Key Points
-
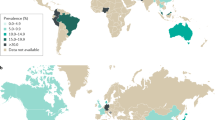
The prevalence of IBS is as high as 20%, with an estimated incidence of 1–2% per year in community samples in Western populations; direct and indirect costs related to IBS are high
-
Individual symptom items taken from the clinical history perform poorly in predicting IBS
-
Symptom-based diagnostic criteria perform only modestly in predicting IBS, with the current gold standard, the Rome III criteria, performing no better than previous recommended symptom-based criteria
-
Biomarkers, with the potential exception of faecal volatile organic molecules and possibly colonic mucosal immune cells, have been disappointing in terms of their performance in diagnosing IBS accurately
-
Combining clinical markers with biomarkers and psychological markers (so-called psychomarkers) could improve our ability to distinguish between IBS and organic disease, but at the cost of increasing complexity
-
Latent class analysis to improve the predictive power of methods used to diagnose IBS, and to discriminate between IBS and non-IBS symptom profiles, might represent a future area of development
Abstract
IBS is estimated to have a prevalence of up to 20% in Western populations and results in substantial costs to health-care services worldwide, estimated to be US$1 billion per year in the USA. IBS remains difficult to diagnose due to its multifactorial aetiology, heterogeneous nature and overlap of symptoms with organic pathologies, such as coeliac disease and IBD. As a result, IBS often continues to be a diagnosis of exclusion, resulting in unnecessary investigations. Available methods for the diagnosis of IBS—including the current gold standard, the Rome III criteria—perform only moderately well. Visceral hypersensitivity and altered pain perception do not discriminate between IBS and other functional gastrointestinal diseases or health with any great accuracy. Attention has now turned to developing novel biomarkers and using psychological markers (so-called psychomarkers) to aid the diagnosis of IBS. This Review describes how useful symptoms, symptom-based criteria, biomarkers and psychomarkers, and indeed combinations of all these approaches, are in the diagnosis of IBS. Future directions in diagnosing IBS could include combining demographic data, gastrointestinal symptoms, biomarkers and psychomarkers using statistical methods. Latent class analysis to distinguish between IBS and non-IBS symptom profiles might also represent a promising avenue for future research.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Longstreth, G. F. et al. Functional bowel disorders. Gastroenterology 130, 1480–1491 (2006).
Lovell, R. M. & Ford, A. C. Global prevalence of and risk factors for irritable bowel syndrome: a meta-analysis. Clin. Gastroenterol. Hepatol. 10, 712–721.e4 (2012).
Ford, A. C., Forman, D., Bailey, A. G., Axon, A. T. & Moayyedi, P. Irritable bowel syndrome: a 10-yr natural history of symptoms and factors that influence consultation behavior. Am. J. Gastroenterol. 103, 1229–1239 (2008).
Koloski, N. A., Talley, N. J. & Boyce, P. M. Epidemiology and health care seeking in the functional GI disorders: a population-based study. Am. J. Gastroenterol. 97, 2290–2299 (2002).
Koloski, N. A., Talley, N. J., Huskic, S. S. & Boyce, P. M. Predictors of conventional and alternative health care seeking for irritable bowel syndrome and functional dyspepsia. Aliment. Pharmacol. Ther. 17, 841–851 (2003).
Lovell, R. M. & Ford, A. C. Effect of gender on prevalence of irritable bowel syndrome in the community: systematic review and meta-analysis. Am. J. Gastroenterol. 107, 991–1000 (2012).
Ford, A. C., Marwaha, A., Lim, A. & Moayyedi, P. Systematic review and meta-analysis of the prevalence of irritable bowel syndrome in individuals with dyspepsia. Clin. Gastroenterol. Hepatol. 8, 401–409 (2010).
Suares, N. C. & Ford, A. C. Prevalence of, and risk factors for, chronic idiopathic constipation in the community: systematic review and meta-analysis. Am. J. Gastroenterol. 106, 1582–1591 (2011).
Riedl, A. et al. Somatic comorbidities of irritable bowel syndrome: a systematic analysis. J. Psychosom. Res. 64, 573–582 (2008).
Everhart, J. E. & Ruhl, C. E. Burden of digestive diseases in the United States part I: overall and upper gastrointestinal diseases. Gastroenterology 136, 376–386 (2009).
Drossman, D. A. et al. U. S. householder survey of functional gastrointestinal disorders. Prevalence, sociodemography, and health impact. Dig. Dis. Sci. 38, 1569–1580 (1993).
Kanazawa, M. et al. Motility response to colonic distention is increased in postinfectious irritable bowel syndrome (PI-IBS). Neurogastroenterol. Motil. 26, 696–704 (2014).
Balestra, B. et al. Colonic mucosal mediators from patients with irritable bowel syndrome excite enteric cholinergic motor neurons. Neurogastroenterol. Motil. 24, 1118–e570 (2012).
Tillisch, K., Mayer, E. A. & Labus, J. S. Quantitative meta-analysis identifies brain regions activated during rectal distension in irritable bowel syndrome. Gastroenterology 140, 91–100 (2011).
Manabe, N. et al. Lower functional gastrointestinal disorders: evidence of abnormal colonic transit in a 287 patient cohort. Neurogastroenterol. Motil. 22, 293–e82 (2010).
Cann, P. A., Read, N. W., Brown, C., Hobson, N. & Holdsworth, C. D. Irritable bowel syndrome: relationship of disorders in the transit of a single solid meal to symptom patterns. Gut 24, 405–411 (1983).
Kassinen, A. et al. The fecal microbiota of irritable bowel syndrome patients differs significantly from that of healthy subjects. Gastroenterology 133, 24–33 (2007).
van Tilburg, M. A., Palsson, O. S. & Whitehead, W. E. Which psychological factors exacerbate irritable bowel syndrome? Development of a comprehensive model. J. Psychosom. Res. 74, 486–492 (2013).
Halpin, S. J. & Ford, A. C. Prevalence of symptoms meeting criteria for irritable bowel syndrome in inflammatory bowel disease: systematic review and meta-analysis. Am. J. Gastroenterol. 107, 1474–1482 (2012).
Gracie, D. J. et al. Prevalence of, and predictors of, bile acid malabsorption in outpatients with chronic diarrhea. Neurogastroenterol. Motil. 24, 983–e538 (2012).
Wedlake, L. et al. Systematic review: the prevalence of idiopathic bile acid malabsorption as diagnosed by SeHCAT scanning in patients with diarrhoea-predominant irritable bowel syndrome. Aliment. Pharmacol. Therap. 30, 707–717 (2009).
Ford, A. C. et al. Yield of diagnostic tests for celiac disease in individuals with symptoms suggestive of irritable bowel syndrome: systematic review and meta-analysis. Arch. Intern. Med. 169, 651–658 (2009).
Sainsbury, A., Sanders, D. S. & Ford, A. C. Prevalence of irritable bowel syndrome-type symptoms in patients with celiac disease: a meta-analysis. Clin. Gastroenterol. Hepatol. 11, 359–365.e1 (2013).
Sanders, D. S. et al. Association of adult coeliac disease with irritable bowel syndrome: a case-control study in patients fulfilling ROME II criteria referred to secondary care. Lancet 358, 1504–1508 (2001).
Yawn, B. P. et al. Diagnosis and care of irritable bowel syndrome in a community-based population. Am. J. Manag. Care 7, 585–592 (2001).
Manning, A. P., Thompson, W. G., Heaton, K. W. & Morris, A. F. Towards positive diagnosis of the irritable bowel. Br. Med. J. 2, 653–654 (1978).
National Institute for Health and Care Excellence. Irritable bowel syndrome in adults: diagnosis and management of irritable bowel syndrome in primary care. National Institute for Health and Care Excellence [online], (2008).
Brandt, L. J. et al. An evidence-based position statement on the management of irritable bowel syndrome. Am. J. Gastroenterol. 104 (Suppl. 1), S1–S35 (2009).
Quigley, E. et al. World Gastroenterology Organisation Global Guideline: Irritable bowel syndrome: a global perspective - April 20, 2009. South African Gastroenterol. Rev. 7, 23–30 (2009).
Ford, A. C. et al. Validation of the Rome III criteria for the diagnosis of irritable bowel syndrome in secondary care. Gastroenterology 145, 1262–1270.e1 (2013).
Dogan, U. B. & Unal, S. Kruis scoring system and Manning's criteria in diagnosis of irritable bowel syndrome: is it better to use combined? Acta Gastroenterol. Belg. 59, 225–228 (1996).
Tibble, J. A., Sigthorsson, G., Foster, R., Forgacs, I. & Bjarnason, I. Use of surrogate markers of inflammation and Rome criteria to distinguish organic from nonorganic intestinal disease. Gastroenterology 123, 450–460 (2002).
van Rheenen, P. F., Van de Vijver, E. & Fidler, V. Faecal calprotectin for screening of patients with suspected inflammatory bowel disease: diagnostic meta-analysis. BMJ 341, c3369 (2010).
Sidhu, R. et al. Faecal lactoferrin—a novel test to differentiate between the irritable and inflamed bowel? Aliment. Pharmacol. Ther. 31, 1365–1370 (2010).
Kruis, W. et al. A diagnostic score for the irritable bowel syndrome. Its value in the exclusion of organic disease. Gastroenterology 87, 1–7 (1984).
Frigerio, G. et al. Irritable bowel syndrome. Still far from a positive diagnosis. Dig. Dis. Sci. 37, 164–167 (1992).
Hammer, J., Eslick, G. D., Howell, S. C., Altiparmak, E. & Talley, N. J. Diagnostic yield of alarm features in irritable bowel syndrome and functional dyspepsia. Gut 53, 666–672 (2004).
Jeong, H., Lee, H. R., Yoo, B. C. & Park, S. M. Manning criteria in irritable bowel syndrome: its diagnostic significance. Korean J. Intern. Med. 8, 34–39 (1993).
Rao, K. P., Gupta, S., Jain, A. K., Agrawal, A. K. & Gupta, J. P. Evaluation of Manning's criteria in the diagnosis of irritable bowel syndrome. J. Assoc. Physicians India 41, 357–358 (1993).
Ford, A. C. et al. Will the history and physical examination help establish that irritable bowel syndrome is causing this patient's lower gastrointestinal tract symptoms? JAMA 300, 1793–1805 (2008).
Whitehead, W. E. et al. Existence of irritable bowel syndrome supported by factor analysis of symptoms in two community samples. Gastroenterology 98, 336–340 (1990).
Talley, N. J., Boyce, P. & Jones, M. Identification of distinct upper and lower gastrointestinal symptom groupings in an urban population. Gut 42, 690–695 (1998).
Drossman, D. A. et al. Identification of sub-groups of functional gastrointestinal disorders. Gastroenterol. Int. 3, 159–172 (1990).
Thompson, W. G. et al. Functional bowel disorders and functional abdominal pain. Gut 45 (Suppl. 2), II43–II47 (1999).
Thompson, W. G., Heaton, K. W., Smyth, G. T. & Smyth, C. Irritable bowel syndrome: the view from general practice. Eur. J. Gastroenterol. Hepatol. 9, 689–692 (1997).
Mertz, H., Naliboff, B., Munakata, J., Niazi, N. & Mayer, E. A. Altered rectal perception is a biological marker of patients with irritable bowel syndrome. Gastroenterology 109, 40–52 (1995).
Naliboff, B. D. et al. Evidence for two distinct perceptual alterations in irritable bowel syndrome. Gut 41, 505–512 (1997).
Bouin, M. et al. Rectal distention testing in patients with irritable bowel syndrome: sensitivity, specificity, and predictive values of pain sensory thresholds. Gastroenterology 122, 1771–1777 (2002).
Ludidi, S. et al. Rectal hypersensitivity as hallmark for irritable bowel syndrome: defining the optimal cutoff. Neurogastroenterol. Motil. 24, 729–733 (2012).
Delvaux, M. Do we need to perform rectal distention tests to diagnose IBS in clinical practice? Gastroenterology 122, 2075–2078 (2002).
Kim, E. S. et al. Colonoscopy as an adjunctive method for the diagnosis of irritable bowel syndrome: focus on pain perception. J. Gastroenterol. Hepatol. 25, 1232–1238 (2010).
Lembo, A. J. et al. Use of serum biomarkers in a diagnostic test for irritable bowel syndrome. Aliment. Pharmacol. Ther. 29, 834–842 (2009).
Jones, M. P. et al. A biomarker panel and psychological morbidity differentiates the irritable bowel syndrome from health and provides novel pathophysiological leads. Aliment. Pharmacol. Ther. 39, 426–437 (2014).
Ahmed, I., Greenwood, R., Costello Bde, L., Ratcliffe, N. M. & Probert, C. S. An investigation of fecal volatile organic metabolites in irritable bowel syndrome. PLoS ONE 8, e58204 (2013).
Öhman, L., Stridsberg, M., Isaksson, S., Jerlstad, P. & Simren, M. Altered levels of fecal chromogranins and secretogranins in IBS: relevance for pathophysiology and symptoms? Am. J. Gastroenterol. 107, 440–447 (2012).
Camilleri, M. Editorial: fecal granins in IBS: cause or indicator of intestinal or colonic irritation? Am. J. Gastroenterol. 107, 448–450 (2012).
Cremon, C. et al. Mucosal immune biomarkers in patients with irritable bowel syndrome [abstract 843]. Gastroenterology 144 (Suppl. 1), S150 (2013).
Cremon, C. et al. Mucosal immune activation in irritable bowel syndrome: gender-dependence and association with digestive symptoms. Am. J. Gastroenterol. 104, 392–400 (2009).
Akbar, A. et al. Increased capsaicin receptor TRPV1-expressing sensory fibres in irritable bowel syndrome and their correlation with abdominal pain. Gut 57, 923–929 (2008).
Kiesslich, R. et al. Identification of epithelial gaps in human small and large intestine by confocal endomicroscopy. Gastroenterology 133, 1769–1778 (2007).
Turcotte, J. F. et al. Breaks in the wall: increased gaps in the intestinal epithelium of irritable bowel syndrome patients identified by confocal laser endomicroscopy (with videos). Gastrointest. Endosc. 77, 624–630 (2013).
Liu, J. J. et al. Increased epithelial gaps in the small intestines of patients with inflammatory bowel disease: density matters. Gastrointest. Endosc. 73, 1174–1180 (2011).
Jones, R., Latinovic, R., Charlton, J. & Gulliford, M. Physical and psychological co-morbidity in irritable bowel syndrome: a matched cohort study using the General Practice Research Database. Aliment. Pharmacol. Ther. 24, 879–886 (2006).
Marshall, S., Haywood, K. & Fitzpatrick, R. Impact of patient-reported outcome measures on routine practice: a structured review. J. Eval. Clin. Pract. 12, 559–568 (2006).
Spiegel, B. M. et al. Understanding gastrointestinal distress: a framework for clinical practice. Am. J. Gastroenterol. 106, 380–385 (2011).
Spiegel, B. M. Patient-reported outcomes in gastroenterology: clinical and research applications. J. Neurogastroenterol. Motil. 19, 137–148 (2013).
Bellentani, S. et al. A simple score for the identification of patients at high risk of organic diseases of the colon in the family doctor consulting room. The Local IBS Study Group. Fam. Pract. 7, 307–312 (1990).
Kato, K., Sullivan, P. F. & Pedersen, N. L. Latent class analysis of functional somatic symptoms in a population-based sample of twins. J. Psychosom. Res. 68, 447–453 (2010).
Schur, E. A. et al. Feeling bad in more ways than one: comorbidity patterns of medically unexplained and psychiatric conditions. J. Gen. Intern. Med. 22, 818–821 (2007).
O'Neill, S. & Brady, R. R. Colorectal smartphone apps: opportunities and risks. Colorectal Dis. 14, e530–e534 (2012).
Author information
Authors and Affiliations
Contributions
All authors contributed equally to all aspects of this manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Sood, R., Law, G. & Ford, A. Diagnosis of IBS: symptoms, symptom-based criteria, biomarkers or 'psychomarkers'?. Nat Rev Gastroenterol Hepatol 11, 683–691 (2014). https://doi.org/10.1038/nrgastro.2014.127
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrgastro.2014.127
This article is cited by
-
A novel stepwise integrative analysis pipeline reveals distinct microbiota-host interactions and link to symptoms in irritable bowel syndrome
Scientific Reports (2021)
-
Gluten-induced symptoms in diarrhea-predominant irritable bowel syndrome are associated with increased myosin light chain kinase activity and claudin-15 expression
Laboratory Investigation (2017)
-
Specific immunotherapy plus Clostridium butyricum alleviates ulcerative colitis in patients with food allergy
Scientific Reports (2016)
-
Microscopic colitis in patients with Takayasu’s arteritis: a potential association between the two disease entities
Clinical Rheumatology (2016)