Abstract
Objective:
To determine age at diagnosis for congenital duodenal obstruction in the neonatal period and the relationship to clinical outcomes.
Study Design:
A children's hospital database reflecting a 7 ½-year period was reviewed to identify infants with the diagnosis of duodenal obstruction in the neonatal period. Infants were grouped according to time of diagnosis: antepartum, postpartum in-hospital or after hospital discharge. Clinical descriptors and outcome variables were assessed between infants in these three groups.
Result:
In total, 27/51 (53%) infants were diagnosed antenatally. Infants with prenatal diagnosis were less mature, more likely to have Down syndrome or other birth defects and the pregnancy was more likely to be complicated by polyhydramnios. Of the 24 infants diagnosed postnatally, 8 (33%) were diagnosed after hospital discharge. These infants tended to be breast fed and discharged before 48 h of age. They had greater weight loss and more metabolic disturbances at readmission for surgery. One infant in the late diagnosis group died.
Conclusion:
Infants with congenital duodenal obstruction, particularly if breast fed, may not present with classical findings of upper gastrointestinal obstruction in the first days of life. Careful in-hospital evaluation of infants with persistent regurgitation, even low volume, is recommended to avoid missing this diagnosis.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Dalla Vecchia LK, Grosfeld JL, West KW, Rescorla FJ, Scherer LR, Engum SA . Intestinal atresia and stenosis: a 25-year experience with 277 cases. Arch Surgery 1998; 133 (5): 496–497.
Millar AJW, Rode H, Cywes S . Intestinal atresia and stenosis In: Ashcroft KW, Holcomb GW, Murphy JP (eds). Pediatric Surgery 2005 4th edn Saunders: Philadelphia, PA pp 416–434.
Wyllie R . Intestinal atresia, stenosis and malrotation In Kliegman RM, Behrman RE, Jenson HB, Staton BF (eds). Nelson Textbook of Pediatrics. 18th edn WB Saunders: Philadelphia, 2004 pp 1558–1562.
Stallion A, Dudgeon DL . Gastrointestinal obstruction In Hoekelman RA, Adam HM, Nelson NM, Weitzma ML, Wilson MH (eds). Primary Pediatric Care. 4th edn Mosby: St Louis, 2001 pp 1493–1502.
Mustafawi AR, Hassan ME . Congenital duodenal obstruction in children: a decade's experience. Eur J Pediatr Surg 2008; 18 (2): 93–97.
Nelson LH, Clark CE, Fishburne JI, Urban RB, Penry MF . Value of serial sonography in the in utero detection of duodenal atresia. Obstet Gynecol 1982; 59 (5): 657–660.
Grosfeld JL, Rescorla FJ . Duodenal atresia and stenosis: reassessment of treatment and outcome based on antenatal diagnosis, pathologic variance, and long-term follow-up. World J Surg 1993; 17 (3): 301–309.
Fonkalsrud EW, DeLorimer AA, Hays DM . Congenital atresia and stenosis of the duodenum: a review compiled from the members of the Surgical Section of the American Academy of Pediatrics. Pediatrics 1969; 43 (1): 79–83.
Britton JR, Britton HL . Gastric aspirate volume at birth as an indicator of congenital intestinal obstruction. Acta Paediatr 1995; 84 (8): 945–946.
Hancock BJ, Wiseman NE . Congenital duodenal obstruction: the impact of an antenatal diagnosis. J Pediatr Surg 1989; 24 (10): 1027–1031.
Bittencourt DG, Barini R, Marba S, Sbragia L . Congenital duodenal obstruction: does prenatal diagnosis improve the outcome? Pediatr Surg Int 2004; 20 (8): 582–585.
Bailey PV, Tracy Jr TF, Connors RH, Mooney DP, Lewis JE, Weber TR . Congenital duodenal obstruction: a 32-year review. J Pediatr Surg 1993; 28 (1): 92–95.
Escobar MA, Ladd AP, Grosfeld JL, West KW, Rescorla FJ, Scherer 3rd LR et al. Duodenal atresia and stenosis: long-term follow-up over 30 years. J Pediatr Surg 2004; 39 (6): 867–871.
Sniderman S, Charton VE . Care and observation In: AM Rudolph, DC Rudolph (eds). Rudolph's Pediatrics. 21st edn McGraw-Hill: New York, 2003 pp 103–107.
American Academy of Pediatrics/American College of Obstetricians and Gynecologists. Care of the neonate In: Charles J Lockwood, James A Lemons (eds). Guidelines for Perinatal Care. American Academy of Pediatrics (AAP); Elk Grove, IL, 2007, pp 205–249.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kilbride, H., Castor, C. & Andrews, W. Congenital duodenal obstruction: timing of diagnosis during the newborn period. J Perinatol 30, 197–200 (2010). https://doi.org/10.1038/jp.2009.143
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2009.143
Keywords
This article is cited by
-
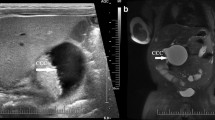
The application of prenatal ultrasound in the diagnosis of congenital duodenal obstruction
BMC Pregnancy and Childbirth (2020)
-
The value of saline-aided ultrasound in diagnosing congenital duodenal obstruction
Pediatric Surgery International (2020)
-
Diagnostic value of the acute angle between the prestenotic and poststenotic duodenum in neonatal annular pancreas
European Radiology (2019)
-
Laparoscopic diagnosis and treatment of neonates with duodenal obstruction associated with an annular pancreas: report of 11 cases
Surgery Today (2015)
-
Congenital duodenal obstruction in neonates: a decade’s experience from one center
World Journal of Pediatrics (2014)