Abstract
Objective:
To measure the neonatal mortality rate (NMR) and investigate its predictors in a rural area of Burkina Faso.
Study Design:
A cohort of infants born in 24 villages in Banfora region was followed until the children were 6 months old. We estimated the risk of neonatal death and used logistic regression to identify its predictors.
Result:
Among 864 live births followed to day 28, there were 40 neonatal deaths, a NMR of 46.3 per 1000 live births (95% confidence intervals (CI): 22 to 70). Multivariable regression identified twin birth (OR=11.5, 95%CI: 4.5 to 29.8), having a nulliparous mother (odds ratio (OR)=4.3, 95% CI: 1.5 to 12.1), and birth into a polygynous household (OR=2.1, 95% CI: 1.0 to 4.7) as main predictors of neonatal death.
Conclusion:
The burden of neonatal mortality in rural Burkina Faso is very high and the observed NMRs in a predominantly rural country suggest that it is unlikely Burkina will meet fourth Millennium Development Goal (MDG-4) by 2015.
Similar content being viewed by others
Introduction
With an estimated annual global burden ranging from 3.1 to 3.6 million deaths, high neonatal mortality remains a challenge for many low-income countries1, 2 and a major threat to the achievement of the fourth Millennium Development Goal (MDG-4) (see ref. 3, 4, 5). In 2009, UNICEF reported that the under-5 mortality rate (U5MR) in sub-Saharan Africa had reduced from 184 in 1990 to 144 per 1000 live births in 2008, a reduction of 22%, whereas the neonatal mortality rate (NMR) had gone from 41 in 1995 to 40 in 2004 per 1000, showing almost no reduction.6
Monitoring progress towards MDG-4 and the planning and implementation of efficient and effective health programs require reliable representative data from countries where the mortality burden is high. Several reports have called for improved estimates of NMRs in sub-Saharan Africa.3, 4, 7
In addition to demographic and health surveys (DHS) based on recall, some countries in sub-Saharan Africa have demographical surveillance sites (DSS), which provide prospective data on mortality trends in the absence of vital registration systems with high coverage.8, 9 In Burkina Faso, two DSS were established in the 1990s in the central and north-western parts of the country.10, 11, 12 However, reports from these DSS suggest under-ascertainment of deaths occurring during the neonatal period.13, 14 Other prospective studies that provide some data on neonatal deaths are restricted to urban populations15, 16 or other specific, atypical study populations17, 18, 19 and there is a lack of reliable prospective data on representative rural populations.
The PROMISE-EBF trial (http://www.clinicaltrials.gov NCT00397150) was a prospective community-based study implemented in four Sub-Saharan African countries including Burkina Faso, during which exclusive breastfeeding was promoted through individual peer counselling.20 This study provided an opportunity to measure the burden of neonatal mortality in a rural area in Burkina Faso and to study its predictors a few years before the 2015 deadline for MDG-4.
Methods
Setting
The study was carried out in Banfora Health District, in the south-west of Burkina Faso. The district covers an area of 15 000 km2 and consists of three administrative areas, Banfora, Soubakénédougou and Sidéradougou, respectively. The annual rainfall is 950 to 1250 mm.21 The population was 410 000 in 2006, dominated by the Gouin, Karaboro and Dioula ethnic groups.22 Farming and animal husbandry are the two main activities in rural areas, whereas the town of Banfora is a trading centre. The region is, relatively speaking, one of the wealthiest in the country.21 The district health care system comprises 60 primary health facilities and one regional hospital in Banfora town.
Study design
The PROMISE-EBF trial was a community-based cluster randomised trial performed in 24 villages from Banfora Health District and is described elsewhere.23 Children born to pregnant women enrolled into the trial were followed prospectively until they were 6 months old.
Sample size
On the basis of the previous estimates of NMR in Burkina Faso (32 per 1000),24 and for a confidence level of 95%, we estimated that a sample of 826 newborns would allow us to measure the NMR with a precision of ±1.2%. This sample size was achieved in the PROMISE-EBF trial.23
Recruitment, follow-up, data collection and main variables
In each study village two to five female ‘recruiters’ were selected and trained to identify all pregnant women through weekly household visits and to record information on pregnancy outcomes. Each month, up to four pregnant women were randomly selected from each village and invited to participate in this study. Women were eligible for the study, if they planned to live in the village for the next 12 months, were 7 months pregnant, intended to breastfeed their child, had no severe illness or known psychiatric disorder and gave written informed consent. Recruitment of pregnant women lasted 1 year from June 2006 to May 2007.
Five data collectors who spoke the main local dialects (Dioula and Gouin/Karaboro) were recruited and trained. They lived in the study area and received monthly supervisory visits. Home visits were performed by data collectors at recruitment and after birth, at day 7, weeks 3, 6, 12 and 24 (±7 days for each visit). Mothers who were not at home on scheduled visit days were revisited. Data were collected on handheld computers (PDAs) using electronic questionnaires with the Epihandy software (http://www.openXdata.org). For quality control purposes, 10 to 20% of the mothers were re-interviewed by the supervisors.
Information recorded at recruitment included the baseline characteristics of the mother. During follow-up, data on pregnancy outcomes, newborn characteristics, infant feeding and child growth were collected. Maternal height and the newborn's birth weight were taken from the antenatal care (ANC) card when available. Data collectors recorded dates of birth and death during weekly visits to each cluster. Infant weight was recorded in kg to the nearest 0.10 kg using Seca 872 scales and recumbent length was measured in cm to the nearest 0.5 cm using a Seca210 infantometer (http://www.seca.com). For multiple births, no data were collected on feeding patterns and growth.
The WHO standard neonatal verbal autopsy questionnaire25 was administered to the mother in the event of infant death, 4 to 6 weeks after the death to respect the mourning period in the area. The probable causes of death were assigned by two independent physicians using a hierarchical grouping adapted both from the Child Health Epidemiology Reference Group Classification26 and ICD-10 (see ref. 27). Multiple causes of death were allowed, although only the primary cause is reported here. The opinion of a senior pediatrician was sought in cases of disagreement between the two physicians.
Definitions
The WHO's standard definition of neonatal death (that is, the death of any live born infant within 28 days of his/her birth) and exclusive breastfeeding (that is, the child is given nothing other than breast milk, with minerals, vitamins and medicines allowed) were used.27, 28 Exclusive breastfeeding (EBF) status was based on ‘since birth’ dietary recall. Delivery with a skilled birth attendant refers to births attended by a nurse, a midwife or a doctor.
Anthropometric status was assessed using WHO's standards (http://www.who.int/childgrowth/en/). Children were classified as wasted, stunted or underweight, if their relevant z-score was below –2.
Data analysis
Data analysis was performed using Stata SE 11.0 (StataCorp LP, College Station, TX 77845, USA). All live births with known vital status at day 28 were included in the analyses.
We generated a relative wealth index as a proxy for socio-economic status based on data collected at recruitment on housing material (walls, floor, windows and roof) and household assets, such as possession of the following items: car/truck, motorcycle/scooter, bicycle, mobile phone/telephone, plough and chart. The index was constructed using principal component analysis.29
Summary statistics for the main outcomes were computed as proportions or means with 95% confidence intervals (CIs) based on robust standard errors to account for the cluster sampling of the PROMISE-EBF trial. Pearson chi-squared tests, correcting for the cluster sampling design, were used for between-group comparisons. The NMR per 1000 live births was calculated as the number of neonatal deaths, divided by the number of live births, multiplied by 1000. We assessed the between-cluster variation in NMR using random-effects logistic regression.
Predictors of neonatal death were screened through univariable random-effects logistic regression. Crude odds ratios (ORs) and their 95% CIs were obtained. To reduce the potential for reverse causality, the analysis of feeding covariates was restricted to singleton births, who survived either the first 24 h (for colostrum and time to initiation of breastfeeding) or the first 7 days (for the EBF status).
Multivariable analyses to identify predictors of neonatal deaths were developed following the model from Mosley and Chen.30 Only covariates that were associated with the outcome (P<0.05) after potential confounders were taken into account were retained. We paid particular attention to the potential association with feeding patterns based on reports from a previous study.31
Ethical and administrative clearances
This study was approved by the Institutional Review Board of Centre MURAZ (N°013/2005/CE-CM) and the Western Regional Committee for Medical and Health Research Ethics in Norway (Sak nr 05/8197). The study was authorised by the Ministry of Health of Burkina Faso.
Results
Study profile
Over 1 year, 1162 pregnant women were identified 21 of whom (1.8%) declined study participation upon initial contact. A total of 900 women were then randomly selected for data collection of whom 895 were eligible; all were enrolled and followed until delivery. These pregnancies resulted in 49 stillbirths and 866 live births, including 20 pairs of twins (2.3%). Vital status at 28 days of age was known for 864 newborns. One pair of twins was lost to follow-up after the first week and was excluded from the analyses.
Maternal and infant baseline characteristics
The mean age of the women was 26 years. Few women were nulliparous (16%) or literate (20%). Almost half of women (49%) lived in polygynous households and polygyny was associated with higher odds of multiparity (OR=5.7, 95% CI: 3.5 to 9.2), with a higher odds of belonging to the least poor two quintiles (OR=1.7, 95% CI: 1.3 to 2.3) and with a higher odds of an unskilled attendant at birth (OR=1.4, 95%CI: 1.1 to 1.9).
A total of 609 women attended at least one antenatal consultation of whom 365 (60%) had their height measured and 480 (79%) had a fundal height recorded. However, only 50 (8%) had the date of their last menstrual period recorded in their ANC card. Only 18% of women completed more than two ANC visits and 38% delivered with a skilled birth attendant (Table 1).
The proportion of women without any ANC visit varied within the study area, by season and by parity (Table 2). There was strong evidence that being of low parity and living near a facility were associated with a higher probability of a facility delivery. There was weaker evidence that living in a monogamous household and increasing maternal education were also associated with facility delivery. However, there was no evidence that socio-economic status, as assessed by asset ownership, was associated with facility delivery.
Birth weight was available for 295 newborns. In this subsample the mean birth weight (s.d.) was 2971 (527) g and 14% had a birth weight <2500 g. Two villages (Karfiguéla and Nafona1) showed a higher odds of low birth weight (OR=3.6, 95% CI: 2.0 to 6.3), but also had a higher odds of twin birth (OR=5.1, 95% CI: 2.0 to 12.8) as compared with other villages. Birth weight was positively correlated with parity (Spearman's coefficient=0.29, P<0.001) in this subsample.
Neonatal mortality outcomes
A total of 40 newborns had died by day 28, a NMR of 46.3 per 1000 (95% CI: 22 to 70). In all, 23 of these deaths (57%) occurred during the first week of life, an early NMR of 26.6 per 1000 (95% CI: 9 to 44). Six of the deaths occurred on the day of birth (15%), 8 (20%) occurred within 24 h. Moreover, 11 deaths (28%) were among twins, giving a NMR of 289 for twins compared with 35 for singleton births (P=0.0001).
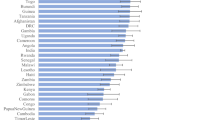
There was evidence that the NMR varied between villages (LR test, P=0.001). NMRs ordered by village reveal two villages, Karfiguéla and Nafona1 with very high-observed NMRs (214 and 250 per 1000, respectively). Both villages house a health facility.
Of the newborns who died, 5 (12%) were taken to the local health facility before death, 2 (5%) were taken to a local healer and 33 (83%) were either treated at home (8 received self-prescribed drugs) or did not receive any care before death (25 infants). In all, 36 (90%) of the deaths occurred at home, 3 (8%) in a health facility and 1 in a local healer's home.
The probable primary causes of neonatal death were birth asphyxia (1 case), complications of pre-term birth (17 cases), infections (7 cases), haemorrhage (1 case) and acute intestinal occlusion syndrome (2 cases). Cause of death could not be identified for 12 neonates.
Infant feeding patterns and anthropometric status at 3 weeks of age
The analysis of the early feeding behaviour in this cohort showed that 684 (90%) of the 764 singletons newborns who survived the first 24 h received colostrum. Five singleton newborns died before initiation of breastfeeding and four of these deaths occurred within 24 h of birth. Only 32 mothers of singletons (4%) initiated breastfeeding within 1 h of birth, whereas a further 371 (49%) did so within 12 h of birth. The proportion of singleton births reported to be EBF by 3 weeks of age was 54% (95% CI: 38 to 69).
Anthropometric data were only available for three of the neonates who died and therefore no useful comparison could be carried out with the survivors. The mean (95% CI) z-scores among newborns with anthropometric data at 3 weeks of age (n=715) were: WLZ=−0.88 (−1.1 to −0.7); LAZ=−0.64 (−0.77 to −0.52); WAZ=−0.96 (−1.07 to −0.85). The corresponding proportions of wasted, stunted and underweight newborns were 17% (95% CI: 13 to 22), 11% (95% CI: 9 to 13) and 16% (95% CI: 13 to 20), respectively.
Predictors of neonatal death
In univariable analyses, twin births had almost 10-fold increased (OR=9.7) odds of neonatal death (Table 1). Having an unskilled attendant at birth was associated with doubling (OR=2.3) in the odds of neonatal death. Living within 5 km of a health facility was unexpectedly associated with doubling in the odds of neonatal death (OR=2.1), although this was not significant (P=0.09). Nulliparous and high multiparae mothers had increased odds of neonatal death with ORs of 2.0 (95% CI: 0.8 to 4.8) and 1.8 (95% CI: 0.8 to 4.2), respectively, although the association was not statistically significant (P=0.15). No other variables examined, including maternal age, newborn's gender, time to initiation of breastfeeding, receiving colostrum, reported EBF-status by 3 weeks, had ORs of <0.5 or >2.0.
In multivariable regression, having a nulliparous mother (OR=4.3), being born in a polygynous household (OR=2.1), and being a twin (OR=11.5) were the factors associated with an increased odds of neonatal death (Table 1). Neither birth attendant (OR=2.1, 95% CI: 0.9 to 4.7), nor distance to health facility (OR=2.1, 95% CI: 0.9 to 4.8) after controlling for other factors, showed evidence that either of these variables were ‘significantly’ associated with the odds of neonatal death. Inclusion of the feeding covariates in a multivariable model did not provide any evidence that time to initiation of breastfeeding or administration of colostrum was associated with the odds of neonatal death (data not shown). Similar analyses using a Cox regression model were also performed and produced results similar to those obtained with the logistic model (data not shown).
Discussion
Estimates of neonatal mortality
We observed a high burden of neonatal mortality in this rural area in Burkina Faso. The NMR of 46.3 per 1000 is one of the highest ever reported from the country.
Our study is a rarity in Burkina Faso, being a community-based, prospective cohort study, which measured the burden of neonatal mortality in a rural area. The study participants were a random sample of pregnant women from 24 villages in the study area. The recruitment lasted exactly 1 year to capture any seasonal variation in maternal and newborn characteristics. The collaboration of local ‘recruiters’ with trained data collectors, the weekly household visits and the regular supervision of data collection and the low proportion of refusals (1.8%) should have resulted in data of high quality from a representative sample of eligible mothers.
However, a limitation of our study was its relatively small sample size, resulting in low power to detect risk factors associated with small increases in neonatal mortality risk. The high proportion of home deliveries meant few babies had birth weight measured and recorded. Most deaths occurred before 14 days, so that no anthropometric comparison of children who died with survivors at 3 weeks was possible. The possibility that some early neonatal deaths were misclassified as stillbirths cannot be excluded, with circumstantial evidence for such misclassification provided by the high stillbirth: early neonatal death ratio,23 the low proportion of neonatal deaths on day 0 (15%) and the fact that only one neonatal death out of 40 was attributed to birth asphyxia. If some of the stillbirths were actually live births who died shortly after delivery, then our estimate of NMR is an underestimate. Several studies have shown that for cultural and economic reasons, some early neonatal deaths may be reported as stillbirths.32, 33
In our study, the probable causes of deaths were dominated by complications of pre-term birth (42%) and infections (18%), differing from a Ghanaian study34 where infections (40.3%), birth asphyxia (33.2%) and pre-maturity (19.7%) were the major causes of neonatal deaths, and a recent meta-analysis showing that in sub-Saharan Africa, infections, pre-term birth complications and birth asphyxia are in decreasing order the main causes of neonatal deaths.1 Again the potential for misclassification and the proportion of deaths with undetermined causes (30%) could explain the observed difference.
One explanation for the high NMR observed in this study is likely to be the weak health system, with health facilities geographically inaccessible, poorly equipped where they exist, and offering a generally poor quality of health care35, 36, 37 In our study, only six villages (25%) had their own primary health facility and the one regional hospital that provides round-the-clock emergency obstetric care serves a population of over 400 000. The proportion of women delivering in a facility was higher in villages located within 5 km of the nearest health facility (56%). Surprisingly, the two villages with the highest observed NMRs both had a health facility (Karfiguéla and Nafona1), and had a higher proportion of facility deliveries than the average in this cohort. The high proportion of twin births and possibly the low birth weights in these two villages may partly explain their high NMRs. Nonetheless, another explanation could be the poor quality of health care offered in the health centres in general. In a recent study conducted in another rural district of Burkina Faso, the authors reported on the poor quality of antenatal and childbirth services.38 Understaffing, de-motivated health personnel and the attitude of health workers in the context of low literacy in rural areas are among the factors contributing to the poor quality in health services.38 Moreover, in rural settings, a proportion of deliveries classified as facility-based may actually have started at home and only been taken to the clinic when progress was slow, masking the expected benefits of delivering in a facility.24
The 2003-DHS reported that neonatal mortality was slightly higher in rural areas of Burkina Faso (NMR=39 per 1000) than in urban settings (NMR=35 per 1000), and a NMR of 50 per 1000 was reported in the region of Banfora, consistent with our results.24 The few longitudinal studies conducted in rural areas of Burkina report NMRs ranging from 94 to 350 per 1000 person-years, all in the DSS of Nouna.14, 39 These estimates are below ours when converted to neonatal deaths per 1000 live births. However, given the low proportion of neonatal deaths in one of the studies (6% of all child deaths), it seems they failed to identify many neonatal deaths.14 Another study conducted in Houndé region reported a somewhat lower NMR of 14.6 per 1000, but this was in the context of a randomised trial of micronutrient supplementation during pregnancy.40
Recent reports on overall child mortality trends in Burkina Faso5, 41 estimated the U5MR to be of 169 per 1000 in 2008 with a target of 68 in 2015. The average annual reduction rate for U5MR between 1990 and 2008 was of 1% (see ref. 5), and the authors concluded that this was insufficient to reach MDG-4 by 2015. Given that Banfora is among the wealthiest regions in Burkina and the high proportion of child deaths, which are neonatal (40%), achieving MDG-4 seems unlikely for Burkina based on our observation of a very high NMR in a rural area, of a largely rural population (>75%) (see ref. 22). A recent publication estimated the national NMR at 32 per 1000 in 2010 (see ref. 2) in Burkina. Our data collected in field up to August 2008 suggest that NMRs may be much higher than this in rural areas where 77% of the Burkina population lives.22 High NMRs have also been reported in Benin and Mali, both neighbours of Burkina Faso.42
Predictors of neonatal death
The multivariable analyses identified that nulliparous mothers, polygynous households and twin births are associated with increased odds of neonatal death.
Nulliparous mothers are at a higher risk of neonatal death because of the higher risk both of complicated and pre-term births in this group, the latter being a result of their higher vulnerability to certain infections such as malaria.43, 44
Our finding of increased risk of neonatal death in polygynous households is consistent with that of two previous studies.45, 46 In our study, polygyny was associated with higher odds of multiparity and of an unskilled attendant at birth, both of which were associated, albeit, weakly with increased odds of neonatal death. Previous studies have hypothesised polygyny may be associated with increased risk of death through resource constraints, lack of paternal investment and selectivity of the husband.47, 48
Multiple births including twins have been reported in several studies as being at a higher risk of neonatal death.3, 4, 34, 49 The high probability of pre-term birth and low birth weight are among the factors suggested to contribute to this poor outcome. The small proportion of babies with measured birth weights and the lack of reliable gestational age data are limitations, which preclude an investigation of the role of gestational age and intra-uterine growth retardation in this study.
We found some weak evidence that having an unskilled attendant at birth was associated with increased odds of neonatal death. Home delivery with an unskilled attendant may increase the risk of neonatal death through increased risk of birth asphyxia at birth and risk of sepsis during the neonatal period.3, 4, 34
We did not find any evidence of an association between the time to initiation of breastfeeding and risk of neonatal death in this study, although our cohort size means that we cannot exclude such an association. A larger study found an increased risk of infection-related neonatal death with delayed initiation of breastfeeding.31 The difference may also be due to the predominantly higher proportion of non-infectious causes of deaths found in our cohort.
The surprising, albeit weak, association of a shorter distance to the nearest health facility with increased odds of neonatal death was mainly because of the two villages with the highest NMRs, as confirmed by analyses that excluded these two clusters (data not shown). However, this observation may also reflect the poor quality of care provided in facilities and underlines that the presence of a health facility itself may not be enough, especially given the recurrent absences of the health personnel. Our findings oppose to that reported in a previous study in Burkina, in which the outcome was rather infant death,50 and show the need of further understanding of the concept of distance.51
Conclusion
The burden of neonatal mortality is high in this rural area of Burkina Faso. With such high NMRs and the high proportion of population living in those areas and the current progress in the reduction of overall child deaths, it is unlikely that Burkina Faso will meet the MDG-4 by 2015. Our findings call for increased health facility access and improved quality of care in childbirth services in rural areas of this country. Primigravidae and mothers of multiple births may require greater attention in the peripartum, and further studies are needed to understand the social determinants of neonatal deaths.
References
Black RE, Cousens S, Johnson HL, Lawn JE, Rudan I, Bassani DG et al. Global, regional, and national causes of child mortality in 2008: a systematic analysis. Lancet 2010; 375 (9730): 1969–1987.
Rajaratnam JK, Marcus JR, Flaxman AD, Wang H, Levin-Rector A, Dwyer L et al. Neonatal, postneonatal, childhood, and under-5 mortality for 187 countries, 1970–2010: a systematic analysis of progress towards Millennium Development Goal 4. Lancet 2010; 375 (9730): 1988–2008.
Lawn JE, Cousens S, Zupan J . 4 million neonatal deaths: when? Where? Why? Lancet 2005; 365 (9462): 891–900.
Lawn JE, Kerber K, Enweronu-Laryea C, Massee Bateman O . Newborn survival in low resource settings—are we delivering? BJOG 2009; 116 (Suppl 1): 49–59.
Bhutta AZ, Chopra M, Axelson H, Berman P, Boerma JT, Bryce J et al. Countdown to 2015 decade report (2000–10): taking stock of maternal, newborn, and child survival. Lancet 2010; 375: 2032.
UNICEF. The State of the World's Children: Celebrating 20 years of the Convention on the rights of the child. UNICEF: New York (USA), 2009.
World Health Organization. Neonatal and Perinatal mortality: Country, Regional and Global estimates 2004. WHO: Geneva, 2007.
Abdullah S, Adazu K, Masanja H, Diallo D, Hodgson A, Ilboudo-Sanogo E et al. Patterns of age-specific mortality in children in endemic areas of sub-Saharan Africa. Am J Trop Med Hyg 2007; 77 (6 Suppl): 99–105.
Ndugwa RP, Ramroth H, Muller O, Jasseh M, Sie A, Kouyate B et al. Comparison of all-cause and malaria-specific mortality from two West African countries with different malaria transmission patterns. Malar J 2008; 7: 15.
Diallo DA, Cousens SN, Cuzin-Ouattara N, Nebie I, Ilboudo-Sanogo E, Esposito F . Child mortality in a West African population protected with insecticide-treated curtains for a period of up to 6 years. Bull World Health Organ 2004; 82 (2): 85–91.
Hammer GP, Kouyate B, Ramroth H, Becher H . Risk factors for childhood mortality in sub-Saharan Africa. A comparison of data from a Demographic and Health Survey and from a Demographic Surveillance System. Acta Trop 2006; 98 (3): 212–218.
Kynast-Wolf G, Sankoh OA, Gbangou A, Kouyate B, Becher H . Mortality patterns, 1993–98, in a rural area of Burkina Faso, West Africa, based on the Nouna demographic surveillance system. Trop Med Int Health 2002; 7 (4): 349–356.
Diallo DA, Habluetzel A, Esposito F, Cousens SN . Comparison of two methods for assessing child mortality in areas without comprehensive registration systems. Trans R Soc Trop Med Hyg 1996; 90 (6): 610–613.
Hammer GP, Some F, Muller O, Kynast-Wolf G, Kouyate B, Becher H . Pattern of cause-specific childhood mortality in a malaria endemic area of Burkina Faso. Malar J 2006; 5: 47.
Koueta F, Dao L, Ye D, Zoungrana A, Kabore A, Sawadogo A . Risk factors for death from severe malaria in children at the Charles de Gaulle pediatric hospital of Ouagadougou (Burkina Faso). Sante 2007; 17 (4): 195–199.
Koueta F, Ye D, Dao L, Neboua D, Sawadogo A . Neonatal morbidity and mortality in 2002–2006 at the Charles de Gaulle pediatric hospital in Ouagadougou (Burkina Faso). Sante 2007; 17 (4): 187–191.
Filippi V, Ganaba R, Baggaley RF, Marshall T, Storeng KT, Sombie I et al. Health of women after severe obstetric complications in Burkina Faso: a longitudinal study. Lancet 2007; 370 (9595): 1329–1337.
Kabore P, Potvliege C, Sanou H, Bawhere P, Dramaix M . Growth velocity and survival of full-term low birth weight infants in an African rural area (Burkina Faso). Arch Pediatr 2004; 11 (7): 807–814.
Koueta F, Ye D, Dao L, Zoungrana-Kabore A, Ouedraogo SA, Napon M et al. Lung disease and HIV infection in children at the Charles de Gaulle university pediatric hospital center in Ouagadougou (Burkina Faso). Sante 2008; 18 (1): 15–18.
Nankunda J, Tumwine JK, Soltvedt A, Semiyaga N, Ndeezi G, Tylleskar T . Community based peer counsellors for support of exclusive breastfeeding: experiences from rural Uganda. Int Breastfeed J 2006; 1: 19.
INSD MEF/Burkina Faso. Annuaire Statistique 2008 de la Region des Cascades (Statistics of the Cascades Region in 2008). MEF/INSD: Ouagadougou (Burkina Faso), 2008.
INSD MEF/Burkina Faso. Recensement General de la Population et de l'Habitat, 2006 (General Population Census, 2006). MEF/INSD: Ouagadougou (Burkina Faso), 2009.
Diallo AH, Meda N, Zabsonré E, Sommerfelt H, Cousens S, Tylleskar T . Perinatal mortality in rural Burkina Faso: a prospective community-based cohort study. BMC Pregnancy Childbirth 2010; 10 (45): 1–9.
Institut National de Statistique et de la Démographie (INSD) et ORC Macro. Enquête Démographique et de Santé du Burkina Faso 2003 (DHS). Calverton, Maryland (USA), 2004.
World Health Organization. Standard neonatal verbal autopsy questionnaire Revised version. WHO Publications: Geneva (Switzerland), 2003.
Winbo IG, Serenius FH, Dahlquist GG, Kallen BA . NICE, a new cause of death classification for stillbirths and neonatal deaths. Neonatal and Intrauterine Death Classification according to Etiology. Int J Epidemiol 1998; 27 (3): 499–504.
World Health Organization. International statistical classification of diseases and related health problem, 10th revision (ICD-10). WHO: Geneva, 2007.
Kramer MS, Kakuma R . Optimal duration of exclusive breastfeeding. Cochrane Database Syst Rev 2002; (1): CD003517.
Kolenikov S, Angeles G . Socioeconomic status measurement with discrete proxy variables: is principal component analysis a reliable answer? Rev Income and Wealth 2009; Series 55 (March 2009): 128.
Mosley WH, Chen LC . An analytical framework for the study of child survival in developing countries. 1984. Bull World Health Organ 2003; 81 (2): 140–145.
Edmond KM, Kirkwood BR, Amenga-Etego S, Owusu-Agyei S, Hurt LS . Effect of early infant feeding practices on infection-specific neonatal mortality: an investigation of the causal links with observational data from rural Ghana. Am J Clin Nutr 2007; 86 (4): 1126–1131.
Lawn JE, Yakoob MY, Haws RA, Soomro T, Darmstadt GL, Bhutta ZA . 3.2 million stillbirths: epidemiology and overview of the evidence review. BMC Pregnancy Childbirth 2009; 9 (Suppl 1):: S2.
Spector JM, Daga S . Preventing those so-called stillbirths. Bull World Health Organ 2008; 86 (4): 315–316.
Edmond KM, Quigley MA, Zandoh C, Danso S, Hurt C, Owusu Agyei S et al. Aetiology of stillbirths and neonatal deaths in rural Ghana: implications for health programming in developing countries. Paediatr Perinat Epidemiol 2008; 22 (5): 430–437.
Direction des Etudes et de la Planification (DEP/MS). Annuaire Statistique Santé (Health Statistics Book)-Edition 2008. Official publication. Ouagadougou (Burkina Faso): MS/DEP, 2009.
Graham WJ, Conombo SG, Zombre DS, Meda N, Byass P, De Brouwere V . Undertaking a complex evaluation of safe motherhood in rural Burkina Faso. Trop Med Int Health 2008; 13 (Suppl 1): 1–5.
Hounton S, Chapman G, Menten J, De Brouwere V, Ensor T, Sombie I et al. Accessibility and utilisation of delivery care within a Skilled Care Initiative in rural Burkina Faso. Trop Med Int Health 2008; 13 (Suppl 1): 44–52.
Nikiema L, Kameli Y, Capon G, Sondo B, Martin-Prevel Y . Quality of antenatal care and obstetrical coverage in rural Burkina Faso. J Health Popul Nutr 2010; 28 (1): 67–75.
Benzler J, Sauerborn R . Rapid risk household screening by neonatal arm circumference: results from a cohort study in rural Burkina Faso. Trop Med Int Health 1998; 3 (12): 962–974.
Roberfroid D, Huybregts L, Lanou H, Henry MC, Meda N, Menten J et al. Effects of maternal multiple micronutrient supplementation on fetal growth: a double-blind randomized controlled trial in rural Burkina Faso. Am J Clin Nutr 2008; 88 (5): 1330–1340.
Bryce J, Daelmans B, Dwivedi A, Fauveau V, Lawn JE, Mason E et al. Countdown to 2015 for maternal, newborn, and child survival: the 2008 report on tracking coverage of interventions. Lancet 2008; 371 (9620): 1247–1258.
Bryce J, Gilroy K, Jones G, Hazel E, Black RE, Victora CG . The Accelerated Child Survival and Development programme in west Africa: a retrospective evaluation. Lancet 2010; 375 (9714): 572–582.
Haws RA, Yakoob MY, Soomro T, Menezes EV, Darmstadt GL, Bhutta ZA . Reducing stillbirths: screening and monitoring during pregnancy and labour. BMC Pregnancy Childbirth 2009; 9 (Suppl 1): S5.
Steketee RW, Wirima JJ, Hightower AW, Slutsker L, Heymann DL, Breman JG . The effect of malaria and malaria prevention in pregnancy on offspring birthweight, prematurity, and intrauterine growth retardation in rural Malawi. Am J Trop Med Hyg 1996; 55 (1 Suppl): 33–41.
Amey FK . Polygyny and child survival in West Africa. Soc Biol 2002; 49 (1–2): 74–89.
Ukwuani AF, Cornwell TG, Suchindran MC . Polygyny and child survival in Nigeria: age-dependant effects. J Popul Res 2002; 19 (2): 17.
Gyimah SO . Polygynous marital structure and child survivorship in sub-Saharan Africa: some empirical evidence from Ghana. Soc Sci Med 2009; 68 (2): 334–342.
Strassmann BI . Polygyny as a risk factor for child mortality among the Dogon. Current Anthropology 1997; 38 (4): 7.
Jahn A, Kynast-Wolf G, Kouyate B, Becher H . Multiple pregnancy in rural Burkina Faso: frequency, survival, and use of health services. Acta Obstet Gynecol Scand 2006; 85 (1): 26–32.
Becher H, Muller O, Jahn A, Gbangou A, Kynast-Wolf G, Kouyate B . Risk factors of infant and child mortality in rural Burkina Faso. Bull World Health Organ 2004; 82 (4): 265–273.
Rutherford ME, Mulholland K, Hill PC . How access to health care relates to under-five mortality in sub-Saharan Africa: systematic review. Trop Med Int Health 2010; 15 (5): 508–519.
Acknowledgements
We would like to address our sincere thanks to all mothers who enrolled in this study for their participation and patience during interviews. We are also grateful to the local ‘recruiters’ in the 24 villages of the Banfora Health District, the five data collectors and the supervisors for their efforts. We acknowledge the contribution of Dr Germain Traoré (Medical officer at the Regional Health Directorate of Hauts-Bassins in Bobo-Dioulasso), Dr Abdoulaye Bara (Director of the Regional Health Directorate of Cascades in Banfora) and Dr Auguste Bicaba (Head of Banfora Health District) for their tireless efforts during the field implementation of the PROMISE-EBF study. Funding source: The PROMISE-EBF study was funded by the European Commission Framework Programme-6 under the contract INCO-CT-2004–003660. The sponsor had no responsibility in the design, conduct, analysis, interpretation or publication of the data.
Author contributions
AHD, NM and TT have designed the study. AHD conducted the study, performed data analyses and drafted the manuscript. WTO contributed to data collection. SC supervised the overall data analyses. SC, NM, WTO and TT contributed to interpretation of the findings.
All authors read and approved the final manuscript.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Appendix
Appendix
The Promise-EBF study group
List of members for the PROMISE-EBF study Group
Steering Committee:
Thorkild Tylleskär, Philippe Van de Perre, Eva-Charlotte Ekström, Nicolas Meda, James K. Tumwine, Chipepo Kankasa, Debra Jackson.
Participating countries and investigators:
Norway: Thorkild Tylleskär, Ingunn MS Engebretsen, Lars Thore Fadnes, Eli Fjeld, Knut Fylkesnes, Jørn Klungsøyr, Anne Nordrehaug-Åstrøm, Øystein Evjen Olsen, Bjarne Robberstad, Halvor Sommerfelt
France: Philippe Van de Perre
Sweden: Eva-Charlotte Ekström, Barni Nor
Burkina Faso: Nicolas Meda, Abdoulaye Hama Diallo, Thomas W. Ouédraogo, Jeremi Rouamba, Bernadette Traoré, Germain Traoré, Emmanuel Zabsonré
Uganda: James K. Tumwine, Caleb Bwengye, Charles Karamagi, Victoria Nankabirwa, Jolly Nankunda, Grace Ndeezi, Margaret Wandera
Zambia: Chipepo Kankasa, Mary Katepa-Bwalya, Chafye Siuluta, Seter Siziya
South Africa: Debra Jackson, Mickey Chopra, Mark Colvin, Tanya Doherty, Ameena E Goga, Lungiswa Nkonki, David Sanders, Wesley Solomons Wanga Zembe.
Rights and permissions
This work is licensed under the Creative Commons Attribution-NonCommercial-No Derivative Works 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Diallo, A., Meda, N., Ouédraogo, W. et al. A prospective study on neonatal mortality and its predictors in a rural area in Burkina Faso: Can MDG-4 be met by 2015?. J Perinatol 31, 656–663 (2011). https://doi.org/10.1038/jp.2011.6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2011.6
Keywords
This article is cited by
-
Determinants of early neonatal mortality (hospital based retrospective cohort study in Somali region of Ethiopia)
Scientific Reports (2023)
-
Incidence and predictors of neonatal mortality among neonates admitted in Amhara regional state referral hospitals, Ethiopia: prospective follow up study
BMC Pediatrics (2020)
-
Neonatal mortality in the neonatal intensive care unit of Debre Markos referral hospital, Northwest Ethiopia: a prospective cohort study
BMC Pediatrics (2020)
-
Predictors of Neonatal mortality in Neonatal intensive care unit at referral Hospital in Southern Ethiopia: a retrospective cohort study
BMC Pregnancy and Childbirth (2019)
-
The effect of antenatal care follow-up on neonatal health outcomes: a systematic review and meta-analysis
Public Health Reviews (2018)