Abstract
Peritoneal dialysis (PD) has achieved its current position as the most commonly used home-based dialysis therapy—and with patient survival equal to that seen with hemodialysis—despite the use of glucose-based dialysis solutions with high concentrations of glucose, glucose degradation products and lactate, high osmolality, and low pH, features that are harmful both for the peritoneum and the patient. Newer PD solutions with alternative buffers, a higher pH and fewer glucose degradation products, or ones that contain icodextrin or amino acids as osmotic agents, have been introduced in many countries and have been shown to improve peritoneal membrane health and viability. Icodextrin solution enhances fluid and sodium removal, and the once-daily use of icodextrin and/or amino acid solutions can lessen the harmful effects caused by the exposure of the peritoneal membrane to glucose. However, whether the newer PD solutions improve patient survival over the older solutions is not clear. Use of PD therapy, with or without the newer PD solutions, is associated with an improvement in patient survival that is equivalent to that obtained with hemodialysis. Therefore, the conventional glucose-based solutions—despite their known negative features—continue to have a well-established role in PD therapy, particularly in the many countries where the newer PD solutions are not easily available.
Key Points
-
Newer peritoneal dialysis (PD) solutions are less harmful for the peritoneal membrane than are conventional glucose-based solutions
-
Non-glucose-based PD solutions offer some protection against the metabolic effects of peritoneal glucose exposure
-
Icodextrin-based solutions improve fluid and sodium removal during the long (8–12 h) dialysis exchange, particularly in patients with an increased peritoneal solute transport rate
-
No firm evidence is available to support improved patient survival with the newer PD solutions
-
Patient survival on PD, both with conventional and with newer PD solutions, is comparable to survival on hemodialysis
Similar content being viewed by others
Introduction
Peritoneal dialysis (PD) is the leading form of home-based dialysis therapy and is a well-established alternative to hemodialysis for the dialytic treatment of end-stage renal disease. This position was reached using conventional PD solutions that contain glucose as osmotic agent. Glucose has served well as the prototypical osmotic agent in PD for more than four decades because it offers many of the characteristics required—it is a cheap, safe, and effective osmotic agent. However, the nonphysiological composition of conventional glucose-based solutions, including the high concentrations of glucose, glucose degradation products (GDPs) and lactate, the high osmolality, and the low pH, is harmful for the peritoneal membrane and also has untoward systemic effects in the patient. The negative local effects,1,2,3,4 which can in part be attributed to the composition of the solutions, include impairment of mesothelial cell viability, adverse effects on leukocyte recruitment, accelerated angiogenesis and vascular proliferation, and low-grade inflammation, which lead to epithelial-to-mesenchymal transition, fibrosis and thickening of the peritoneal membrane.5,6,7,8,9,10,11 In addition, the high concentration of glucose and GDPs promotes the formation of advanced glycation end products (AGEs), which are deposited within the peritoneal membrane.12,13,14 These changes alter the dialytic properties of the peritoneal membrane and lead to increased peritoneal small solute transport rate (called 'high transport' or—more appropriately—'fast transport') and reduced osmotic conductance (that is, a reduced capacity of each unit of the osmotic agent to generate one unit of peritoneal ultrafiltration); in addition, they cause partial loss of peritoneal ultrafiltration capacity, which leads to fluid retention, left ventricular hypertrophy, heart failure, and an increased risk of cardiovascular morbidity and mortality. These systemic effects of conventional PD solutions are indirect consequences of their impact on the peritoneum. In addition, the absorption of 100–200 g of glucose per day from the solutions worsens metabolic and nutritional problems—such as impaired glucose tolerance, hyperinsulinemia, hyperlipidemia, and, in some patients, abdominal obesity—that burden patients with end-stage renal disease. Moreover, a substantial fraction of GDPs from PD solutions is absorbed from the peritoneal cavity, resulting in the accelerated formation of systemic AGEs.15
Newer PD solutions were developed over the past two decades to avoid the problems associated with conventional solutions, and are more 'biocompatible'. They have fewer negative local and systemic effects than conventional solutions as they have one or more of the following: an alternative osmotic agent, an alternative buffer, a more physiological pH, and/or a reduced content of GDPs. We will refer to the modified glucose-based solutions as low GDP solutions; however, it should be noted that solutions with an alternative osmotic agent also contain fewer, or no, GDPs.
Currently, two commercially available alternatives to glucose as an osmotic agent are available: icodextrin and amino acids (Table 1). Icodextrin (Extraneal® 7.5%, Baxter, Deerfield, IL, USA) is an iso-osmolar mixture of glucose polymers with different molecular weights that are more slowly absorbed than glucose from the peritoneal cavity, mainly via the lymphatics. This solution, which is buffered with lactate, has a low pH, contains no glucose and has a low concentration of GDPs,16 generates peritoneal ultrafiltration rates that are broadly similar to solutions containing 2.27% glucose during the first few hours. However, ultrafiltration continues for several more hours with icodextrin as slow absorption of the oncotic agent prevents the fluid reabsorption that occurs with glucose-based solutions once the glucose has dissipated—making icodextrin particularly suited for long (8–12 h) dwells.17 Concerns about increased levels of circulating icodextrin metabolites, in particular maltose, currently limit the approved use of this solution to one single daily exchange.18 Icodextrin has been widely used for more than a decade—especially in Europe but also in other parts of the world—mainly because of its demonstrated superiority in terms of fluid and sodium removal during the long dwells, particularly in patients with inadequate peritoneal ultrafiltration owing to a high transport status.
Amino acids are the other available alternative osmotic agent (Table 1). The amino acid solution (Nutrineal® 1.1%, Baxter, Deerfield, IL, USA), which is used by fewer patients than is icodextrin, is lactate-buffered, free from glucose and GDPs, and has the equivalent ultrafiltration capacity of fluids containing 1.36% glucose. It was designed to enhance nutrition in malnourished, hypoalbuminemic PD patients as it acts both as a dialysis solution and as a protein source.19,20 It is recommended to restrict its use to one daily exchange to reduce the risk of symptomatic uremia and acidosis.21
The larger family of low GDP solutions comprises glucose-based solutions buffered either with lactate (Balance®, Fresenius, Bad Homburg, Germany; and Gambrosol Trio®, Fresenius, Bad Homburg, Germany), bicarbonate and lactate (Physioneal®, Baxter, Deerfield, IL, USA), or bicarbonate (BicaVera®, Fresenius, Bad Homburg, Germany), contained in a multicompartment bag system to separate out the buffer from the glucose compartment (Table 1). This system allows heat sterilization and storage to occur at a low pH, which minimizes glucose degradation and formation of GDPs,22 and also prevents precipitation following the mixing of a bicarbonate buffer with magnesium and calcium. After mixing, the solution has a neutral or close to neutral pH.
A growing number of studies are investigating the local and systemic effects of newer PD solutions. In this brief Review, conventional and newer PD solutions are compared with regard to their documented impact on the peritoneum and their systemic effects such as removal of sodium and fluid, metabolic alterations, risk of cardiovascular disease and infections, and patient survival.
Local effects on the peritoneal membrane
Glucose has a dose-dependent inhibitory effect on mesothelial cell proliferation23,24,25 that is mediated by oxidative stress.24 Mitochondrial DNA damage also occurs after exposure of human peritoneal mesothelial cells (HPMCs) to glucose.26 The local toxicity of glucose is, in part, related to a variety of GDPs that are formed in PD solutions and may cause mesothelial cell injury.8 However, the different GDPs differ with regard to their toxicity; 3,4-di-deoxyglucosone-3-ene is especially cytotoxic.27 GDP-induced mesothelial cell injury and apoptosis lead to intracellular hydrogen peroxide production and free radical formation, which are inciting events for peritoneal membrane inflammation and injury.28 Moreover, GDPs induce production of the profibrotic cytokine transforming growth factor (TGF)-β, and stimulate vascular endothelial growth factor (VEGF) synthesis in HPMCs.29,30,31,32 TGF-β and VEGF are thought to have key roles in the progressive peritoneal membrane fibrosis and vascular proliferation that is seen with long-term PD.33 Glucose and GDPs promote the formation of AGEs,9 which increase vascular permeability by disruption of the vascular basement membrane as a result of protein cross-linking to basement membrane components or by the activation of the receptor for AGEs (RAGE) on endothelial cells.9 The changes in the peritoneal membrane, induced in part by high levels of glucose and GDPs, initiate a cascade of events that lead to progressive peritoneal membrane injury (Figure 1).11,34
A wealth of in vitro and animal data demonstrate that specific components in conventional PD solutions contribute to peritoneal toxicity; however, confirmatory data in humans are lacking, owing to the challenges of obtaining serial peritoneal membrane biopsies in patients undergoing PD therapy. Therefore, evaluation of peritoneal membrane status has to rely on the measurement of effluent biomarkers such as cancer antigen-125 (CA-125), VEGF, and interleukin (IL)-6 in the dialysate.9
CA-125, a glycoprotein produced by mesothelial cells, is used as a biomarker of mesothelial cell mass in patients on PD.35 The use of conventional PD solutions results in a decrease in dialysate CA-125 concentration with time on PD,9,36,37 and clinical studies have shown that the use of low GDP solutions leads to increased dialysate CA-125 levels compared with use of conventional PD solutions.38,39,40,41,42,43,44,45 However, it is not clear whether the increase in CA-125 level reflects increased mesothelial cell mass or greater synthesis per remaining mesothelial cell. Furthermore, in a prospective 1-year observational study of incident patients using conventional or low GDP solutions published in 2010, increases in dialysate appearance rates of TGF-β, VEGF and IL-6 were seen but no significant changes in dialysate CA-125 levels occurred over time compared with baseline.46 In the absence of studies examining the relationship between effluent CA-125 levels and peritoneal membrane morphology and function, the validity of dialysate CA-125 as a marker of peritoneal membrane health and integrity can be disputed.
VEGF production by HPMCs seems to be stimulated by proinflammatory cytokines and by AGEs such as glycated albumin, and not only by glucose itself.47 High dialysate levels of VEGF have been associated with an increased peritoneal small solute transport rate and increased macromolecular permeability, likely a reflection of an increase in peritoneal vascular surface area.48,49 In animal models, dialysate levels of VEGF, peritoneal VEGF staining, and signs of angiogenesis were reduced with intraperitoneal use of low GDP solutions compared with conventional PD solutions.12 Furthermore, animal studies suggest that low GDP solutions may reduce peritoneal angiogenesis.50 In humans, the impact of low GDP solutions on dialysate levels of VEGF has been investigated in several studies.44,51,52 However, most of these studies did not demonstrate significant differences in dialysate VEGF levels with the different solutions. It is possible that dialysate VEGF level may not only reflect the local peritoneal production but also systemic VEGF levels, as transperitoneal transport of VEGF from the systemic circulation may obscure the picture.53
Dialysate levels of IL-6 are associated with baseline peritoneal transport status and downstream inflammatory factors (such as membrane chemoattractant protein-1, angiogenic factors such as VEGF, and adhesion molecules), which suggests that IL-6 may have a role in the initial induction of peritoneal membrane inflammation.54 However, IL-6 also has anti-inflammatory effects, inducing downregulation of inflammatory cytokines by activation of IL-1 and tumor necrosis factor receptor antagonists. Some studies suggest that dialysate IL-6 levels are reduced when low GDP solutions are used; however, this finding has not been confirmed by other studies.38,43
Some, but not all, studies suggest that icodextrin may preserve the peritoneal membrane and prolong the use of PD over conventional solutions, possibly because it contains no glucose, has a low GDP content, and is iso-osmolar.55,56,57,58 Amino-acid-based dialysis solutions have been reported to result in less mesothelial damage in animals compared with conventional glucose solutions.12,59,60 Although not well studied, some data suggest that amino-acid-based solutions may also have a protective effect on the peritoneal membrane in humans.56
Systemic effects of newer PD solutions
The main systemic effect of PD solutions is that they allow blood purification through diffusive and convective transport, which results in the removal of water and uremic waste products. Important differences exist between the PD solutions as regards to removal of sodium and fluid and effects related to the uptake of the osmotic agent and other components from PD solutions. Some of the potential benefits of the newer PD solutions are summarized in Figure 1.
Sodium and water removal
The removal of sodium and water is as essential in PD therapy as it is in any other dialytic modality. However, inadequate removal of sodium and water and subsequent ultrafiltration failure are major causes of late technique failure in patients undergoing long-term PD.61,62 As a consequence of the longitudinal changes in the peritoneal membrane, its functional properties are altered, and many patients have a gradual increase in the peritoneal small solute transport rate accompanied by a reduction in peritoneal ultrafiltration capacity.63 During long-term PD treatment, ultrafiltration failure occurs in about one-third of patients,64 and contributes to hypertension, fluid overload and left ventricular hypertrophy.65 Overhydration may be exacerbated by inadequate sodium removal during PD.66 Apart from the need to restrict sodium and fluid intake, the key elements needed to optimize the removal of water and sodium in long-term PD patients are to minimize the harmful impact of dialysis solutions on peritoneal ultrafiltration, protect residual renal function (RRF), optimize dialysis regimens, and, if available, consider use of icodextrin.
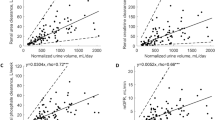
The superiority of icodextrin (over glucose-based solutions) on ultrafiltration has been demonstrated in several studies,67,68,69,70,71,72 and it has been shown to improve control of fluid balance, especially in so-called 'high transporters' (that is, patients with a high peritoneal solute transport rate).71,73 As use of icodextrin during the long dwell can improve fluid balance, it may help anuric patients to be maintained on PD.55 Use of icodextrin has also been shown to preserve RRF, despite the increase of peritoneal ultrafiltration,73,74 although this finding was not reported by other studies.75 Icodextrin use is associated with sustained and improved net ultrafiltration and an increased convective contribution to total small solute clearance, in the absence of free water removal, thereby eliminating the gap between ultrafiltration and sodium removal that is seen with crystalloid osmotic agents.76 Several studies have shown that icodextrin effectively clears small solutes—including sodium—with higher ultrafiltration rates.73,76
Preservation of residual renal function
The ability of GDPs to promote renal tubular apoptosis in cell culture and the established role of AGEs in the induction of glomerulosclerosis and progression of diabetic nephropathy77 led to the hypothesis that the use of a low GDP solution could potentially result in improved preservation of RRF over conventional solutions.77,78 Although some studies have supported this idea,38,39,44,79 others have not shown a significant benefit of low GDP solutions.41,45,80 These conflicting results might, in part, be explained by the use of solutions with different profiles of GDPs in the different studies. In addition, the studies included a heterogeneous mix of both incident and prevalent PD patients.
Metabolic effects
The systemic effects of newer PD fluids, beyond their effect on the peritoneal membrane and its role in the removal of sodium and fluid, are largely determined by the absorption of glucose.81 With the use of conventional PD solutions, about 50–80% of the instilled glucose is absorbed from the peritoneal cavity. In extreme situations, this process can lead to an additional carbohydrate load of more than 300 g per day. This excess of carbohydrates may promote obesity, glucose intolerance, insulin resistance, and an atherogenic lipid profile.65,82
Studies have shown that using icodextrin rather than glucose-based solutions for the long dwell leads to a significant reduction in mean blood glucose level and significantly better control of blood glucose levels in patients with diabetes on PD.83,84,85 It should be noted that blood glucose measurements in patients receiving icodextrin must be performed using a method of glucose determination that is specific for glucose, to avoid interference by maltose, a metabolite of icodextrin; glucose-dehydrogenase-based systems using the pyrroloquinoline quinone method is nonspecific for glucose and must not be used as it results in falsely elevated blood glucose levels.86 Two prospective, multicenter open-label studies reported that a significant reduction in hemoglobin A1c (HbA1c) level can be achieved with the use of icodextrin in patients with diabetes on PD.84,85
The role of glucose absorption in the observed changes in body composition of patients on PD remains controversial. It is well established that patients on PD frequently gain weight, especially during the first year of PD therapy, particularly if they have diabetes or a high body mass index (BMI) at dialysis initiation. However, despite the daily caloric contribution that glucose provides to patients on PD, no major differences in BMI distribution between hemodialysis and PD patients have been identified to date. Obesity, defined as a BMI >30 kg/m2, was independently associated with an increased risk of death and technique failure in a large cohort of patients on PD in Australia and New Zealand;87 by contrast, other researchers have reported that obesity has no association with survival in patients on PD.88,89
The location of fat accumulation has different metabolic implications, with abdominal fat being associated with increased cardiovascular risk in both patients on PD and those on hemodialysis.65,90,91 Interestingly, the increase in truncal fat mass observed over time in patients on PD is associated with a genetic polymorphism of the gene encoding uncoupling protein-2 as well as with circulating levels of leptin, IL-6, and triglycerides, and, inversely, with adiponectin and HDL cholesterol.92 In vitro studies have demonstrated that glucose-based solutions lead to leptin being secreted by adipocytes in a concentration-dependent manner, which is not seen with non-glucose-containing dialysis solutions such as those based on icodextrin or amino acids.93 Two small clinical studies evaluated the effect of icodextrin on plasma leptin levels in mainly nondiabetic patients on PD with opposite results with regard to the direction of changes in leptin levels.94,95 Reasons for this discrepancy are unclear but likely include differences in study design and statistical power.
Uremic dyslipidemia usually worsens with time on PD, with markedly elevated levels of triglycerides, and increases in levels of total cholesterol, LDL cholesterol, lipoprotein(a), and apolipoprotein B. A multicenter 12-month observational study of 51 patients with diabetes on continuous ambulatory peritoneal dialysis (CAPD) using icodextrin for their overnight dwell found a positive correlation between changes in triglyceride levels and glucose absorption; by contrast, total and LDL cholesterol levels and triglyceride levels decreased significantly over the observation period.85 More recently, a randomized controlled trial by Paniagua et al.84 reported that triglyceride levels decreased in diabetic patients on PD treated with icodextrin.
Cardiovascular disease risk
Cardiovascular disease is present in almost all patients initiating dialysis, but may also develop or worsen during chronic dialysis treatment. Aside from the traditional risk factors present in the general population and the risk factors for cardiovascular disease that are associated with end-stage renal disease, patients on PD have additional risk factors for cardiovascular disease, mainly caused by the absorption of glucose from the peritoneal cavity.65
Furthermore, the instillation of a dialysis solution into the peritoneal cavity not only causes an increase in intraperitoneal pressure, but also results in a modest elevation of systemic blood pressure owing to a rise in total peripheral resistance when hypertonic glucose is used.65 Continuous exposure to the high dialysate glucose concentrations leads to the formation of AGEs in peritoneal tissues. Plasma AGE concentrations are higher in both patients on PD and in patients on hemodialysis than they are in healthy individuals, but circulating levels do not differ between patients on the two dialysis modalities.96 Therefore it is unlikely that AGEs generated in peritoneal tissue lead to significant systemic vascular effects,65 although lower plasma AGE concentrations are reported with the use of some low GDP solutions.15,44
Inflammation is an independent risk factor for cardiovascular events and mortality in patients with chronic kidney disease (CKD).97 Moreover, an association between inflammation and an increase in circulating markers of endothelial activation, including soluble vascular cellular adhesion molecule (VCAM)-1 and intercellular adhesion molecule (ICAM)-1, has been found.98 In 2011, Park et al. found that patients receiving low GDP solutions had less elevation of vascular adhesion molecules than did patients using conventional solutions, which could possibly be due to reduced elevation of levels of systemic AGEs in patients treated with low GDP solutions.99 In addition, indirect evidence, such as the fact that a single exposure to GDPs has been shown to induce VCAM-1 expression in cultured human peritoneal mesothelial cells,100 suggests that GDPs have a direct effect on vascular endothelial cells.
It is uncertain whether use of low GDP solutions leads to a reduction in cardiovascular risk factors, but improved preservation of both the peritoneal membrane and potentially also preservation of residual renal function could potentially reduce the risk of ultrafiltration failure.
Overhydration is a well-recognized problem in patients on PD, especially when RRF is lost, leading to left ventricular hypertrophy accompanied by elevated serum concentrations of natriuretic peptides; associations between increased levels of N-terminal pro-brain natriuretic peptide and RRF, cardiovascular congestion, and cardiovascular death are reported in patients on PD.101 The development of overhydration may be exacerbated by the limited capacity for sodium removal during peritoneal dialysis.65,66 Associations between poor peritoneal ultrafiltration and mortality have been reported in anuric patients.62 In this context the use of icodextrin to improve salt and water removal, as discussed above, may be of particular value in anuric patients who have signs of overhydration.
Vascular calcification is an important cause of cardiovascular mortality. PD should improve control of calcium and phosphate as compared to intermittent dialysis owing to improved preservation of RRF and also because of the continuous peritoneal diffusive removal of calcium that occurs when using newer PD solutions with a physiological calcium concentration (1.25 mmol/l) and the convective removal that accompanies sustained peritoneal net ultrafiltration.102 The improved control of calcium enables the increased use of calcium-containing phosphate binders. The provision of dietary protein with intraperitoneal amino acids (around 30% of daily requirement), without the delivered phosphate load attendant with oral complex protein, may improve the nutritional status of malnourished patients on PD.103 Whether use of low GDP solutions, icodextrin-based fluids or amino-acid-based fluids is associated with a clinically significant advantage over use of conventional solutions as regards vascular calcification is, however, not clear.
Peritonitis and infectious complications
Infectious complications are common in patients on dialysis, accounting for about 13% (among older patients) to 21% (among younger patients) of all deaths.104 The high rate of infectious complications in patients on dialysis is a result of the increased susceptibility to infections owing to the immune dysfunction that occurs in uremia as well as the increased risk of exposure to infection via vascular or peritoneal access.105 Local peritoneal immunity has an important role in the prevention and resolution of peritonitis in patients on PD. Following exposure to conventional PD solutions, impaired survival of leukocytes106,107 and peritoneal mesothelial cells108 has been demonstrated. These detrimental effects could be the result of high osmolality,107,109 dialysate acidity and/or high lactate content.109 Low GDP solutions were shown by one study to reduce intraperitoneal inflammation,43 but this finding was not made by other studies,110 and may be associated with improved maintenance of macrophage function. Another study has shown that during long-term clinical use, icodextrin did not result in the deterioration of peritoneal defense determinants more than was seen with glucose; in addition, icodextrin had a beneficial effect on some aspects of the peritoneal defense system—for example, an increase in absolute numbers and percentages of effluent peritoneal macrophages.111 Icodextrin is not associated with altered rate or altered course of peritonitis;112,113 however, during peritonitis, icodextrin-treated patients in general lose less ultrafiltration capacity than do patients on conventional solutions.114 Switching to icodextrin for the long dwell can also better maintain ultrafiltration capacity when patients not previously on icodextrin develop peritonitis.
Low GDP solutions may be associated with improved peritoneal immune function,115 but it is not clear whether they reduce peritonitis rates. A retrospective study of 1,909 incident patients on CAPD showed no difference in peritonitis-free survival rates or peritonitis rates between patients treated with a conventional peritoneal dialysis fluid and patients treated with a low GDP solution, although patient survival was reported to be greater among patients treated with low GDP solutions.116,117 By contrast, three other observational studies have shown peritonitis rates to be lower in patients using low GDP solutions than in those treated with conventional dialysis solutions.118,119,120 A possible explanation for these conflicting results could be that as the patients in the observational studies were not randomized they could therefore have differed in their comorbidities and in other aspects that could have influenced peritonitis risk. Two randomized studies did not show any difference in the peritonitis risk between low GDP and standard solutions,39,80 and another randomized study involving 267 patients also showed no significant difference in the peritonitis rate between groups treated with conventional and low GDP solutions.121 Thus there is still no proof that the use of newer PD solutions reduces the risk of peritonitis. However, infection rates in PD have declined over the past three decades, and more rapidly than the decline in infection rates seen with hemodialysis, owing to advances in the prevention of peritonitis;122 the risk of death caused by infection is now comparable between the two modalities.122
Better survival with newer PD solutions?
Most clinical studies investigating the newer PD solutions have focused on their potential to improve peritoneal membrane morphology and function, ultrafiltration, RRF, and peritonitis rates, whereas only a few studies have looked at survival. Mortality rates among patients on dialysis are declining—more rapidly so among patients on PD than in those on hemodialysis—and survival on PD is now equal to that on hemodialysis.123,124 However, long-term survival in patients on dialysis remains poor. Cardiovascular disease accounts for most patient deaths on dialysis, but so far strategies aimed at reducing some of the modifiable traditional—and nontraditional—cardiovascular risk factors have in general been ineffective in patients on dialysis.125
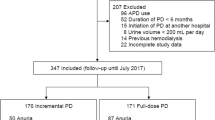
Icodextrin solutions have been used for many years and we now have evidence of their beneficial effects on ultrafiltration and volume control, together with promising data with regards to their effect on RRF.4,71,73,75,84,126,127,128,129 Icodextrin may extend technique survival,62,130,131 but so far no clear evidence exists that it improves patient survival. In a 2-year study, mortality rate was significantly lower in icodextrin-treated patients than in patients not using icodextrin, but the study was not a randomized controlled trial, and the authors considered this finding a coincidence.68 In a study from Japan, the use of icodextrin solution for the long dwell was reported to significantly reduce both mortality and drop-out rate compared with use of conventional solutions.132 A study published in 2011 looked at the effect of icodextrin use on mortality and technique failure in a total of 2,163 patients who initiated PD between July 2003 and December 2006 in 54 included centers in Korea.133 The authors reported that the 640 patients who had been prescribed icodextrin for >50% of their PD duration had improved patient and technique survival compared with patient and technique survival among propensity-score-matched pairs of 640 patients not on icodextrin.133 However, these studies were observational ones, and randomized, controlled trials would be needed to show such an effect.
A study from Hong Kong reported that mortality rate and technique survival were the same in malnourished patients who used conventional PD solution as they were in those who used amino-acid-based solutions for 3 years.134 Two longitudinal observational cohort studies conducted in two single centers, together comprising over 2,000 patients treated with PD, reported that mortality rates were lower in patients who used low GDP solutions than in those who used conventional solutions.116,135 The latter two studies, plus another randomized study that compared clinical outcomes between patients on conventional solutions and those on low GDP solutions,121 showed no differences in technique survival between the groups. In another 3-year prospective, but nonrandomized, study the number of deaths was lower among patients using low GDP solutions than among those using conventional solutions.118 Together, these promising results may suggest that low GDP solutions could contribute to the prolongation of patient lifetime; however prospective, randomized studies are needed to confirm these observations.
Potential future PD solutions
The newer PD solutions are increasingly being used all over the world and in some parts of Europe they have now almost completely replaced conventional solutions. This gradual change has been driven by demonstrated specific properties of the newer solutions such as improved biocompatibility, and, for icodextrin, increased net ultrafiltration particularly in patients with an increased peritoneal solute transport rate. However, we still know too little about the newer PD solutions because large randomized, controlled studies of their effects on clinical outcomes and in particular on patient survival are lacking.
Thus, disappointingly, the use of low GDP solutions has not as yet unequivocally been shown to result in clinically meaningful beneficial effects such as improved peritoneal ultrafiltration, decreased infection rates or the prevention of longitudinal membrane injury.9,136 Demonstrating these potential benefits is challenging and large studies with sufficient follow-up are still awaited. The results of IMPENDIA, a randomized controlled trial investigating whether the use of glucose-sparing PD solutions in patients with diabetes on PD leads to improved metabolic control,137 and BalANZ, a randomized controlled trial investigating whether a low GDP, neutral pH solution is associated with better preservation of RRF over a standard peritoneal dialysis solution,138 are eagerly awaited. According to preliminary results from the latter study reported by David Johnson at the 10th European Peritoneal Dialysis meeting in Birmingham, UK, in October 2011,139 the use of low GDP solutions did not attain the primary end point of preservation of RRF, although this result was borderline significant. However, the time to appearance of first episode of peritonitis was longer with the low GDP solution, and there seemed to be a positive impact on peritoneal membrane transport characteristics (D. Johnson, unpublished work).
In the future, research should focus on developing novel PD solutions that could further improve peritoneal health and viability during long-term PD therapy, and, even more importantly, address the major causes of death in dialysis patients, in particular cardiovascular and infection-related deaths. Some potential future PD solutions are already on the horizon. A recent study suggests that L-carnitine could be used as an osmotic agent in PD solutions,140 and that it could be more than just an alternative to glucose as L-carnitine may reduce glucose-mediated injury to the aquaporin pathway, thus enhancing peritoneal ultrafiltration.141 A novel low-sodium solution was designed to enhance the diffusive removal of sodium; however, use of these solutions requires the addition of glucose (to compensate for the lower osmolality), which could have untoward metabolic consequences.142 Various combinations of osmotic agents have been proposed; for example, a combination of glucose and icodextrin, which enhances sodium and fluid removal in patients on PD.143 In a rat model of chronic kidney failure, a combination of 1.4% glycerol, 0.5% amino acids, and 1.1% dextrose (equal to 1% glucose) (GLAD) was associated with improved preservation of peritoneal morphology compared with a conventional glucose-based solution.144
PD is unique compared with intermittent forms of dialysis in that it allows a continuous supply of substances, potentially including those that are inactivated or short-lived if provided orally. One such compound is pyrophosphate, an endogenous molecule that inhibits soft tissue calcification and has a very short half-life in the circulation and may be present at decreased levels in patients on dialysis; animal studies suggest that this additive in a peritoneal dialysis solution may reduce vascular calcification.145
Conclusions
PD has achieved its current position as the major home-based dialysis therapy—with patient survival rates equal to those seen with hemodialysis—despite the use of glucose-based dialysis solutions that have high concentrations of glucose, GDPs and lactate, high osmolality, and low pH, factors that may be harmful both for the peritoneum and the patient. Newer PD solutions seem to improve at least some aspects of peritoneal membrane health and viability (Figure 1). In addition, newer PD solutions seem to have systemic benefits. Thus, icodextrin solutions may improve functional characteristics of the peritoneal membrane and enhance peritoneal ultrafiltration during the long dwell in patients with intrinsic or acquired rapid solute transfer, with associated cardiovascular benefits. Furthermore, once daily use of icodextrin and/or amino-acid-based solutions can potentially reduce some of the harmful systemic metabolic effects caused by peritoneal glucose adsorption. However, it is still not clear whether the newer PD solutions can improve patient survival; large randomized, controlled trials would be needed to demonstrate such an effect. Therefore, the conventional glucose-based solutions—despite their known negative features—continue to have a well-established role in PD therapy, particularly in the many countries where the newer PD solutions are not available or can only seldom be used because of their higher cost. PD therapy as such, with or without the newer PD solutions, is associated with improving clinical outcomes year by year despite the increasing age of patients and their increasing number of comorbidities. Patient survival on PD is now equivalent—in most countries where this has been studied—to those obtained with hemodialysis.
Review criteria
PubMed was searched using the search terms: “chronic kidney disease”, “dialysis”, “peritoneal dialysis solutions”, “biocompatibility of PD solutions”, “advanced glycation end-products”, “peritoneal membrane”, “ultrafiltration” and “fluid balance”. We mainly selected articles published during the past 10 years but older manuscripts were also selected if they were deemed to be important. In addition, we searched the reference lists of the selected articles for further relevant articles. We searched mainly for articles written in English.
References
Topley, N. Membrane longevity in peritoneal dialysis: impact of infection and bio-incompatible solutions. Adv. Ren. Replace. Ther. 5, 179–184 (1998).
Hoff, C. M. In vitro biocompatibility performance of Physioneal. Kidney Int. Suppl. S57–S74 (2003).
Higuchi, C., Nishimura, H. & Sanaka, T. Biocompatibility of peritoneal dialysis fluid and influence of compositions on peritoneal fibrosis. Ther. Apher. Dial. 10, 372–379 (2006).
McIntyre, C. W. Update on peritoneal dialysis solutions. Kidney Int. 71, 486–490 (2007).
Mortier, S. et al. Effects of conventional and new peritoneal dialysis fluids on leukocyte recruitment in the rat peritoneal membrane. J. Am. Soc. Nephrol. 14, 1296–1306 (2003).
Witowski, J. et al. Effect of glucose degradation products on human peritoneal mesothelial cell function. J. Am. Soc. Nephrol. 11, 729–739 (2000).
Morgan, L. W. et al. Glucose degradation products (GDP) retard remesothelialization independently of D-glucose concentration. Kidney Int. 64, 1854–1866 (2003).
Witowski, J. et al. Prolonged exposure to glucose degradation products impairs viability and function of human peritoneal mesothelial cells. J. Am. Soc. Nephrol. 12, 2434–2441 (2001).
Perl, J., Nessim, S. J. & Bargman, J. M. The biocompatibility of neutral pH, low-GDP peritoneal dialysis solutions: benefit at bench, bedside, or both? Kidney Int. 79, 814–824 (2011).
Selgas, R. et al. Risk factors responsible for ultrafiltration failure in early stages of peritoneal dialysis. Perit. Dial. Int. 20, 631–636 (2000).
Aroeira, L. S. et al. Epithelial to mesenchymal transition and peritoneal membrane failure in peritoneal dialysis patients: pathologic significance and potential therapeutic interventions. J. Am. Soc. Nephrol. 18, 2004–2013 (2007).
Mortier, S., Faict, D., Schalkwijk, C. G., Lameire, N. H. & De Vriese, A. S. Long-term exposure to new peritoneal dialysis solutions: effects on the peritoneal membrane. Kidney Int. 66, 1257–1265 (2004).
Mortier, S., Faict, D., Lameire, N. H. & De Vriese, A. S. Benefits of switching from a conventional to a low-GDP bicarbonate/lactate-buffered dialysis solution in a rat model. Kidney Int. 67, 1559–1565 (2005).
Honda, K. et al. Accumulation of advanced glycation end products in the peritoneal vasculature of continuous ambulatory peritoneal dialysis patients with low ultra-filtration. Nephrol. Dial. Transplant. 14, 1541–1549 (1999).
Zeier, M. et al. Glucose degradation products in PD fluids: do they disappear from the peritoneal cavity and enter the systemic circulation? Kidney Int. 63, 298–305 (2003).
Posthuma, N. et al. Amadori albumin and advanced glycation end-product formation in peritoneal dialysis using icodextrin. Perit. Dial. Int. 21, 43–51 (2001).
Ho-dac-Pannekeet, M. M. et al. Peritoneal transport characteristics with glucose polymer based dialysate. Kidney Int. 50, 979–986 (1996).
Garcia-Lopez, E. & Lindholm, B. Icodextrin metabolites in peritoneal dialysis. Perit. Dial. Int. 29, 370–376 (2009).
Taylor, G. S., Patel, V., Spencer, S., Fluck, R. J. & McIntyre, C. W. Long-term use of 1.1% amino acid dialysis solution in hypoalbuminemic continuous ambulatory peritoneal dialysis patients. Clin. Nephrol. 58, 445–450 (2002).
Jones, M. et al. Treatment of malnutrition with 1.1% amino acid peritoneal dialysis solution: results of a multicenter outpatient study. Am. J. Kidney Dis. 32, 761–769 (1998).
Dombros, N. et al. European best practice guidelines for peritoneal dialysis. 5 Peritoneal dialysis solutions. Nephrol. Dial. Transplant. 20 (Suppl. 9), ix16–ix20 (2005).
Passlick-Deetjen, J. & Lage, C. Lactate-buffered and bicarbonate-buffered solutions with less glucose degradation products in a two-chamber system. Perit. Dial. Int. 20 (Suppl. 2), S42–S47 (2000).
Boulanger, E. et al. The triggering of human peritoneal mesothelial cell apoptosis and oncosis by glucose and glycoxydation products. Nephrol. Dial. Transplant. 19, 2208–2216 (2004).
Ciszewicz, M., Wu, G., Tam, P., Polubinska, A. & Breborowicz, A. Changes in peritoneal mesothelial cells phenotype after chronic exposure to glucose or N-acetylglucosamine. Transl. Res. 150, 337–342 (2007).
Di Paolo, N., Garosi, G., Petrini, G. & Monaci, G. Morphological and morphometric changes in mesothelial cells during peritoneal dialysis in the rabbit. Nephron 74, 594–599 (1996).
Ishibashi, Y. et al. Glucose dialysate induces mitochondrial DNA damage in peritoneal mesothelial cells. Perit. Dial. Int. 22, 11–21 (2002).
Catalan, M. P., Santamaría, B., Reyero, A., Ortiz, A. & Egido, J. 3,4-di-deoxyglucosone-3-ene promotes leukocyte apoptosis. Kidney Int. 68, 1303–1311 (2005).
Noh, H. et al. Oxidative stress during peritoneal dialysis: implications in functional and structural changes in the membrane. Kidney Int. 69, 2022–2028 (2006).
Kang, D. H. et al. High glucose solution and spent dialysate stimulate the synthesis of transforming growth factor-β1 of human peritoneal mesothelial cells: effect of cytokine costimulation. Perit. Dial. Int. 19, 221–230 (1999).
Ha, H., Yu, M. R. & Lee, H. B. High glucose-induced PKC activation mediates TGF-β1 and fibronectin synthesis by peritoneal mesothelial cells. Kidney Int. 59, 463–470 (2001).
Inagi, R. et al. Glucose degradation product methylglyoxal enhances the production of vascular endothelial growth factor in peritoneal cells: role in the functional and morphological alterations of peritoneal membranes in peritoneal dialysis. FEBS Lett. 463, 260–264 (1999).
Leung, J. C. et al. Glucose degradation products downregulate ZO-1 expression in human peritoneal mesothelial cells: the role of VEGF. Nephrol. Dial. Transplant. 20, 1336–1349 (2005).
De Vriese, A. S., Tilton, R. G., Stephan, C. C. & Lameire, N. H. Vascular endothelial growth factor is essential for hyperglycemia-induced structural and functional alterations of the peritoneal membrane. J. Am. Soc. Nephrol. 12, 1734–1741 (2001).
Bajo, M. A. et al. Low-GDP peritoneal dialysis fluid ('balance') has less impact in vitro and ex vivo on epithelial-to-mesenchymal transition (EMT) of mesothelial cells than a standard fluid. Nephrol. Dial. Transplant. 26, 282–291 (2011).
Visser, C. E. et al. Cancer antigen 125: a bulk marker for the mesothelial mass in stable peritoneal dialysis patients. Nephrol. Dial. Transplant. 10, 64–69 (1995).
Krediet, R. T. Dialysate cancer antigen 125 concentration as marker of peritoneal membrane status in patients treated with chronic peritoneal dialysis. Perit. Dial. Int. 21, 560–567 (2001).
Sampimon, D. E. et al. Early diagnostic markers for encapsulating peritoneal sclerosis: a case-control study. Perit. Dial. Int. 30, 163–169 (2010).
Kim, S. et al. Benefits of biocompatible PD fluid for preservation of residual renal function in incident CAPD patients: a 1-year study. Nephrol. Dial. Transplant. 24, 2899–2908 (2009).
Haag-Weber, M. et al. Low-GDP fluid (Gambrosol trio) attenuates decline of residual renal function in PD patients: a prospective randomized study. Nephrol. Dial. Transplant. 25, 2288–2296 (2010).
Rippe, B. et al. Long-term clinical effects of a peritoneal dialysis fluid with less glucose degradation products. Kidney Int. 59, 348–357 (2001).
Choi, H. Y. et al. The clinical usefulness of peritoneal dialysis fluids with neutral pH and low glucose degradation product concentration: an open randomized prospective trial. Perit. Dial. Int. 28, 174–182 (2008).
Haas, S. et al. Improved acidosis correction and recovery of mesothelial cell mass with neutral-pH bicarbonate dialysis solution among children undergoing automated peritoneal dialysis. J. Am. Soc. Nephrol. 14, 2632–2638 (2003).
Fusshoeller, A., Plail, M., Grabensee, B. & Plum, J. Biocompatibility pattern of a bicarbonate/lactate-buffered peritoneal dialysis fluid in APD: a prospective, randomized study. Nephrol. Dial. Transplant. 19, 2101–2106 (2004).
Williams, J. D. et al. The Euro-Balance Trial: the effect of a new biocompatible peritoneal dialysis fluid (balance) on the peritoneal membrane. Kidney Int. 66, 408–418 (2004).
Szeto, C. C. et al. Clinical biocompatibility of a neutral peritoneal dialysis solution with minimal glucose-degradation products—a 1-year randomized control trial. Nephrol. Dial. Transplant. 22, 552–559 (2007).
Cho, J. H. et al. Impact of systemic and local peritoneal inflammation on peritoneal solute transport rate in new peritoneal dialysis patients: a 1-year prospective study. Nephrol. Dial. Transplant. 25, 1964–1973 (2010).
Mandl-Weber, S., Cohen, C. D., Haslinger, B., Kretzler, M. & Sitter, T. Vascular endothelial growth factor production and regulation in human peritoneal mesothelial cells. Kidney Int. 61, 570–578 (2002).
Pecoits-Filho, R. et al. Plasma and dialysate IL-6 and VEGF concentrations are associated with high peritoneal solute transport rate. Nephrol. Dial. Transplant. 17, 1480–1486 (2002).
van Esch, S. et al. Determinants of peritoneal solute transport rates in newly started nondiabetic peritoneal dialysis patients. Perit. Dial. Int. 24, 554–561 (2004).
Hekking, L. H. et al. Better preservation of peritoneal morphologic features and defense in rats after long-term exposure to a bicarbonate/lactate-buffered solution. J. Am. Soc. Nephrol. 12, 2775–2786 (2001).
Cooker, L. A. et al. Interleukin-6 levels decrease in effluent from patients dialyzed with bicarbonate/lactate-based peritoneal dialysis solutions. Perit. Dial. Int. 21 (Suppl. 3), S102–S107 (2001).
Witowski, J. et al. Peritoneal dialysis with solutions low in glucose degradation products is associated with improved biocompatibility profile towards peritoneal mesothelial cells. Nephrol. Dial. Transplant. 19, 917–924 (2004).
Zweers, M. M., de Waart, D. R., Smit, W., Struijk, D. G. & Krediet, R. T. Growth factors VEGF and TGF-β1 in peritoneal dialysis. J. Lab. Clin. Med. 134, 124–132 (1999).
Oh, K. H. et al. Intra-peritoneal interleukin-6 system is a potent determinant of the baseline peritoneal solute transport in incident peritoneal dialysis patients. Nephrol. Dial. Transplant. 25, 1639–1646 (2010).
Davies, S. J. et al. Longitudinal membrane function in functionally anuric patients treated with APD: data from EAPOS on the effects of glucose and icodextrin prescription. Kidney Int. 67, 1609–1615 (2005).
Martikainen, T. A., Teppo, A. M., Gronhagen-Riska, C. & Ekstrand, A. V. Glucose-free dialysis solutions: inductors of inflammation or preservers of peritoneal membrane? Perit. Dial. Int. 25, 453–460 (2005).
Moriishi, M., Kawanishi, H., Watanabe, H. & Tsuchiya, S. Effect of icodextrin-based peritoneal dialysis solution on peritoneal membrane. Adv. Perit. Dial. 21, 21–24 (2005).
Bajo, M. A. et al. Icodextrin effluent leads to a greater proliferation than glucose effluent of human mesothelial cells studied ex vivo. Perit. Dial. Int. 20, 742–747 (2000).
Zareie, M. et al. Better preservation of the peritoneum in rats exposed to amino acid-based peritoneal dialysis fluid. Perit. Dial. Int. 25, 58–67 (2005).
Garosi, G., Gaggiotti, E., Monaci, G., Brardi, S. & Di Paolo, N. Biocompatibility of a peritoneal dialysis solution with amino acids: histological evaluation in the rabbit. Perit. Dial. Int. 18, 610–619 (1998).
Ates¸, K. et al. Effect of fluid and sodium removal on mortality in peritoneal dialysis patients. Kidney Int. 60, 767–776 (2001).
Brown, E. A. et al. Survival of functionally anuric patients on automated peritoneal dialysis: the European APD Outcome Study. J. Am. Soc. Nephrol. 14, 2948–2957 (2003).
Davies, S. J. Longitudinal relationship between solute transport and ultrafiltration capacity in peritoneal dialysis patients. Kidney Int. 66, 2437–2445 (2004).
Smit, W. et al. Analysis of the prevalence and causes of ultrafiltration failure during long-term peritoneal dialysis: a cross-sectional study. Perit. Dial. Int. 24, 562–570 (2004).
Krediet, R. T. & Balafa, O. Cardiovascular risk in the peritoneal dialysis patient. Nat. Rev. Nephrol. 6, 451–460 (2010).
Krediet, R. T. Dry body weight: water and sodium removal targets in PD. Contrib. Nephrol. 150, 104–110 (2006).
Mistry, C. D., Gokal, R. & Peers, E. A randomized multicenter clinical trial comparing isosmolar icodextrin with hyperosmolar glucose solutions in CAPD. MIDAS Study Group. Multicenter Investigation of Icodextrin in Ambulatory Peritoneal Dialysis. Kidney Int. 46, 496–503 (1994).
Posthuma, N. et al. Assessment of the effectiveness, safety, and biocompatibility of icodextrin in automated peritoneal dialysis. The Dextrin in APD in Amsterdam (DIANA) Group. Perit. Dial. Int. 20 (Suppl. 2), S106–S113 (2000).
Woodrow, G. et al. Comparison of icodextrin and glucose solutions for the daytime dwell in automated peritoneal dialysis. Nephrol. Dial. Transplant. 14, 1530–1535 (1999).
Wolfson, M., Piraino, B., Hamburger, R. J. & Morton, A. R. A randomized controlled trial to evaluate the efficacy and safety of icodextrin in peritoneal dialysis. Am. J. Kidney Dis. 40, 1055–1065 (2002).
Finkelstein, F. et al. Superiority of icodextrin compared with 4.25% dextrose for peritoneal ultrafiltration. J. Am. Soc. Nephrol. 16, 546–554 (2005).
Lin, A. et al. Randomized controlled trial of icodextrin versus glucose containing peritoneal dialysis fluid. Clin. J. Am. Soc. Nephrol. 4, 1799–1804 (2009).
Davies, S. J. et al. Icodextrin improves the fluid status of peritoneal dialysis patients: results of a double-blind randomized controlled trial. J. Am. Soc. Nephrol. 14, 2338–2344 (2003).
Adachi, Y., Nakagawa, Y. & Nishio, A. Icodextrin preserves residual renal function in patients treated with automated peritoneal dialysis. Perit. Dial. Int. 26, 405–407 (2006).
Konings, C. J. et al. Effect of icodextrin on volume status, blood pressure and echocardiographic parameters: a randomized study. Kidney Int. 63, 1556–1563 (2003).
Asghar, R. B., Diskin, A. M., Spanel, P., Smith, D. & Davies, S. J. Influence of convection on the diffusive transport and sieving of water and small solutes across the peritoneal membrane. J. Am. Soc. Nephrol. 16, 437–443 (2005).
Justo, P., Sanz, A. B., Egido, J. & Ortiz, A. 3,4-Dideoxyglucosone-3-ene induces apoptosis in renal tubular epithelial cells. Diabetes 54, 2424–2429 (2005).
Forbes, J. M., Cooper, M. E., Oldfield, M. D. & Thomas, M. C. Role of advanced glycation end products in diabetic nephropathy. J. Am. Soc. Nephrol. 14, S254–S258 (2003).
Montenegro, J. et al. Long-term clinical experience with pure bicarbonate peritoneal dialysis solutions. Perit. Dial. Int. 26, 89–94 (2006).
Fan, S. L., Pile, T., Punzalan, S., Raftery, M. J. & Yaqoob, M. M. Randomized controlled study of biocompatible peritoneal dialysis solutions: effect on residual renal function. Kidney Int. 73, 200–206 (2008).
Delarue, J. et al. Glucose oxidation after a peritoneal and an oral glucose load in dialyzed patients. Kidney Int. 45, 1147–1152 (1994).
Prinsen, B. H. et al. A broad-based metabolic approach to study VLDL apoB100 metabolism in patients with ESRD and patients treated with peritoneal dialysis. Kidney Int. 65, 1064–1075 (2004).
Marshall, J., Jennings, P., Scott, A., Fluck, R. J. & McIntyre, C. W. Glycemic control in diabetic CAPD patients assessed by continuous glucose monitoring system (CGMS). Kidney Int. 64, 1480–1486 (2003).
Paniagua, R. et al. Icodextrin improves metabolic and fluid management in high and high-average transport diabetic patients. Perit. Dial. Int. 29, 422–432 (2009).
Babazono, T. et al. Effects of icodextrin on glycemic and lipid profiles in diabetic patients undergoing peritoneal dialysis. Am. J. Nephrol. 27, 409–415 (2007).
Floré, K. M. & Delanghe, J. R. Analytical interferences in point-of-care testing glucometers by icodextrin and its metabolites: an overview. Perit. Dial. Int. 29, 377–383 (2009).
McDonald, S. P., Collins, J. F. & Johnson, D. W. Obesity is associated with worse peritoneal dialysis outcomes in the Australia and New Zealand patient populations. J. Am. Soc. Nephrol. 14, 2894–2901 (2003).
Abbott, K. C. et al. Body mass index, dialysis modality, and survival: analysis of the United States Renal Data System Dialysis Morbidity and Mortality Wave II Study. Kidney Int. 65, 597–605 (2004).
Aslam, N., Bernardini, J., Fried, L. & Piraino, B. Large body mass index does not predict short-term survival in peritoneal dialysis patients. Perit. Dial. Int. 22, 191–196 (2002).
Lu, Q. et al. Visceral fat, arterial stiffness, and endothelial function in peritoneal dialysis patients. J. Ren. Nutr. 18, 495–502 (2008).
Holmes, C. J. Reducing cardiometabolic risk in peritoneal dialysis patients: role of the dialysis solution. J. Diabetes Sci. Technol. 3, 1472–1480 (2009).
Wang, X. et al. Changes in fat mass after initiation of maintenance dialysis is influenced by the uncoupling protein 2 exon 8 insertion/deletion polymorphism. Nephrol. Dial. Transplant. 22, 196–202 (2007).
Teta, D. et al. Glucose-containing peritoneal dialysis fluids regulate leptin secretion from 3T3-L1 adipocytes. Nephrol. Dial. Transplant. 20, 1329–1335 (2005).
Furuya, R., Odamaki, M., Kumagai, H. & Hishida, A. Beneficial effects of icodextrin on plasma level of adipocytokines in peritoneal dialysis patients. Nephrol. Dial. Transplant. 21, 494–498 (2006).
Takeguchi, F., Nakayama, M. & Nakao, T. Effects of icodextrin on insulin resistance and adipocytokine profiles in patients on peritoneal dialysis. Ther. Apher. Dial. 12, 243–249 (2008).
Ateshkadi, A., Johnson, C. A., Founds, H. W. & Zimmerman, S. W. Serum advanced glycosylation end-products in patients on hemodialysis and CAPD. Perit. Dial. Int. 15, 129–233 (1995).
Stenvinkel, P. et al. Strong association between malnutrition, inflammation, and atherosclerosis in chronic renal failure. Kidney Int. 55, 1899–1911 (1999).
Stenvinkel, P., Lindholm, B., Heimbürger, M. & Heimbürger, O. Elevated serum levels of soluble adhesion molecules predict death in pre-dialysis patients: association with malnutrition, inflammation, and cardiovascular disease. Nephrol. Dial. Transplant. 15, 1624–1630 (2000).
Park, S. H. et al. Effects of neutral pH and low-glucose degradation product-containing peritoneal dialysis fluid on systemic markers of inflammation and endothelial dysfunction: a randomized controlled 1-year follow-up study. Nephrol. Dial. Transplant. http://dx.doi.org/10.1093/ndt/gfr451.
Welten, A. G. et al. Single exposure of mesothelial cells to glucose degradation products (GDPs) yields early advanced glycation end-products (AGEs) and a proinflammatory response. Perit. Dial. Int. 23, 213–221 (2003).
Wang, A. Y. et al. N-terminal pro-brain natriuretic peptide: an independent risk predictor of cardiovascular congestion, mortality, and adverse cardiovascular outcomes in chronic peritoneal dialysis patients. J. Am. Soc. Nephrol. 18, 321–330 (2007).
Wang, A. Y. Vascular and other tissue calcification in peritoneal dialysis patients. Perit. Dial. Int. 29 (Suppl. 2), S9–S14 (2009).
Tjiong, H. L. et al. Dialysate as food: combined amino acid and glucose dialysate improves protein anabolism in renal failure patients on automated peritoneal dialysis. J. Am. Soc. Nephrol. 16, 1486–1493 (2005).
de Jager, D. J. et al. Cardiovascular and noncardiovascular mortality among patients starting dialysis. JAMA 302, 1782–1789 (2009).
Kato, S. et al. Endotoxin-induced chemokine expression in murine peritoneal mesothelial cells: the role of toll-like receptor 4. J. Am. Soc. Nephrol. 15, 1289–1299 (2004).
Catalan, M. P., Reyero, A., Egido, J. & Ortiz, A. Acceleration of neutrophil apoptosis by glucose-containing peritoneal dialysis solutions: role of caspases. J. Am. Soc. Nephrol. 12, 2442–2449 (2001).
Brulez, H. F., ter Wee, P. M., Snijders, S. V., Donker, A. J. & Verbrugh, H. A. Mononuclear leucocyte function tests in the assessment of the biocompatibility of peritoneal dialysis fluids. J. Clin. Pathol. 52, 901–909 (1999).
Ha, H. et al. Effects of conventional and new peritoneal dialysis solutions on human peritoneal mesothelial cell viability and proliferation. Perit. Dial. Int. 20 (Suppl. 5), S10–S8 (2000).
Plum, J., Schoenicke, G. & Grabensee, B. Osmotic agents and buffers in peritoneal dialysis solution: monocyte cytokine release and in vitro cytotoxicity. Am. J. Kidney Dis. 30, 413–422 (1997).
Pajek, J. et al. Short-term effects of a new bicarbonate/lactate-buffered and conventional peritoneal dialysis fluid on peritoneal and systemic inflammation in CAPD patients: a randomized controlled study. Perit. Dial. Int. 28, 44–52 (2008).
Posthuma, N. et al. Peritoneal defense using icodextrin or glucose for daytime dwell in CCPD patients. Perit. Dial. Int. 19, 334–342 (1999).
Gokal, R., Mistry, C. D. & Peers, E. M. Peritonitis occurrence in a multicenter study of icodextrin and glucose in CAPD. MIDAS Study Group. Multicenter Investigation of Icodextrin in Ambulatory Dialysis. Perit. Dial. Int. 15, 226–230 (1995).
Vychytil, A. et al. Icodextrin does not impact infectious and culture-negative peritonitis rates in peritoneal dialysis patients: a 2-year multicentre, comparative, prospective cohort study. Nephrol. Dial. Transplant. 23, 3711–3719 (2008).
Peers, E. & Gokal, R. Icodextrin provides long dwell peritoneal dialysis and maintenance of intraperitoneal volume. Artif. Organs 22, 8–12 (1998).
Libetta, C. et al. Effects of different peritoneal dialysis fluids on the TH1/TH2 balance. Eur. Cytokine Netw. 22, 24–31 (2011).
Lee, H. Y. et al. Superior patient survival for continuous ambulatory peritoneal dialysis patients treated with a peritoneal dialysis fluid with neutral pH and low glucose degradation product concentration (Balance). Perit. Dial. Int. 25, 248–255 (2005).
Lee, H. Y. et al. Changing prescribing practice in CAPD patients in Korea: increased utilization of low GDP solutions improves patient outcome. Nephrol. Dial. Transplant. 21, 2893–2899 (2006).
Montenegro, J. et al. Use of pure bicarbonate-buffered peritoneal dialysis fluid reduces the incidence of CAPD peritonitis. Nephrol. Dial. Transplant. 22, 1703–1708 (2007).
Ahmad, S. et al. Impact of new dialysis solutions on peritonitis rates. Kidney Int. Suppl. S63–S66 (2006).
Furkert, J., Zeier, M. & Schwenger, V. Effects of peritoneal dialysis solutions low in GDPs on peritonitis and exit-site infection rates. Perit. Dial. Int. 28, 637–640 (2008).
Srivastava, S., Hildebrand, S. & Fan, S. L. Long-term follow-up of patients randomized to biocompatible or conventional peritoneal dialysis solutions show no difference in peritonitis or technique survival. Kidney Int. 80, 986–991 (2011).
Aslam, N., Bernardini, J., Fried, L., Burr, R. & Piraino, B. Comparison of infectious complications between incident hemodialysis and peritoneal dialysis patients. Clin. J. Am. Soc. Nephrol. 1, 1226–1233 (2006).
Mehrotra, R., Chiu, Y. W., Kalantar-Zadeh, K., Bargman, J. & Vonesh, E. Similar outcomes with hemodialysis and peritoneal dialysis in patients with end-stage renal disease. Arch. Intern. Med. 171, 110–118 (2011).
Weinhandl, E. D. et al. Propensity-matched mortality comparison of incident hemodialysis and peritoneal dialysis patients. J. Am. Soc. Nephrol. 21, 499–506 (2010).
Stenvinkel, P. et al. Emerging biomarkers for evaluating cardiovascular risk in the chronic kidney disease patient: how do new pieces fit into the uremic puzzle? Clin. J. Am. Soc. Nephrol. 3, 505–521 (2008).
Chaudhary, K. & Khanna, R. Biocompatible peritoneal dialysis solutions: do we have one? Clin. J. Am. Soc. Nephrol. 5, 723–732 (2010).
Paniagua, R. et al. Echocardiographic, electrocardiographic and blood pressure changes induced by icodextrin solution in diabetic patients on peritoneal dialysis. Kidney Int. Suppl. S125–S130 (2008).
Davies, S. J. et al. Longitudinal relationships between fluid status, inflammation, urine volume and plasma metabolites of icodextrin in patients randomized to glucose or icodextrin for the long exchange. Nephrol. Dial. Transplant. 23, 2982–2988 (2008).
Rodriguez-Carmona, A., Fontan, M. P., Lopez, E. G., Falcon, T. G. & Cambre, H. D. Use of icodextrin during nocturnal automated peritoneal dialysis allows sustained ultrafiltration while reducing the peritoneal glucose load: a randomized crossover study. Perit. Dial. Int. 27, 260–266 (2007).
Wilkie, M. E., Plant, M. J., Edwards, L. & Brown, C. B. Icodextrin 7.5% dialysate solution (glucose polymer) in patients with ultrafiltration failure: extension of CAPD technique survival. Perit. Dial. Int. 17, 84–87 (1997).
Takatori, Y. et al. Icodextrin increases technique survival rate in peritoneal dialysis patients with diabetic nephropathy by improving body fluid management: a randomized controlled trial. Clin. J. Am. Soc. Nephrol. 6, 1337–1344 (2011).
Kuriyama, R., Tranaeus, A. & Ikegami, T. Icodextrin reduces mortality and the drop-out rate in Japanese peritoneal dialysis patients. Adv. Perit. Dial. 22, 108–110 (2006).
Han, S. H., Ahn, S. V., Yun, J. Y., Tranaeus, A. & Han, D. S. Effects of icodextrin on patient survival and technique success in patients undergoing peritoneal dialysis. Nephrol. Dial. Transplant. http://dx.doi.org/10.1093/ndt/gfr580.
Li, F. K. et al. A 3-year, prospective, randomized, controlled study on amino acid dialysate in patients on CAPD. Am. J. Kidney Dis. 42, 173–183 (2003).
Han, S. H., Ahn, S. V., Yun, J. Y., Tranaeus, A. & Han, D. S. Mortality and technique failure in peritoneal dialysis patients using advanced peritoneal dialysis solutions. Am. J. Kidney Dis. 54, 711–720 (2009).
Pajek, J. et al. Short-term effects of bicarbonate/lactate-buffered and conventional lactate-buffered dialysis solutions on peritoneal ultrafiltration: a comparative crossover study. Nephrol. Dial. Transplant. 24, 1617–1625 (2009).
US National Library of Medicine. ClinicalTrials.gov [online], (2011).
Johnson, D. W., Clarke, M., Wilson, V., Woods, F. & Brown, F. G. Rationale and design of the balANZ trial: a randomised controlled trial of low GDP, neutral pH versus standard peritoneal dialysis solution for the preservation of residual renal function. BMC Nephrol. 11, 25 (2010).
Johnson, D. W. Biocompatibility: Insights from the balANZ Study. Presented at the 10th European Peritoneal Dialysis meeting, Birmingham, UK, October 20–24, 2011.
Bonomini, M. et al. L-carnitine is an osmotic agent suitable for peritoneal dialysis. Kidney Int. 80, 645–654 (2011).
Davies, S. J. L-carnitine: more than just an alternative to glucose as an osmotic agent for peritoneal dialysis? Kidney Int. 80, 565–566 (2011).
Nakayama, M., Kasai, K., Imai, H. & TRM-280 Study Group. Novel low Na peritoneal dialysis solutions designed to optimize Na gap of effluent: kinetics of Na and water removal. Perit. Dial. Int. 29, 528–535 (2009).
Davies, S. et al. The effects of low-sodium peritoneal dialysis fluids on blood pressure, thirst and volume status. Nephrol. Dial. Transplant. 24, 1609–1617 (2009).
de Graaff, M. et al. The effects of a dialysis solution with a combination of glycerol/amino acids/dextrose on the peritoneal membrane in chronic renal failure. Perit. Dial. Int. 30, 192–200 (2010).
Riser, B. L. et al. Daily peritoneal administration of sodium pyrophosphate in a dialysis solution prevents the development of vascular calcification in a mouse model of uraemia. Nephrol. Dial. Transplant. 26, 3349–3357 (2011).
Author information
Authors and Affiliations
Contributions
The authors contributed equally to all aspects of this article.
Corresponding author
Ethics declarations
Competing interests
Bengt Lindholm is employed by Baxter Healthcare Corporation, owns stock options from Baxter Healthcare Corporation and receives research funding from Baxter Healthcare Corporation. Simon Davies declares an association with Baxter Healthcare Corporation (consultant, speaker's bureau, grant/research support) and is a consultant and has received honoraria for speaking from Gambro and Fresenius Medical Care. Elvia García-López declares no competing interests.
Rights and permissions
About this article
Cite this article
García-López, E., Lindholm, B. & Davies, S. An update on peritoneal dialysis solutions. Nat Rev Nephrol 8, 224–233 (2012). https://doi.org/10.1038/nrneph.2012.13
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrneph.2012.13