Abstract
Objectives:
Increased energy expenditure (EE) has been proposed as an important mechanism for weight loss following Roux-en-Y gastric bypass (RYGB). However, this has never been investigated in a controlled setting independent of changes in energy balance. Similarly, only few studies have investigated the effect of RYGB on glycaemic control per se. Here, we investigated the effect of RYGB on EE, appetite, glycaemic control and specific signalling molecules compared with a control group in comparable negative energy balance.
Subjects/Methods:
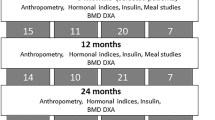
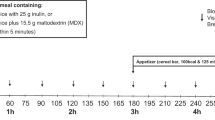
Obese normal glucose-tolerant participants were randomized to receive RYGB after 8 (n=14) or 12 weeks (n=14). The protocol included a visit at week 0 and three visits (weeks 7, 11 and 78) where 24-h EE, appetite and blood parameters were assessed. Participants followed a low-calorie diet from weeks 0–11, with those operated at week 12 serving as a control group for those operated at week 8.
Results:
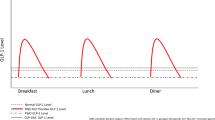
Compared with controls, RYGB-operated participants had lower body composition-adjusted 24-h EE and basal EE 3 weeks postoperatively (both P<0.05) but EE parameters at week 78 were not different from preoperative values (week 7). Surgery changed the postprandial response of glucagon-like peptide-1 (GLP-1), peptide YY3–36 (PYY), ghrelin, cholecystokinin, fibroblast growth factor-19 and bile acids (all P<0.05). Particularly, increases in GLP-1, PYY and decreases in ghrelin were associated with decreased appetite. None of HOMA-IR (homeostasis model assessment-estimated insulin resistance), Matsuda index, the insulinogenic index, the disposition index and fasting hepatic insulin clearance were different between the groups, but RYGB operated had lower fasting glucose (P<0.05) and the postprandial glucose profile was shifted to the left (P<0.01).
Conclusions:
Our data do not support that EE is increased after RYGB. More likely, RYGB promotes weight loss by reducing appetite, partly mediated by changes in gastrointestinal hormone secretion. Furthermore, we found that the early changes in glycaemic control after RYGB is to a large extent mediated by caloric restriction.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Sjostrom L, Narbro K, Sjostrom CD, Karason K, Larsson B, Wedel H et al. Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med 2007; 357: 741–752.
Astrup A, Gotzsche PC, van de Werken K, Ranneries C, Toubro S, Raben A et al. Meta-analysis of resting metabolic rate in formerly obese subjects. Am J Clin Nutr 1999; 69: 1117–1122.
Bueter M, Lowenstein C, Olbers T, Wang M, Cluny NL, Bloom SR et al. Gastric bypass increases energy expenditure in rats. Gastroenterology 2010; 138: 1845–1853.
Stylopoulos N, Hoppin AG, Kaplan LM . Roux-en-Y gastric bypass enhances energy expenditure and extends lifespan in diet-induced obese rats. Obesity (Silver Spring, MD) 2009; 17: 1839–1847.
Zechner JF, Mirshahi UL, Satapati S, Berglund ED, Rossi J, Scott MM et al. Weight-independent effects of Roux-en-Y Gastric Bypass on glucose homeostasis via melanocortin-4 receptors in mice and humans. Gastroenterology 2013; 144: 580–590.e7.
Bobbioni-Harsch E, Morel P, Huber O, Assimacopoulos-Jeannet F, Chassot G, Lehmann T et al. Energy economy hampers body weight loss after gastric bypass. J Clin Endocrinol Metab 2000; 85: 4695–4700.
Carey DG, Pliego GJ, Raymond RL, Skau KB . Body composition and metabolic changes following bariatric surgery: effects on fat mass, lean mass and basal metabolic rate. Obes Surg 2006; 16: 469–477.
Carrasco F, Papapietro K, Csendes A, Salazar G, Echenique C, Lisboa C et al. Changes in resting energy expenditure and body composition after weight loss following Roux-en-Y gastric bypass. Obes Surg 2007; 17: 608–616.
Clements RH, Saraf N, Kakade M, Yellumahanthi K, White M, Hackett JA . Nutritional effect of oral supplement enriched in beta-hydroxy-beta-methylbutyrate, glutamine and arginine on resting metabolic rate after laparoscopic gastric bypass. Surg Endosc 2011; 25: 1376–1382.
Das SK, Roberts SB, McCrory MA, Hsu LK, Shikora SA, Kehayias JJ et al. Long-term changes in energy expenditure and body composition after massive weight loss induced by gastric bypass surgery. Am J Clin Nutr 2003; 78: 22–30.
de Castro CM, de Lima Montebelo MI, Rasera I Jr, de Oliveira AVJ, Gomes Gonelli PR, Aparecida CG . Effects of Roux-en-Y gastric bypass on resting energy expenditure in women. Obes Surg 2008; 18: 1376–1380.
Del GF, Alfonsi L, Marra M, Finelli C, Del GG, Rossetti G et al. Metabolic and nutritional status changes after 10% weight loss in severely obese patients treated with laparoscopic surgery vs integrated medical treatment. Obes Surg 2007; 17: 1592–1598.
Faria SL, Faria OP, Buffington C, de Almeida CM, Rodrigues de GH . Energy expenditure before and after Roux-en-Y gastric bypass. Obes Surg 2012; 22: 1450–1455.
Faria SL, Faria OP, de Almeida CM, Gouvea HR, Buffington C . Diet-induced thermogenesis and respiratory quotient after Roux-en-Y gastric bypass. Surg Obes Relat Dis 2012; 8: 797–802.
Flancbaum L, Choban PS, Bradley LR, Burge JC . Changes in measured resting energy expenditure after Roux-en-Y gastric bypass for clinically severe obesity. Surgery 1997; 122: 943–949.
Knuth ND, Johannsen DL, Tamboli RA, Marks-Shulman PA, Huizenga R, Chen KY et al. Metabolic adaptation following massive weight loss is related to the degree of energy imbalance and changes in circulating leptin. Obesity (Silver Spring, MD) 2014; 22: 2563–2569.
Liu X, Lagoy A, Discenza I, Papineau G, Lewis E, Braden G et al. Metabolic and neuroendocrine responses to Roux-en-Y gastric bypass. I: energy balance, metabolic changes, and fat loss. J Clin Endocrinol Metab 2012; 97: E1440–E1450.
Olbers T, Bjorkman S, Lindroos A, Maleckas A, Lonn L, Sjostrom L, Lonroth H . Body composition, dietary intake, and energy expenditure after laparoscopic Roux-en-Y gastric bypass and laparoscopic vertical banded gastroplasty: a randomized clinical trial. Ann Surg 2006; 244: 715–722.
Simonen M, Dali-Youcef N, Kaminska D, Venesmaa S, Kakela P, Paakkonen M et al. Conjugated bile acids associate with altered rates of glucose and lipid oxidation after Roux-en-Y Gastric Bypass. Obes Surg 2012; 22: 1473–1480.
Rabl C, Rao MN, Schwarz JM, Mulligan K, Campos GM . Thermogenic changes after gastric bypass, adjustable gastric banding or di. Surgery 2014; 156: 806–812.
Harvey EJ, Arroyo K, Korner J, Inabnet WB . Hormone changes affecting energy homeostasis after metabolic surgery. Mt Sinai J Med 2010; 77: 446–465.
Borg CM, le Roux CW, Ghatei MA, Bloom SR, Patel AG, Aylwin SJ . Progressive rise in gut hormone levels after Roux-en-Y gastric bypass suggests gut adaptation and explains altered satiety. Br J Surg 2006; 93: 210–215.
Kruseman M, Leimgruber A, Zumbach F, Golay A . Dietary, weight, and psychological changes among patients with obesity, 8 years after gastric bypass. J Am Diet Assoc 2010; 110: 527–534.
Faria SL, Faria OP, Lopes TC, Galvao MV, de Oliveira KE, Ito MK . Relation between carbohydrate intake and weight loss after bariatric surgery. Obes Surg 2009; 19: 708–716.
Watanabe M, Houten SM, Mataki C, Christoffolete MA, Kim BW, Sato H et al. Bile acids induce energy expenditure by promoting intracellular thyroid hormone activation. Nature 2006; 439: 484–489.
Pournaras DJ, Glicksman C, Vincent RP, Kuganolipava S, Alaghband-Zadeh J, Mahon D et al. The role of bile after Roux-en-Y gastric bypass in promoting weight loss and improving glycaemic control. Endocrinology 2012; 153: 3613–3619.
Sloth B, Holst JJ, Flint A, Gregersen NT, Astrup A . Effects of PYY1-36 and PYY3-36 on appetite, energy intake, energy expenditure, glucose and fat metabolism in obese and lean subjects. Am J Physiol Endocrinol Metab 2007; 292: E1062–E1068.
Rubino F, Schauer PR, Kaplan LM, Cummings DE . Metabolic surgery to treat type 2 diabetes: clinical outcomes and mechanisms of action. Annu Rev Med 2010; 61: 393–411.
Madsbad S, Dirksen C, Holst JJ . Mechanisms of changes in glucose metabolism and bodyweight after bariatric surgery. Lancet Diabetes Endocrinol 2014; 2: 152–164.
Henry RR, Wiest-Kent TA, Scheaffer L, Kolterman OG, Olefsky JM . Metabolic consequences of very-low-calorie diet therapy in obese non-insulin-dependent diabetic and nondiabetic subjects. Diabetes 1986; 35: 155–164.
Foo J, Krebs J, Hayes MT, Bell D, Macartney-Coxson D, Croft T et al. Studies in insulin resistance following very low calorie diet and/or gastric bypass surgery. Obes Surg 2011; 21: 1914–1920.
Lips MA, de Groot GH, van Klinken JB, Aarts E, Berends FJ, Janssen IM et al. Calorie restriction is a major determinant of the short-term metabolic effects of gastric bypass surgery in obese type 2 diabetic patients. Clin Endocrinol (Oxf) 2014; 80: 834–842.
Jackness C, Karmally W, Febres G, Conwell IM, Ahmed L, Bessler M et al. Very low-calorie diet mimics the early beneficial effect of Roux-en-Y gastric bypass on insulin sensitivity and beta-cell Function in type 2 diabetic patients. Diabetes 2013; 62: 3027–3032.
Isbell JM, Tamboli RA, Hansen EN, Saliba J, Dunn JP, Phillips SE et al. The importance of caloric restriction in the early improvements in insulin sensitivity after Roux-en-Y gastric bypass surgery. Diabetes Care 2010; 33: 1438–1442.
Levitt DG, Beckman LM, Mager JR, Valentine BJ, Sibley SD, Beckman TR et al. Comparison of DXA and water measurements of body fat following gastric bypass surgery and a physiological model of body water, fat, and muscle composition. J Appl Physiol 2010.
Elia M, Livesey G . Energy expenditure and fuel selection in biological systems: the theory and practice of calculations based on indirect calorimetry and tracer methods. World Rev Nutr Diet 1992; 70: 68–131.
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC . Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 1985; 28: 412–419.
Kahn SE . The relative contributions of insulin resistance and beta-cell dysfunction to the pathophysiology of Type 2 diabetes. Diabetologia 2003; 46: 3–19.
R Core Team. R: A Language and Environment for Statiscial Computing R Foundation for Statistical Computing. R Core Team: Vienna, Austria, 2012; ISBN 3-900051-07-0 2012.
Radikova Z, Koska J, Huckova M, Ksinantova L, Imrich R, Vigas M et al. Insulin sensitivity indices: a proposal of cut-off points for simple identification of insulin-resistant subjects. Exp Clin Endocrinol Diabetes 2006; 114: 249–256.
Tamboli RA, Hossain HA, Marks PA, Eckhauser AW, Rathmacher JA, Phillips SE et al. Body composition and energy metabolism following Roux-en-Y Gastric Bypass Surgery. Obesity (Silver Spring, MD) 2010; 18: 1718–1724.
Pavlou KN, Hoefer MA, Blackburn GL . Resting energy expenditure in moderate obesity. Predicting velocity of weight loss. Ann Surg 1986; 203: 136–141.
Werling M, Olbers T, Fandriks L, Bueter M, Lonroth H, Stenlof K et al. Increased postprandial energy expenditure may explain superior long term weight loss after roux-en-y gastric bypass compared to vertical banded gastroplasty. PLoS One 2013; 8: e60280.
Ravussin E, Bogardus C . Relationship of genetics, age, and physical fitness to daily energy expenditure and fuel utilization. Am J Clin Nutr 1989; 49 (Suppl): 968–975.
Allison DB, Paultre F, Goran MI, Poehlman ET, Heymsfield SB . Statistical considerations regarding the use of ratios to adjust data. Int J Obes Relat Metab Disord 1995; 19: 644–652.
Weinsier RL, Nagy TR, Hunter GR, Darnell BE, Hensrud DD, Weiss HL . Do adaptive changes in metabolic rate favor weight regain in weight-reduced individuals? An examination of the set-point theory. Am J Clin Nutr 2000; 72: 1088–1094.
Kaiyala KJ, Schwartz MW . Toward a more complete (and less controversial) understanding of energy expenditure and its role in obesity pathogenesis. Diabetes 2011; 60: 17–23.
Rosenbaum M, Leibel RL . Adaptive thermogenesis in humans. Int J Obes (Lond) 2010; 34 (Suppl): S47–S55.
Dardeno TA, Chou SH, Moon HS, Chamberland JP, Fiorenza CG, Mantzoros CS . Leptin in human physiology and therapeutics. Front Neuroendocrinol 2010; 31: 377–393.
Kohli R, Bradley D, Setchell KD, Eagon JC, Abumrad N, Klein S . Weight loss induced by Roux-en-Y gastric bypass but not laparoscopic adjustable gastric banding increases circulating bile acids. J Clin Endocrinol Metab 2013; 98: E708–E712.
Westerterp KR . Diet induced thermogenesis. Nutr Metab (Lond) 2004; 1: 5.
Dirksen C, Damgaard M, Bojsen-Moller KN, Jorgensen NB, Kielgast U, Jacobsen SH et al. Fast pouch emptying, delayed small intestinal transit, and exaggerated gut hormone responses after Roux-en-Y gastric bypass. Neurogastroenterol Motil 2013; 25: 346–e255.
Horowitz M, Collins PJ, Chatterton BE, Harding PE, Watts JM, Shearman DJ . Gastric emptying after gastroplasty for morbid obesity. Br J Surg 1984; 71: 435–437.
Deitel M, Khanna RK, Hagen J, Ilves R . Vertical banded gastroplasty as an antireflux procedure. Am J Surg 1988; 155: 512–516.
Burton PR, Yap K, Brown WA, Laurie C, O'Donnell M, Hebbard G et al. Changes in satiety, supra- and infraband transit, and gastric emptying following laparoscopic adjustable gastric banding: a prospective follow-up study. Obes Surg 2011; 21: 217–223.
le Roux CW, Borg C, Wallis K, Vincent RP, Bueter M, Goodlad R et al. Gut hypertrophy after gastric bypass is associated with increased glucagon-like peptide 2 and intestinal crypt cell proliferation. Ann Surg 2010; 252: 50–56.
Vijgen GH, Bouvy ND, Teule GJ, Brans B, Schrauwen P, van Marken Lichtenbelt WD . Brown adipose tissue in morbidly obese subjects. PLoS One 2011; 6: e17247.
le Roux CW, Welbourn R, Werling M, Osborne A, Kokkinos A, Laurenius A et al. Gut hormones as mediators of appetite and weight loss after Roux-en-Y gastric bypass. Ann Surg 2007; 246: 780–785.
Dirksen C, Jorgensen NB, Bojsen-Moller KN, Kielgast U, Jacobsen SH, Clausen TR et al. Gut hormones, early dumping and resting energy expenditure in patients with good and poor weight loss response after Roux-en-Y gastric bypass. Int J Obes (Lond) 2013; 37: 1452–1459.
Bryant EJ, King N, Falken Y, Hellstrom PM, Holst JJ, Blundell J et al. Relationship among tonic and episodic aspects of motovation to eat, gut peptide, and weight before and after bariatric surgery. Surg Obesity Relat Dis 2012; 9: 802–808.
Falken Y, Hellstrom PM, Holst JJ, Naslund E . Changes in glucose homeostasis after Roux-en-Y gastric bypass surgery for obesity at day three, two months, and one year after surgery: role of gut peptides. J Clin Endocrinol Metab 2011; 96: 2227–2235.
Korner J, Inabnet W, Conwell IM, Taveras C, Daud A, Olivero-Rivera L et al. Differential effects of gastric bypass and banding on circulating gut hormone and leptin levels. Obesity (Silver Spring, MD) 2006; 14: 1553–1561.
Pournaras DJ, Osborne A, Hawkins SC, Mahon D, Ghatei MA, Bloom SR et al. The gut hormone response following Roux-en-Y gastric bypass: cross-sectional and prospective study. Obes Surg 2010; 20: 56–60.
Matsuda M, DeFronzo RA . Insulin sensitivity indices obtained from oral glucose tolerance testing: comparison with the euglycemic insulin clamp. Diabetes Care 1999; 22: 1462–1470.
Dirksen C, Jorgensen NB, Bojsen-Moller KN, Jacobsen SH, Hansen DL, Worm D et al. Mechanisms of improved glycaemic control after Roux-en-Y gastric bypass. Diabetologia 2012; 55: 1890–1901.
Patti ME, Houten SM, Bianco AC, Bernier R, Larsen PR, Holst JJ et al. Serum bile acids are higher in humans with prior gastric bypass: potential contribution to improved glucose and lipid metabolism. Obesity (Silver Spring, MD) 2009; 17: 1671–1677.
Odstrcil EA, Martinez JG, Santa Ana CA, Xue B, Schneider RE, Steffer KJ et al. The contribution of malabsorption to the reduction in net energy absorption after long-limb Roux-en-Y gastric bypass. Am J Clin Nutr 2010; 92: 704–713.
Thorell A, Nygren J, Hirshman MF, Hayashi T, Nair KS, Horton ES et al. Surgery-induced insulin resistance in human patients: relation to glucose transport and utilization. Am J Physiol 1999; 276: E754–E761.
Nygren J, Thorell A, Efendic S, Nair KS, Ljungqvist O . Site of insulin resistance after surgery: the contribution of hypocaloric nutrition and bed rest. Clin Sci (Lond) 1997; 93: 137–146.
Acknowledgements
We thank Luise Gunvald, John Gargul Lind, Lene Stevner, Jane Jørgensen, Søren Andresen, Marianne Juul, Ulla Skovbæch Pedersen (all from the Department of Nutrition, Exercise and Sports, Denmark), Gitte Kølander Hansen (Novo Nordisk, Måløv, Denmark), Lene Albæk (MFI) for technical assistance and surgeons and the surgical staff (Hvidovre Hospital, Denmark). Except for Lind, Stevner, Jørgensen, Andresen, Juul and Pedersen, no financial compensation was given to the above-mentioned for their role in the study. The study was carried out as a part of UNIK: Food, Fitness and Pharma for Health and Disease at the University of Copenhagen. The UNIK project was funded by the Danish Ministry of Science, Technology and Innovation. Cambridge Weight Plan, UK provided the low-calorie diet products and Novo Nordisk A/S, DK supported costs of analysis of bile acids. The study was registered at ClinicalTrials.gov.
Author contributions
Dr Schmidt and Dr Sjödin had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Conception and design: Gregersen, Pedersen, Madsbad, Astrup, Holst, Sjödin, Worm, Hansen. Acquisition of data: Schmidt, Gregersen, Vestergaard, Søndergaard, Madsbad, Clausen, Holst, Rehfeld. Analysis and interpretation of data: Schmidt, Gregersen, Pedersen, Vestergaard, Søndergaard, Ritz, Madsbad, Clausen, Astrup, Holst, Sjödin, Rehfeld, Worm, Hansen. Drafting of the manuscript: Schmidt, Pedersen, Madsbad, Sjödin, Holst. Critical revision of the manuscript for important intellectual content: Schmidt, Gregersen, Pedersen, Vestergaard, Søndergaard, Ritz, Madsbad, Clausen, Astrup, Holst, Sjödin, Rehfeld, Worm, Hansen. Statistical analysis: Schmidt, Vestergaard, Søndergaard, Ritz. Obtained funding: Gregersen, Pedersen, Astrup, Holst, Sjödin, Worm, Hansen. Administrative, technical or material support: Schmidt, Clausen, Astrup, Sjödin, Rehfeld. Study supervision: Gregersen, Pedersen, Madsbad, Astrup, Holst, Sjödin. Final approval of the submitted manuscript: Schmidt, Gregersen, Pedersen, Vestergaard, Søndergaard, Ritz, Madsbad, Clausen, Astrup, Holst, Sjödin, Rehfeld, Worm, Hansen.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
Dr Schmidt reported receiving a research grant from University of Copenhagen personal grant support from Twinlab and a travel grant from Cambridge Weight Plan UK. Dr Gregersen reported receiving a travel grant from Cambridge Weight Plan UK, and reported being employed by Novo Nordisk A/S (Dr Gregersen was employed at the Department of Nutrition, Exercise and Sports at the time of the study). Dr Pedersen reported receiving travel grants from Cambridge Weight Plan UK and receiving travel expenses and speakers’ honoraria from Novo Nordisk A/S, Eli Lilly and Sanofi Aventis and speakers’ honoraria from Astra Zeneca. M Søndergaard reported receiving a travel grant from Cambridge Weight Plan UK. T Clausen reported being employed by Novo Nordisk A/S, a former employee by Zealand Pharma A/S and holding stocks in Novo Nordisk A/S and Zealand Pharma A/S. Dr Astrup reported receiving research grants from Danish Ministry of Science, Technology and Innovation, and consulting fees from Arena Pharmaceuticals Inc., Basic Research, BioCare Copenhagen, BoehringerIngelheimPharma GmbH & Co.KG, Dutch Beer Knowledge Institute, Gelesis, Gerson Lehrman Group, Global Dairy Platform, Jenny Craig, McCain Foods Limited, McDonald’s, Novo Nordisk, Pathway Genomics Corporation, S-Biotek and Twinlab and personal fees from Vivus. Dr Holst reported that he serves as an advisory board member for Glaxo, Smith, Kline, Novo Nordisk and Zealand Pharmaceuticals and receives grants from NOVARTIS and Merck and consulting fees from Novo Nordisk. The remaining authors declare no conflict of interest.
The Danish Ministry of Science, Technology and Innovation and the Strategic Research Council of the Capital Area had no role in the collection, management, analysis and interpretation of the study data, and had no part in the preparation of the manuscript.
Additional information
Supplementary Information accompanies this paper on International Journal of Obesity website
Supplementary information
Rights and permissions
About this article
Cite this article
Schmidt, J., Pedersen, S., Gregersen, N. et al. Effects of RYGB on energy expenditure, appetite and glycaemic control: a randomized controlled clinical trial. Int J Obes 40, 281–290 (2016). https://doi.org/10.1038/ijo.2015.162
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2015.162
This article is cited by
-
Primary weight loss failure after Roux-en-Y gastric bypass is characterized by impaired gut-hormone mediated regulation of food intake
International Journal of Obesity (2023)
-
Suboptimal Weight Loss 13 Years After Roux-en-Y Gastric Bypass: Is Hedonic Hunger, Eating Behaviour and Food Reward to Blame?
Obesity Surgery (2022)
-
The Leading Role of Peptide Tyrosine Tyrosine in Glycemic Control After Roux-en-Y Gastric Bypass in Rats
Obesity Surgery (2020)
-
Bypassed and Preserved Stomach Resulted in Superior Glucose Control in Sprague-Dawley Rats with Streptozotocin-Induced Diabetes
Scientific Reports (2019)
-
Ongoing Inconsistencies in Weight Loss Reporting Following Bariatric Surgery: a Systematic Review
Obesity Surgery (2019)