Abstract
The majority of fatal cases of pulmonary embolism in hospitalized patients occur in acutely ill, medically treated patients. Current guidelines, based on a large number of prospective, randomized, controlled trials evaluating the safety and efficacy of pharmacologic venous thromboembolism (VTE) prophylaxis in medical patients, now recommend using VTE prophylaxis in this population. Unfortunately, prophylaxis rates in medical patients are unacceptably low, despite efforts to develop strategies for improving implementation of prophylaxis regimens. Studies indicate that a substantial proportion of patients with VTE present after hospital discharge, but no clinical trials evaluating VTE prophylaxis for medical outpatients have yet been published. In this Review, we examine the literature on VTE prophylaxis in hospitalized medical patients, and evaluate the available data for the outpatient setting.
Key Points
-
Patients should be assessed for their risk of venous thromboembolism (VTE) at hospital admission
-
Anticoagulant medication should be given to patients at risk of VTE unless contraindications exist, in which case mechanical prophylaxis should be used
-
American College of Chest Physicians guidelines recommend the use of low-molecular-weight heparin, low-dose unfractionated heparin, or fondaparinux for VTE prophylaxis in at-risk medical patients
-
Data from observational studies indicate that rates of VTE prophylaxis need to be improved
-
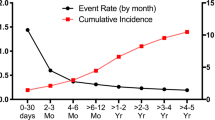
A large proportion of outpatient cases of VTE occur within 3 months of hospitalization
-
Most medical patients do not receive the duration of VTE prophylaxis given in clinical trials, owing to shorter hospital stays
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Geerts, W. H. et al. Prevention of venous thromboembolism: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest 133, 381S–453S (2008).
Cohen, A. T. et al. for the ENDORSE Investigators. Venous thromboembolism risk and prophylaxis in the acute hospital care setting (ENDORSE study): a multinational cross-sectional study. Lancet 371, 387–394 (2008).
Goldhaber, S. Z. & Tapson, V. F. for the DVT FREE Steering Committee. A prospective registry of 5451 patients with ultrasound-confirmed deep vein thrombosis. Am. J. Cardiol. 93, 259–262 (2004).
Kahn, S. R. et al. for the CURVE Study Investigators . Multicenter evaluation of the use of venous thromboembolism prophylaxis in acutely ill medical patients in Canada. Thromb. Res. 119, 145–155 (2007).
Tapson, V. F. et al. for the IMPROVE Investigators. Venous thromboembolism prophylaxis in acutely ill hospitalized medical patients: findings from the International Medical Prevention Registry on Venous Thromboembolism. Chest 132, 936–945 (2007).
Tapson, V. F. Prophylaxis strategies for patients with acute venous thromboembolism. Am. J. Manag. Care 7 (17 Suppl.), S524–S531 (2001).
Anderson, F. A. Jr et al. A population-based perspective of the hospital incidence and case-fatality rates of deep vein thrombosis and pulmonary embolism. The Worcester DVT Study. Arch. Intern. Med. 151, 933–938 (1991).
Monreal, M. et al. for the RIETE Investigators. The outcome after treatment of venous thromboembolism is different in surgical and acutely ill medical patients. Findings from the RIETE registry. J. Thromb. Haemost. 2, 1892–1898 (2004).
Heit, J. A. et al. Relative impact of risk factors for deep vein thrombosis and pulmonary embolism: a population-based study. Arch. Intern. Med. 162, 1245–1248 (2002).
Baglin, T. P., White, K. & Charles, A. Fatal pulmonary embolism in hospitalised medical patients. J. Clin. Pathol. 50, 609–610 (1997).
Cohen, A. T., Edmondson, R. A., Phillips, M. J., Ward, V. P. & Kakkar, V. V. The changing pattern of venous thromboembolic disease. Haemostasis 26, 65–71 (1996).
Spencer, F. A., Lessard, D., Emery, C., Reed, G. & Goldberg, R. J. Venous thromboembolism in the outpatient setting. Arch. Intern. Med. 167, 1471–1475 (2007).
Samama, M. M. et al. A comparison of enoxaparin with placebo for the prevention of venous thromboembolism in acutely ill medical patients. Prophylaxis in Medical Patients with Enoxaparin Study Group. N. Engl. J. Med. 341, 793–800 (1999).
Leizorovicz, A. et al. for the PREVENT Medical Thromboprophylaxis Study Group. Randomized, placebo-controlled trial of dalteparin for the prevention of venous thromboembolism in acutely ill medical patients. Circulation 110, 874–879 (2004).
Cohen, A. T. et al. for the ARTEMIS Investigators. Efficacy and safety of fondaparinux for the prevention of venous thromboembolism in older acute medical patients: randomised placebo controlled trial. BMJ 332, 325–329 (2006).
Lloyd, N. S., Douketis, J. D., Moinuddin, I., Lim, W. & Crowther, M. A. Anticoagulant prophylaxis to prevent asymptomatic deep vein thrombosis in hospitalized medical patients: a systematic review and meta-analysis. J. Thromb. Haemost. 6, 405–414 (2008).
Fraisse, F. et al. Nadroparin in the prevention of deep vein thrombosis in acute decompensated COPD. The Association of Non-University Affiliated Intensive Care Specialist Physicians of France. Am. J. Respir. Crit. Care Med. 161, 1109–1114 (2000).
Hull, R. D. et al. Extended-duration thromboprophylaxis in acutely ill medical patients with recent reduced mobility: methodology for the EXCLAIM study. J. Thromb. Thrombolysis 22, 31–38 (2006).
Dentali, F., Douketis, J. D., Gianni, M., Lim, W. & Crowther, M. A. Meta-analysis: anticoagulant prophylaxis to prevent symptomatic venous thromboembolism in hospitalized medical patients. Ann. Intern. Med. 146, 278–288 (2007).
Lechler, E., Schramm, W. & Flosbach, C. W. The venous thrombotic risk in non-surgical patients: epidemiological data and efficacy/safety profile of a low-molecular-weight heparin (enoxaparin). The Prime Study Group. Haemostasis 26 (Suppl. 2), 49–56 (1996).
Kleber, F. X. et al. for the PRINCE Study Group. Randomized comparison of enoxaparin with unfractionated heparin for the prevention of venous thromboembolism in medical patients with heart failure or severe respiratory disease. Am. Heart J. 145, 614–621 (2003).
Sherman, D. G. et al. for the PREVAIL Investigators. The efficacy and safety of enoxaparin versus unfractionated heparin for the prevention of venous thromboembolism after acute ischaemic stroke (PREVAIL Study): an open-label randomised comparison. Lancet 369, 1347–1355 (2007).
Kanaan, A. O., Silva, M. A., Donovan, J. L., Roy, T. & Al-Homsi, A. S. Meta-analysis of venous thromboembolism prophylaxis in medically ill patients. Clin. Ther. 29, 2395–2405 (2007).
Wein, L., Wein, S., Haas, S. J., Shaw, J. & Krum, H. Pharmacological venous thromboembolism prophylaxis in hospitalized medical patients: a meta-analysis of randomized controlled trials. Arch. Intern. Med. 167, 1476–1486 (2007).
King, C. S., Holley, A. B., Jackson, J. L., Shorr, A. F. & Moores, L. K. Twice vs three times daily heparin dosing for thromboembolism prophylaxis in the general medical population: a meta-analysis. Chest 131, 507–516 (2007).
Samama, M. M. An epidemiologic study of risk factors for deep vein thrombosis in medical outpatients: the Sirius study. Arch. Intern. Med. 160, 3415–3420 (2000).
Kucher, N. et al. Electronic alerts to prevent venous thromboembolism among hospitalized patients. N. Engl. J. Med. 352, 969–977 (2005).
Mosen, D. et al. The effect of a computerized reminder system on the prevention of postoperative venous thromboembolism. Chest 125, 1635–1641 (2004).
McMullin, J. et al. Minimizing errors of omission: behavioural reenforcement of heparin to avert venous emboli: the BEHAVE study. Crit. Care Med. 34, 694–699 (2006).
Tooher, R. et al. A systematic review of strategies to improve prophylaxis for venous thromboembolism in hospitals. Ann. Surg. 241, 397–415 (2005).
Warkentin, T. E. et al. Heparin induced thrombocytopenia in patients treated with low molecular weight heparin or unfractionated heparin. N. Engl. J. Med. 332, 1330–1335 (1995).
McGarry, L. J., Thompson, D., Weinstein, M. C. & Goldhaber, S. Z. Cost effectiveness of thromboprophylaxis with a low molecular weight heparin versus unfractionated heparin in acutely ill medical patients. Am. J. Manag. Care 10, 632–642 (2004).
Tapson, V. F. Acute pulmonary embolism. N. Engl. J. Med. 358, 1037–1052 (2008).
Hull, R. D. et al. Extended-duration venous thromboembolism prophylaxis in acutely ill medical patients with recent reduced mobility: The EXCLAIM study. Late-breaking clinical trials [Abstract]. J. Thromb. Haemost. 5 (Suppl. 2), O-S-001 (2007).
Geerts, W. H. et al. Prevention of venous thromboembolism: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest 126, 338S–400S (2004).
Tapson, V. F. et al. for the NABOR (National Anticoagulation Benchmark and Outcomes Report) Steering Committee. Antithrombotic therapy practices in US hospitals in an era of practice guidelines. Arch. Intern. Med. 165, 1458–1464 (2005).
Acknowledgements
Charles P Vega, University of California, Irvine, CA, is the author of and is solely responsible for the content of the learning objectives, questions and answers of the Medscape-accredited continuing medical education activity associated with this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
V. F. Tapson has acted as a consultant for Genentech. He has also acted as a consultant and received research support from Sanofi-Aventis. G. J. Stashenko declared no competing interests.
Rights and permissions
About this article
Cite this article
Stashenko, G., Tapson, V. Prevention of venous thromboembolism in medical patients and outpatients. Nat Rev Cardiol 6, 356–363 (2009). https://doi.org/10.1038/nrcardio.2009.33
Issue Date:
DOI: https://doi.org/10.1038/nrcardio.2009.33
This article is cited by
-
Formal and informal venous thromboembolism risk assessment and impact on prescribing of thromboprophylaxis: a retrospective cohort study
International Journal of Clinical Pharmacy (2023)
-
Risk of venous thromboembolism in people admitted to hospital with selected immune-mediated diseases: record-linkage study
BMC Medicine (2011)