Abstract
Anxiety disorders are a diverse group of clinical states. Post-traumatic stress disorder (PTSD) and generalized anxiety disorder (GAD), eg, share elevated anxiety symptoms, but differ with respect to fear-related memory dysregulation. As the hippocampus is implicated in both general anxiety and fear memory, it may be an important brain locus for mapping the similarities and differences among anxiety disorders. Anxiety and fear also functionally associate with different subdivisions of the hippocampus along its longitudinal axis: the human posterior (rodent dorsal) hippocampus is involved in memory, through connectivity with the medial prefrontal-medial parietal default-mode network, whereas the anterior (rodent ventral) hippocampus is involved in anxiety, through connectivity with limbic-prefrontal circuits. We examined whether differential hippocampal network functioning may help account for similarities and differences in symptoms in PTSD and GAD. Network-sensitive functional magnetic resonance imaging-based resting-state intrinsic connectivity methods, along with task-based assessment of posterior hippocampal/default-mode network function, were used. As predicted, in healthy subjects resting-state connectivity dissociated between posterior hippocampal connectivity with the default-mode network, and anterior hippocampal connectivity to limbic-prefrontal circuitry. The posterior hippocampus and the associated default-mode network, across both resting-state connectivity and task-based measures, were perturbed in PTSD relative to each of the other groups. By contrast, we found only modest support for similarly blunted anterior hippocampal connectivity across both patient groups. These findings provide new insights into the neural circuit-level dysfunctions that account for similar vs different features of two major anxiety disorders, through a translational framework built on animal work and carefully selected clinical disorders.
Similar content being viewed by others
INTRODUCTION
Our understanding of neural circuit abnormalities underlying anxiety disorders in humans has greatly benefitted from work in experimental animals, which has emphasized dysregulation of limbic and prefrontal regions. Animal work has also implicated the hippocampus in both memory, including fear extinction and reconsolidation (Corcoran et al, 2005; Debiec et al, 2002; Myers and Davis, 2002), as well as endogenous anxiety and avoidance behaviors (Bannerman et al, 2003; Kjelstrup et al, 2002), which are considered core symptom of anxiety disorders in general (American Psychiatric Association, 1994). Fanselow and Dong (2010), building on prior animal work (Moser and Moser, 1998), have furthermore shown that the hippocampus can be split into three discrete subdivisions along its longitudinal axis, based on the patterns of gene expression and anatomical connectivity.
In rodents, the dorsal third of the hippocampus (corresponding to the posterior hippocampus in primates (Amaral, 1987; Moser and Moser, 1998; Sasaki et al, 2004)) is involved in memory storage, through projections to cortical structures involved in memory (eg, anterior cingulate cortex and retrosplenial cortex (posterior cingulate cortex (PCC) in primates)) (Buckner et al, 2008; Cenquizca and Swanson, 2007; Squire, 1992). By contrast, in rodents the ventral third (anterior in primates (Amaral, 1987; Moser and Moser, 1998; Sasaki et al, 2004)) is involved in endogenous anxiety, through connections with the amygdala (Cenquizca and Swanson, 2007; Kishi et al, 2006), the bed nucleus of the stria terminalis (Cenquizca and Swanson, 2006), striatum, and the prelimibic and infralimbic areas of the medial prefrontal cortex that lie ventral to the anatomical targets of the dorsal hippocampus (ie, anterior cingulate cortex) (Groenewegen et al, 1996; Parent et al, 2010). As such, the hippocampus may be an important brain locus for understanding the similarities and differences among anxiety disorders.
Anxiety disorders are a diverse group of clinical conditions that share a set of core symptoms commonly associated with fear or anxiety, but also differ in important fear/anxiety-relevant ways (American Psychiatric Association, 1994). For example, both post-traumatic stress disorder (PTSD) and generalized anxiety disorder (GAD) share an elevated level of anxiety or general distress, but only PTSD involves persistent and intrusive fear-based memories. Our current neurobiological understanding of how neural circuit-level abnormalities account for these similar vs different symptoms, however, exists at only a rudimentary level.
In line with the rodent work, Poppenk and Moscovitch (2011) found in healthy humans that the posterior hippocampus is preferentially involved in recollection memory, through its connection with the default-mode network, which includes the pregenual anterior cingulate cortex (pgACC), PCC, and precuneus. This observation is consistent more generally with the involvement of the default-mode network in memory (Buckner et al, 2008). Moreover, abnormalities in the default-mode network have been found in patients with PTSD (Bluhm et al, 2009; Sripada et al, 2012b; Yin et al, 2011).
These findings in healthy subjects and patients with PTSD suggest that hippocampal interactions with the default-mode network may be an important basis on which to compare PTSD and GAD—a disorder in which no work has yet examined the hippocampus or the default-mode network. Moreover, studies of both PTSD and GAD have implicated abnormalities in amygdala connectivity (Etkin et al, 2009; Rabinak et al, 2011; Sripada et al, 2012a), which may be more closely related to the anterior hippocampus. Direct functional neuroimaging comparisons of PTSD with any other psychiatric disorder, however, are still extremely rare (Etkin and Wager, 2007). We are aware of only a single small study comparing PTSD (N=8) with another anxiety disorder (panic disorder; N=8), which was done using fear conditioning (Tuescher et al, 2011). Thus, with respect to either posterior or anterior hippocampal network functioning, a critical question remains whether PTSD and GAD have a similar deficit, or display dissociable abnormalities.
We therefore examined two hypotheses regarding PTSD and GAD: (1) given the common elevated level of general anxiety and depression in these disorders, both patient groups would differ similarly from healthy subjects but not from each other (‘common deficit’). This hypothesis is also supported by studies on symptom structure and emotion-modulated acoustic startle, which have shown that these disorders can be described by a common ‘anxious-misery’ symptom factor and are associated with similar disruptions in defensive responding, respectively (McTeague and Lang, 2012; Watson, 2005). Alternatively, (2) because of the existence of PTSD-specific (ie, fear memory-related) symptoms beyond the common elevated general anxiety and depression, PTSD patients would be distinguishable from GAD patients in terms of disrupted hippocampal network function (‘disorder-specific deficit’).
To test these hypotheses in a similar manner for the posterior and anterior hippocampus, we used resting-state functional connectivity analyses of functional magnetic resonance imaging (rs-fcMRI) scans to examine connectivity patterns of the posterior and anterior hippocampus in patients with PTSD or GAD, as well as a healthy control sample. To corroborate rs-fcMRI abnormalities within the default-mode network in particular, we examined task-independent deactivation during two unrelated task paradigms in these groups. This task-based analysis took advantage of the long-standing observation that the default-mode network deactivates, in a task-independent manner, during any attention-demanding task (compared with a rest period), and thus helps address potential shortcomings of rs-fcMRI related to the unconstrained nature of resting scans. Consistent with our conceptual framing above, we tested our first hypothesis (common deficit) by contrasting connectivity and deactivation in healthy subjects against the combination of both patient groups. For the second hypothesis (disorder-specific deficit), we contrasted the PTSD and GAD groups, in comparison with healthy subjects as a secondary analysis.
MATERIALS AND METHODS
Subjects
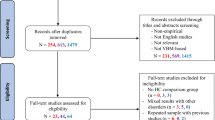
One-hundred and sixteen subjects participated in this study, including 17 patients with PTSD, 39 with GAD, and 60 healthy subjects (split into a 22-subject and a 38-subject cohort). The latter healthy cohort and the two patient groups were of similar age and education (Table 1), whereas the first cohort was used in a set of independent analyses to define a priori rs-fcMRI regions of interest (ROIs) for hippocampal connectivity. Psychiatric diagnoses based on the DSM-IV were determined using the structured diagnostic Mini-International Neuropsychiatric Interview (American Psychiatric Association, 1994; Sheehan et al, 1998). General exclusion criteria included a history of a neurological disorder, head trauma or loss of consciousness, claustrophobia, and regular use of benzodiazepines, opiates, thyroid medications, or other CNS medication. Both healthy cohort groups were free of any current or past Axis I conditions and were not taking psychiatric medications. Specific exclusion criteria for the patient groups were bipolar, psychosis, and substance abuse disorders. No GAD patient had PTSD, and no PTSD patient had GAD (see Supplementary Materials for other diagnoses, as well as index traumas for the PTSD group). All subjects completed a set of general mood and anxiety symptom scales (Beck and Steer, 1993; Beck et al, 1996; Spielberger et al, 1970; Watson et al, 1995).
Of the 17 patients with a primary PTSD diagnosis, 4 were taking psychiatric medications and 12 had comorbid MDD (71%). Of the 39 GAD patients, none were taking psychiatric medications and 23 had comorbid MDD (59%). There was no difference in the proportion of patients with comorbid MDD in the two cohorts (χ2=0.68, p=0.41). In addition, no subject took benzodiazepine within 48 h of the scan. Because accounting for medication status in the four PTSD patients did not alter our findings, we included all subjects in the analyses.
MRI Data Acquisition
General scan parameters
Imaging was performed on a 3T GE Signa Excite scanner (General Electric, Milwaukee, Wisconsin) at Stanford. We acquired 29 axial slices (4-mm slice thickness) covering the whole brain, using a T2-weighted gradient-echo spiral-pulse sequence (repetition time, 2000 ms; echo time, 30 ms; flip angle, 80°; field of view, 22 cm; matrix size, 64 × 64; and 1 interleave) (Glover and Lai, 1998). An automated high-order shimming method based on spiral acquisitions was used before acquiring fMRI scans (Kim et al, 2002) in order to reduce blurring and signal loss arising from field inhomogeneities.
Resting-state scan
All subjects underwent an 8-min (240 volumes) resting-state fMRI scan. Subjects were instructed to hold still and remain awake with their eyes closed. No subject fell asleep.
Task-independent deactivation task 1: flashing checkerboards
Subjects viewed a 1-s presentation of a 10-Hz counter-flashing checkerboard pattern, pressing a finger when the checkerboard appeared. Checkerboards were separated by a fixation cross with random duration of 8–12 s. One-hundred and sixty-eight volumes were collected for each subject. Because of technical or scan-timing difficulties, there were no data for one healthy subject and two PTSD patients.
Task-independent deactivation task 2: emotional faces
Subjects viewed facial expressions that were artificially colorized (red, yellow, and blue), and were instructed to indicate color of each faces by button press (Etkin et al, 2004). Faces were presented in 20-s blocks, with 20 s of rest (fixation cross). There were four different types of block: fearful, neutral, backwardly masked fearful, and backwardly masked neutral. Color of the faces varied randomly within block (288 volumes total). Because of technical or scan-timing difficulties, there were no data for one healthy subject and one PTSD patient.
Structural scan
A high-resolution T1-weighted SPGR MRI sequence was used with the following parameters: TI=300 ms, TR=8 ms, TE=3.6 ms, flip angle=15o, 22 cm field of view, 124 slices in coronal plane, 256 × 192 matrix, 2 NEX, and acquired resolution=1.5 × 0.9 × 1.1 mm3.
fMRI Data Preprocessing
All data were preprocessed with the common procedures described below. A linear shim correction was applied separately for each slice during reconstruction using a magnetic field map acquired automatically by the pulse sequence at the beginning of the scan (Glover and Lai, 1998). Functional images were preprocessed using SPM8 software (http://www.fil.ion.ucl.ac.uk/spm) in MATLAB (Mathworks, Massachusetts). Images were realigned, slice-timing corrected, spatially normalized to the Montreal Neurologic Institute template (Friston et al, 1995), resampled every 2 mm, and smoothed with a 6-mm full-width half-maximum Gaussian kernel. No participants had movement >3 mm of translation or 3° of rotation. Resting-state scans were bandpass filtered (0.008–0.1 Hz) (Cordes et al, 2001). For activation task scans, only low-frequency signal drift was removed (high-pass temporal filter; 128 s cutoff).
fMRI Data Analysis
Resting-state functional connectivity analysis
Seed ROIs were constructed, in MNI space, from maximum probability maps (MPMs) defined through the Anatomy Toolbox in SPM8 (Eickhoff et al, 2005), which are based on postmortem cytoarchitectonic mapping of 10 human brains and subsequent transformation to MNI space. Voxels were only included in the hippocampus MPM (including CA1-4 and the dentate gyrus) if the probability of their being assigned to the hippocampus was higher than to other nearby temporal lobe structures, and furthermore had a minimum of 60% likelihood of being in the hippocampus (Amunts et al, 2005) (to decrease type 1 error). Importantly, we also excluded any voxels that have any probability of being in the amygdala. This prevented any possibility that anterior hippocampus connectivity may partially reflect amygdala connectivity. Subsequently, the hippocampus MPMs from both hemispheres were further divided, along the A–P axis, into three equal sections (y=−10 to −21 mm, y=−21 to −32 mm, and y=−32 to −43 mm; Figure 1) in a way that is broadly consistent with the rodent gene expression findings that motivated this study (Fanselow and Dong, 2010).
Illustration of the seed regions of interest (ROI). Bilateral anterior and posterior hippocampal subdivisions (see arrows) were used in the functional connectivity analyses. Notably, we excluded voxels with any probability of being in the amygdala (black) from the anterior hippocampus ROI.
The resting-state seed-based functional connectivity analyses were performed using a previously published method (Etkin et al, 2009). In brief, each extracted time series was put into first-level fixed-effects general linear model in SPM8, which also included several covariates controlling for the global signal and six motion parameters. Four separate connectivity analyses were conducted for each subject, using a different time series extracted from one of the four seed ROIs (right/left × anterior/posterior). Contrast images corresponding to the ROI time-series regressor were derived for each ROI in each subject.
Group effects for the independent healthy cohort were thresholded at p=0.05 with a minimal cluster size of 10 voxels (uncorrected; see Supplementary Figure 1), the results of which were used only to identify differential connectivity ‘targets’ of the hippocampus subdivisions (ie, regions that showed greater relative anterior or posterior hippocampal connectivity), which could be used as a functional mask for subsequent analyses. This analysis allowed us to create functionally relevant ROIs in the most unbiased manner possible. These connectivity targets were further anatomically constrained to gray matter in conjunction with the WFU PickAtlas toolbox (Maldjian et al, 2003). Extractions involved averaging across all voxels within the ROI.
Task-independent deactivation task data analysis
Data from the flashing checkerboard task and emotional face task were also analyzed in SPM8. First-level fixed-effect general linear models were run separately for each task. Each model included regressors that code for all task conditions (convolved with a canonical HRF) within each task, with motion parameters as nuisance regressors. As described above, it is well established that the deactivation of default-mode network occurs reliably across a wide variety of task contexts (Buckner et al, 2008). To characterize this task-independent deactivation, we therefore examined the main effect of task for each model by creating contrast images that correspond to the regressors of interest (ie, any active task condition (vs implicit baseline, periods with a fixation cross)). From the contrast images, we then extracted mean beta values within each ROI, as defined above. We then averaged the mean beta values across the two separate tasks for each subject, further generalizing the measure of task-independent deactivation.
To supplement the a priori ROI analysis, we also entered the fixed-effect contrast images into a second-level random-effect analysis with whole-brain voxel-wise analysis of variance (ANOVA) (three-level between-group factor: healthy, PTSD, and GAD; two-level within-subject factor: checkerboard task and emotional face task) (Supplementary Figure 2c).
Structural Data Analysis
Voxel-based morphometry (VBM) was performed using the VBM8 toolbox for SPM8 (http://dbm.neuro.uni-jena.de/vbm/download/). The individual T1-weighted images from all subjects were first segmented into gray matter, white matter, and CSF using a unified segmentation routine through the toolbox (Ashburner and Friston, 2005). The segmented, modulated gray matter images were then smoothed at 6 mm full-width half-maximum (Ashburner and Friston, 2000). The volumes of interest corresponding to gray matter volume (modulated images) were extracted for the anterior and posterior hippocampus ROIs on both sides for statistical analyses.
Statistical Analyses
ANOVAs and t-tests (after running Levene’s test of the equality of variance) on the extracted beta values were conducted using SPSS 18 (SPSS, Chicago, IL). To test the ‘common deficit hypothesis’, we modeled the ANOVAs with a three-level between-subject factor ‘group’ (healthy, PTSD, and GAD) and a three-level within-subject factor ‘ROI’ (amygdala, striatum, and dorsal anterior cingulate cortex (dACC)/pre-supplementary motor area (pre-SMA) for anterior hippocampal connectivity targets; PCC, pgACC, and precuneus for posterior hippocampal connectivity targets (also used in task-independent deactivation analysis)). We then created contrasts reflecting the ‘patient status effect’ (healthy>PTSD and GAD; (2, −1, and −1) for the ‘group’ factor). By modeling the PTSD and GAD groups separately, rather than as a single patient group (ie, two-level between-subject factor ‘group’ (healthy and patients)), we were able to separately model the variance associated with each anxiety disorder group, as these groups had different sample sizes. To test the ‘disorder-specific deficit hypothesis’, similar ANOVAs were modeled, except that the between-subject factor ‘group’ was instead with two-level only (eg, PTSD and GAD). As such, the ANOVA main effect of ‘group’ reflected the comparison between disorders.
We also conducted several analyses to rule out a potential confounding effect of motion on resting-state connectivity (see Supplementary Materials) (Power et al, 2012; Van Dijk et al, 2012).
RESULTS
Reproducible and Dissociable Functional Connectivity of Hippocampus Subdivisions
We began by examining the dissociability of anterior and posterior hippocampus connectivity in rs-fcMRI scans in healthy subjects. Figure 2a shows (voxel-wise analyses, FDR q<0.05) the preferential functional connectivity of the posterior and anterior hippocampal subdivisions in our patient-comparison healthy cohort, using a priori target masks determined in a separate group of healthy subjects (see masks in Supplementary Figure 1). The posterior hippocampus was preferentially connected to the default-mode network, including the pgACC, PCC, and precuneus. The anterior subdivision was preferentially connected to bilateral amygdala, striatum, and an extended region spanning across dACC, pre-SMA, and the dorsal medial prefrontal cortices (dMPFCs), as well as the precentral gyrus and small regions in the temporal lobe. Likewise, when we used masks comprising the entire anterior or posterior hippocampus target maps derived from the independent healthy subjects as seed ROIs for our patient-comparison healthy cohort, voxel-wise analyses (FDR q<0.05) in the hippocampus revealed that the targets of each subdivision were preferentially connected with the expected portion of the hippocampus in healthy subjects (Figure 2b). These findings provide further support for the dissociability of functional connectivity from the anterior and posterior thirds of the hippocampus (and hence our choice of these ROIs).
Dissociable neural circuits within the human hippocampus revealed by resting-state functional connectivity. (a) Distinct connectivity profiles of the anterior and posterior hippocampus in humans mirrored anatomical connectivity of the ventral and dorsal hippocampus in experimental animals. Although the anterior hippocampus was preferentially connected to subcortical limbic structures and dorsal anterior cingulate cortex (dACC)/pre-supplementary motor area (pre-SMA) (blue), the posterior hippocampus was more connected to the memory-related default-mode network (red). Displays are in neurological convention. MNI x-coordinates of the sagital slices on the top row are: −26, −13, −6, −3, and 0, respectively. MNI y-coordinates of the coronal slices at the bottom row are: −14, −4, −2, 6, and 8, respectively. (b) Findings from a connectivity analysis, seeding with the ‘targets’ of each subdivision (defined by a separate cohort), revealed a parcellation, along the anterior–posterior axis, within the hippocampus. PCC, posterior cingulate cortex; pgACC, pregenual anterior cingulate cortex; preCG, precentral gyrus.
Clinical Characterization
Table 1 shows the level of symptoms on all measures of general anxiety and depression taken on all subjects. Despite the wide range in anxiety and depressive symptoms represented, the PTSD and GAD groups in our sample do not differ on any symptom measure (t-test, p>0.13).
Testing the ‘Common Deficit’ Hypothesis
We tested our first hypothesis (common deficit) for posterior hippocampal connectivity with a repeated measures ANOVA in the healthy, PTSD, and GAD groups that modeled the three patient groups (between-subject factor), as well as the posterior hippocampal connectivity targets (PCC, pgACC, and precuneus; within-subject factor). We found a significant patient vs healthy subject effect (F1,91=4.52, p=0.036; Figure 3a and Supplementary Figure 2a), consistent with the common deficit hypothesis. This contrast was also significant for just the PCC ROI (F1,91=4.88, p=0.03).
Posterior and anterior hippocampal resting-state functional connectivity in matched cohorts of healthy individuals and patients with post-traumatic stress disorder (PTSD) and generalized anxiety disorder (GAD). (a) Group comparisons for the posterior hippocampus show that diminished posterior hippocampal connectivity is specific to PTSD (asterisk ‘*’ signifies a group difference at p<0.05). (b) Group comparisons for the anterior hippocampus suggest a general impairment in anxiety disorders (asterisk ‘*’ signifies a group difference (healthy vs PTSD or GAD) at p<0.05). Plotted are mean beta estimates±SE. dACC, dorsal anterior cingulate cortex; PCC, posterior cingulate cortex; pgACC, pregenual anterior cingulate cortex; pre-SMA, pre-supplementary motor area.
With respect to connectivity of the anterior hippocampus with its targets, the repeated measures ANOVA did not yield a significant patient vs healthy subject effect (F1,91=1.45, p=0.23). Follow-up tests, however, revealed reduced anterior hippocampal connectivity only with the dACC/pre-SMA in patients compared with healthy subjects (F1,91=4.51, p=0.036; Figure 3b and Supplementary Figure 2b).
The abnormality in connectivity of the posterior hippocampus to these core elements of the default-mode network (PCC, pgACC, and precuneus) suggests that task-evoked activity within this memory-related network may also be perturbed. One of the most salient and robust features of the default-mode network is that it deactivates whenever subjects are engaged in cognitively demanding tasks, referred to as task-independent deactivation (Buckner et al, 2008). We therefore examined the degree of task-independent deactivation in the default-mode targets of the posterior hippocampus. A repeated measures ANOVA on task deactivation data yielded a trend patient vs healthy subject effect (F1,88=3.74, p=0.056; Figure 4 and Supplementary Figure 2c). There was a significant effect for the precuneus ROI alone (F1,88=4.09, p=0.046).
Task-independent deactivation in the posterior hippocampus/default-mode network during attention-demanding tasks. The degree of task-independent deactivation in the same default-mode network components that in the resting state were preferentially connected with the posterior hippocampus was blunted only in post-traumatic stress disorder (PTSD) patients, relative to healthy individuals, as well as generalized anxiety disorder (GAD) patients. Asterisk ‘*’ signifies a group difference at p<0.05. Plotted are mean beta estimates±SE. PCC, posterior cingulate cortex; pgACC, pregenual anterior cingulate cortex.
Testing the ‘Disorder-Specific Deficit’ Hypothesis
Although the analyses above lend some statistical support to the common deficit hypothesis, closer examination of the results suggest that the patient vs healthy subject differences may actually be driven by the PTSD group alone. We therefore examined our alternative hypothesis (disorder-specific deficit) by contrasting the PTSD and GAD group to each other.
Across the posterior hippocampal connectivity target ROIs, we found a selective deficit in PTSD, such that PTSD patients had diminished posterior hippocampal connectivity compared with GAD patients (F1,54=4.03, p=0.05). At the level of individual ROIs, this contrast was significant for the PCC (t(54)=−2.42, p=0.019, d=0.63) and pgACC (t(54)=−2.14, p=0.037, d=0.66). In a secondary analysis, we found that connectivity in PTSD patients was also diminished relative to healthy subjects (F1,53=4.79, p=0.033), which was significant for each individual ROI (PCC: t(53)=−3.01, p=0.004, d=0.68; pgACC: t(53)=−2.08, p=0.043, d=0.66; precuneus: t(53)=−2.29, p=0.026, d=0.55; Figure 3a and Supplementary Figure 2a). GAD patients and healthy subjects did not differ in connectivity to any posterior hippocampal target ROI (p>0.29). For anterior hippocampal connectivity, no differences were observed between PTSD and GAD (p>0.2).
Similarly, we found a significant blunting of task-independent deactivation in PTSD patients relative to GAD patients across the posterior hippocampal target ROIs (F1,52=8.92, p=0.004; Figure 4 and Supplementary Figure 2c). Follow-up tests revealed that PTSD patients had significantly reduced task-independent deactivation compared with GAD patients in each individual ROI (PCC: (t(52)=−1.97, p=0.05, d=0.64; pgACC: t(52)=−2.18, p=0.034, d=0.65; precuneus: t(52)=−2.94, p=0.005, d=0.86). In a secondary analysis, we found that PTSD patients had reduced task-independent deactivation relative to healthy subjects (F1,50=9.54, p=0.003), which was significant for the pgACC (t(50)=−2.25, p=0.029, d=0.71) and precuneus (t(50)=−2.78, p=0.008, d=0.84; Figure 4 and Supplementary Figure 2c). GAD patients and healthy subjects did not differ in task-independent deactivation for any ROI (p>0.42).
Other Analyses
We examined gray matter volume in each hippocampal subdivision with VBM, and found that it was not different between groups, nor accounted for group differences in posterior hippocampal connectivity (see Supplementary text). We also examined the effect of comorbid major depression on posterior hippocampal connectivity in the significant PTSD vs GAD comparisons, and found that it did not moderate the group effects in PTSD (see Supplementary text).
DISCUSSION
In this study, we provide evidence for functional parcellation of the human hippocampus. Our results are consistent with a recent report of a preferential role for the posterior hippocampus in memory in humans, through its functional connectivity with the default-mode network (Poppenk and Moscovitch, 2011). Using this information, we identified abnormalities in the posterior hippocampus/default-mode network that differentiated between PTSD and GAD patients, who furthermore did not differ from healthy controls. Importantly, these abnormalities were similarly present for rs-fcMRI as well as for task-based deactivation. As such, our ‘disorder-specific deficit’ hypothesis received significant support from the findings in posterior hippocampus network.
Findings in anterior hippocampus network, however, were less robust. We only identified an across-disorder abnormality in anterior hippocampus connectivity with the dACC/pre-SMA, but not the entire anterior hippocampus network (unlike the posterior hippocampus). Therefore, our ‘common deficit’ hypothesis found only nonsignificant support, ostensibly at a trend level.
A Default-Mode Network-Based Posterior Hippocampus Circuitry for Memory-Related Functions is Selectively Perturbed in PTSD
Using rs-fcMRI, we found that the posterior hippocampus-connected network maps well onto the classic Papez circuit, which has a crucial role in episodic memory (Mesulam, 2000), consistent with results from a very recent study in healthy subjects (Poppenk and Moscovitch, 2011). Key elements of the posterior hippocampus circuit (pgACC, PCC, and precuneus) have also been recognized as core nodes of the default-mode network. Moreover, related in part to the role of the default-mode network in supporting internally directed mental processes, this network also deactivates in a task-independent way when subjects engage in attention-demanding cognitive tasks (Buckner et al, 2008). Thus, by examining not only rs-fcMRI abnormalities in posterior hippocampal connectivity to the default-mode network but also task-based deactivation dynamics within this network in this study, we can constrain our interpretation of the results in a manner that would not be possible with resting-state data alone.
Overall, we found a robust and selective blunting in both connectivity and task-independent deactivation within the posterior hippocampus/default-mode network in PTSD patients, which was dissociable from the intact connectivity and deactivation patterns in GAD patients, who were furthermore indistinguishable from healthy cohorts. The specificity of our findings is underscored by the fact that PTSD and GAD patients were similar on all demographic and clinical measures, including similarly heightened anxiety and depression symptoms, and rates of comorbid major depressive disorder.
As a hallmark dysfunction in PTSD, but not GAD, includes intrusive memories of the trauma and an inability to update fear memories such that safe contexts can be distinguished from dangerous ones, our findings suggest that the posterior hippocampus is a prime candidate for mediating these abnormalities, through its connections with the default-mode network. This work also underscores the importance of examining the same neurobiological measure across psychiatric cohorts, as similarities and differences in symptom profiles can provide key tools for delineating the pathophysiological relevance of specific neural abnormalities that would not be possible with comparisons of a single patient group with healthy subjects alone (Bluhm et al, 2009; Sripada et al, 2012b; Yin et al, 2011).
There is also a considerable amount of animal work relevant to the posterior (ie, dorsal) hippocampal dissociation between PTSD and GAD, as well as more generally the homology between the human posterior hippocampus and rodent dorsal hippocampus. Using fMRI, for example the connectivity profile of hippocampal subdivisions in human have been shown to largely mirror those in monkeys (Kahn et al, 2008; Libby et al, 2012), whereas manual tracing of the structure acquired through anatomical MRI scans has identified that the tail of the hippocampus in human is homologous to the dorsal hippocampus in several non-primate species (Sasaki et al, 2004). Our finding of a default-mode network-based posterior hippocampus circuitry in human has also recently been extended to rodents using similar neuroimaging approach. Lu et al (2012) demonstrated in rats that the default-mode network not only exists but also includes homologues of key structures noted in our work and that of others (Poppenk and Moscovitch, 2011) (eg, anterior cingulate cortex, retrosplenial cortex, and the dorsal hippocampus), which further strengthens the basis for parcellating hippocampus along its longitudinal axis. As such, converging evidence from noninvasive neuroimaging methods, along with those based on comparative anatomy techniques (ie, tract tracing) in rats (Van Groen and Wyss, 2003) and monkeys (Aggleton et al, 2012; Roberts et al, 2007), together provide support for the homology of hippocampal subdivisions that are the basis for this study (dorsal/ventral and posterior/anterior, respectively).
Our approach for parcellation of the hippocampus into thirds was furthermore informed by prior gene expression work in rodents. Using information from a genome-wide atlas of gene expression in the adult mouse brain (Lein et al, 2007), two studies found that the hippocampus can be divided roughly into thirds along its longitudinal axis based solely on patterns of gene expression (Dong et al, 2009; Thompson et al, 2008). We therefore chose to define our human hippocampus subdivisions by dividing this structure into equal thirds, serving as an initial step forward for translating animal work to humans, in the absence of gene expression or other means to more precisely parcellate the human hippocampus.
Finally, there is a causal link in animal work between regional-specific manipulation of rodent dorsal hippocampus and PTSD-like behaviors in rodents. Kaouane et al (2012) have recently shown that infusion of glucocorticoids—which are secreted naturally in response to stressors—directly into the dorsal hippocampus both impairs the processing of memory and results in generalized fear memory and hyperreactive amygdala activity that also typically characterizes PTSD. Further, stressors also result in methylation of the Bdnf gene and decreased BDNF gene expression in the dorsal hippocampus (Kozlovsky et al, 2007; Roth et al, 2011). Site-specific deletion of Bdnf gene in the dorsal hippocampus results both in poor spatial memory and, importantly, in reduced extinction of conditioned fear, while preserving fear learning and endogenous anxiety (Heldt et al, 2007). Consistent with these findings, BDNF is reduced in the cerebrospinal fluid of patients with PTSD (Bonne et al, 2011). Interestingly, infusion of BDNF into the dorsal hippocampus can cause extinction of conditioned fear, which is blocked by inhibiting the function of BDNF in the medial prefrontal cortex (Peters et al, 2010), consistent with our findings of abnormal posterior hippocampal/default-mode network connectivity and function in PTSD.
Anterior Hippocampus Circuitry: Implications for Anxiety Across Psychiatric Disorders
With respect to the anterior hippocampus, we found that it was preferentially connected with bilateral amygdala, striatum, and an extended region spanning across the pre-SMA, dACC, and dMPFC. This connectivity pattern in general mirrors its anatomical connectivity predicted by animal work across a range of species, which may be linked to various aspects of motivated behavior (Groenewegen et al, 1996; Parent et al, 2010).
In rodents, the prelimbic cortex also has been implicated in the modulation of fear responses and anxiety (Etkin et al, 2011). Intriguingly, inactivation of the ventral hippocampus results in increased responses to fear-conditioned cues in prelimbic cortex (and thus fear expression) (Sotres-Bayon et al, 2010), mirroring our dACC/pre-SMA hypoconnectivity across both anxiety disorder groups. Others have also found increased ventral hippocampal-prelimbic synchronization in anxiogenic environments (Adhikari et al, 2010). Thus, converging lines of research have demonstrated a pivotal role for the anterior hippocampus–dACC/pre-SMA (ventral hippocampus-prelimbic cortex) pathway in the expression of anxiety-related behavior. We found a reduction in anterior hippocampus–dACC/pre-SMA connectivity in a comparison of all patients with healthy subjects, albeit in the context of a nonsignificant overall ANOVA. Future work focusing on this pathway with larger sample sizes will be necessary to confirm the observed effects.
The Importance of Direct Comparisons Between Disorders
This study is one of the first to directly compare PTSD with any other anxiety disorder—a gap in the literature that has prevented testing of key conceptualizations of the anxiety spectrum and the biological validity of individual diagnoses as formulated in DSM. Strikingly, by contrast to the comparable elevated general anxiety and depressive symptoms in our samples of PTSD and GAD, we found that these disorders can be differentiated in terms of both connectivity and deactivation in the posterior hippocampus/default-mode network. As such, these data reflect an important challenge to the view suggested by prior studies, focusing on symptom structure and defensive responding during emotion-modulated startle (McTeague and Lang, 2012; Watson, 2005), which argues for a similarity between these disorders under the umbrella concept of ‘anxious-misery’ disorders. Therefore, it will be critical for future studies to consider inclusion of other diagnostic groups, which may serve as ‘active’ control groups, thus enhancing arguments regarding specificity of findings or reinforcing the generality of a deficit across disorders. These findings also help inform new ways to understand the similarities and differences across a variety of clinical states, such as proposed in the Research Domain Criteria initiative from the National Institute of Mental Health (Insel et al, 2010).
Limitations
Our study did not have a separate trauma-exposed healthy cohort, which may be a limitation relevant to the PTSD patient comparison. However, we note that in a recent study that included trauma-exposed combat veterans with and without PTSD, Sripada et al (2012b) reported PTSD-specific hypoconnectivity in the default-mode network, and provided initial evidence that the observed network abnormality may not be attributed to trauma exposure alone. Moreover, our goal was to demonstrate that disorders that do not differ across a broad range of anxiety and depressive symptoms could nonetheless be distinguished using neurocircuitry measures informed by principled work in experimental animals. Because trauma-exposed healthy subjects do not have anxiety symptoms that are comparable to PTSD patients (and trauma is just one of the many factors that differ between the patient groups), the inclusion of this group may not have furthered our primary goal. Lastly, further work with larger sample size groups will be important for furthering the findings from our study.
CONCLUSIONS
In this study, we first provide evidence for functional parcellation of the human hippocampus along its posterior–anterior axis in a manner consistent with partitioning of the rodent dorsal/ventral hippocampus along genetic–anatomical lines. We then identify abnormalities of the posterior hippocampus/default-mode network that were selectively present in PTSD compared with GAD–disorders with similar levels of general anxiety and depression but differ in fear-related memory.
FUNDING AND DISCLOSURE
This research was supported by the National Institute of Mental Health (R01MH091860 and P30MH089888). The authors declare no conflict of interest.
References
Adhikari A, Topiwala MA, Gordon JA (2010). Synchronized activity between the ventral hippocampus and the medial prefrontal cortex during anxiety. Neuron 65: 257–269.
Aggleton JP, Wright NF, Vann SD, Saunders RC (2012). Medial temporal lobe projections to the retrosplenial cortex of the macaque monkey. Hippocampus 22: 1883–1900.
Amaral DG (1987). Memory: anatomical organization of candidate brain regions. In Handbook of Physiology, the Nervous System. Waverly Press: Baltimore. pp 211–294.
American Psychiatric Association (1994) Diagnostic and Statistical Manual of Mental Disorders 4th edn. American Psychiatric Association: Washington, DC.
Amunts K, Kedo O, Kindler M, Pieperhoff P, Mohlberg H, Shah NJ et al (2005). Cytoarchitectonic mapping of the human amygdala, hippocampal region and entorhinal cortex: intersubject variability and probability maps. Anat Embryol (Berl) 210: 343–352.
Ashburner J, Friston KJ (2000). Voxel-based morphometry—the methods. Neuroimage 11: 805–821.
Ashburner J, Friston KJ (2005). Unified segmentation. Neuroimage 26: 839–851.
Bannerman DM, Grubb M, Deacon RM, Yee BK, Feldon J., Rawlins JN (2003). Ventral hippocampal lesions affect anxiety but not spatial learning. Behav Brain Res 139: 197–213.
Beck AT, Steer RA (1993) Beck Anxiety Inventory Manual. Psychological Corporation: San Antonio, TX.
Beck AT, Steer RA, Brown GK (1996) Manual for Beck Depression Inventory II (BDI-II). Psychological Corporation: San Antonio, TX.
Bluhm RL, Williamson PC, Osuch EA, Frewen PA, Stevens TK, Boksman K et al (2009). Alterations in default network connectivity in posttraumatic stress disorder related to early-life trauma. J Psychiatry Neurosci 34: 187–194.
Bonne O, Gill JM, Luckenbaugh DA, Collins C, Owens MJ, Alesci S et al (2011). Corticotropin-releasing factor, interleukin-6, brain-derived neurotrophic factor, insulin-like growth factor-1, and substance P in the cerebrospinal fluid of civilians with posttraumatic stress disorder before and after treatment with paroxetine. J Clin Psychiatry 72: 1124–1128.
Buckner RL, Andrews-Hanna JR, Schacter DL (2008). The brain's default network: anatomy, function, and relevance to disease. Ann N Y Acad Sci 1124: 1–38.
Cenquizca LA, Swanson LW (2006). Analysis of direct hippocampal cortical field CA1 axonal projections to diencephalon in the rat. J Comp Neurol 497: 101–114.
Cenquizca LA, Swanson LW (2007). Spatial organization of direct hippocampal field CA1 axonal projections to the rest of the cerebral cortex. Brain Res Rev 56: 1–26.
Corcoran KA, Desmond TJ, Frey KA, Maren S (2005). Hippocampal inactivation disrupts the acquisition and contextual encoding of fear extinction. J Neurosci 25: 8978–8987.
Cordes D, Haughton VM, Arfanakis K, Carew JD, Turski PA, Moritz CH et al (2001). Frequencies contributing to functional connectivity in the cerebral cortex in "resting-state" data. Am J Neuroradiol 22: 1326–1333.
Debiec J, LeDoux JE, Nader K (2002). Cellular and systems reconsolidation in the hippocampus. Neuron 36: 527–538.
Dong HW, Swanson LW, Chen L, Fanselow MS, Toga AW (2009). Genomic-anatomic evidence for distinct functional domains in hippocampal field CA1. Proc Natl Acad Sci USA 106: 11794–11799.
Eickhoff SB, Stephan KE, Mohlberg H, Grefkes C, Fink GR, Amunts K et al (2005). A new SPM toolbox for combining probabilistic cytoarchitectonic maps and functional imaging data. Neuroimage 25: 1325–1335.
Etkin A, Egner T, Kalisch R (2011). Emotional processing in anterior cingulate and medial prefrontal cortex. Trends Cogn Sci 15: 85–93.
Etkin A, Klemenhagen KC, Dudman JT, Rogan MT, Hen R, Kandel ER et al (2004). Individual differences in trait anxiety predict the response of the basolateral amygdala to unconsciously processed fearful faces. Neuron 44: 1043–1055.
Etkin A, Prater KE, Schatzberg AF, Menon V, Greicius MD (2009). Disrupted amygdalar subregion functional connectivity and evidence of a compensatory network in generalized anxiety disorder. Arch Gen Psychiatry 66: 1361–1372.
Etkin A, Wager TD (2007). Functional neuroimaging of anxiety: a meta-analysis of emotional processing in PTSD, social anxiety disorder, and specific phobia. Am J Psychiatry 164: 1476–1488.
Fanselow MS, Dong HW (2010). Are the dorsal and ventral hippocampus functionally distinct structures? Neuron 65: 7–19.
Friston KJ, Ashburner J, Poline JB, Frith CD, Heather JD, Frackowiak RS (1995). Spatial registration and normalization of images. Hum Brain Mapp 3: 165–189.
Glover GH, Lai S (1998). Self-navigated spiral fMRI: interleaved vs single-shot. Magn Reson Med 39: 361–368.
Groenewegen HJ, Wright CI, Beijer AV (1996). The nucleus accumbens: gateway for limbic structures to reach the motor system? Prog Brain Res 107: 485–511.
Heldt SA, Stanek L, Chhatwal JP, Ressler KJ (2007). Hippocampus-specific deletion of BDNF in adult mice impairs spatial memory and extinction of aversive memories. Mol Psychiatry 12: 656–670.
Insel T, Cuthbert B, Garvey M, Heinssen R, Pine DS, Quinn K et al (2010). Research domain criteria (RDoC): toward a new classification framework for research on mental disorders. Am J Psychiatry 167: 748–751.
Kahn I, Andrews-Hanna JR, Vincent JL, Snyder AZ, Buckner RL (2008). Distinct cortical anatomy linked to subregions of the medial temporal lobe revealed by intrinsic functional connectivity. J Neurophysiol 100: 129–139.
Kaouane N, Porte Y, Vallee M, Brayda-Bruno L, Mons N, Calandreau L et al (2012). Glucocorticoids can induce PTSD-like memory impairments in mice. Science 335: 1510–1513.
Kim DH, Adalsteinsson E, Glover GH, Spielman DM (2002). Regularized higher-order in vivo shimming. Magn Reson Med 48: 715–722.
Kishi T, Tsumori T, Yokota S, Yasui Y (2006). Topographical projection from the hippocampal formation to the amygdala: a combined anterograde and retrograde tracing study in the rat. J Comp Neurol 496: 349–368.
Kjelstrup KG, Tuvnes FA, Steffenach HA, Murison R, Moser EI, Moser MB (2002). Reduced fear expression after lesions of the ventral hippocampus. Proc Natl Acad Sci USA 99: 10825–10830.
Kozlovsky N, Matar MA, Kaplan Z, Kotler M, Zohar J, Cohen H (2007). Long-term down-regulation of BDNF mRNA in rat hippocampal CA1 subregion correlates with PTSD-like behavioural stress response. Int J Neuropsychopharmacol 10: 741–758.
Lein ES, Hawrylycz MJ, Ao N, Ayres M, Bensinger A, Bernard A et al (2007). Genome-wide atlas of gene expression in the adult mouse brain. Nature 445: 168–176.
Libby LA, Ekstrom AD, Ragland JD, Ranganath C (2012). Differential connectivity of perirhinal and parahippocampal cortices within human hippocampal subregions revealed by high-resolution functional imaging. J Neurosci 32: 6550–6560.
Lu H, Zou Q, Gu H, Raichle ME, Stein EA, Yang Y (2012). Rat brains also have a default mode network. Proc Natl Acad Sci USA 109: 3979–3984.
Maldjian JA, Laurienti PJ, Kraft RA, Burdette JH (2003). An automated method for neuroanatomic and cytoarchitectonic atlas-based interrogation of fMRI data sets. Neuroimage 19: 1233–1239.
McTeague LM, Lang PJ (2012). The anxiety spectrum and the reflex physiology of defense: from circumscribed fear to broad distress. Depress Anxiety 29: 264–281.
Mesulam M (2000) Principles of Cognitive and Behavioral Neurology 2nd edn. Oxford University Press: New York.
Moser MB, Moser EI (1998). Functional differentiation in the hippocampus. Hippocampus 8: 608–619.
Myers KM, Davis M (2002). Behavioral and neural analysis of extinction. Neuron 36: 567–584.
Parent MA, Wang L, Su J, Netoff T, Yuan LL (2010). Identification of the hippocampal input to medial prefrontal cortex in vitro. Cereb Cortex 20: 393–403.
Peters J, Dieppa-Perea LM, Melendez LM, Quirk GJ (2010). Induction of fear extinction with hippocampal-infralimbic BDNF. Science 328: 1288–1290.
Poppenk J, Moscovitch M (2011). A hippocampal marker of recollection memory ability among healthy young adults: contributions of posterior and anterior segments. Neuron 72: 931–937.
Power JD, Barnes KA, Snyder AZ, Schlaggar BL, Petersen SE (2012). Spurious but systematic correlations in functional connectivity MRI networks arise from subject motion. Neuroimage 59: 2142–2154.
Rabinak CA, Angstadt M, Welsh RC, Kenndy AE, Lyubkin M, Martis B et al (2011). Altered amygdala resting-state functional connectivity in post-traumatic stress disorder. Front Psychiatry 2: 62.
Roberts AC, Tomic DL, Parkinson CH, Roeling TA, Cutter DJ, Robbins TW et al (2007). Forebrain connectivity of the prefrontal cortex in the marmoset monkey (Callithrix jacchus): an anterograde and retrograde tract-tracing study. J Comp Neurol 502: 86–112.
Roth TL, Zoladz PR, Sweatt JD, Diamond DM (2011). Epigenetic modification of hippocampal Bdnf DNA in adult rats in an animal model of post-traumatic stress disorder. J Psychiatr Res 45: 919–926.
Sasaki M, Tohyama K, Matsunaga S, Nakamura M, Tomizawa N, Inoue T et al (2004). MRI identification of dorsal hippocampus homologue in human brain. Neuroreport 15: 2173–2176.
Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E et al (1998). The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry 59 (Suppl 20): 22–33, quiz 34–57.
Sotres-Bayon F, Sierra-Mercado D, Pardilla-Delgado E, Quirk GJ (2012). Gating of fear in prelimbic cortex by hippocampal and amygdala inputs. Neuron 76: 804–812.
Spielberger CD, Gorsuch RL, Lushene RE (1970) Manual for the State-Trait Anxiety Inventory. Consulting Psychologists Press: Palo Alto, CA.
Squire LR (1992). Memory and the hippocampus: a synthesis from findings with rats, monkeys, and humans. Psychol Rev 99: 195–231.
Sripada RK, King AP, Garfinkel SN, Wang X, Sripada CS, Welsh RC et al (2012a). Altered resting-state amygdala functional connectivity in men with posttraumatic stress disorder. J Psychiatry Neurosci 37: 241–249.
Sripada RK, King AP, Welsh RC, Garfinkel SN, Wang X, Sripada CS et al (2012b). Neural dysregulation in posttraumatic stress disorder: evidence for disrupted equilibrium between salience and default mode brain networks. Psychosom Med 74: 904–911.
Thompson CL, Pathak SD, Jeromin A, Ng LL, MacPherson CR, Mortrud MT et al (2008). Genomic anatomy of the hippocampus. Neuron 60: 1010–1021.
Tuescher O, Protopopescu X, Pan H, Cloitre M, Butler T, Goldstein M et al (2011). Differential activity of subgenual cingulate and brainstem in panic disorder and PTSD. J Anxiety Disord 25: 251–257.
Van Dijk KR, Sabuncu MR, Buckner RL (2012). The influence of head motion on intrinsic functional connectivity MRI. Neuroimage 59: 431–438.
Van Groen T, Wyss JM (2003). Connections of the retrosplenial granular b cortex in the rat. J Comp Neurol 463: 249–263.
Watson D (2005). Rethinking the mood and anxiety disorders: a quantitative hierarchical model for DSM-V. J Abnorm Psychol 114: 522–536.
Watson D, Clark LA, Weber K, Assenheimer JS, Strauss ME, McCormick RA (1995). Testing a tripartite model: II. Exploring the symptom structure of anxiety and depression in student, adult, and patient samples. J Abnorm Psychol 104: 15–25.
Yin Y, Jin C, Hu X, Duan L, Li Z, Song M et al (2011). Altered resting-state functional connectivity of thalamus in earthquake-induced posttraumatic stress disorder: a functional magnetic resonance imaging study. Brain Res 1411: 98–107.
Acknowledgements
We thank Katie Prater for assistance in subject recruitment and data collection. We also thank Dr Michael Greicius for providing useful insights and also sharing an independent data set that allows for our unbiased approach, as well as Lisa McTeague and Keith Sudheimer for their helpful comments on the manuscript.
Author information
Authors and Affiliations
Corresponding authors
Additional information
This work was presented in abstract form at the Society of Biological Psychiatry, May 2011, San Francisco, CA, USA, and in oral symposium form at the Organization on Human Brain Mapping, June 2011, Quebec City, Canada.
Supplementary Information accompanies the paper on the Neuropsychopharmacology website
Supplementary information
Rights and permissions
About this article
Cite this article
Chen, A., Etkin, A. Hippocampal Network Connectivity and Activation Differentiates Post-Traumatic Stress Disorder From Generalized Anxiety Disorder. Neuropsychopharmacol 38, 1889–1898 (2013). https://doi.org/10.1038/npp.2013.122
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/npp.2013.122
Keywords
This article is cited by
-
Spatiotemporal dynamics of hippocampal-cortical networks underlying the unique phenomenological properties of trauma-related intrusive memories
Molecular Psychiatry (2024)
-
Long term structural and functional neural changes following a single infusion of Ketamine in PTSD
Neuropsychopharmacology (2023)
-
Machine learning-based identification of a psychotherapy-predictive electroencephalographic signature in PTSD
Nature Mental Health (2023)
-
Aberrant intrinsic hippocampal and orbitofrontal connectivity in drug-naive adolescent patients with major depressive disorder
European Child & Adolescent Psychiatry (2023)
-
The effect of SSRIs on fear learning: a systematic review and meta-analysis
Psychopharmacology (2023)