively, discontinued the study treatment during the trial. Therefore, 125 patients (62 in the HD group and 63 in the D group) completed the study and were included in the analysis. Clinical characteristics among patients in the two groups did not differ (Table 1; P⩾0.25). Neither critical blood pressure changes nor clinically relevant abnormal laboratory test results were observed during the trial period.
Changes in blood pressure and achievement of target level
Compared with the baseline run-in period, both systolic and diastolic blood pressure significantly decreased in the HD and D groups using both home and clinic measurements (P⩽0.0029). Heart rate did not change in both groups during the trial (P⩾0.13). The blood-pressure-lowering effect from baseline to the end of the follow-up was statistically the same between the HD and D groups (P⩾0.19); reductions of home systolic and diastolic blood pressure in the HD group were 1.7 mmHg (95% confidence intervals (CI), −2.4 to 5.7) and 0.9 mmHg (CI, −1.4 to 3.2) less than those in the D group, respectively, whereas reductions of clinic systolic and diastolic pressure in the HD group were 1.6 mmHg (CI, −4.3 to 7.5) and 2.7 mmHg (CI, −1.4 to 6.7) greater than those in the D group, respectively. The achievement rate of the target blood pressure level was also statistically the same based on home (HD group vs. D group: 45.2% vs. 42.9%, P=0.80) and clinic blood pressure measurements (66.1% vs. 58.7%, P=0.39). Significant differences were not observed among blood pressure measurements taken at visits 3, 4 and 5 when compared separately (P⩾0.23).
Variability of home blood pressure and heart rate
Variability of home blood pressure and heart rate at baseline before randomization and during follow-up is shown in Tables 2 and 3, respectively. The blood pressure levels and variability indices were not significantly different between the two groups (P⩾0.064). The variability indices of systolic home blood pressure during the follow-up period were statistically the same compared with those at baseline (P⩾0.18); the same finding was also observed in the variability indices derived from diastolic home blood pressure (P⩾0.15) and heart rate (P⩾0.25). Consequently, changes did not differ between the two groups regarding variability independent of the mean index (P⩾0.74) and other variability indices (P⩾0.55).
Antihypertensive drug effect and stabilization time
In both groups, the blood-pressure-lowering effect on home systolic blood pressure after drug initiation was significantly fitted to the exponential function decay model (P⩽0.0007). The estimated maximum effect, stabilizing time and blood pressure level were 6.9 (CI, 5.8–8.0) mmHg, 13.1 (CI, 8.4–30.0) days and 133.9 (CI, 131.4–136.3) mmHg, respectively, in the HD group and 8.4 (CI, 7.3–9.6) mmHg, 11.4 (CI, 8.5–17.3) days and 131.0 (CI, 127.6–134.5) mmHg, respectively, in the D group. As shown in Figure 2, the difference in the maximum home systolic blood-pressure-lowering effect was marginal (P=0.052), while stabilizing time and final blood pressure levels were statistically the same (P⩾0.18).
Daily levels of home systolic blood pressure after randomization and exponential decay curves in the HD and D groups. Patients allocated to the HD group (circle and dotted line) took the combination regimen of 100 mg per day irbesartan and 10 mg of amlodipine, and those allocated to the D group (square and solid line) took the combination regimen of 100 mg per day irbesartan, 5 mg per day amlodipine and 1 mg of indapamide. The dotted line and solid line denote changes in systolic blood pressure in the HD and D groups, respectively. The circle and square symbols denote blood pressure averages of each day after randomization in the HD and D groups, respectively.
Changes in blood chemistry data
As shown in Table 4, there was no significant change in serum uric acid level from baseline until 3 months after treatment in the HD group (−0.08±0.81 mg dl−1, P=0.44), but it was significantly increased in the D group (0.80±0.90 mg dl−1, P<0.0001). Significant decreases in serum sodium, potassium and chloride levels were observed in the D group (P⩽0.031) but not in the HD group (P⩾0.28). Fasting blood glucose and serum lipid profiles did not change during the trial period in both treatment groups (P⩾0.14).
Discussion
In patients with essential hypertension and insufficient blood pressure control despite treatment with a combination of 100 mg per day irbesartan and 5 mg per day amlodipine, both dose increments of amlodipine at 10 mg per day or adding 1 mg of indapamide to their existing regimen resulted in significant blood pressure reduction; however, there were no statistically significant differences in clinic or morning home blood pressure reduction between the two groups. Furthermore, no significant differences in the secondary end points of stabilizing time and variability of blood pressure and heart rate were observed, suggesting that both combination treatments may be similarly effective for tight blood pressure control. We used the Omron HEM-7251G equipped with a mobile phone line that enabled data transfer of morning home blood pressure and heart rate immediately after each measurement. The present study demonstrated the feasibility of such a telemonitoring system for research trials even though 15 patients in each group were not able to provide blood pressure data before the completion of the study.
In hypertensive patients, low rates of treatment and low rates of achieving target blood pressure levels have been common challenges. If the clinic blood pressure of all hypertensive patients decreases to less than 140/90 mmHg, the decrease in the long-term risk of cardiovascular diseases will make the treatments more cost-effective despite the increased cost of antihypertensive treatment.29 Moreover, the systolic blood pressure intervention trial,3, 30 which had a systolic blood pressure target level of <120 mmHg in the intensive treatment group, has reported reductions in the risk of cardiovascular diseases and death in hypertensive patients,3, 30 even among ambulatory adults aged 75 years or older.30 In addition, the recent meta-analysis demonstrated that a reduction in systolic blood pressure to 130 mmHg was effective in preventing cardiovascular diseases.31 Intensive blood pressure control would be necessary in routine medical practice for patients with hypertension. Because single antihypertensive agent therapy may decrease blood pressure by only 7–9 mmHg,6 combination therapy using multiple antihypertensive drugs is required to achieve intensive blood pressure control to prevent cardiovascular diseases.
Although numerous indicators have been used to evaluate the efficacy of antihypertensive drugs, the variability of blood pressure measurements, including home blood pressure and heart rate, as well as the stability of blood pressure reduction, remain to be elucidated.16, 22, 24, 32, 33, 34, 35 The present study was conducted to investigate blood pressure variability using s.d., coefficient of variation, maximum minus minimum difference, variability independent of the mean index and average real variability. However, similar to the other Japanese trial,24 none of these indices differed between the two drug groups, indicating that antihypertensive drug classes had no significant impact on blood pressure variability. Blood pressure variability might be useful in daily clinical practice, but it currently remains a research tool that requires further prospective studies with hard end points to define potential applications.36
The final blood pressure levels were similar, and the stabilizing time as well as estimated maximum blood-pressure-lowering effect that was calculated using fitting model analyses were also similar between the HD and D groups (Figure 2). Similar antihypertensive effects are therefore expected from either of these two combination therapies. The current findings partly support the previous report in which further antihypertensive effects were observed after an increased dose of amlodipine from 5 to 10 mg.37 Rakugi et al.38 reported that compared with the fixed-dose combination therapy, adding 12.5 mg of hydrochlorothiazide, a thiazide diuretic, to the fixed-dose combination treatment of 50 mg of losartan and 5 mg of amlodipine resulted in a significant reduction in clinic systolic blood pressure (3.2 mmHg; 95% CI, 0.8 to 5.7; P=0.011) but did not significantly reduce diastolic blood pressure (1.1 mmHg; 95% CI, −0.6 to 2.7; P=0.21). Recent meta-analyses reported that indapamide, a thiazide-like diuretic, was more potent39 and effective40 in preventing cardiovascular complications than thiazide diuretics. The addition of indapamide can be effective for patients who do not achieve adequate blood pressure control by conventional antihypertensive drugs, such as the combination of a low-to-moderate dose of angiotensin receptor blocker and calcium channel blocker. Meanwhile, simplified treatment using fixed-combination drugs is associated with an improvement in adherence.10, 41, 42 Aimix HD, a fixed-dose combination of 100 mg per day irbesartan and 10 mg per day amlodipine, might be useful in terms of drug adherence in patients, even though treatment adherence was not assessed in the present study.
Among blood chemistry profiles, significant differences in uric acid and sodium, potassium and chloride levels between baseline and 3 months after randomization were observed in the D group (Table 4). The changes in uric acid and serum electrolyte levels would be considered as an adverse effect caused by diuretics. However, there were no distinct hyperuricemia events such as gout attack reported during the follow-up period. Changes in the electrolyte levels were also within normal limits (−0.70 mEql l−1, −0.15 mEq l−1 and −1.68 mEq l−1 for sodium, potassium and chloride, respectively). Although changes in blood chemistry profiles may worry doctors, high blood pressure is much more hazardous for cardiovascular disease risk compared with these changes, as long as blood chemistry changes are within normal limits. Recently, Higaki et al.41 reported that the adverse events over a >1-year period among patients who were prescribed antihypertensive polypills with 12.5 mg per day hydrochlorothiazide were generally mild and well tolerated. Therefore, the impact of diuretic use on laboratory profiles may be acceptable; however, a long-term effect should be considered. Inaba et al.43 reported that daily administration of 1 mg of indapamide resulted in increased uric acid levels from 5.6 to 6.1 mg dl−1 with a subsequent normalization to 5.8 mg dl−1 while maintaining reduced clinic blood pressure levels when the patient was switched to an every-other-day regimen of indapamide. Extension of the oral medication interval may be an option when such metabolic changes are observed.
The standard prices of 1 mg of indapamide, Aimix LD, and Aimix HD in Japan are 11.4, 128.2 and 148.6 yen, respectively, as of February 2017.44 Total drug costs in the HD group vs. the D group were 139.6 and 148.6 yen per day, respectively; this is one factor in estimating treatment adherence, along with the number of drugs and adverse effects. Combination tablets are usually distributed at a lower price than single agents;45 the standard prices of Irbesartan (100 mg), amlodipine (5 mg) and amlodipine (10 mg) as generic medicines are 111.9, 20.0–26.2 and 32.1–40.7 yen, respectively.44 The use of angiotensin receptor blocker-containing combination tablets reduces the medication cost for patients,46 as long as the present drug pricing system continues to support such an initiative.
The present findings must be interpreted with potential limitations in mind. First, because this study was an open-label study, a potential bias for the results cannot be ruled out. Second, 30 patients did not measure blood pressure regularly during the follow-up period, and data on 14 patients could not be used for analysis; therefore, only 125 of the 169 randomized patients were analyzed. Third, there may be inter-institutional differences in clinic blood pressure measurements, diagnoses of hypertension and treatments with drugs other than antihypertensive agents, since these decisions were left to the discretion of the physicians that participated in the study. Fourth, patients who reached target blood pressure levels during the study period were excluded before randomization, and the defined target levels were not fully evidence-based, as noted in the Guidelines.18 Therefore, the rate of blood pressure control cannot be evaluated in the present study even though this type of trial design has been used in other studies when assessing antihypertensive drug combination therapy.7, 28, 41 Finally, the drug dose in the present study was set, for example, at 1 mg per day indapamide, which complies with the recent Japanese Guidelines;10 the results might have been different if the dose of indapamide was 2 mg or higher or if other types of antihypertensive drug classes were prescribed.
In conclusion, increased amlodipine dosage and the addition of 1 mg of indapamide were both effective treatment options for further home and clinic systolic blood pressure reduction without any impacts on blood pressure variability and heart rate among patients with insufficient blood pressure control who use the combination regimen of 100 mg per day irbesartan and 5 mg per day amlodipine. The results suggest that both combination therapies may have similar antihypertensive effects; however, further investigation is required regarding the appropriate use of these drugs depending on various complications associated with hypertension.
References
Lewington S, Clarke R, Qizilbash N, Peto R, Collins R . Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 2002; 360: 1903–1913.
Lawes CM, Rodgers A, Bennett DA, Parag V, Suh I, Ueshima H, MacMahon S . Blood pressure and cardiovascular disease in the Asia Pacific region. J Hypertens 2003; 21: 707–716.
The SPRINT Research Group. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med 2015; 373: 2103–2116.
Persell SD . Prevalence of resistant hypertension in the United States, 2003-2008. Hypertension 2011; 57: 1076–1080.
Obara T, Ohkubo T, Asayama K, Metoki H, Inoue R, Kikuya M, Kato T, Tanaka K, Hara A, Hashimoto J, Totsune K, Imai Y . Home blood pressure measurements associated with better blood pressure control: the J-HOME study. J Hum Hypertens 2008; 22: 197–204.
Wald DS, Law M, Morris JK, Bestwick JP, Wald NJ . Combination therapy versus monotherapy in reducing blood pressure: meta-analysis on 11,000 participants from 42 trials. Am J Med 2009; 122: 290–300.
Hosaka M, Metoki H, Satoh M, Ohkubo T, Asayama K, Kikuya M, Inoue R, Obara T, Hirose T, Imai Y . Randomized trial comparing the velocities of the antihypertensive effects on home blood pressure of candesartan and candesartan with hydrochlorothiazide. Hypertens Res 2015; 38: 701–707.
Dahlof B, Sever PS, Poulter NR, Wedel H, Beevers DG, Caulfield M, Collins R, Kjeldsen SE, Kristinsson A, McInnes GT, Mehlsen J, Nieminen M, O'Brien E, Ostergren J . Prevention of cardiovascular events with an antihypertensive regimen of amlodipine adding perindopril as required versus atenolol adding bendroflumethiazide as required, in the Anglo-Scandinavian Cardiac Outcomes Trial-Blood Pressure Lowering Arm (ASCOT-BPLA): a multicentre randomised controlled trial. Lancet 2005; 366: 895–906.
Jamerson K, Weber MA, Bakris GL, Dahlof B, Pitt B, Shi V, Hester A, Gupte J, Gatlin M, Velazquez EJ Investigators AT. Benazepril plus amlodipine or hydrochlorothiazide for hypertension in high-risk patients. N Engl J Med 2008; 359: 2417–2428.
Shimamoto K, Ando K, Fujita T, Hasebe N, Higaki J, Horiuchi M, Imai Y, Imaizumi T, Ishimitsu T, Ito M, Ito S, Itoh H, Iwao H, Kai H, Kario K, Kashihara N, Kawano Y, Kim-Mitsuyama S, Kimura G, Kohara K, Komuro I, Kumagai H, Matsuura H, Miura K, Morishita R, Naruse M, Node K, Ohya Y, Rakugi H, Saito I, Saitoh S, Shimada K, Shimosawa T, Suzuki H, Tamura K, Tanahashi N, Tsuchihashi T, Uchiyama M, Ueda S, Umemura S Japanese Society of Hypertension Committee for Guidelines for the Management of Hypertension. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2014). Hypertens Res 2014; 37: 253–390.
Asayama K, Ohkubo T, Metoki H, Obara T, Inoue R, Kikuya M, Thijs L, Staessen JA, Imai Y . Cardiovascular outcomes in the first trial of antihypertensive therapy guided by self-measured home blood pressure. Hypertens Res 2012; 35: 1102–1110.
Kario K, Saito I, Kushiro T, Teramukai S, Ishikawa Y, Mori Y, Kobayashi F, Shimada K . Home blood pressure and cardiovascular outcomes in patients during antihypertensive therapy: primary results of HONEST, a large-scale prospective, real-world observational study. Hypertension 2014; 64: 989–996.
Jung MH, Kim GH, Kim JH, Moon KW, Yoo KD, Rho TH, Kim CM . Reliability of home blood pressure monitoring: in the context of validation and accuracy. Blood Press Monit 2015; 20: 215–220.
Tsakiri C, Stergiou GS, Boivin JM . Implementation of home blood pressure monitoring in clinical practice. Clin Exp Hypertens 2013; 35: 558–562.
McManus RJ, Mant J, Bray EP, Holder R, Jones MI, Greenfield S, Kaambwa B, Banting M, Bryan S, Little P, Williams B, Hobbs FD . Telemonitoring and self-management in the control of hypertension (TASMINH2): a randomised controlled trial. Lancet 2010; 376: 163–172.
Rothwell PM, Howard SC, Dolan E, O'Brien E, Dobson JE, Dahlof B, Sever PS, Poulter NR . Prognostic significance of visit-to-visit variability, maximum systolic blood pressure, and episodic hypertension. Lancet 2010; 375: 895–905.
World Medical Association declaration of Helsinki. Recommendations guiding physicians in biomedical research involving human subjects. JAMA 1997; 277: 925–926.
Ogihara T, Kikuchi K, Matsuoka H, Fujita T, Higaki J, Horiuchi M, Imai Y, Imaizumi T, Ito S, Iwao H, Kario K, Kawano Y, Kim-Mitsuyama S, Kimura G, Matsubara H, Matsuura H, Naruse M, Saito I, Shimada K, Shimamoto K, Suzuki H, Takishita S, Tanahashi N, Tsuchihashi T, Uchiyama M, Ueda S, Ueshima H, Umemura S, Ishimitsu T, Rakugi H . The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2009). Hypertens Res 2009; 32: 3–107.
Takahashi H, Yoshika M, Yokoi T . Validation of two automatic devices: Omron HEM-7252G-HP and Omron HEM-7251G for self-measurement of blood pressure according to the European Society of Hypertension International Protocol revision 2010. Blood Press Monit 2015; 20: 286–290.
Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, Yamagata K, Tomino Y, Yokoyama H, Hishida A Collaborators developing the Japanese equation for estimated GFR. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis 2009; 53: 982–992.
McKee PA, Castelli WP, McNamara PM, Kannel WB . The natural history of congestive heart failure: the Framingham study. N Engl J Med 1971; 285: 1441–1446.
Asayama K, Kikuya M, Schutte R, Thijs L, Hosaka M, Satoh M, Hara A, Obara T, Inoue R, Metoki H, Hirose T, Ohkubo T, Staessen JA, Imai Y . Home blood pressure variability as cardiovascular risk factor in the population of Ohasama. Hypertension 2013; 61: 61–69.
Schutte R, Thijs L, Liu YP, Asayama K, Jin Y, Odili A, Gu YM, Kuznetsova T, Jacobs L, Staessen JA . Within-subject blood pressure level—not variability—predicts fatal and nonfatal outcomes in a general population. Hypertension 2012; 60: 1138–1147.
Asayama K, Ohkubo T, Hanazawa T, Watabe D, Hosaka M, Satoh M, Yasui D, Staessen JA, Imai Y, Hypertensive Objective Treatment Based on Measurement by Electrical Devices of Blood Pressure Study Investigators. Does antihypertensive drug class affect day-to-day variability of self-measured home blood pressure? The HOMED-BP Study. J Am Heart Assoc 2016; 5: e002995.
Mena L, Pintos S, Queipo NV, Aizpurua JA, Maestre G, Sulbaran T . A reliable index for the prognostic significance of blood pressure variability. J Hypertens 2005; 23: 505–511.
Hansen TW, Thijs L, Li Y, Boggia J, Kikuya M, Björklund-Bodegård K, Richart T, Ohkubo T, Jeppesen J, Torp-Pedersen C, Dolan E, Kuznetsova T, Stolarz-Skrzypek K, Tikhonoff V, Malyutina S, Casiglia E, Nikitin Y, Lind L, Sandoya E, Kawecka-Jaszcz K, Imai Y, Wang J, Ibsen H, O'Brien E, Staessen JA . Prognostic value of reading-to-reading blood pressure variability over 24 hours in 8938 subjects from 11 populations. Hypertension 2010; 55: 1049–1057.
Satoh M, Haga T, Hosaka M, Obara T, Metoki H, Murakami T, Kikuya M, Inoue R, Asayama K, Mano N, Ohkubo T, Imai Y . The velocity of antihypertensive effects of seven angiotensin II receptor blockers determined by home blood pressure measurements. J Hypertens 2016; 34: 1218–1223.
Metoki H, Ohkubo T, Kikuya M, Asayama K, Inoue R, Obara T, Hirose T, Sato M, Imai Y . The velocity of antihypertensive effect of losartan/hydrochlorothiazide and angiotensin II receptor blocker. J Hypertens 2012; 30: 1478–1486.
Moran AE, Odden MC, Thanataveerat A, Tzong KY, Rasmussen PW, Guzman D, Williams L, Bibbins-Domingo K, Coxson PG, Goldman L . Cost-effectiveness of hypertension therapy according to 2014 guidelines. N Engl J Med 2015; 372: 447–455.
Williamson JD, Supiano MA, Applegate WB, Berlowitz DR, Campbell RC, Chertow GM, Fine LJ, Haley WE, Hawfield AT, Ix JH, Kitzman DW, Kostis JB, Krousel-Wood MA, Launer LJ, Oparil S, Rodriguez CJ, Roumie CL, Shorr RI, Sink KM, Wadley VG, Whelton PK, Whittle J, Woolard NF, Wright JT Jr., Pajewski NM Sprint Research Group. Intensive vs standard blood pressure control and cardiovascular disease outcomes in adults aged >/=75 years: a randomized clinical trial. JAMA 2016; 315: 2673–2682.
Ettehad D, Emdin CA, Kiran A, Anderson SG, Callender T, Emberson J, Chalmers J, Rodgers A, Rahimi K . Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet 2016; 387: 957–967.
Johansson JK, Niiranen TJ, Puukka PJ, Jula AM . Prognostic value of the variability in home-measured blood pressure and heart rate: the Finn-Home Study. Hypertension 2012; 59: 212–218.
Kario K . Prognosis in relation to blood pressure variability: pro side of the argument. Hypertension 2015; 65: 1163–1169.
Asayama K, Wei FF, Hara A, Hansen TW, Li Y, Staessen JA . Prognosis in relation to blood pressure variability: con side of the argument. Hypertension 2015; 65: 1170–1179.
Umemoto S, Ogihara T, Matsuzaki M, Rakugi H, Ohashi Y, Saruta T Combination Therapy of Hypertension to Prevent Cardiovascular Events CTG. Effects of calcium channel blocker-based combinations on intra-individual blood pressure variability: post hoc analysis of the COPE trial. Hypertens Res 2016; 39: 46–53.
Asayama K, Wei FF, Liu YP, Hara A, Gu YM, Schutte R, Li Y, Thijs L, Staessen JA . Does blood pressure variability contribute to risk stratification? Methodological issues and a review of outcome studies based on home blood pressure. Hypertens Res 2015; 38: 97–101.
Fujiwara T, Ii Y, Hatsuzawa J, Murase H, Watanabe T, Murakami M, Kimura N, Buch J, Tsuchihashi T, Saruta T . The phase III, double-blind, parallel-group controlled study of amlodipine 10 mg once daily in Japanese patients with essential hypertension who insufficiently responded to amlodipine 5 mg once daily. J Hum Hypertens 2009; 23: 521–529.
Rakugi H, Tsuchihashi T, Shimada K, Numaguchi H, Nishida C, Yamaguchi H, Shirakawa M, Azuma K, Fujita KP . Add-on effect of hydrochlorothiazide 12.5 mg in Japanese subjects with essential hypertension uncontrolled with losartan 50 mg and amlodipine 5 mg. Hypertens Res 2015; 38: 329–335.
Roush GC, Ernst ME, Kostis JB, Tandon S, Sica DA . Head-to-head comparisons of hydrochlorothiazide with indapamide and chlorthalidone: antihypertensive and metabolic effects. Hypertension 2015; 65: 1041–1046.
Chen P, Chaugai S, Zhao F, Wang DW . Cardioprotective effect of thiazide-like diuretics: a meta-analysis. Am J Hypertens 2015; 28: 1453–1463.
Higaki J, Komuro I, Shiki K, Ugai H, Taniguchi A, Ikeda H, Kuroki D, Nishimura S, Ogihara T . The efficacy and long-term safety of a triple combination of 80 mg telmisartan, 5 mg amlodipine and 12.5 mg hydrochlorothiazide in Japanese patients with essential hypertension: a randomized, double-blind study with open-label extension. Hypertens Res 2017; 40: 51–60.
Gupta AK, Arshad S, Poulter NR . Compliance, safety, and effectiveness of fixed-dose combinations of antihypertensive agents: a meta-analysis. Hypertension 2010; 55: 399–407.
Inaba M, Noguchi Y, Yamamoto T, Imai T, Hatano M, Yagi S, Katayama S . Effects of a low dose of indapamide, a diuretic, given daily or every-other-day on blood pressure and metabolic parameters. Hypertens Res 2004; 27: 141–145.
Ministry of Health, Labour and Welfare. National Health Insurance Drug List. 2017; 2017.
Teramachi H, Takahashi T, Tachi T, Noguchi Y, Nagasawa H, Ino Y, Mizui T, Goto C, Tsuchiya T . Influence of angiotensin II receptor blocker combination tablet prescription on drug number and cost. SAGE Open Med 2014; 2: 2050312114563318.
Akazawa M, Fukuoka K . Economic impact of switching to fixed-dose combination therapy for Japanese hypertensive patients: a retrospective cost analysis. BMC Health Serv Res 2013; 13: 124.
Acknowledgements
The authors thank the following physicians and staff members, as well as their respective institutions, for their gracious assistance and cooperation with this study: K Hirofumi, H Takahashi, Y Mesuda and N Fujimoto (Nihon University Hospital, Tokyo, Japan); H Kihara (Kihara Clinic, Asahikawa, Japan); Y Ogasawara (Takiyama Hospital, Tokyo, Japan); M Matsumoto and M Kobori (Japan Community Health Care Organization, Yokohama Chuo Hospital, Yokohama, Japan); K Sugino (Sugino Clinic, Tokyo, Japan); H Kurumatani (Kurumatani Clinic, Tokyo, Japan); Y Akamine (Life Planning Center, Tokyo, Japan); H Emoto (Baigou Clinic, Tokyo, Japan); and T Ebuchi (Ebuchi Clinic, Tokyo, Japan). Omron Healthcare (Kyoto, Japan) developed and managed the internet-based MedicalLINK online registration and telemonitoring system.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
ST received grant funds from Sumitomo Dainippon Pharma and OmronHealthcare, Kyoto, Japan. TK received grant funds and lecture fees from Sumitomo Dainippon Pharma. The remaining authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Tani, S., Asayama, K., Oiwa, K. et al. The effects of increasing calcium channel blocker dose vs. adding a diuretic to treatment regimens for patients with uncontrolled hypertension. Hypertens Res 40, 892–898 (2017). https://doi.org/10.1038/hr.2017.56
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2017.56
Keywords
This article is cited by
-
Thiazide Diuretic–Induced Change in Fasting Plasma Glucose: a Meta-analysis of Randomized Clinical Trials
Journal of General Internal Medicine (2020)
-
Treatment patterns and adherence to antihypertensive combination therapies in Japan using a claims database
Hypertension Research (2019)
-
Analysis of antihypertensive treatment using real-world Japanese data—the retrospective study of antihypertensives for lowering blood pressure (REAL) study
Hypertension Research (2019)