Key Points
-
Piecemeal endoscopic mucosal resection (PEMR) for complex colorectal polyps is an established technique with good outcomes compared with traditional surgery
-
Patient preparation and careful lesion assessment are essential to achieving good endoscopic resection outcomes for large, complex colorectal polyps
-
Colorectal endoscopic submucosal dissection (ESD) is more complex and has higher risks than PEMR but has the potential to provide an en bloc specimen for accurate histological assessment and reduced recurrence
-
ESD is the procedure of choice for endoscopically resectable lesions that have a high risk of containing very early submucosally invasive cancer
-
New devices and endoscopic platforms to make ESD safer, technically easier and quicker are under development
Abstract
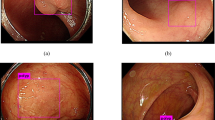
Almost all large and complex colorectal polyps can now be resected endoscopically. Piecemeal endoscopic mucosal resection (PEMR) is an established technique with fairly low complication risk and good short-term and medium-term outcomes. Several modifications to the basic injection and snare technique have been developed contributing to safer and more complete resections. Delayed bleeding requiring reintervention is the most troublesome complication in 2–7% of patients, particularly in those with comorbidities and large, right-sided polyps. Endoscopic submucosal dissection (ESD) has become popular in Japan and has theoretical advantages over PEMR in providing a complete, en bloc excision for accurate histological staging and reduced local recurrence. These advantages come at the cost of a more complex, expensive and time-consuming procedure with a higher risk of perforation, particularly early in the procedure learning curve. These factors have contributed to the slow adoption of ESD in the West and the challenge to develop new devices and endoscopic platforms that will make ESD easier and safer. Currently, ESD indications are limited to large rectal lesions, in which procedural complications are easily managed, and for colorectal polyps with a high risk of containing tiny foci of early submucosally invasive cancer, whereby ESD may be curative compared with PEMR.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Ahlenstiel, G. et al. Actual endoscopic versus predicted surgical mortality for treatment of advanced mucosal neoplasia of the colon. Gastrointest. Endosc. 80, 668–676 (2014).
Pabby, A. et al. Analysis of colorectal cancer occurrence during surveillance colonoscopy in the dietary Polyp Prevention Trial. Gastrointest. Endosc. 61, 385–391 (2005).
Logan, R. F. et al. Outcomes of the Bowel Cancer Screening Programme (BCSP) in England after the first 1 million tests. Gut 61, 1439–1446 (2012).
Carden, A. B. & Morson, B. C. Recurrence after local excision of malignant polyps of the rectum. Proc. R. Soc. Med. 57, 559–561 (1964).
Shirai, M., Nakamura, T., Matsuura, A., Ito, Y. & Kobayashi, S. Safer colonoscopic polypectomy with local submucosal injection of hypertonic saline-epinephrine solution. Am. J. Gastroenterol. 89, 334–338 (1994).
Lee, T. J. W. et al. Management of large sessile or flat colonic polyps in the English bowel cancer screening programme. Br. J. Surg. 100, 1633–1639 (2013).
Moss, A. et al. Endoscopic mucosal resection outcomes and prediction of submucosal cancer from advanced colonic mucosal neoplasia. Gastroenterology 140, 1909–1918 (2011).
Buchner, A. M., Guarner-Argente, C. & Ginsberg, G. G. Outcomes of EMR of defiant colorectal lesions directed to an endoscopy referral center. Gastrointest. Endosc. 76, 255–263 (2012).
Binmoeller, K. F., Weilert, F., Shah, J., Bhat, Y. & Kane, S. 'Underwater' EMR without submucosal injection for large sessile colorectal polyps (with video). Gastrointest. Endosc. 75, 1086–1091 (2012).
Pimentel-Nunes, P. et al. Endoscopic submucosal dissection: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy 47, 829–854 (2015).
Tanaka, S. et al. JGES guidelines for colorectal endoscopic submucosal dissection/endoscopic mucosal resection. Dig. Endosc. 27, 417–434 (2015).
Saito, Y. et al. Clinical outcome of endoscopic submucosal dissection versus endoscopic mucosal resection of large colorectal tumors as determined by curative resection. Surg. Endosc. 24, 343–352 (2010).
Repici, A. et al. Efficacy and safety of endoscopic submucosal dissection for colorectal neoplasia: a systematic review. Endoscopy 44, 137–150 (2012).
Heldwein, W. et al. The Munich Polypectomy Study (MUPS): prospective analysis of complications and risk factors in 4000 colonic snare polypectomies. Endoscopy 37, 1116–1122 (2005).
Lee, E. J. et al. Clinical risk factors for perforation during endoscopic submucosal dissection (ESD) for large-sized, nonpedunculated colorectal tumors. Surg. Endosc. 26, 1587–1594 (2012).
Ramirez, J. M., Aguilella, V., Arribas, D. & Martinez, M. Transanal full-thickness excision of rectal tumours: should the defect be sutured? A randomized controlled trial. Colorectal Dis. 4, 51–55 (2002).
Saito, Y., Sakamoto, T., Nakajima, T. & Matsuda, T. Colorectal ESD: current indications and latest technical advances. Gastrointest. Endosc. Clin. N. Am. 24, 245–255 (2014).
Deprez, P. H. et al. Current practice with endoscopic submucosal dissection in Europe: position statement from a panel of experts. Endoscopy 42, 853–858 (2010).
Hayashi, N. et al. Endoscopic prediction of deep submucosal invasive carcinoma: validation of the narrow-band imaging international colorectal endoscopic (NICE) classification. Gastrointest. Endosc. 78, 625–632 (2013).
Hayashi, N. et al. Relationship between narrow-band imaging magnifying observation and pit pattern diagnosis in colorectal tumors. Digestion 87, 53–58 (2013).
Matsuda, T. et al. Efficacy of the invasive/non-invasive pattern by magnifying chromoendoscopy to estimate the depth of invasion of early colorectal neoplasms. Am. J. Gastroenterol. 103, 2700–2706 (2008).
Probst, A., Golger, D., Anthuber, M., Märkl, B. & Messmann, H. Endoscopic submucosal dissection in large sessile lesions of the rectosigmoid: learning curve in a European center. Endoscopy 44, 660–667 (2012).
Fujiya, M. et al. Efficacy and adverse events of EMR and endoscopic submucosal dissection for the treatment of colon neoplasms: a meta-analysis of studies comparing EMR and endoscopic submucosal dissection. Gastrointest. Endosc. 81, 583–595 (2015).
Kantsevoy, S. V. et al. Endoscopic mucosal resection and endoscopic submucosal dissection. Gastrointest. Endosc. 68, 11–18 (2008).
Kaimakliotis, P. Z. & Chandrasekhara, V. Endoscopic mucosal resection and endoscopic submucosal dissection of epithelial neoplasia of the colon. Expert Rev. Gastroenterol. Hepatol. 8, 521–531 (2014).
Wang, J. et al. Endoscopic submucosal dissection versus endoscopic mucosal resection for colorectal tumors: a meta-analysis. World J. Gastroenterol. 20, 8282–8287 (2014).
Iacopini, F. et al. Stepwise training in rectal and colonic endoscopic submucosal dissection with differentiated learning curves. Gastrointest. Endosc. 76, 1188–1196 (2012).
Cohen, L. B. Advances in bowel preparation for colonoscopy. Gastrointest. Endosc. Clin. N. Am. 25, 183–197 (2015).
Anderson, M. A. et al. Management of antithrombotic agents for endoscopic procedures. Gastrointest. Endosc. 70, 1060–1070 (2009).
Boustiere, C. et al. Endoscopy and antiplatelet agents. European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy 43, 445–461 (2011).
Veitch, A. M. et al. Endoscopy in patients on antiplatelet or antocoagulant therapy, including direct oral anticoagulants: British Society of Gastroenterology (BSG) and European Society of Gastrointestinal Endoscopy (ESGE) guidelines. Gut 65, 374–389 (2016).
Shalman, D. & Gerson, L. B. Systematic review with meta-analysis: the risk of gastrointestinal haemorrhage post-polypectomy in patients receiving anti-platelet, anti-coagulant and/or thienopyridine medications. Aliment. Pharmacol. Ther. 42, 949–956 (2015).
Bassan, M. S. et al. Carbon dioxide insufflation reduces number of postprocedure admissions after endoscopic resection of large colonic lesions: a prospective cohort study. Gastrointest. Endosc. 77, 90–95 (2013).
Maple, J. T. et al. Methods of luminal distention for colonoscopy. Gastrointest. Endosc. 77, 519–525 (2013).
Longcroft-Wheaton, G., Duku, M., Mead, R., Basford, P. & Bhandari, P. Risk stratification system for evaluation of complex polyps can predict outcomes of endoscopic mucosal resection. Dis. Colon Rectum 56, 960–966 (2013).
Yoshikane, H., Hidano, H., Sakakibara, A., Niwa, Y. & Goto, H. Efficacy of a distal attachment in endoscopic resection of colorectal polyps situated behind semilunar folds. Endoscopy 33, 440–442 (2001).
Tsiamoulos, Z. P. & Saunders, B. P. A new accessory, endoscopic cuff, improves colonoscopic access for complex polyp resection and scar assessment in the sigmoid colon (with video). Gastrointest. Endosc. 76, 1242–1245 (2012).
Mönkemüller, K. et al. Diagnostic and therapeutic impact of double-balloon enteroscopy. Endoscopy 38, 67–72 (2006).
Uraoka, T. et al. Endoscopic indications for endoscopic mucosal resection of laterally spreading tumours in the colorectum. Gut 55, 1592–1597 (2006).
Yoda, Y. et al. A large scale multicenter study of long-term outcomes after endoscopic resection for submucosal invasive colorectal cancer. Endoscopy 45, 718–724 (2013).
Participants in the Paris Workshop. The Paris endoscopic classification of superficial neoplastic lesions: esophagus, stomach, and colon. Gastrointest. Endosc. 58, S2–S43 (2003).
Kethu, S. R. et al. Endoscopic tattooing. Gastrointest. Endosc. 72, 681–685 (2010).
Elarini, T., Wexner, S. D. & Isenberg, G. A. The need for standardization of colonoscopic tattooing of colonic lesions. Dis. Colon Rectum 58, 264–267 (2015).
Kudo, S. et al. Colorectal tumours and pit pattern. J. Clin. Pathol. 47, 880–885 (1994).
Kaminski, M. F. et al. Advanced imaging for detection and differentiation of colorectal neoplasia: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy 46, 435–457 (2014).
Kato, H. et al. Lifting of lesions during endoscopic mucosal resection (EMR) of early colorectal cancer: implications for the assessment of respectability. Endoscopy 33, 568–573 (2001).
Kobayashi, N. et al. Determining the treatment strategy for colorectal neoplastic lesions: endoscopic assessment or the non-lifting sign for diagnosing invasion depth? Endoscopy 39, 701–705 (2007).
Kim, H. G., Thosani, N., Banerjee, S., Chen, A. & Friedland, S. Effect of prior biopsy sampling, tattoo placement, and snare sampling on endoscopic resection of large nonpedunculated colorectal lesions. Gastrointest. Endosc. 81, 204–213 (2015).
Pohl, H. et al. Incomplete polyp resection during colonoscopy-results of the complete adenoma resection (CARE) study. Gastroenterology 144, 74–80.e1 (2013).
Tsiamoulos, Z. P., Bourikas, L. A. & Saunders, B. P. Endoscopic mucosal ablation: a new argon plasma coagulation/injection technique to assist complete resection of recurrent, fibrotic colon polyps (with video). Gastrointest. Endosc. 75, 400–404 (2012).
Lee, S. P. et al. Effect of submucosal fibrosis on endoscopic submucosal dissection of colorectal tumors: pathologic review of 173 cases. J. Gastroenterol. Hepatol. 30, 872–878 (2015).
Fujishiro, M. et al. Comparison of various submucosal injection solutions for maintaining mucosal elevation during endoscopic mucosal resection. Endoscopy 36, 579–583 (2004).
Polymeros, D. et al. Comparative performance of novel solutions for submucosal injection in porcine stomachs: an ex vivo study. Dig. Liver Dis. 42, 226–229 (2010).
Moss, A., Bourke, M. J. & Metz, A. J. A randomized, double-blind trial of succinylated gelatin submucosal injection for endoscopic resection of large sessile polyps of the colon. Am. J. Gastroenterol. 105, 2375–2382 (2010).
Fujishiro, M. et al. Tissue damage of different submucosal injection solutions for EMR. Gastrointest. Endosc. 62, 933–942 (2005).
Lee, S. H. et al. Comparison of polypectomy bleeding between epinephrine and saline submucosal injection for large colon polyps by conventional polypectomy: a prospective randomized, multicenter study. World J. Gastroenterol. 13, 2973–2977 (2007).
Dobrowolski, S., Dobosz, M., Babicki, A., Dymecki, D. & Hac, S. Prophylactic submucosal saline-adrenaline injection in colonoscopic polypectomy: prospective randomized study. Surg. Endosc. 18, 990–993 (2004).
Hsieh, Y. H. et al. Is submucosal epinephrine injection necessary before polypectomy? A prospective, comparative study. Hepatogastroenterology 48, 1379–1382 (2001).
ASGE Technology Committee et al. Endoscopic mucosal resection. Gastrointest. Endosc. 82, 215–226 (2015).
Moss, A. et al. Succinylated gelatin substantially increases en bloc resection size in colonic EMR: a randomized, blinded trial in a porcine model. Gastrointest. Endosc. 71, 589–595 (2010).
Turner, J., Green, J. & Dolwani, S. Use of gelofusine for endoscopic mucosal resection. Gut 59, 1446–1447 (2010).
Moss, A. et al. Lesion isolation by circumferential submucosal incision prior to endoscopic mucosal resection (CSI-EMR) substantially improves en bloc resection rates for 40-mm colonic lesions. Endoscopy 42, 400–404 (2010).
Katsinelos, P. et al. A comparative study of 50% dextrose and normal saline solution on their ability to create submucosal fluid cushions for endoscopic resection of sessile rectosigmoid polyps. Gastrointest. Endosc. 68, 692–698 (2008).
Hirasaki, S. et al. Usefulness and safety of 0.4% sodium hyaluronate solution as a submucosal fluid 'cushion' for endoscopic resection of colorectal mucosal neoplasms: a prospective multi-center open-label trial. BMC Gastroenterol. 9, 1 (2009).
Woodward, T., Crook, J. E., Raimondo, M. & Wallace, M. Improving complete EMR of colorectal neoplasia: a randomized trial comparing snares and injectate in the resection of large sessile colon polyps. Gastrointest. Endosc. 81, 673–681 (2015).
Saunders, B. P. 'How I Do it'. Removing large or sessile colonic polyps. World Endoscopy Organization (2005–2016).
Anderloni, A., Jovani, M., Hassan, C. & Repici, A. Advances, problems, and complications of polypectomy. Clin. Exp. Gastroenterol. 7, 285–296 (2014).
Rey, J. F., Beilenhoff, U., Neumann, C. S. & Dumonceau, J. M. European Society of Gastrointestinal Endoscopy (ESGE) guideline: the use of electrosurgical units. Endoscopy 42, 764–772 (2010).
Morris, M. L., Tucker, R. D., Baron, T. H. & Song, L. M. Electrosurgery in gastrointestinal endoscopy: principles to practice. Am. J. Gastroenterol. 104, 1563–1574 (2009).
Parra-Blanco, A. et al. Colonoscopic polypectomy with cutting current: is it safe? Gastrointest. Endosc. 51, 676–681 (2000).
Van Gossum, A., Cozzoli, A., Adler, M., Taton, G. & Cremer, M. Colonoscopic snare polypectomy: analysis of 1485 resections comparing two types of current. Gastrointest. Endosc. 38, 472–475 (1992).
Chino, A. et al. A comparison of depth of tissue injury caused by different modes of electrosurgical current in a pig colon model. Gastrointest. Endosc. 59, 374–379 (2004).
Ah Soune, P. et al. Large endoscopic mucosal resection for colorectal tumors exceeding 4 cm. World J. Gastroenterol. 16, 588–595 (2010).
Brooker, J. C. et al. Treatment with argon plasma coagulation reduces recurrence after piecemeal resection of large sessile colonic polyps: a randomized trial and recommendations. Gastrointest. Endosc. 55, 371–375 (2002).
Zlatanic, J., Waye, J. D., Kim, P. S., Baiocco, P. J. & Gleim, G. W. Large sessile colonic adenomas: use of argon plasma coagulator to supplement piecemeal snare polypectomy. Gastrointest. Endosc. 49, 731–735 (1999).
Regula, J. et al. Argon plasma coagulation after piecemeal polypectomy of sessile colorectal adenomas: long-term follow-up study. Endoscopy 35, 212–218 (2003).
Kim, E. S. et al. Factors predictive of perforation during endoscopic submucosal dissection for the treatment of colorectal tumors. Endoscopy 43, 573–578 (2011).
Tsiamoulos, Z. P. et al. Augmented endoscopic resection for fibrotic or recurrent colonic polyps using an ablation and cold avulsion technique. Endoscopy http://dx.doi.org/10.1055/s-0042-109601 (2016).
Bahin, F. F. et al. Prophylactic endoscopic coagulation to prevent bleeding after wide-field endoscopic mucosal resection of large sessile colon polyps. Clin. Gastroenterol. Hepatol. 13, 724–730.e2 (2015).
Lee, C. K. et al. Prophylactic argon plasma coagulation ablation does not decrease delayed postpolypectomy bleeding. Gastrointest. Endosc. 70, 353–361 (2009).
Ono, S. et al. Endoscopic submucosal dissection for colonic laterally spreading tumours is difficult after target tattooing. Gastrointest. Endosc. 69, 763–766 (2009).
Curcio, G. et al. Underwater colorectal EMR: remodeling endoscopic mucosal resection. Gastrointest. Endosc. 81, 1238–1242 (2015).
Wang, A. Y. et al. Underwater endoscopic mucosal resection of colorectal neoplasia is easily learned, efficacious, and safe. Surg. Endosc. 28, 1348–1354 (2014).
Kim, H. G., Thosani, N., Banerjee, S., Chen, A. & Friedland, S. Underwater endoscopic mucosal resection for recurrences after previous piecemeal resection of colorectal polyps (with video). Gastrointest. Endosc. 80, 1094–1102 (2014).
Winawer, S. J. et al. Guidelines for colonoscopy surveillance after polypectomy: a consensus update by the US Multi-Society Task Force on Colorectal Cancer and the American Cancer Society. Gastroenterology 130, 1872–1885 (2006).
Atkin, W. S. & Saunders, B. P. Surveillance guidelines after removal of colorectal adenomatous polyps. Gut 51, v6–v9 (2002).
Belderbos, T. D. G., Leenders, M., Moons, L. M. G. & Siersema, P. D. Local recurrence after endoscopic mucosal resection of nonpedunculated colorectal lesions: systematic review and meta-analysis. Endoscopy 46, 388–400 (2014).
Knabe, M. et al. Standardized long-term follow-up after endoscopic resection of large, nonpedunculated colorectal lesions: a prospective two-center study. Am. J. Gastroenterol. 109, 183–189 (2014).
Paspatis, G. et al. Diagnosis and management of iatrogenic endoscopic perforations: European Society of Gastrointestinal Endoscopy (ESGE) Position Statement. Endoscopy 46, 693–711 (2014).
Swan, M. P. et al. The target sign: an endoscopic marker for the resection of the muscularis propria and potential perforation during colonic endoscopic mucosal resection. Gastrointest. Endosc. 73, 79–85 (2011).
Burgess, N. G. et al. A management algorithm based on delayed bleeding after wide-field endoscopic mucosal resection of large colonic lesions. Clin. Gastroenterol. Hepatol. 12, 1525–1533 (2014).
Burgess, N. G. et al. A management algorithm based on delayed bleeding after wide-field endoscopic mucosal resection of large colonic lesions. Clin. Gastroenterol. Hepatol. 12, 1525–1533 (2014).
Metz, A. J. et al. Factors that predict bleeding following endoscopic mucosal resection of large colonic lesions. Endoscopy 43, 506–511 (2011).
Sorbi, D. et al. Postpolypectomy lower GI bleeding: descriptive analysis. Gastrointest. Endosc. 51, 690–696 (2000).
Buddingh, K. T. et al. Location in the right hemi-colon is an independent risk factor for delayed post-polypectomy hemorrhage: a multi-center case-control study. Am. J. Gastroenterol. 106, 1119–1124 (2011).
Sawhney, M. S., Salfiti, N., Nelson, D. B., Lederle, F. A. & Bond, J. H. Risk factors for severe delayed postpolypectomy bleeding. Endoscopy 40, 115–119 (2008).
Rutter, M. D., Nickerson, C., Rees, C. J., Patnick, J. & Blanks, R. G. Risk factors for adverse events related to polypectomy in the English Bowel Cancer Screening Programme. Endoscopy 46, 90–97 (2014).
Tsiamoulos, Z. et al. Predicting delayed bleeding after piecemeal Endoscopic Mucosal Resection of complex colorectal polyps. Gastrointest. Endosc. 83 (Suppl.), AB200 (2016).
Liaquat, H., Rohn, E. & Rex, D. K. Prophylactic clip closure reduced the risk of delayed postpolypectomy hemorrhage: experience in 277 clipped large sessile or flat colorectal lesions and 247 control lesions. Gastrointest. Endosc. 77, 401–407 (2013).
Bahin, F. F. et al. Prophylactic endoscopic coagulation to prevent bleeding after wide-field endoscopic mucosal resection of large sessile colon polyps. Clin. Gastroenterol. Hepatol. 13, 724–730 (2015).
Swan, M. P., Bourke, M. J., Alexander, S., Moss, A. & Williams, S. J. Large refractory colonic polyps: is it time to change our practice? A prospective study of the clinical and economic impact of a tertiary referral colonic mucosal resection and polypectomy service (with videos). Gastrointest. Endosc. 70, 1128–1136 (2009).
Tanaka, S., Oka, S., Chayama, K. & Kawashima, K. Knack and practical technique of colonoscopic treatment focused on endoscopic mucosal resection using snare. Dig. Endosc. 21, S38–S42 (2009).
Holt, B. A. & Bourke, M. J. Wide field endoscopic resection for advanced colonic mucosal neoplasia: current status and future directions. Clin. Gastroenterol. Hepatol. 10, 969–979 (2012).
Oka, S. et al. Local recurrence after endoscopic resection for large colorectal neoplasia: a multicenter prospective study in Japan. Am. J. Gastroenterol. 110, 697–707 (2015).
Lee, E. J., Lee, J. B., Lee, S. H. & Youk, E. G. Endoscopic treatment of large colorectal tumors: comparison of endoscopic mucosal resection, endoscopic mucosal resection-precutting, and endoscopic submucosal dissection. Surg. Endosc. 26, 2220–2230 (2012).
Moss, A. et al. Long-term adenoma recurrence following wide-field endoscopic mucosal resection (WF-EMR) for advanced colonic mucosal neoplasia is infrequent: results and risk factors in 1000 cases from the Australian Colonic EMR (ACE) study. Gut 64, 57–65 (2015).
Khashab, M., Eid, E., Rusche, M. & Rex, D. K. Incidence and predictors of 'late' recurrences after endoscopic piecemeal resection of large sessile adenomas. Gastrointest. Endosc. 70, 344–349 (2009).
Woodward, T. A. et al. Predictors of complete endoscopic mucosal resection of flat and depressed neoplasia of the colon. Am. J. Gastroenterol. 107, 650–654 (2012).
Ortiz, A. M., Bhargavi, P., Zuckerman, M. J. & Othman, M. O. Endoscopic mucosal resection recurrence rate for colorectal lesions. South Med. J. 107, 615–621 (2014).
Mannath, J., Subramanian, V., Singh, R., Telakis, E. & Ragunath, K. Polyp recurrence after endoscopic mucosal resection of sessile and flat colonic adenomas. Dig. Dis. Sci. 56, 2389–2395 (2011).
Ono, H. et al. Guidelines for endoscopic submucosal dissection and endoscopic mucosal resection for early gastric cancer. Dig. Endosc. 28, 3–15 (2016).
Miura, Y., Hayashi, Y., Lefor, A. K., Osawa, H. & Yamamoto, H. The pocket-creation method of ESD for gastric neoplasms. Gastrointest. Endosc. 15, 2841–2842 (2015).
Toyonaga, T. et al. Endoscopic treatment for early stage colorectal tumors: the comparison between EMR with small incision, simplified ESD, and ESD using the standard flush knife and the ball tipped flush knife. Acta Chir. Iugosl. 57, 41–46 (2010).
Tanaka, S. et al. Multicenter questionnaire survey on the current situation of colorectal endoscopic submucosal dissection in Japan. Dig. Endosc. 22, S2–S8 (2010).
Yahagi, N. et al. Comparison of standard endoscopic submucosal dissection (ESD) versus an optimized ESD technique for the colon: an animal study. Endoscopy 41, 340–345 (2009).
Low, D. E. et al. Prospective assessment of risk of bacteremia with colonoscopy and polypectomy. Dig. Dis. Sci. 32, 1239–1243 (1987).
Spychalski, M. & Dziki, A. Safe and efficient colorectal endoscopic submucosal dissection in European settings: is successful implementation of the procedure possible? Dig. Endosc. 27, 368–373 (2015).
Nakajima, T. et al. Current status of endoscopic resection strategy for large, early colorectal neoplasia in Japan. Surg. Endosc. 27, 3262–3270 (2013).
Suzuki, S. et al. Risk factors for bleeding after endoscopic submucosal dissection of colorectal neoplasms. World J. Gastroenterol. 21, 1839–1845 (2014).
Terasaki, M. et al. Risk factors for delayed bleeding after endoscopic submucosal dissection for colorectal neoplasms. Int. J. Colorectal Dis. 29, 877–882 (2014).
Cao, Y. et al. Meta-analysis of endoscopic submucosal dissection versus endoscopic mucosal resection for tumors of the gastrointestinal tract. Endoscopy 41, 751–757 (2009).
Toyonaga, T., Man-I. M., Morita, Y. & Azuma, T. Endoscopic submucosal dissection (ESD) versus simplified/hybrid ESD. Gastrointest. Endosc. Clin. N. Am. 24, 191–199 (2014).
Białek, A. et al. Treatment of large colorectal neoplasms by endoscopic submucosal dissection: a European single-center study. Eur. J. Gastroenterol. Hepatol. 26, 607–615 (2014).
Terasaki, M. et al. Clinical outcomes of endoscopic submucosal dissection and endoscopic mucosal resection for laterally spreading tumors larger than 20 mm. J. Gastroenterol. Hepatol. 27, 734–740 (2012).
Fukami, N. ESD around the world: United States. Gastrointest. Endosc. Clin. N. Am. 24, 313–320 (2014).
Neuhaus, H. ESD around the world: Europe. Gastrointest. Endosc. Clin. N. Am. 24, 295–311 (2014).
Othman, M. O. & Wallace, M. B. Endoscopic mucosal resection (EMR) and endoscopic submucosal dissection (ESD) in 2011, a Western perspective. Clin. Res. Hepatol. Gastroenterol. 35, 288–294 (2011).
Farhat, S. et al. Endoscopic submucosal dissection in a European setting. A multi-institutional report of a technique in development. Endoscopy 43, 664–670 (2011).
Hori, K. et al. Predictive factors for technically difficult endoscopic submucosal dissection in the colorectum. Endoscopy 46, 862–870 (2014).
Isomoto, H. et al. Clinicopathological factors associated with clinical outcomes of endoscopic submucosal dissection for colorectal epithelial neoplasms. Endoscopy 41, 679–683 (2009).
Imai, K. et al. Preoperative indicators for failure of en bloc resection or perforation in colorectal endoscopic submucosal dissection: implications for lesion stratification by technical difficulties during stepwise training. Gastrointest. Endosc. 83, 954–962 (2016).
Sato, K. et al. Factors affecting the technical difficulty and clinical outcome of endoscopic submucosal dissection for colorectal tumors. Surg. Endosc. 28, 2959–2965 (2014).
Niimi, K. et al. Long-term outcomes of endoscopic submucosal dissection for colorectal epithelial neoplasms. Endoscopy 42, 723–729 (2010).
Saito, Y. et al. A prospective, multicenter study of 1111 colorectal endoscopic submucosal dissections (with video). Gastrointest. Endosc. 72, 1217–1225 (2010).
Sakamoto, T. Y., Fukunaga, S., Nakajima, T. & Matsuda, T. Learning curve associated with colorectal endoscopic submucosal dissection for endoscopists experienced in gastric endoscopic submucosal dissection. Dis. Colon Rectum 54, 1307–1312 (2011).
Tsiamoulos, Z. P. et al. A new instrumental platform for Trans-Anal Submucosal Endoscopic Resection (TASER). Gut 64, 1844–1846 (2015).
Tsiamoulos, Z. P., Warusavitarne, J. & Saunders, B. P. Transanal submucosal endoscopic resection: a new endosurgical approach to the resection of giant rectal lesions. Endoscopy 46 (Suppl. 1), E401–E402 (2014).
Saito, Y. et al. A new sinker-assisted endoscopic submucosal dissection for colorectal cancer. Gastrointest. Endosc. 62, 297–301 (2005).
Gotoda, T. et al. Prospective clinical trial of magnetic-anchor-guided endoscopic submucosal dissection for large early gastric cancer (with videos). Gastrointest. Endosc. 69, 10–15 (2009).
Sakamoto, N. et al. Endoscopic submucosal dissection of large colorectal tumors by using a novel spring-action S-O clip for traction (with video). Gastrointest. Endosc. 69, 1370–1374 (2009).
Phee, S. J. et al. Robot-assisted endoscopic submucosal dissection is effective in treating patients with early-stage gastric neoplasia. Clin. Gastroenterol. Hepatol. 10, 1117–1121 (2012).
von Renteln, D. et al. Endoscopic submucosal dissection with a flexible Maryland dissector: randomized comparison of mesna and saline solution for submucosal injection (with videos). Gastrointest. Endosc. 74, 906–911 (2011).
Saunders, B. P., Tsiamoulos, Z. P., Bourikas, L. A., Sibbons, P. D. & Hancock, C. P. The 'speedboat': a new multi-modality instrument for endoscopic resection in the gastrointestinal tract. Gastrointest. Endosc. 62, A25 (2013).
Tsiamoulos, Z. P., Sibbons, P., Morris, S., Hancock, C. P. & Saunders, B. P. A novel multimodality endoscopic device for colonic submucosal dissection using a combination of bipolar radiofrequency and microwave modalities. Endoscopy 48, 271–276 (2016).
Rutter, M. D. et al. British Society of Gastroenterology/Association of Coloproctologists of Great Britain and Ireland guidelines for the management of large non-pedunculated colorectal polyps. Gut http://dx.doi.org/10.1136/gutjnl-2015-309576 (2015).
Tanaka, S. et al. Feasibility and safety of endoscopic submucosal dissection for large colorectal tumors. Surg. Laparosc. Endosc. Percutan. Tech. 25, 223–228 (2015).
Acknowledgements
We would like to thank N. Suzuki, A. Wawszczak, A. Polecina and the Multimedia Consultant, S. Preston, for their kind contribution in helping us collect and edit polyp images.
Author information
Authors and Affiliations
Contributions
B.P.S. and Z.P.T. researched data for article, contributed to discussion of content, wrote, reviewed and edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
B.P.S. declares that he received loan equipment, teaching support and consultancy from Olympus, as well as loan equipment from Aquilant Medical. He is a paid speaker for Boston Scientific and is a paid consultant for Creo Medical. Z.P.T. declares that he has acted as a consultant for Creo Medical.
Rights and permissions
About this article
Cite this article
Saunders, B., Tsiamoulos, Z. Endoscopic mucosal resection and endoscopic submucosal dissection of large colonic polyps. Nat Rev Gastroenterol Hepatol 13, 486–496 (2016). https://doi.org/10.1038/nrgastro.2016.96
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrgastro.2016.96
This article is cited by
-
Comparison of efficiency and safety between dual-clip and rubber band-assisted ESD and conventional ESD for colonic lateral spreading tumors (LSTs) with different levels of technical difficulty: a retrospective case–control study
BMC Gastroenterology (2022)
-
Efficacy and Safety of Four Different Endoscopic Treatments for Early Esophageal Cancer: a Network Meta-analysis
Journal of Gastrointestinal Surgery (2022)
-
Complex polypectomy in the sigmoid colon using a double-balloon endolumenal intervention platform
Techniques in Coloproctology (2021)
-
Multiparametric MRI-based machine learning models for preoperatively predicting rectal adenoma with canceration
Magnetic Resonance Materials in Physics, Biology and Medicine (2021)
-
Intra-abdominal pressure during endoscopic full-thickness resection comparing manual and automatic control insufflation: a block-randomized porcine study
Surgical Endoscopy (2020)