Key Points
-
Women and men with acute coronary syndrome (ACS) tend to present with a similar constellation of symptoms, although at different rates
-
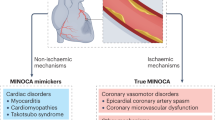
Women often have alternative mechanisms of ACS, such as spontaneous coronary artery dissection and vasospasm, beyond the plaque rupture most typically seen in men
-
Across the range of ACS, women generally receive less-aggressive invasive and pharmacological care than men
-
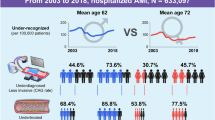
Sex-related outcomes after ACS vary by age; young women have worse short-term and long-term outcomes than men, but old women have similar outcomes to those of old men
-
Representation of women in clinical cardiovascular trials needs to increase in order to address the plethora of unknowns that remain about sex-related differences in ACS
Abstract
Evidence of sex-related disparities in the care and outcomes of patients with acute coronary syndrome (ACS) emerged >30 years ago, and yet the mechanisms behind these sex-specific differences remain unclear. In this Review, we discuss the current literature on differences between women and men in the clinical presentation, pathophysiology, evaluation, management, and outcomes of ACS. Although the symptoms of ACS and the benefits of therapy generally overlap between women and men, women continue to receive less-aggressive invasive and pharmacological therapy than men. In addition, young women in particular have worse short-term and long-term outcomes than men. To understand better the mechanisms behind these continued disparities, we have identified areas of future research that need to be urgently addressed in fields that range from clinical evaluation and management, to increasing representation of women in research.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
US Centers for Disease Control and Prevention. Health, United States, 2013. http://www.cdc.gov/nchs/data/hus/hus13.pdf (2013).
Mozaffarian, D. et al. Heart disease and stroke statistics — 2015 update: a report from the American Heart Association. Circulation 131, e29–e322 (2015).
Kannel, W. B., Sorlie, P. & McNamara, P. M. Prognosis after initial myocardial infarction: the Framingham study. Am. J. Cardiol. 44, 53–59 (1979).
Kim, E. S., Carrigan, T. P. & Menon, V. Enrollment of women in National Heart, Lung, and Blood Institute-funded cardiovascular randomized controlled trials fails to meet current federal mandates for inclusion. J. Am. Coll. Cardiol. 52, 672–673 (2008).
Hochman, J. S. et al. Sex, clinical presentation, and outcome in patients with acute coronary syndromes. N. Engl. J. Med. 341, 226–232 (1999).
Jneid, H. et al. Sex differences in medical care and early death after acute myocardial infarction. Circulation 118, 2803–2810 (2008).
Worrall-Carter, L., McEvedy, S., Wilson, A. & Rahman, M. A. Gender differences in presentation, coronary intervention, and outcomes of 28,985 acute coronary syndrome patients in Victoria, Australia. Womens Health Issues 26, 14–20 (2016).
Poon, S. et al. Bridging the gender gap: Insights from a contemporary analysis of sex-related differences in the treatment and outcomes of patients with acute coronary syndromes. Am. Heart J. 163, 66–73 (2012).
Song, X. T., Chen, Y. D., Pan, W. Q. & Lu, S. Z. & CRACE Investigators. Gender based differences in patients with acute coronary syndrome: findings from Chinese Registry of Acute Coronary Events (CRACE). Chin. Med. J. (Engl.) 120, 1063–1067 (2007).
Yu, H. T. et al. Gender-based differences in the management and prognosis of acute coronary syndrome in Korea. Yonsei Med. J. 52, 562–568 (2011).
Shehab, A. et al. Gender disparities in the presentation, management and outcomes of acute coronary syndrome patients: data from the 2nd Gulf Registry of Acute Coronary Events (Gulf RACE-2). PLoS ONE 8, e55508 (2013).
Canto, J. G. et al. Association of age and sex with myocardial infarction symptom presentation and in-hospital mortality. JAMA 307, 813–822 (2012).
Anand, S. S. et al. Risk factors for myocardial infarction in women and men: insights from the INTERHEART study. Eur. Heart J. 29, 932–940 (2008).
Peters, S. A., Huxley, R. R. & Woodward, M. Diabetes as risk factor for incident coronary heart disease in women compared with men: a systematic review and meta-analysis of 64 cohorts including 858,507 individuals and 28,203 coronary events. Diabetologia 57, 1542–1551 (2014).
Kappert, K. et al. Impact of sex on cardiovascular outcome in patients at high cardiovascular risk: analysis of the Telmisartan Randomized Assessment Study in ACE-Intolerant Subjects With Cardiovascular Disease (TRANSCEND) and the Ongoing Telmisartan Alone and in Combination With Ramipril Global End Point Trial (ONTARGET). Circulation 126, 934–941 (2012).
Dreyer, R. P. et al. Gender differences in pre-event health status of young patients with acute myocardial infarction: a VIRGO study analysis. Eur. Heart J. Acute Cardiovasc. Care 5, 43–54 (2016).
Lopez-Jimenez, F. et al. Prevalence and secular trends of excess body weight and impact on outcomes after myocardial infarction in the community. Chest 125, 1205–1212 (2004).
Njolstad, I., Arnesen, E. & Lund-Larsen, P. G. Smoking, serum lipids, blood pressure, and sex differences in myocardial infarction. A 12-year follow-up of the Finnmark Study. Circulation 93, 450–456 (1996).
White, S. J., Newby, A. C. & Johnson, T. W. Endothelial erosion of plaques as a substrate for coronary thrombosis. Thromb. Haemost. 115, 509–519 (2016).
Parashar, S. et al. Impact of depression on sex differences in outcome after myocardial infarction. Circ. Cardiovasc. Qual. Outcomes 2, 33–40 (2009).
Smolderen, K. G. et al. Depressive symptoms in younger women and men with acute myocardial infarction: insights from the VIRGO study. J. Am. Heart Assoc. 4, e001424 (2015).
Sederholm Lawesson, S., Alfredsson, J., Szummer, K., Fredrikson, M. & Swahn, E. Prevalence and prognostic impact of chronic kidney disease in STEMI from a gender perspective: data from the SWEDEHEART register, a large Swedish prospective cohort. BMJ Open 5, e008188 (2015).
Sederholm Lawesson, S. et al. Gender difference in prevalence and prognostic impact of renal insufficiency in patients with ST-elevation myocardial infarction treated with primary percutaneous coronary intervention. Heart 97, 308–314 (2011).
Chakrabarti, S., Morton, J. S. & Davidge, S. T. Mechanisms of estrogen effects on the endothelium: an overview. Can. J. Cardiol. 30, 705–712 (2014).
Mehta, L. S. et al. Acute myocardial infarction in women: a scientific statement from the American Heart Association. Circulation 133, 916–947 (2016).
Rossouw, J. E., Manson, J. E., Kaunitz, A. M. & Anderson, G. L. Lessons learned from the Women's Health Initiative trials of menopausal hormone therapy. Obstet. Gynecol. 121, 172–176 (2013).
Marjoribanks, J., Farquhar, C., Roberts, H. & Lethaby, A. Long term hormone therapy for perimenopausal and postmenopausal women. Cochrane Database Syst. Rev. 7, CD004143 (2012).
Schierbeck, L. L. et al. Effect of hormone replacement therapy on cardiovascular events in recently postmenopausal women: randomised trial. BMJ 345, e6409 (2012).
Rossouw, J. E., Manson, J. E., Kaunitz, A. M. & Stefanick, M. L. Study had insufficient power to investigate safety. BMJ 345, e8146 (2012).
Marjoribanks, J., Farquhar, C., Roberts, H. & Lethaby, A. Trial does not change the conclusions of Cochrane review of long term hormone therapy for perimenopausal and postmenopausal women. BMJ 345, e8141 (2012).
Lidegaard, O., Lokkegaard, E., Jensen, A., Skovlund, C. W. & Keiding, N. Thrombotic stroke and myocardial infarction with hormonal contraception. N. Engl. J. Med. 366, 2257–2266 (2012).
Canto, J. G. et al. Symptom presentation of women with acute coronary syndromes: myth versus reality. Arch. Intern. Med. 167, 2405–2413 (2007).
Dey, S. et al. Sex-related differences in the presentation, treatment and outcomes among patients with acute coronary syndromes: the Global Registry of Acute Coronary Events. Heart 95, 20–26 (2009).
DeVon, H. A., Ryan, C. J., Ochs, A. L. & Shapiro, M. Symptoms across the continuum of acute coronary syndromes: differences between women and men. Am. J. Crit. Care 17, 14–24; quiz 25 (2008).
Noureddine, S., Arevian, M., Adra, M. & Puzantian, H. Response to signs and symptoms of acute coronary syndrome: differences between Lebanese men and women. Am. J. Crit. Care 17, 26–35 (2008).
Arslanian-Engoren, C. et al. Symptoms of men and women presenting with acute coronary syndromes. Am. J. Cardiol. 98, 1177–1181 (2006).
Lovlien, M., Schei, B. & Gjengedal, E. Are there gender differences related to symptoms of acute myocardial infarction? A Norwegian perspective. Prog. Cardiovasc. Nurs. 21, 14–19 (2006).
Canto, J. G., Canto, E. A. & Goldberg, R. J. Time to standardize and broaden the criteria of acute coronary syndrome symptom presentations in women. Can. J. Cardiol. 30, 721–728 (2014).
Coventry, L. L., Finn, J. & Bremner, A. P. Sex differences in symptom presentation in acute myocardial infarction: a systematic review and meta-analysis. Heart Lung 40, 477–491 (2011).
Shin, J. Y., Martin, R. & Suls, J. Meta-analytic evaluation of gender differences and symptom measurement strategies in acute coronary syndromes. Heart Lung 39, 283–295 (2010).
Chen, W., Woods, S. L. & Puntillo, K. A. Gender differences in symptoms associated with acute myocardial infarction: a review of the research. Heart Lung 34, 240–247 (2005).
DeVon, H. A. & Zerwic, J. J. Symptoms of acute coronary syndromes: are there gender differences? A review of the literature. Heart Lung 31, 235–245 (2002).
Kyker, K. A. & Limacher, M. C. Gender differences in the presentation and symptoms of coronary artery disease. Curr. Womens Health Rep. 2, 115–119 (2002).
Herlitz, J., Bang, A., Karlson, B. W. & Hartford, M. Is there a gender difference in aetiology of chest pain and symptoms associated with acute myocardial infarction? Eur. J. Emerg. Med. 6, 311–315 (1999).
Vaccarino, V. et al. Presentation, management, and outcomes of ischaemic heart disease in women. Nat. Rev. Cardiol. 10, 508–518 (2013).
Virmani, R., Kolodgie, F. D., Burke, A. P., Farb, A. & Schwartz, S. M. Lessons from sudden coronary death: a comprehensive morphological classification scheme for atherosclerotic lesions. Arterioscler. Thromb. Vasc. Biol. 20, 1262–1275 (2000).
Burke, A. P., Virmani, R., Galis, Z., Haudenschild, C. C. & Muller, J. E. 34th Bethesda Conference: task force #2 — what is the pathologic basis for new atherosclerosis imaging techniques? J. Am. Coll. Cardiol. 41, 1874–1886 (2003).
Lansky, A. J. et al. Gender and the extent of coronary atherosclerosis, plaque composition, and clinical outcomes in acute coronary syndromes. JACC Cardiovasc. Imaging 5, S62–S72 (2012).
Falk, E., Nakano, M., Bentzon, J. F., Finn, A. V. & Virmani, R. Update on acute coronary syndromes: the pathologists' view. Eur. Heart J. 34, 719–728 (2013).
Pozzati, A., Pancaldi, L. G., Di Pasquale, G., Pinelli, G. & Bugiardini, R. Transient sympathovagal imbalance triggers 'ischemic' sudden death in patients undergoing electrocardiographic Holter monitoring. J. Am. Coll. Cardiol. 27, 847–852 (1996).
Yoo, S. Y. & Kim, J. Y. Recent insights into the mechanisms of vasospastic angina. Korean Circ. J. 39, 505–511 (2009).
Egashira, K. et al. Basal release of endothelium-derived nitric oxide at site of spasm in patients with variant angina. J. Am. Coll. Cardiol. 27, 1444–1449 (1996).
Selzer, A., Langston, M., Ruggeroli, C. & Cohn, K. Clinical syndrome of variant angina with normal coronary arteriogram. N. Engl. J. Med. 295, 1343–1347 (1976).
Waters, D. D. et al. Factors influencing the long-term prognosis of treated patients with variant angina. Circulation 68, 258–265 (1983).
Walling, A. et al. Long-term prognosis of patients with variant angina. Circulation 76, 990–997 (1987).
Saw, J. Spontaneous coronary artery dissection. Can. J. Cardiol. 29, 1027–1033 (2013).
Vrints, C. J. Spontaneous coronary artery dissection. Heart 96, 801–808 (2010).
Yip, A. & Saw, J. Spontaneous coronary artery dissection — a review. Cardiovasc. Diagn. Ther. 5, 37–48 (2015).
Shamloo, B. K. et al. Spontaneous coronary artery dissection: aggressive versus conservative therapy. J. Invasive Cardiol. 22, 222–228 (2010).
Vanzetto, G. et al. Prevalence, therapeutic management and medium-term prognosis of spontaneous coronary artery dissection: results from a database of 11,605 patients. Eur. J. Cardiothorac. Surg. 35, 250–254 (2009).
Mortensen, K. H., Thuesen, L., Kristensen, I. B. & Christiansen, E. H. Spontaneous coronary artery dissection: a Western Denmark Heart Registry study. Catheter Cardiovasc. Interv. 74, 710–717 (2009).
DeMaio, S. J. Jr, Kinsella, S. H. & Silverman, M. E. Clinical course and long-term prognosis of spontaneous coronary artery dissection. Am. J. Cardiol. 64, 471–474 (1989).
Thompson, E. A., Ferraris, S., Gress, T. & Ferraris, V. Gender differences and predictors of mortality in spontaneous coronary artery dissection: a review of reported cases. J. Invasive Cardiol. 17, 59–61 (2005).
Ito, H. et al. Presentation and therapy of spontaneous coronary artery dissection and comparisons of postpartum versus nonpostpartum cases. Am. J. Cardiol. 107, 1590–1596 (2011).
Akashi, Y. J., Nef, H. M., Mollmann, H. & Ueyama, T. Stress cardiomyopathy. Annu. Rev. Med. 61, 271–286 (2010).
Azzarelli, S. et al. Clinical features of transient left ventricular apical ballooning. Am. J. Cardiol. 98, 1273–1276 (2006).
Parodi, G. et al. Incidence, clinical findings, and outcome of women with left ventricular apical ballooning syndrome. Am. J. Cardiol. 99, 182–185 (2007).
Gianni, M. et al. Apical ballooning syndrome or takotsubo cardiomyopathy: a systematic review. Eur. Heart J. 27, 1523–1529 (2006).
Sy, F. et al. Frequency of Takotsubo cardiomyopathy in postmenopausal women presenting with an acute coronary syndrome. Am. J. Cardiol. 112, 479–482 (2013).
Daniels, L. B. & Maisel, A. S. Cardiovascular biomarkers and sex: the case for women. Nat. Rev. Cardiol. 12, 588–596 (2015).
Pope, J. H. et al. Missed diagnoses of acute cardiac ischemia in the emergency department. N. Engl. J. Med. 342, 1163–1170 (2000).
Vaccarino, V., Parsons, L., Every, N. R., Barron, H. V. & Krumholz, H. M. Sex-based differences in early mortality after myocardial infarction. N. Engl. J. Med. 341, 217–225 (1999).
Moser, D. K. et al. Reducing delay in seeking treatment by patients with acute coronary syndrome and stroke: a scientific statement from the American Heart Association Council on cardiovascular nursing and stroke council. Circulation 114, 168–182 (2006).
Nguyen, H. L. et al. Age and sex differences and 20-year trends in prehospital delay in patients hospitalized with acute myocardial infarction (1986 to 2005). Circ. Cardiovasc. Qual. Outcomes 3, 590–598 (2010).
Nguyen, H. L., Saczynski, J. S., Gore, J. M. & Goldberg, R. J. Age and sex differences in duration of prehospital delay in patients with acute myocardial infarction: a systematic review. Circ. Cardiovasc. Qual. Outcomes 3, 82–92 (2010).
Kaur, R., Lopez, V. & Thompson, D. R. Factors influencing Hong Kong Chinese patients' decision-making in seeking early treatment for acute myocardial infarction. Res. Nurs. Health 29, 636–646 (2006).
DeVon, H. A., Saban, K. L. & Garrett, D. K. Recognizing and responding to symptoms of acute coronary syndromes and stroke in women. J. Obstet. Gynecol. Neonatal Nurs. 40, 372–382 (2011).
Lichtman, J. H. et al. Symptom recognition and healthcare experiences of young women with acute myocardial infarction. Circ. Cardiovasc. Qual. Outcomes 8, S31–S38 (2015).
DeVon, H. A. Promoting cardiovascular health in women across the life span. J. Obstet. Gynecol. Neonatal Nurs. 40, 335–336 (2011).
Antman, E. M. et al. ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (committee to revise the 1999 guidelines for the management of patients with acute myocardial infarction). Circulation 110, e82–e292 (2004).
Anderson, J. L. et al. ACC/AHA 2007 guidelines for the management of patients with unstable angina/non ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (writing committee to revise the 2002 guidelines for the management of patients with unstable angina/non ST-elevation myocardial infarction): developed in collaboration with the American College of Emergency Physicians, the Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons: endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation and the Society for Academic Emergency Medicine. Circulation 116, e148–e304 (2007).
Izadnegahdar, M., Norris, C., Kaul, P., Pilote, L. & Humphries, K. H. Basis for sex-dependent outcomes in acute coronary syndrome. Can. J. Cardiol. 30, 713–720 (2014).
Tamis-Holland, J. E. et al. Benefits of direct angioplasty for women and men with acute myocardial infarction: results of the Global Use of Strategies to Open Occluded Arteries in Acute Coronary Syndromes Angioplasty (GUSTO II-B) angioplasty substudy. Am. Heart J. 147, 133–139 (2004).
Dolor, R. J. et al. Treatment Strategies for Women with Coronary Artery Disease (Agency for Healthcare Research and Quality (US), 2012).
Bavry, A. A. et al. Invasive therapy along with glycoprotein IIb/IIIa inhibitors and intracoronary stents improves survival in non-ST-segment elevation acute coronary syndromes: a meta-analysis and review of the literature. Am. J. Cardiol. 93, 830–835 (2004).
Glaser, R. et al. Benefit of an early invasive management strategy in women with acute coronary syndromes. JAMA 288, 3124–3129 (2002).
O'Donoghue, M. et al. Early invasive versus conservative treatment strategies in women and men with unstable angina and non-ST-segment elevation myocardial infarction: a meta-analysis. JAMA 300, 71–80 (2008).
Anand, S. S. et al. Differences in the management and prognosis of women and men who suffer from acute coronary syndromes. J. Am. Coll. Cardiol. 46, 1845–1851 (2005).
Lu, H. T. et al. Sex differences in acute coronary syndrome in a multiethnic asian population: results of the malaysian national cardiovascular disease database-acute coronary syndrome (NCVD-ACS) registry. Glob. Heart 9, 381–390 (2014).
de-Miguel-Balsa, E. et al. Accessibility to reperfusion therapy among women with acute myocardial infarction: impact on hospital mortality. J. Womens Health (Larchmt) 24, 882–888 (2015).
Kuhn, L., Page, K., Rahman, M. A. & Worrall-Carter, L. Gender difference in treatment and mortality of patients with ST-segment elevation myocardial infarction admitted to Victorian public hospitals: a retrospective database study. Aust. Crit. Care 28, 196–202 (2015).
Leurent, G. et al. Gender differences in presentation, management and inhospital outcome in patients with ST-segment elevation myocardial infarction: data from 5000 patients included in the ORBI prospective French regional registry. Arch. Cardiovasc. Dis. 107, 291–298 (2014).
Tavris, D. et al. Gender differences in the treatment of non-ST-segment elevation myocardial infarction. Clin. Cardiol. 33, 99–103 (2010).
Antithrombotic Trialists, C. et al. Aspirin in the primary and secondary prevention of vascular disease: collaborative meta-analysis of individual participant data from randomised trials. Lancet 373, 1849–1860 (2009).
Berger, J. S. et al. Aspirin for the primary prevention of cardiovascular events in women and men: a sex-specific meta-analysis of randomized controlled trials. JAMA 295, 306–313 (2006).
[No authors listed.] Randomized trial of intravenous streptokinase, oral aspirin, both, or neither among 17,187 cases of suspected acute myocardial infarction: ISIS-2. ISIS-2 (Second International Study of Infarct Survival) Collaborative Group. J. Am. Coll. Cardiol. 12, 3A–13A (1988).
Mehta, S. R. et al. Effects of pretreatment with clopidogrel and aspirin followed by long-term therapy in patients undergoing percutaneous coronary intervention: the PCI-CURE study. Lancet 358, 527–533 (2001).
Boersma, E., Harrington, R. A., Moliterno, D. J., White, H. & Simoons, M. L. Platelet glycoprotein IIb/IIIa inhibitors in acute coronary syndromes. Lancet 360, 342–343 (2002).
Subherwal, S. et al. Baseline risk of major bleeding in non-ST-segment-elevation myocardial infarction: the CRUSADE (Can Rapid risk stratification of Unstable angina patients Suppress ADverse outcomes with Early implementation of the ACC/AHA Guidelines) Bleeding Score. Circulation 119, 1873–1882 (2009).
Mehran, R. et al. A risk score to predict bleeding in patients with acute coronary syndromes. J. Am. Coll. Cardiol. 55, 2556–2566 (2010).
Mehta, S. K. et al. Bleeding in patients undergoing percutaneous coronary intervention: the development of a clinical risk algorithm from the National Cardiovascular Data Registry. Circ. Cardiovasc. Interv. 2, 222–229 (2009).
Lansky, A. J. et al. Percutaneous coronary intervention and adjunctive pharmacotherapy in women: a statement for healthcare professionals from the American Heart Association. Circulation 111, 940–953 (2005).
Hess, C. N. et al. Sex-based differences in outcomes after percutaneous coronary intervention for acute myocardial infarction: a report from TRANSLATE-ACS. J. Am. Heart Assoc. 3, e000523 (2014).
Bangalore, S. et al. Clinical outcomes with β-blockers for myocardial infarction: a meta-analysis of randomized trials. Am. J. Med. 127, 939–953 (2014).
Flather, M. D. et al. Long-term ACE-inhibitor therapy in patients with heart failure or left-ventricular dysfunction: a systematic overview of data from individual patients. Lancet 355, 1575–1581 (2000).
Heart Protection Study Collaborative, G. MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20,536 high-risk individuals: a randomised placebo-controlled trial. Lancet 360, 7–22 (2002).
Cheung, B. M., Lauder, I. J., Lau, C. P. & Kumana, C. R. Meta-analysis of large randomized controlled trials to evaluate the impact of statins on cardiovascular outcomes. Br. J. Clin. Pharmacol. 57, 640–651 (2004).
Akhter, N. et al. Gender differences among patients with acute coronary syndromes undergoing percutaneous coronary intervention in the American College of Cardiology-National Cardiovascular Data Registry (ACC-NCDR). Am. Heart J. 157, 141–148 (2009).
Koopman, C. et al. Persisting gender differences and attenuating age differences in cardiovascular drug use for prevention and treatment of coronary heart disease, 1998–2010. Eur. Heart J. 34, 3198–3205 (2013).
Blomkalns, A. L. et al. Gender disparities in the diagnosis and treatment of non-ST-segment elevation acute coronary syndromes: large-scale observations from the CRUSADE (Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes With Early Implementation of the American College of Cardiology/American Heart Association Guidelines) National Quality Improvement Initiative. J. Am. Coll. Cardiol. 45, 832–837 (2005).
Gan, S. C. et al. Treatment of acute myocardial infarction and 30-day mortality among women and men. N. Engl. J. Med. 343, 8–15 (2000).
Berger, J. S. et al. Sex differences in mortality following acute coronary syndromes. JAMA 302, 874–882 (2009).
Johansson, S. et al. Sex differences in preinfarction characteristics and longterm survival among patients with myocardial infarction. Am. J. Epidemiol. 119, 610–623 (1984).
Bucholz, E. M. et al. Sex differences in long-term mortality after myocardial infarction: a systematic review. Circulation 130, 757–767 (2014).
Koek, H. L. et al. Short- and long-term prognosis after acute myocardial infarction in men versus women. Am. J. Cardiol. 98, 993–999 (2006).
Dreyer, R. P. et al. Sex differences in the rate, timing, and principal diagnoses of 30-day readmissions in younger patients with acute myocardial infarction. Circulation 132, 158–166 (2015).
Vaccarino, V., Krumholz, H. M., Yarzebski, J., Gore, J. M. & Goldberg, R. J. Sex differences in 2-year mortality after hospital discharge for myocardial infarction. Ann. Intern. Med. 134, 173–181 (2001).
Redfors, B. et al. Trends in gender differences in cardiac care and outcome after acute myocardial infarction in Western Sweden: a report from the Swedish Web System for Enhancement of Evidence-Based Care in Heart Disease Evaluated According to Recommended Therapies (SWEDEHEART). J. Am. Heart Assoc. 4, e001995 (2015).
Champney, K. P. et al. The joint contribution of sex, age and type of myocardial infarction on hospital mortality following acute myocardial infarction. Heart 95, 895–899 (2009).
Kumbhani, D. J. et al. Influence of gender on long-term mortality in patients presenting with non-ST-elevation acute coronary syndromes undergoing percutaneous coronary intervention. Am. J. Cardiol. 109, 1087–1091 (2012).
Otten, A. M. et al. Is the difference in outcome between men and women treated by primary percutaneous coronary intervention age dependent? Gender difference in STEMI stratified on age. Eur. Heart J. Acute Cardiovasc. Care 2, 334–341 (2013).
D'Onofrio, G. et al. Sex differences in reperfusion in young patients with ST-segment-elevation myocardial infarction: results from the VIRGO study. Circulation 131, 1324–1332 (2015).
Bangalore, S. et al. Age and gender differences in quality of care and outcomes for patients with ST-segment elevation myocardial infarction. Am. J. Med. 125, 1000–1009 (2012).
Davis, M. et al. Acute coronary syndrome in young women under 55 years of age: clinical characteristics, treatment, and outcomes. Clin. Res. Cardiol. 104, 648–655 (2015).
US Congress. National Institutes of Health revitalization act of 1993. National Institutes of Health http://orwh.od.nih.gov/about/pdf/NIH-Revitalization-Act-1993.pdf (1993).
US Food and Drug Administration. Guideline for the study and evaluation of gender differences in the clinical evaluation of drugs; notice. Fed. Regist. 58, 39406–39416 (1993).
United States General Accounting Office. Women sufficiently represented in new drug testing, but FDA oversight needs improvement. GAO http://www.gao.gov/new.items/d01754.pdf (2001).
Lee, P. Y., Alexander, K. P., Hammill, B. G., Pasquali, S. K. & Peterson, E. D. Representation of elderly persons and women in published randomized trials of acute coronary syndromes. JAMA 286, 708–713 (2001).
Harris, D. J. & Douglas, P. S. Enrollment of women in cardiovascular clinical trials funded by the National Heart, Lung, and Blood Institute. N. Engl. J. Med. 343, 475–480 (2000).
Johnson, S. M., Karvonen, C. A., Phelps, C. L., Nader, S. & Sanborn, B. M. Assessment of analysis by gender in the Cochrane reviews as related to treatment of cardiovascular disease. J. Womens Health (Larchmt) 12, 449–457 (2003).
Cucherat, M., Bonnefoy, E. & Tremeau, G. Primary angioplasty versus intravenous thrombolysis for acute myocardial infarction. Cochrane Database Syst. Rev. 3, CD001560 (2000).
Bucholz, E. M. & Krumholz, H. M. Women in clinical research: what we need for progress. Circ. Cardiovasc. Qual. Outcomes 8, S1–S3 (2015).
Mosca, L. et al. Fifteen-year trends in awareness of heart disease in women: results of a 2012 American Heart Association national survey. Circulation 127, 1254–1263 (2013).
Leifheit-Limson, E. C. et al. Sex differences in cardiac risk factors, perceived risk, and health care provider discussion of risk and risk modification among young patients with acute myocardial infarction: The VIRGO Study. J. Am. Coll. Cardiol. 66, 1949–1957 (2015).
Karam Sadoon Alzuhairi, P. S. et al. Incidence and outcome of first myocardial infarction according to gender and age in Denmark over a 35-year period (1978–2012). Eur. Heart J. 1, 72–78 (2015).
Gottlieb, S. et al. Mortality trends in men and women with acute myocardial infarction in coronary care units in Israel. A comparison between 1981–1983 and 1992–1994. Eur. Heart J. 21, 284–295 (2000).
Takii, T. et al. Trends in acute myocardial infarction incidence and mortality over 30 years in Japan: report from the MIYAGI-AMI Registry Study. Circ. J. 74, 93–100 (2010).
Lundblad, D., Holmgren, L., Jansson, J. H., Naslund, U. & Eliasson, M. Gender differences in trends of acute myocardial infarction events: the Northern Sweden MONICA study 1985–2004. BMC Cardiovasc. Disord. 8, 17 (2008).
Singh, J. A., Lu, X., Ibrahim, S. & Cram, P. Trends in and disparities for acute myocardial infarction: an analysis of Medicare claims data from 1992 to 2010. BMC Med. 12, 190 (2014).
Australian Government. National Statement on Ethical Conduct in Human Research (2007) - Updated May 2015. National Health and Medical Research Council https://www.nhmrc.gov.au/guidelines-publications/e72 (2015).
Health Canada. Guidance Document: Considerations for Inclusion of Women in Clinical Trials and Analysis of Sex Differences. http://www.hc-sc.gc.ca/dhp-mps/prodpharma/applic-demande/guide-ld/clini/womct_femec-eng.php (2013).
European Commission. Gender Mainstreaming in the 6th Framework Programme – Reference Guide for Scientific Officers/Project Officers. ftp://ftp.cordis.europa.eu/pub/science-society/docs/gendervademecum.pdf (2003).
European Medicines Agency. Gender Considerations in the Conduct of Clinical Trials. http://www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2010/01/WC500059887.pdf (2005).
Japan Pharmaceutical Manufacturers Association. Pharmaceutical Administration and Regulations in Japan. http://www.nihs.go.jp/mhlw/yakuji/yakuji-e_20110502-02.pdf (2011).
US Department of Health and Human Services. NIH Policy and Guidelines on The Inclusion of Women and Minorities as Subjects in Clinical Research – Amended, October, 2001. National Institutes of Health https://grants.nih.gov/grants/funding/women_min/guidelines_amended_10_2001.htm (2001).
US Department of Health and Human Services. Guidance for Industry: M3(R2) Nonclinical Safety Studies for the Conduct of Human Clinical Trials and Marketing Authorization for Pharmaceuticals. Food and Drug Administration http://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/ucm073246.pdf (2010).
Author information
Authors and Affiliations
Contributions
N.J.P. researched data for the article. N.J.P. and E.D.P. contributed to the discussion of content, wrote the manuscript, and reviewed and edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Related links
Rights and permissions
About this article
Cite this article
Pagidipati, N., Peterson, E. Acute coronary syndromes in women and men. Nat Rev Cardiol 13, 471–480 (2016). https://doi.org/10.1038/nrcardio.2016.89
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrcardio.2016.89
This article is cited by
-
Sex differences in secondary preventive follow-up after coronary heart events
BMC Cardiovascular Disorders (2023)
-
Sex differences in machine learning computed tomography-derived fractional flow reserve
Scientific Reports (2022)
-
Sex-differences in the management and clinical outcome among patients with acute coronary syndrome
BMC Cardiovascular Disorders (2021)
-
Sex-related impacts on clinical outcomes after percutaneous coronary intervention
Scientific Reports (2020)
-
Disparities in Cardiovascular Care and Outcomes for Women From Racial/Ethnic Minority Backgrounds
Current Treatment Options in Cardiovascular Medicine (2020)