Abstract
Background:
Probiotics are commonly used after bariatric surgery; however, uncertainty remains regarding their efficacy. Our aim was to compare the effect of probiotics vs placebo on hepatic, inflammatory and clinical outcomes following laparoscopic sleeve gastrectomy (LSG).
Methods:
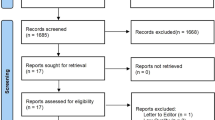
This randomized, double-blind, placebo-controlled, trial of 6-month treatment with probiotics (Bio-25; Supherb) vs placebo and 6 months of additional follow-up was conducted among 100 morbidly obese nonalcoholic fatty liver disease (NAFLD) patients who underwent LSG surgery. The primary outcome was a reduction in liver fat content, measured by abdominal ultrasound, and secondary outcomes were improvement of fibrosis, measured by shear-wave elastography, metabolic and inflammatory parameters, anthropometrics and quality of life (QOL). Fecal samples were collected and analyzed for microbial composition.
Results:
One hundred patients (60% women, mean age of 41.9±9.8 years and body mass index of 42.3±4.7 kg m−2) were randomized, 80% attended the 6-month visit and 77% completed the 12-month follow-up. Fat content and NAFLD remission rate were similarly reduced in the probiotics and placebo groups at 6 months postsurgery (−0.9±0.5 vs −0.7±0.4 score; P=0.059 and 52.5 vs 40%; P=0.262, respectively) and at 12 months postsurgery. Fibrosis, liver-enzymes, C-reactive protein (CRP), leptin and cytokeratin-18 levels were significantly reduced and QOL significantly improved within groups (P⩽0.014 for all), but not between groups (P⩾0.173 for all) at 6 and 12 months postsurgery. Within-sample microbiota diversity (alpha-diversity) increased at 6-month postsurgery compared with baseline in both study arms (P⩽0.008) and decreased again at 12 months postsurgery compared with 6 months postsurgery (P⩽0.004) but did not reach baseline values.
Conclusions:
Probiotics administration does not improve hepatic, inflammatory and clinical outcomes 6- and 12 months post-LSG.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Hannah Jr WN, Harrison SA . Effect of weight loss, diet, exercise, and bariatric surgery on nonalcoholic fatty liver disease. Clin Liver Dis 2016; 20: 339–350.
Bower G, Toma T, Harling L, Jiao LR, Efthimiou E, Darzi A et al. Bariatric surgery and non-alcoholic fatty liver disease: a systematic review of liver biochemistry and histology. Obes Surg 2015; 25: 2280–2289.
Lee WJ, Almulaifi A . Recent advances in bariatric/metabolic surgery: appraisal of clinical evidence. J Biomed Res 2015; 29: 98–104.
Benaiges D, Mas-Lorenzo A, Goday A, Ramon JM, Chillaron JJ, Pedro-Botet J et al. Laparoscopic sleeve gastrectomy: more than a restrictive bariatric surgery procedure? World J Gastroenterol 2015; 21: 11804–11814.
Sweeney TE, Morton JM . Metabolic surgery: action via hormonal milieu changes, changes in bile acids or gut microbiota? A summary of the literature. Best Pract Res Clin Gastroenterol 2014; 28: 727–740.
Graessler J, Qin Y, Zhong H, Zhang J, Licinio J, Wong ML et al. Metagenomic sequencing of the human gut microbiome before and after bariatric surgery in obese patients with type 2 diabetes: correlation with inflammatory and metabolic parameters. Pharmacogenomics J 2013; 13: 514–522.
Furet JP, Kong LC, Tap J, Poitou C, Basdevant A, Bouillot JL et al. Differential adaptation of human gut microbiota to bariatric surgery-induced weight loss: links with metabolic and low-grade inflammation markers. Diabetes 2010; 59: 3049–3057.
Zhang H, DiBaise JK, Zuccolo A, Kudrna D, Braidotti M, Yu Y et al. Human gut microbiota in obesity and after gastric bypass. Proc Natl Acad Sci USA 2009; 106: 2365–2370.
Kong LC, Tap J, Aron-Wisnewsky J, Pelloux V, Basdevant A, Bouillot JL et al. Gut microbiota after gastric bypass in human obesity: increased richness and associations of bacterial genera with adipose tissue genes. Am J Clin Nutr 2013; 98: 16–24.
Damms-Machado A, Mitra S, Schollenberger AE, Kramer KM, Meile T, Konigsrainer A et al. Effects of surgical and dietary weight loss therapy for obesity on gut microbiota composition and nutrient absorption. Biomed Res Int 2015; 2015: 806248.
Palleja A, Kashani A, Allin KH, Nielsen T, Zhang C, Li Y et al. Roux-en-Y gastric bypass surgery of morbidly obese patients induces swift and persistent changes of the individual gut microbiota. Genome Med 2016; 8: 67.
Murphy R, Tsai P, Jullig M, Liu A, Plank L, Booth M . Differential changes in gut microbiota after gastric bypass and sleeve gastrectomy bariatric surgery vary according to diabetes remission. Obes Surg 2017; 27: 917–925.
Woodard GA, Encarnacion B, Downey JR, Peraza J, Chong K, Hernandez-Boussard T et al. Probiotics improve outcomes after Roux-en-Y gastric bypass surgery: a prospective randomized trial. J Gastrointest Surg 2009; 13: 1198–1204.
Bashiardes S, Shapiro H, Rozin S, Shibolet O, Elinav E . Non-alcoholic fatty liver and the gut microbiota. Mol Metab 2016; 5: 782–794.
Loguercio C, Federico A, Tuccillo C, Terracciano F, D'Auria MV, De Simone C et al. Beneficial effects of a probiotic VSL#3 on parameters of liver dysfunction in chronic liver diseases. J Clin Gastroenterol 2005; 39: 540–543.
Alisi A, Bedogni G, Baviera G, Giorgio V, Porro E, Paris C et al. Randomised clinical trial: the beneficial effects of VSL#3 in obese children with non-alcoholic steatohepatitis. Aliment Pharmacol Ther 2014; 39: 1276–1285.
Nabavi S, Rafraf M, Somi MH, Homayouni-Rad A, Asghari-Jafarabadi M . Effects of probiotic yogurt consumption on metabolic factors in individuals with nonalcoholic fatty liver disease. J Dairy Sci 2014; 97: 7386–7393.
Fernandes R, Beserra BT, Mocellin MC, Kuntz MG, da Rosa JS, de Miranda RC et al. Effects of prebiotic and synbiotic supplementation on inflammatory markers and anthropometric indices after Roux-en-Y gastric bypass: a randomized, triple-blind, placebo-controlled pilot study. J Clin Gastroenterol 2016; 50: 208–217.
Chen JC, Lee WJ, Tsou JJ, Liu TP, Tsai PL . Effect of probiotics on postoperative quality of gastric bypass surgeries: a prospective randomized trial. Surg Obes Relat Dis 2016; 12: 57–61.
Doig GS, Simpson F . Randomization and allocation concealment: a practical guide for researchers. J Crit Care 2005; 20: 187–191; discussion 91–93.
Ho PM, Bryson CL, Rumsfeld JS . Medication adherence: its importance in cardiovascular outcomes. Circulation 2009; 119: 3028–3035.
Schulz KF, Altman DG, Moher D . CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. J Pharmacol Pharmacother 2010; 1: 100–107.
Keinan-Boker L, Noyman N, Chinich A, Green MS, Nitzan-Kaluski D . Overweight and obesity prevalence in Israel: findings of the first national health and nutrition survey (MABAT). Isr Med Assoc J 2005; 7: 219–223.
Bentur N, King Y . The challenge of validating SF-12 for its use with community-dwelling elderly in Israel. Qual Life Res 2010; 19: 91–95.
Gore R . Diffuse liver disease. In: Gore R, Levine M, Laufer I (eds). Editor Textbook of Gastrointestinal Radiology. Saunders: Philadelphia, PA, USA, 1994; pp 1968–2017.
Zelber-Sagi S, Buch A, Yeshua H, Vaisman N, Webb M, Harari G et al. Effect of resistance training on non-alcoholic fatty-liver disease a randomized-clinical trial. World J Gastroenterol 2014; 20: 4382–4392.
Webb M, Yeshua H, Zelber-Sagi S, Santo E, Brazowski E, Halpern Z et al. Diagnostic value of a computerized hepatorenal index for sonographic quantification of liver steatosis. AJR Am J Roentgenol 2009; 192: 909–914.
Landis JR, Koch GG . The measurement of observer agreement for categorical data. Biometrics 1977; 33: 159–174.
Poynard T, Munteanu M, Luckina E, Perazzo H, Ngo Y, Royer L et al. Liver fibrosis evaluation using real-time shear wave elastography: applicability and diagnostic performance using methods without a gold standard. J Hepatol 2013; 58: 928–935.
Toolabi K, Arefanian S, Golzarand M, Arefanian H . Effects of laparoscopic Roux-en-Y gastric bypass (LRYGB) on weight loss and biomarker parameters in morbidly obese patients: a 12-month follow-up. Obes Surg 2011; 21: 1834–1842.
Mirrakhimov AE, Lunegova OS, Kerimkulova AS, Moldokeeva CB, Nabiev MP, Mirrakhimov EM . Cut off values for abdominal obesity as a criterion of metabolic syndrome in an ethnic Kyrgyz population (Central Asian region). Cardiovasc Diabetol 2012; 11: 16.
Zeevi D, Korem T, Zmora N, Israeli D, Rothschild D, Weinberger A et al. Personalized nutrition by prediction of glycemic responses. Cell 2015; 163: 1079–1094.
Forslund K, Hildebrand F, Nielsen T, Falony G, Le Chatelier E, Sunagawa S et al. Disentangling type 2 diabetes and metformin treatment signatures in the human gut microbiota. Nature 2015; 528: 262–266.
Tremaroli V, Karlsson F, Werling M, Stahlman M, Kovatcheva-Datchary P, Olbers T et al. Roux-en-Y gastric bypass and vertical banded gastroplasty induce long-term changes on the human gut microbiome contributing to fat mass regulation. Cell Metab 2015; 22: 228–238.
Ma YY, Li L, Yu CH, Shen Z, Chen LH, Li YM . Effects of probiotics on nonalcoholic fatty liver disease: a meta-analysis. World J Gastroenterol 2013; 19: 6911–6918.
Aron-Wisnewsky J, Dore J, Clement K . The importance of the gut microbiota after bariatric surgery. Nat Rev Gastroenterol Hepatol 2012; 9: 590–598.
Tanaka Y, Takami K, Nishijima T, Aoki R, Mawatari T, Ikeda T . Short- and long-term dynamics in the intestinal microbiota following ingestion of Bifidobacterium animalis subsp. lactis GCL2505. Biosci Microbiota Food Health 2015; 34: 77–85.
Mancini M, Prinster A, Annuzzi G, Liuzzi R, Giacco R, Medagli C et al. Sonographic hepatic-renal ratio as indicator of hepatic steatosis: comparison with (1)H magnetic resonance spectroscopy. Metabolism 2009; 58: 1724–1730.
Acknowledgements
This study was supported (in part) by grant no. 3-10470 from the Chief Scientist Office of the Ministry of Health, Israel. The funding source did not have a role in the design, conduct and analysis of the study or the decision to submit the manuscript for publication.
Author contributions
SS-D, SZ-S and OS designed and performed the study, analyzed the data and wrote the paper. GZ-S, EE, ES, JAM, MP-F, NZ and MD-B carried out the microbiota analysis. MW performed the US examinations and NG assisted in MRI decoding. AB, AK, AR, DG and NS assisted in data collection. All authors critically reviewed the manuscript, agreed to be fully accountable for ensuring the integrity and accuracy of the work and read and approved the final manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on International Journal of Obesity website
Rights and permissions
About this article
Cite this article
Sherf-Dagan, S., Zelber-Sagi, S., Zilberman-Schapira, G. et al. Probiotics administration following sleeve gastrectomy surgery: a randomized double-blind trial. Int J Obes 42, 147–155 (2018). https://doi.org/10.1038/ijo.2017.210
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2017.210