Key Points
-
On average, the annual risk of contralateral breast cancer following a diagnosis of breast cancer is 0.5%, but this risk varies between individuals
-
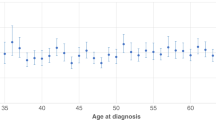
A young age at first diagnosis is associated with a very high relative risk of contralateral breast cancer
-
The risk of contralateral breast cancer is increased in women with mutations in BRCA1, BRCA2, CHEK2 or a strong family history of breast cancer
-
The reduction in mortality associated with contralateral mastectomy is a consequence of the prevention of deaths from contralateral cancer
-
Risk assessment for contralateral breast cancer is appropriate before recommending contralateral mastectomy
Abstract
An increasingly large proportion of women with unilateral breast cancer are treated with bilateral mastectomy. The rationale behind bilateral surgery is to prevent a second primary breast cancer and thereby to avoid the resultant therapy and eliminate the risk of death from contralateral breast cancer. Bilateral mastectomy has been proposed to benefit women at high risk of contralateral cancer, such as carriers of BRCA1 and BRCA2 mutations, but for women without such mutations, the decision to remove the contralateral breast is controversial. It is important to evaluate the risk of contralateral breast cancer on an individual basis, and to tailor surgical treatment accordingly. On average, the annual risk of contralateral breast cancer is approximately 0.5%, but increases to 3% in carriers of a BRCA1 or BRCA2 mutation. Risk factors for contralateral breast cancer include a young age at first diagnosis of breast cancer and a family history of breast cancer. Contralateral mastectomy has not been proven to reduce mortality from breast cancer, but the benefit of such surgery is not expected to become apparent until the second decade after treatment. An alternative to contralateral mastectomy is adjuvant hormonal therapy (such as tamoxifen), but the extent of risk reduction is smaller (approximately 50%) compared to 95% or more for contralateral mastectomy. This Review focuses on the risk factors for contralateral breast cancer, and discusses the evidence that bilateral mastectomy might reduce mortality in patients with unilateral breast cancer.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Barry, M. & Sacchini, V. When is contralateral mastectomy warranted in unilateral breast cancer? Expert Rev. Anticancer Ther. 11, 1209–1214 (2011).
Murphy, J. A., Milner, T. D. & O'Donoghue, J. M. Contralateral risk-reducing mastectomy in sporadic breast cancer. Lancet Oncol. 14, e262–e269 (2013).
Gilbert, A. Why more women are choosing double mastectomies [online], (2013).
Tuttle, T. M., Habermann, E. B., Grund, E. H., Morris, T. J. & Virnig, B. A. Increasing use of contralateral prophylactic mastectomy for breast cancer patients: a trend toward more aggressive surgical treatment. J. Clin. Oncol. 25, 5203–5209 (2007).
King, T. A. et al. Clinical management factors contribute to the decision for contralateral prophylactic mastectomy. J. Clin. Oncol. 29, 2158–2164 (2011).
Rosenberg, S. M. et al. Perceptions, knowledge, and satisfaction with contralateral prophylactic mastectomy among young women with breast cancer: a cross-sectional survey. Ann. Intern. Med. 159, 373–381 (2013).
Banelli, B. et al. Pathological and molecular characteristics distinguishing contralateral metastatic from new primary breast cancer. Ann. Oncol. 21, 1237–1242 (2010).
Kim, M. Y. et al. Tumor self-seeding by circulating cancer cells. Cell 139, 1315–1326 (2009).
Hartman, M. et al. Incidence and prognosis of synchronous and metachronous bilateral breast cancer. J. Clin. Oncol. 25, 4210–4216 (2007).
Schaapveld, M. et al. The impact of adjuvant therapy on contralateral breast cancer risk and the prognostic significance of contralateral breast cancer: a population based study in the Netherlands. Breast Cancer Res. Treat. 110, 189–197 (2008).
Intra, M. et al. Clinicopathologic characteristics of 143 patients with synchronous bilateral invasive breast carcinomas treated in a single institution. Cancer 101, 905–912 (2004).
Huo, D., Melkonian, S., Rathouz, P. J., Khramtsov, A. & Olopade, O. I. Concordance in histological and biological parameters between first and second primary breast cancers. Cancer 117, 907–915 (2011).
Brennan, M. E. et al. Magnetic resonance imaging screening of the contralateral breast in women with newly diagnosed breast cancer: systematic review and meta-analysis of incremental cancer detection and impact on surgical management. J. Clin. Oncol. 27, 5640–5649 (2009).
King, T. A. et al. Occult malignancy in patients undergoing contralateral prophylactic mastectomy. Ann. Surg. 254, 2–7 (2011).
Sorbero, M. E., Dick, A. W., Beckjord, E. B. & Ahrendt, G. Diagnostic breast magnetic resonance imaging and contralateral prophylactic mastectomy. Ann. Surg. Oncol. 16, 1597–1605 (2009).
Chen, Y., Thompson, W., Semenciw, R. & Mao, Y. Epidemiology of contralateral breast cancer. Cancer Epidemiol. Biomarkers Prev. 8, 855–861 (1999).
National Comprehensive Cancer Network (NCCN) in Breast Cancer NCCN Practice Guidelines in Oncology (ver. 2.2011) binv-16 (NCCN, 2011).
Houssami, N., Ciatto, S., Martinelli, F., Bonardi, R. & Duffy, S. W. Early detection of second breast cancers improves prognosis in breast cancer survivors. Ann. Oncol. 20, 1505–1510 (2009).
Solin, L. J., Orel, S. G., Hwang, W. T., Harris, E. E. & Schnall, M. D. Relationship of breast magnetic resonance imaging to outcome after breast-conservation treatment with radiation for women with early-stage invasive breast carcinoma or ductal carcinoma in situ. J. Clin. Oncol. 26, 386–391 (2008).
Cancer Incidence in Five Continents Volume VIII (eds Parkin, D. M. et al.) (International Agency for Research on Cancer, 2002).
Rutqvist, L. E. et al. Contralateral primary tumors in breast cancer patients in a randomized trial of adjuvant tamoxifen therapy. J. Natl Cancer Inst. 83, 1299–1306 (1991).
Vaittinen, P. & Hemminki, K. Risk factors and age-incidence relationships for contralateral breast cancer. Int. J. Cancer 88, 998–1002 (2000).
Kurian, A. W. et al. Second primary breast cancer occurrence according to hormone receptor status. J. Natl Cancer Inst. 101, 1058–1065 (2009).
Walsh, T. & King, M. C. Ten genes for inherited breast cancer. Cancer Cell 11, 103–105 (2007).
Metcalfe, K. et al. Predictors of contralateral breast cancer risk in BRCA1 and BRCA2 mutation carriers. Br. J. Cancer 104, 1384–1392 (2011).
Mavaddat, N. et al. Cancer risks for BRCA1 and BRCA2 mutation carriers: results from prospective analysis of EMBRACE. J. Natl Cancer Inst. 105, 812–822 (2013).
Malone, K. E. et al. Population-based study of the risk of second primary contralateral breast cancer associated with carrying a mutation in BRCA1 or BRCA2. J. Clin. Oncol. 28, 2404–2410 (2010).
Narod, S. A. et al. A prior diagnosis of breast cancer is a risk factor for breast cancer in BRCA1 and BRCA2 carriers Curr. Oncol. (in press).
Graeser, M. K. et al. Contralateral breast cancer risk in BRCA1 and BRCA2 mutation carriers. J. Clin. Oncol. 27, 5887–5892 (2009).
Gronwald, J. et al. Tamoxifen and contralateral breast cancer in BRCA1 and BRCA2 carriers: an update. Int. J. Cancer 118, 2281–2284 (2006).
Phillips, K. A. et al. Tamoxifen and risk of contralateral breast cancer for BRCA1 and BRCA2 mutation carriers. J. Clin. Oncol. 31, 3091–3099 (2013).
Domchek, S. M. et al. Association of risk-reducing surgery in BRCA1 or BRCA2 mutation carriers with cancer risk and mortality. JAMA 304, 967–975 (2010).
Reding, K. W. et al. Adjuvant systemic therapy for breast cancer in BRCA1/BRCA2 mutation carriers in a population-based study of risk of contralateral breast cancer. Breast Cancer Res. Treat. 123, 491–498 (2010).
Metcalfe, K. A. et al. International variation in rates of uptake of preventive options in BRCA1 and BRCA2 mutation carriers. Int. J. Cancer 122, 2017–2022 (2008).
Lodder, L. N. et al. One year follow-up of women opting for presymptomatic testing for BRCA1 and BRCA2: emotional impact of the test outcome and decisions on risk management (surveillance or prophylactic surgery). Breast Cancer Res. Treat. 73, 97–112 (2002).
Evans, D. G. et al. Contralateral mastectomy improves survival in women with BRCA1/2-associated breast cancer. Breast Cancer Res. Treat. 140, 135–142 (2013).
Laitman, Y. et al. Rates of risk-reducing surgery in Israeli BRCA1 and BRCA2 mutation carriers. Clin. Genet. 85, 68–71 (2014).
Singer, C. F. et al. Clinical implications of genetic testing for BRCA1 and BRCA2 mutations in Austria. Clin. Genet. 85, 72–75 (2014).
Zhang, S. et al. Frequency of the CHEK2 1100delC mutation among women with breast cancer: an international study. Cancer Res. 68, 2154–2157 (2008).
Mellemkjaer, L. et al. Risk for contralateral breast cancer among carriers of the CHEK2*1100delC mutation in the WECARE Study. Br. J. Cancer 98, 728–733 (2008).
Broeks, A. et al. Excess risk for contralateral breast cancer in CHEK2*1100delC germline mutation carriers. Breast Cancer Res. Treat. 83, 91–93 (2004).
Narod, S. A. Testing for CHEK2 in the cancer genetics clinic: ready for prime time? Clin. Genet. 78, 1–7 (2010).
Ghoussaini, M. & Pharoah, P. D. Polygenic susceptibility to breast cancer: current state-of-the-art. Future Oncol. 5, 689–701 (2009).
Teraoka, S. N. et al. Single nucleotide polymorphisms associated with risk for contralateral breast cancer in the Women's Environment, Cancer, and Radiation Epidemiology (WECARE) Study. Breast Cancer Res. 13, R114 (2011).
Horn, P. L. & Thompson, W. D. Risk of contralateral breast cancer: associations with factors related to initial breast cancer. Am. J. Epidemiol. 128, 309–323 (1998).
Reiner, A. S. et al. Risk of asynchronous contralateral breast cancer in noncarriers of BRCA1 and BRCA2 mutations with a family history of breast cancer: a report from the Women's Environmental Cancer and Radiation Epidemiology Study. J. Clin. Oncol. 31, 433–439 (2013).
Poynter, J. N. et al. Reproductive factors and risk of contralateral breast cancer by BRCA1 and BRCA2 mutation status: results from the WECARE study. Cancer Causes Control 21, 839–846 (2010).
Largent, J. A. et al. Reproductive history and risk of second primary breast cancer: the WECARE study. Cancer Epidemiol. Biomarkers Prev. 16, 906–911 (2007).
Knight, J. A. et al. Alcohol intake and cigarette smoking and risk of a contralateral breast cancer: The Women's Environmental Cancer and Radiation Epidemiology Study. Am. J. Epidemiol. 169, 962–968 (2009).
Figueiredo, J. C. et al. Oral contraceptives, postmenopausal hormones, and risk of asynchronous bilateral breast cancer: the WECARE Study Group. J. Clin. Oncol. 26, 1411–1418 (2008).
Brooks, J. D. et al. Body mass index and risk of second primary breast cancer: the WECARE Study. Breast Cancer Res. Treat. 131, 571–580 (2012).
Boyd, N. F., Martin, L. J., Yaffe, M. J. & Minkin, S. Mammographic density and breast cancer risk: current understanding and future prospects. Breast Cancer Res. 13, 223 (2011).
Cil, T. et al. Mammographic density and the risk of breast cancer recurrence after breast-conserving surgery. Cancer 115, 5780–5787 (2009).
Sandberg, M. E. et al. Change of mammographic density predicts the risk of contralateral breast cancer: a case–control study. Breast Cancer Res. 15, R57 (2013).
Vogel, V. G. et al. Update of the National Surgical Adjuvant Breast and Bowel Project Study of Tamoxifen and Raloxifene (STAR) P-2 trial: preventing breast cancer. Cancer Prev. Res. (Phila.) 3, 696–706 (2010).
Goss, P. E. Letrozole in the extended adjuvant setting: MA.17. Breast Cancer Res. Treat. 105, 45–53 (2007).
Alkner, S. et al. Tamoxifen reduces the risk of contralateral breast cancer in premenopausal women: results from a controlled randomised trial. Eur. J. Cancer 45, 2496–2502 (2009).
Early Breast Cancer Trialists Collaborative Group. Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. Lancet 365, 1687–1717 (2005).
Arpino, G., Bardou, V. J., Clark, G. M. & Elledge, R. M. Infiltrating lobular carcinoma of the breast: tumor characteristics and clinical outcome. Breast Cancer Res. 6, R149–R156 (2004).
Saltzman, B. S., Malone, K. E., McDougall, J. A., Daling, J. R. & Li, C. I. Estrogen receptor, progesterone receptor, and HER2-neu expression in first primary breast cancers and risk of second primary contralateral breast cancer. Breast Cancer Res. Treat. 135, 849–855 (2012).
Swain, S. M. et al. Estrogen receptor status of primary breast cancer is predictive of estrogen receptor status of contralateral breast cancer. J. Natl Cancer Inst. 96, 516–523 (2004).
Arpino, G., Weiss, H. L., Clark, G. M., Hilsenbeck, S. G. & Osborne, C. K. Hormone receptor status of a contralateral breast cancer is independent of the receptor status of the first primary in patients not receiving adjuvant tamoxifen. J. Clin. Oncol. 23, 4687–4694 (2005).
Safal, M. et al. Bilateral synchronous breast cancer and HER-2/neu overexpression. Breast Cancer Res. Treat. 72, 195–201 (2002).
Bessonova, L., Taylor, T. H., Mehta, R. S., Zell, J. A. & Anton-Culver, H. Risk of a second breast cancer associated with hormone-receptor and HER2/neu status of the first breast cancer. Cancer Epidemiol. Biomarkers Prev. 20, 389–396 (2011).
Stark, A., Lu, M., Mackowiak, P. & Linden, M. Concordance of the hormone receptors and correlation of HER-2/neu overexpression of the metachronous cancers of contralateral breasts. Breast J. 11, 183–187 (2005).
Russnes, H. G. et al. Paired distribution of molecular subtypes in bilateral breast carcinomas. Cancer Genet. 204, 96–102 (2011).
Coradini, D. et al. Is steroid receptor profile in contralateral breast cancer a marker of independence of the corresponding primary tumour? J. Cancer 34, 825–830 (1998).
Kollias, J. et al. Phenotypic similarities in bilateral breast cancer. Breast Cancer Res. Treat. 85, 255–261 (2004).
Weitzel, J. N. et al. A comparison of bilateral breast cancers in BRCA carriers. Cancer Epidemiol. Biomarkers Prev. 14, 1534–1538 (2005).
Suspitsin, E. N. et al. TP53 mutations in synchronous and metachronous bilateral breast carcinomas. Cancer Genet. Cytogenet. 184, 119–121 (2008).
Suspitsin, E. N. et al. Nonrandom distribution of oncogene amplifications in bilateral breast carcinomas: possible role of host factors and survival bias. Int. J. Cancer 120, 297–302 (2007).
Narod, S. A. Breast cancer in young women. Nat. Rev. Clin. Oncol. 9, 460–470 (2012).
Narod, S. A. A model for breast cancer risk based on stem-cell theory. Curr. Oncol. 19, 9–11 (2012).
Dontu, G., El-Ashry, D. & Wicha, M. S. Breast cancer, stem/progenitor cells and the estrogen receptor. Trends Endocrinol. Metab. 15, 193–197 (2004).
Ruark, E. et al. Mosaic PPM1D mutations are associated with predisposition to breast and ovarian cancer. Nature 493, 406–410 (2013).
Pal, B. et al. Global changes in the mammary epigenome are induced by hormonal cues and coordinated by Ezh2. Cell Rep. 3, 411–426 (2013).
Narod, S. A. The impact of contralateral mastectomy on mortality in BRCA1 and BRCA2 mutation carriers with breast cancer. Breast Cancer Res. Treat. 128, 581–583 (2011).
Brewster, A. M. et al. Association between contralateral prophylactic mastectomy and breast cancer outcomes by hormone receptor status. Cancer 118, 5637–5643 (2012).
Herrinton, L. J. et al. Efficacy of prophylactic mastectomy in women with unilateral breast cancer: a cancer research network project. J. Clin. Oncol. 23, 4275–4286 (2005).
Bedrosian, I., Hu, C. Y. & Chang, G. J. Population-based study of contralateral prophylactic mastectomy and survival outcomes of breast cancer patients. J. Natl Cancer Inst. 102, 401–409 (2010).
Tyrer, J., Duffy, S. W. & Cuzick, J. A breast cancer prediction model incorporating familial and personal risk factors. Stat. Med. 23, 1111–1130 (2004).
Campbell, H. E., Taylor, M. A., Harris, A. L. & Gray, A. M. An investigation into the performance of the Adjuvant! Online prognostic programme in early breast cancer for a cohort of patients in the United Kingdom. Br. J. Cancer 101, 1074–1084 (2009).
Wishart, G. C. et al. PREDICT: a new UK prognostic model that predicts survival following surgery for invasive breast cancer. Breast Cancer Res. 12, R1 (2010).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The author declares no competing financial interests.
PowerPoint slides
Rights and permissions
About this article
Cite this article
Narod, S. Bilateral breast cancers. Nat Rev Clin Oncol 11, 157–166 (2014). https://doi.org/10.1038/nrclinonc.2014.3
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrclinonc.2014.3
This article is cited by
-
Long-term survival of screen-detected synchronous and metachronous bilateral non-palpable breast cancer among Chinese women: a hospital-based study (2003–2017)
Breast Cancer Research and Treatment (2022)
-
PredictCBC-2.0: a contralateral breast cancer risk prediction model developed and validated in ~ 200,000 patients
Breast Cancer Research (2022)
-
Increased risk of breast cancer-specific mortality among cancer survivors who developed breast cancer as a second malignancy
BMC Cancer (2021)
-
The risk of contralateral breast cancer: a SEER-based analysis
British Journal of Cancer (2021)
-
Tumor phenotype and concordance in synchronous bilateral breast cancer in young women
Breast Cancer Research and Treatment (2021)