Abstract
Few elderly patients have been included in randomized trials assessing recombinant tissue plasminogen activator (rtPA) in stroke. In North America, intravenous thrombolysis is allowed in these patients; however, the European Medicines Agency does not recommend rtPA for the treatment of stroke in patients over 80 years of age. The influence of age on outcome following stroke-unit care and rehabilitation also remains controversial. In the absence of randomized trials, the efficacy of thrombolysis in elderly patients is difficult to measure. The majority of rtPA cohort studies demonstrate that patients over 80 years of age have lower rates of positive outcomes following treatment than younger patients. These studies are, however, reassuring with regard to the risk of symptomatic intracerebral hemorrhage and death, and suggest that rtPA can be safely administered to carefully selected elderly patients within 3 h of the onset of stroke. Further randomized studies will lead to more-accurate conclusions about the efficacy and safety of rtPA in the elderly subgroup. Admission to a stroke unit rather than to a general ward and early rehabilitation are justified in elderly patients. In this article, we review the literature regarding the effect of thrombolysis, stroke-unit care, and rehabilitation in patients over 80 years of age with stroke.
Key Points
-
Elderly patients constitute 30% of all patients with ischemic stroke; however, such individuals are at risk of receiving suboptimal care
-
Patients aged 80 years or over with stroke have a substantially higher mortality risk than younger patients and are less likely to make a favorable recovery
-
Intravenous thrombolysis, using recombinant tissue plasminogen activator, is safe and potentially effective in patients aged 80 years or over with stroke; however, data from randomized placebo-controlled studies are lacking in this subgroup
-
Admission to a stroke unit is beneficial across all age ranges, and is associated with reductions in the probabilities of death, disability, and institutionalization
-
Rehabilitation might be more challenging in elderly patients with stroke than in younger individuals, but no evidence exists to suggest that age alone should influence decisions on eligibility for rehabilitation
Similar content being viewed by others
Introduction
The efficacy of intravenous thrombolysis using recombinant tissue plasminogen activator (rtPA) in acute ischemic stroke is no longer in doubt, and increasing numbers of stroke centers are able to provide this treatment 24 h a day. This therapy is, however, barely used in Europe and the US. The underuse of rtPA is largely explained by the following factors: the therapeutic window, which is currently limited to 3 h; insufficient public knowledge of the warning signs of stroke; excessive admission delay; and a lack of stroke-center coverage.1,2 The exclusion of numerous patients because of the—sometimes excessive—fear of hemorrhagic complications is another reason why only a low percentage of patients receive rtPA treatment.
Contrary to the recommendations and conditions for use in the US, Canada and Switzerland, the European Medicines Agency (EMEA) does not advocate the use of rtPA in the treatment of ischemic stroke in patients over 80 years of age. One of the reasons for this contraindication is that very old patients were not included in the large-scale European randomized trials of thrombolysis for stroke.3,4 Given the aging nature of the population living in developed countries and the fact that the incidence of acute ischemic stroke (AIS) increases with age, the stance of the EMEA means that up to 30% of patients with AIS are excluded from receiving rtPA treatment.5,6,7
Excluding the subgroup of the population that has the highest risk of developing ischemic stroke from the only curative emergency treatment on the grounds of age alone seems somewhat paradoxical.8 Moreover, results indicate that elderly patients with stroke who are not given thrombolytic therapy have a poorer prognosis than younger patients in terms of mortality and long-term physical and cognitive disability.9,10,11,12 The peculiar severity of AIS in elderly patients might be explained by several factors, including the influence of associated pathologies (for example, atrial fibrillation), the presence of physical disabilities or cognitive disorders before the onset of stroke, the increase in frequency of complications during hospitalization, and the diminished access to healthcare.13,14,15 Indeed, prestroke institutionalization has been found to be a strong and independent determinant of 3-month disability in patients over 80 years of age or older who have experienced a stroke.14 Furthermore, elderly patients with stroke, even if they were previously independent in activities of daily living, are at risk of receiving suboptimal care, particularly in terms of investigation, admission to stroke units, and access to early rehabilitation.7,14 The issue of suboptimal care has long been recognized and remains particularly important in hospitals with a shortage of neurological beds.16
Safety and efficacy of thrombolysis
In coronary heart disease, the benefit of thrombolysis in elderly patients is well accepted, despite increases in the risk of intracerebral hemorrhage (ICH) and the rate of mortality with age.17 Data from the National Registry of Myocardial Infarction 2 revealed that the rate of ICH in this context is 0.4% in individuals under 65 years of age, 1.2% in 65–74-year-olds, and 2.1% in those aged over 75 years.18
In ischemic stroke, elderly patients have been either excluded from or underrepresented in the large-scale randomized controlled trials of thrombolysis. The conclusions that can be drawn from these trials regarding the safety and efficacy of thrombolytic therapy in the elderly remain very limited. Age was, however, associated with an increase in the risk of rtPA-related ICH in several studies.19,20,21,22,23 In the first European Cooperative Acute Stroke Study (ECASS), age was the only independent predictive factor of parenchymal hematoma, with an odds ratio (OR) of 1.3 for every 10 years of age.19 In ECASS II, approximately one in five patients over 70 years of age developed severe hemorrhage following administration of rtPA.21 A study investigating the in-hospital mortality of patients with stroke who were treated with rtPA also concluded that age had an effect on the risk of ICH—4.9% of patients under 55 years of age developed ICH, whereas 10.3% of patients 75 years of age or over developed the condition.24
The increase with age in the risk of developing rtPA-related ICH might be linked to the particularly high frequency of microangiopathic processes, such as leukoaraiosis and cerebral amyloid angiopathy (CAA), in elderly patients. A multicenter retrospective study using MRI revealed that leukoaraiosis was a risk factor for symptomatic ICH when thrombolysis was delivered within 6 h of the onset of stroke.25 In this study, patients who exhibited moderate or severe leukoaraiosis were older than patients who exhibited no leukoaraiosis, although age itself was not found to be an independent predictor of symptomatic ICH. Indeed, age might be merely a 'biological' marker of the various age-linked degenerative processes that are responsible for cerebral microangiopathy and, hence, the possible risk of hemorrhage. CAA itself leads to microvascular impairment, which increases the risk of rtPA-related parenchymal hematomas. Histopathological examinations revealed the presence of underlying CAA in three out of five patients who had died from ICH following thrombolysis with rtPA.26 Data concerning the safety and the efficacy of rtPA in elderly patients are summarized in Table 1.27,28,29,30,31,32,33,34,35,36,37,38,39,40
Randomized controlled rtPA trials in stroke have included very few elderly patients. In the NINDS tPA Stroke Trial, for example, which included 624 participants, only 42 patients were over 80 years of age (6.7%).19 In this pivotal study, the beneficial effect of rtPA was persistent across all age groups and the authors concluded that the subselection of patients for stroke thrombolysis on the basis of age was not supported by post hoc analysis.41
One of the first studies that specifically focused on thrombolysis in elderly patients with stroke was conducted by the tPA Stroke Survey Group and published in 2000.27 The results from the study showed that the risk of symptomatic or lethal ICH following rtPA was not increased in patients aged 80 years or over compared with patients under 80 years of age, although the older age group only comprised 30 individuals (189 patients in total were involved in the study). The study also reported that elderly patients were more frequently treated by stroke specialists than were younger patients (87% versus 60%; P = 0.005), and violations of protocol were less frequent in the older group (13% versus 33%; P = 0.03). Furthermore, institutionalization was more frequently necessary following hospitalization in elderly patients than in younger individuals (17% versus 5%; P = 0.003).
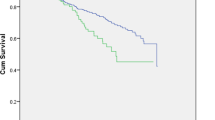
Results from the Canadian Alteplase for Stroke Effectiveness Study indicated that the risk–benefit ratio of intravenous rtPA might be favorable for some carefully selected elderly patients (80 years of age or over) treated within 3 hours of the onset of AIS.34 In the 270 elderly patients included in this study, the rate of symptomatic ICH was 4% in treated patients. Despite this low rate of severe hemorrhage, the rate of good clinical outcomes within 3 months (as denoted by a modified Rankin score ≤1) was only 26% in the elderly subgroup. A systematic review of cohort studies of intravenous thrombolysis for stroke in octogenarians has shown that patients over 80 years of age have a substantially higher mortality risk than younger patients, and are less likely to recover favorably. The risk of symptomatic ICH was similar in both age groups.42 Overall, the analysis of the current data show that the incidence of symptomatic ICH following rtPA treatment is not markedly increased in stroke patients over 80 years of age compared with younger patients. The incidence of unfavorable outcomes, however, was greater in the older subgroup.38 Nevertheless, 25–37% of patients over 80 years of age recovered completely or to a reasonable level of independence after thrombolysis with intravenous rtPA.
The use of pretherapeutic MRI to select octogenarians for stroke thrombolysis might further improve safety. A monocentric study, in which patients with acute stroke were treated with rtPA on the basis of results from MRI, reported a 7% rate of symptomatic ICH in patients 80 years of age or older versus 5% in patients under 80 years of age.36 Potential MRI predictors of rtPA-related ICH are presented in Table 2.22,25,43,44,45,46,47,48,49 Some studies have suggested that diffusion-weighted imaging (DWI) sequences could help in identifying stroke patients who are at risk of ICH after thrombolysis.22,44,45,46,47,48 Apparent diffusion coefficient values might also influence the risk of rtPA-related ICH.22,44,45,46 Results from a prospective, multicenter study showed that patients with large baseline DWI lesion volumes who achieved reperfusion after treatment with intravenous rtPA seemed to be at the greatest risk of rtPA-related symptomatic ICH.48 Early blood–brain barrier disruption, an independent predictor of hemorrhagic transformation, might also be assayed by an urgent MRI scan.49 The rate of symptomatic ICH after stroke thrombolysis is markedly higher in patients with moderate to severe leukoaraiosis of the deep white matter (as captured by MRI) than in patients without leukoaraiosis.25 To summarize, results suggest that MRI parameters might help to predict rtPA-related ICH in elderly patients with stroke, although further large studies are needed to confirm the usefulness of this imaging technique.50
Limited data are available concerning intra-arterial thrombolysis in elderly patients with stroke. A retrospective analysis of 33 patients did not reveal any substantial difference in the recanalization rate between patients over 80 years of age and younger patients (79% versus 68%, respectively).51 Similarly, the rates of symptomatic ICH (7% versus 8%) and total ICH (39% versus 37%) were not appreciably different between the two groups. Nevertheless, marked differences between the elderly cohort and the younger subgroup were reported in the rate of excellent clinical outcome (modified Rankin score <2; 26% versus 40%) and the survival rate (57% versus 80%).
In conclusion, observational studies suggest that rtPA given within 3 h of stroke onset is safe and potentially effective in patients over 80 years of age, although the use of rtPA in this age group falls outside the current European labeling.52 Randomized, placebo-controlled clinical trials that include stroke patients aged over 80 years are necessary before definite recommendations on the use of rtPA in elderly patients can be given.40,42
Stroke-unit admission
Admission to a stroke unit, which has been shown to provide higher standards of care than a conventional ward, can clearly improve the outcomes of patients with acute stroke.53 Several randomized trials and meta-analyses have shown that stroke-unit care decreases mortality, physical and cognitive disability, and the need for institutionalization.16,54,55 Furthermore, the beneficial effects from stroke-unit care are not dependent on age, sex, or stroke severity.16,54,55 Indeed, the European Stroke Organisation (ESO) recommends that all patients with stroke, irrespective of age, should be treated in a stroke unit (class I, level A evidence).52
An observational follow-up study was conducted for 11,572 acute stroke patients—identified retrospectively from the discharge records of 260 Italian hospitals—who were hospitalized within 48 h of the onset of symptoms and placed into either a stroke unit (4,936 patients) or a conventional ward (6,636 patients).56 The primary outcome of the study was mortality or disability (Rankin score >2), which was assessed prospectively by independent, blinded assessors 2 years after admission of the patient. Compared with care on a conventional ward, stroke-unit care was associated with a reduced probability of death or being disabled at the end of the follow-up period (OR 0.81, 95% CI 0.72–0.91; P = 0.0001). The potential benefit of stroke-unit care was apparent across all age ranges and clinical characteristics (for example, sex, time of admission, or presence of ICH). The results from the study support the view that no firm evidence exists for restricting access to stroke units on the basis of age. Another study has shown that well-organized management of elderly patients with stroke is associated with improvements in both clinical outcome and economical use of resources.16
Despite the evidence that all patients tend to do better in stroke units than general wards, the National Sentinel Audit of stroke performed in 2004 revealed clear evidence of an age effect on the delivery of stroke care in the UK. Data from the audit showed that older patients (85 years of age or older) were less likely to be treated in a stroke unit than younger patients (65 years of age or under; risk ratio 0.82, 95% CI 0.75–0.90).53 Older patients were also less likely than younger patients to receive a brain scan within 24 h of stroke onset, secondary prevention, and some aspects of rehabilitation (especially relating to areas of higher-level functioning, such as leisure pursuits, driving, and returning to work).53 Multiple reasons exist for this apparent ageism. The often frail nature of elderly patients leads some physicians to the belief that older patients should be admitted to a geriatric ward rather than a stroke unit. Moreover, health professionals seem to view a year of life in old age as being of less value than a year of life in younger individuals. Indeed, younger patients are often given priority treatment over older individuals when medical resources are limited.53
Early rehabilitation
Several studies have clearly demonstrated that the benefits of intensive stroke rehabilitation programs with regard to maximizing functional recovery extend to patients of every age. In addition, these studies show that benefits can be achieved without increases in therapy resources.57,58 The ESO recommends that physiotherapy and occupational therapy are included in rehabilatory programs (class I, level A). Moreover, the organization recommends that stroke rehabilitation should be considered for all patients irrespective of age (class II, level B).52
A prospective study showed that age alone accounted for only 3% of the variation in functional outcome after stroke rehabilitation.59 This finding suggests that denying patients access to intensive rehabilitation solely on the basis of advanced age is not justifiable. Most of the apparent relationship between age and functional outcome seems to be attributable to the functional status of the patient before admission to a stroke rehabilitation program.59 Results from a prospective cohort study of 303 stroke survivors, however, showed that advanced age alone (over 80 years of age) was associated with increased physical and cognitive disability at 12 months compared with patients 80 years of age or younger.60 Post-stroke depression can greatly influence stroke outcome in elderly patients. Indeed, depression is strongly associated with post-stroke disability at 12 months.60 Specific rehabilitation interventions (such as exercise and activity groups in collaboration with family caregivers) for this high-risk group of older patients with smaller social networks should be implemented to prevent disability levels from increasing.
Rehabilitation might be more challenging in elderly patients with stroke than in younger patients because of associated cognitive, cardiac and orthopedic pathologies. Despite such challenges, individual rehabilitation plans for all patients, regardless of age, should be recommended and implemented. Cohort studies have demonstrated that good functional outcomes can be achieved in elderly patients with stroke following inpatient rehabilitation.61,62 In a consecutive case series of 59 elderly patients with stroke (mean age 80.4 ± 3.2 years) who were admitted to a rehabilitation facility, substantial improvements in functional status, motor power, continence, and dysphagia were noted after rehabilitation. Indeed, 53 of the patients followed (89.8% of the total patient number) were successfully discharged home.61 In another case series, which examined the effects of rehabilitation on patients with a first-time stroke, most individuals 80 years of age or over (72.7% of the total number) were eventually able to return home, although the rate in the comparator group (under 80 years of age) was 90.5%.62 The predictive value of age on the success of stroke rehabilitation has been assessed in a retrospective study of 878 patients with stroke. In the study, patients were enrolled into an inpatient multidisciplinary rehabilitation program in a neurorehabilitation ward (mean length of stay 30.7 ± 0.8 days).63 Results from the study indicated that advanced age was not an independent predictor of a poor outcome. A good functional status on admission to the neurorehabilitation ward, employment, or living at home before the stroke (but not younger age per se) were predictors of a good outcome following stroke rehabilitation.
Given that elderly patients show marked improvements during stroke rehabilitation, intensive rehabilitation should not be withheld on the basis of age. Nevertheless, clear evidence exists that only a low proportion of elderly European patients with stroke have access to rehabilitation, despite their high disability rates.64 Moreover, old patients are more likely to be institutionalized than younger patients.64,65 The resources necessary to ensure that functional gains are maintained in elderly patients after rehabilitation should be determined, as physical and cognitive disability has been reported to increase 12 months after stroke in patients aged over 80 years.61
Stroke patients with cognitive impairment (especially those with attention and memory deficits) are less likely to do well after rehabilitation than stroke patients who are not cognitively impaired, as rehabilitation is an active process that requires the ability to follow, learn and remember specific instructions.61 These reasons also probably explain why patients with cognitive impairments require notably longer periods of rehabilitation than patients with intact cognition. A retrospective analysis suggests, however, that patients with stroke and cognitive impairment can benefit from admission to an acute rehabilitation unit and that many such patients can be discharged home.66 At present, no evidence exists for the efficacy of specific memory rehabilitation or cognitive training for attention deficit in stroke rehabilitation programs.52
Conclusions
Results from open studies demonstrate that the risk of ICH in patients who have received rtPA is largely unaffected by age. Moreover, data from such studies indicate that elderly patients with stroke show marked improvements following rtPA treatment, although such therapy might be less effective in older patient subgroups than in younger individuals. Data from randomized thrombolytic studies in elderly patients with stroke are not yet available, however, and the results from open studies might be distorted by selection biases (for example, by the selection of elderly patients affected by less severe strokes).67 Nevertheless, evidence from cohort studies suggests that rtPA treatment does not increase the mortality rate in elderly patients with stroke. Estimating the benefits of thrombolysis from case series has been difficult, although the use of predictive models in such studies might facilitate such assessments.68 To formulate more-objective conclusions relating to the use of rtPA in elderly patients, randomized, controlled clinical trials that include individuals over 80 years of age are required. Indeed, one such trial—the Third International Stroke Trial Study—is underway and is aiming to recruit 6,000 patients, including elderly individuals. Further studies on the integration of urgent MRI into the therapeutic decision-making process in elderly stroke patients are also needed.
In addition to an increase in the availability of rtPA therapy, elderly patients should be given wider access to acute stroke units. Data indicate that stroke-unit care can facilitate the recovery of patients from every age group following a stroke, in terms of reductions in mortality, disability and institutionalization. Similarly, no firm evidence exists for restricting access to intensive rehabilitation after stroke on the basis of a patient's age. Strategies need to be implemented to ensure that elderly patients receive optimal stroke care at all stages of their illness. The limited intervention currently received by elderly patients with stroke might contribute to their poor prognosis.
Review criteria
Relevant studies were identified by a search of the published literature in EMBASE and MEDLINE, using the Ovid and PubMed search engines, respectively. Search terms included “stroke”, “cerebrovascular accident”, “thrombolytic therapy”, “tissue plasminogen activator”, “elderly”, “aged 80 and over”, “stroke unit”, and “rehabilitation”. The search was limited to studies published in the English language before 1 June 2009. Abstracts of the retrieved citations were reviewed and prioritized by relevance. Full articles were obtained and references checked for additional material where appropriate. The classes of evidence and levels of recommendations were defined according to the criteria of the European Federation of Neurological Societies.
References
Qureshi, A. I. et al. Thrombolysis for ischemic stroke in the United States: data from national hospital discharge survey 1999–2001. Neurosurgery 57, 647–654 (2005).
Ringelstein, E. B. et al. European stroke facilities survey: the German and Austrian perspective. Cerebrovasc. Dis. 27, 138–145 (2009).
Hacke, W. et al. Randomised double-blind placebo-controlled trial of thrombolytic therapy with intravenous alteplase in acute ischaemic stroke (ECASS II). Second European–Australasian Acute Stroke Study Investigators. Lancet 352, 1245–1251 (1998).
Hacke, W. et al. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N. Engl. J. Med. 359, 1317–1329 (2008).
Bonita, R., Solomon, N. & Broad, J. B. Prevalence of stroke and stroke-related disability: estimates from the Auckland stroke studies. Stroke 28, 1898–1902 (1997).
Di Carlo, A. et al. Sex differences in the clinical presentation, resource use, and 3-month outcome of acute stroke in Europe: data from a multicenter multinational hospital-based registry. Stroke 34, 1114–1119 (2003).
Marini, C. et al. Burden of first-ever ischemic stroke in the oldest old: evidence from a population-based study. Neurology 62, 77–81 (2004).
Hemphill, J. C. Jr & Lyden, P. Stroke thrombolysis in the elderly: risk or benefit? Neurology 65, 1690–1691 (2005).
Dennis, M. S. et al. Long-term survival after first-ever stroke: the Oxfordshire Community Stroke Project. Stroke 24, 796–800 (1993).
Nakayama, H., Jorgensen, H. S., Raaschou, H. O. & Olsen, T. S. The influence of age on stroke outcome. The Copenhagen Stroke Study. Stroke 25, 808–813 (1994).
Lai, S. M., Alter, M., Friday, G. & Sobel, E. Prognosis for survival after an initial stroke. Stroke 26, 2011–2015 (1995).
Kammersgaard, L. P. et al. Short- and long-term prognosis for very old stroke patients. The Copenhagen Stroke Study. Age Ageing 33, 149–154 (2004).
Sharma, J. C., Fletcher, S. & Vassallo, M. Stroke in the elderly: higher acute and 3-month mortality-an explanation. Cerebrovasc. Dis. 9, 2–9 (1999).
Di Carlo, A. et al. Stroke in the very old: clinical presentation and determinants of 3-month functional outcome. A European perspective. European BIOMED Study of Stroke Care Group. Stroke 30, 2313–2319 (1999).
Olindo, S. et al. Acute stroke in the very elderly: epidemiological features, stroke subtypes, management, and outcome in Martinique, French West Indies. Stroke 34, 1593–1597 (2003).
Kaste, M., Palomäki, H. & Sarna, S. Where and how should elderly stroke patients be treated? A randomized trial. Stroke 26, 249–253 (1995).
Ridker, P. M. & Hennekens, C. H. Age and thrombolytic therapy. Circulation 94, 1807–1808 (1996).
Gurwitz, J. H. et al. Risk for intracranial hemorrhage after tissue plasminogen activator treatment for acute myocardial infarction. Ann. Intern. Med. 129, 597–604 (1998).
The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. Intracerebral hemorrhage after intravenous t-PA therapy for ischemic stroke. Stroke 28, 2109–2118 (1997).
Larrue, V., von Kummer, R., del Zoppo, G. & Bluhmki, E. Hemorrhagic transformation in acute ischemic stroke. Potential contributing factors in the European Cooperative Acute Stroke Study. Stroke 28, 957–960 (1997).
Larrue, V., von Kummer, R., Müller, A. & Bluhmki, E. Risk factors for severe hemorrhagic transformation in ischemic stroke patients treated with recombinant tissue plasminogen activator. A secondary analysis of the European–Australasian Acute Stroke Study (ECASS II). Stroke 32, 438–441 (2001).
Derex, L. et al. Clinical and imaging predictors of intracerebral haemorrhage in stroke patients treated with intravenous tissue plasminogen activator. J. Neurol. Neurosurg. Psychiatry 76, 70–75 (2005).
Tanne, D. et al. Markers of increased risk of intracerebral hemorrhage after intravenous recombinant tissue plasminogen activator therapy for acute ischemic stroke in clinical practice: the Multicenter rt-PA Stroke Survey. Circulation 105, 1679–1685 (2002).
Heuschmann, P. U. et al. Predictors of in-hospital mortality in patients with acute ischemic stroke treated with thrombolytic therapy. JAMA 292, 1831–1838 (2004).
Neumann-Haefelin, T. et al. Leukoaraiosis is a risk factor for symptomatic intracerebral hemorrhage after thrombolysis for acute stroke. Stroke 37, 2463–2466 (2006).
Sloan, M. A. et al. Clinical features and pathogenesis of intracerebral hemorrhage after rt-PA and heparin therapy for acute myocardial infarction: the Thrombolysis in Myocardial Infarction (TIMI) II pilot and randomised clinical trial combined experience. Neurology 45, 649–658 (1995).
Tanne, D. et al. Intravenous tissue plasminogen activator for acute ischemic stroke in patients aged 80 years and older: the tPA Stroke Survey experience. Stroke 31, 370–375 (2000).
Simon, J. E, Sandler, D. L., Pexman, J. H., Hill, M. D. & Buchan, A. M., for the Calgary Stroke Programme. Is intravenous recombinant tissue plasminogen activator (rt-PA) safe for use in patients over 80 years old with acute ischaemic stroke? The Calgary experience. Age Ageing 33, 143–149 (2004).
Berrouschot, J. et al. Outcome and severe hemorrhagic complications of intravenous thrombolysis with tissue plasminogen activator in very old (≥80 years) stroke patients. Stroke 36, 2421–2425 (2005).
Engelter, S. T. et al. Thrombolysis in stroke patients aged 80 years and older. Swiss survey of IV thrombolysis. Neurology 65, 1795–1798 (2005).
Mouradian, M. S. et al. Intravenous rt-PA for acute stroke: comparing its effectiveness in younger and older patients. J. Neurol. Neurosurg. Psychiatry 76, 1234–1237 (2005).
Chen, C. I. et al. Intravenous tPA for very old stroke patients. Eur. Neurol. 54, 140–144 (2005).
Van Oostenbrugge, R. J., Hupperts, R. M. & Lodder J. Thrombolysis for acute stroke with special emphasis on the very old: experience from a single Dutch centre. J. Neurol. Neurosurg. Psychiatry 77, 375–377 (2006).
Sylaja, P. N., Cote, R., Buchan, A. M. & Hill, M. D. Thrombolysis in patients older than 80 years with acute ischaemic stroke: Canadian Alteplase for Stroke Effectiveness Study. J Neurol. Neurosurg. Psychiatry. 77, 826–829 (2006).
Jauss, M., Allendörfer, J., Stolz, E., Schütz, H. J. & Misselwitz, B. Treatment results of stroke patients aged >80 years receiving intravenous rt-PA. Cerebrovasc. Dis. 24, 305–306 (2007).
Ringleb, P. A. et al. Thrombolytic therapy for acute ischaemic stroke in octogenarians: selection by magnetic resonance imaging improves safety but does not improve outcome. J. Neurol. Neurosurg. Psychiatry 78, 690–693 (2007).
Uyttenboogaart, M., Schrijvers, E. M., Vroomen, P. C., De Keyser, J. & Luijckx, G. J. Routine thrombolysis with intravenous tissue plasminogen activator in acute ischaemic stroke patients aged 80 years or older: a single centre experience. Age Ageing 36, 577–579 (2007).
Meseguer, E. et al. Determinants of outcome and safety of intravenous rt-PA therapy in the very old: a clinical registry study and systematic review. Age Ageing 37, 107–111 (2008).
Gómez-Choco, M. et al. The response to IV rt-PA in very old stroke patients. Eur. J. Neurol. 15, 253–256 (2008).
Toni, D. et al. Intravenous thrombolysis with rt-PA in acute ischemic stroke patients aged older than 80 years in Italy. Cerebrovasc. Dis. 25, 129–135 (2008).
The NINDS t-PA Stroke Study Group. Generalized efficacy of t-PA for acute stroke. Subgroup analysis of the NINDS t-PA Stroke Trial. Stroke 28, 2119–2125 (1997).
Engelter, S. T., Bonati, L. H. & Lyrer, P. A. Intravenous thrombolysis in stroke patients of ≥80 versus <80 years of age—a systematic review across cohort studies. Age Ageing 35, 572–580 (2006).
Derex, L. & Nighoghossian, N. Intracerebral haemorrhage after thrombolysis for acute ischaemic stroke: an update. J. Neurol. Neurosurg. Psychiatry 79, 1093–1099 (2008).
Tong, D. C., Adami, A., Moseley, M. E. & Marks, M. P. Relationship between apparent diffusion coefficient and subsequent hemorrhagic transformation following acute ischemic stroke. Stroke 31, 2378–2384 (2000).
Tong, D. C., Adami, A., Moseley, M. E. & Marks, M. P. Prediction of hemorrhagic transformation following acute stroke: role of diffusion- and perfusion-weighted magnetic resonance imaging. Arch. Neurol. 58, 587–593 (2001).
Selim, M. et al. Predictors of hemorrhagic transformation after intravenous recombinant tissue plasminogen activator: prognostic value of the initial apparent diffusion coefficient and diffusion-weighted lesion volume. Stroke 33, 2047–2052 (2002).
Albers, G. W. et al. Magnetic resonance imaging profiles predict clinical response to early reperfusion: the diffusion and perfusion imaging evaluation for understanding stroke evolution (DEFUSE) study. Ann. Neurol. 60, 508–517 (2006).
Lansberg, M. G. et al. Risk factors of symptomatic intracerebral hemorrhage after tPA therapy for acute stroke. Stroke 38, 2275–2278 (2007).
Latour, L. L., Kang, D. W., Ezzedine, M. A., Chalela, J. A. & Warach, S. Early blood–brain barrier disruption in human focal brain ischemia. Ann. Neurol. 56, 468–477 (2004).
Thomalla, G. et al. Outcome and symptomatic bleeding complications of intravenous thrombolysis within 6 hours in MRI-selected stroke patients: comparison of a German multicenter study with the pooled data of ATLANTIS, ECASS, and NINDS tPA trials. Stroke 37, 852–858 (2006).
Kim, D. et al. Intra-arterial thrombolysis for acute stroke in patients 80 and older. A comparison of results in patients younger than 80 years. AJNR Am. J. Neuroradiol. 28, 159–163 (2007).
European Stroke Organisation (ESO) Executive Committee; ESO Writing Committee. Guidelines for management of ischaemic stroke and transient ischaemic attack 2008. Cerebrovasc. Dis. 25, 457–507 (2008).
Rudd, A. G., Hoffman, A., Down, C., Pearson, M. & Lowe, D. Access to stroke care in England, Wales and Northern Ireland: the effect of age, gender and weekend admission. Age Ageing 36, 247–255 (2007).
Langhorne, P., Williams, B. O., Gilchrist, W. & Howie, K: Do stroke units save lives? Lancet 342, 395–398 (1993).
Stroke Unit Trialists' Collaboration. Organised inpatient (stroke unit) care for stroke. Cochrane Database of Systematic Reviews, Issue 4. Art. No.:CD000197.doi:10.1002/14651858.CD000197.pub2 (2007).
Candelise, L. et al. Stroke-unit care for acute stroke patients: an observational follow-up study. Lancet 369, 299–305 (2007).
Garraway, W. M., Whisnant, J. P. & Drury, I. The changing pattern of survival following stroke. Stroke 14, 699–703 (1983).
Kalra, L. Does age affect benefits of stroke unit rehabilitation? Stroke 25, 346–351 (1994).
Bagg, S., Pombo, A. P. & Hopman, W. M. Effect of age on functional outcomes after stroke rehabilitation. Stroke 33, 179–185 (2002).
Lo, R. S. et al. Handicap and its determinants of change in stroke survivors. One-year follow-up study. Stroke 39, 148–153 (2008).
Kong, K. H., Chua, K. S. & Tow, A. P. Clinical characteristics and functional outcome of stroke patients 75 years old and older. Arch. Phys. Med. Rehabil. 79, 1535–1539 (1998).
Ergeletzis, D., Kevorkian, C. G. & Rintala, D. Rehabilitation of the older stroke patient: functional outcome and comparison with younger patients. Am. J. Phys. Med. Rehabil. 81, 881–889 (2002).
Luk, J. K., Cheung, R. T., Ho, S. L. & Li, L. Does age predict outcome in stroke rehabilitation? A study of 878 Chinese subjects. Cerebrovasc. Dis. 21, 229–234 (2006).
Bhalla, A., Grieve, R., Tilling, K., Rudd, A. G. & Wolfe, C. D. Older stroke patients in Europe: stroke care and determinants of outcome. Age Ageing 33, 618–624 (2004).
Saposnik, G. et al. Stroke outcome in those over 80: a multicenter cohort study across Canada. Stroke 39, 2310–2317 (2008).
Rabadi, M. H., Rabadi, F. M., Edelstein, L. & Peterson, M. Cognitively impaired stroke patients do benefit from admission to an acute rehabilitation unit. Arch. Phys. Med. Rehabil. 89, 441–448 (2008).
Vatankhah, B. et al. Thrombolysis for stroke in the elderly. J. Thromb. Thrombolysis 20, 5–10 (2005).
Ford, G. A. Thrombolysis for stroke in the over 80s. Age Ageing 33, 95–97 (2004).
Acknowledgements
The authors would like to thank Miss Frédérique Groga-Bada for her help in the preparation of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Derex, L., Nighoghossian, N. Thrombolysis, stroke-unit admission and early rehabilitation in elderly patients. Nat Rev Neurol 5, 506–511 (2009). https://doi.org/10.1038/nrneurol.2009.127
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrneurol.2009.127
This article is cited by
-
Acute stroke treatment and outcome in the oldest old (90 years and older) at a tertiary care medical centre in Germany-a retrospective study showing safety and efficacy in this particular patient population
BMC Geriatrics (2021)
-
Impact of leukoaraiosis on parenchymal hemorrhage in elderly patients treated with thrombolysis
Neuroradiology (2016)
-
Quality of Life After Off-Label Thrombolysis for Ischemic Stroke in Elderly Patients
Drugs & Aging (2015)
-
Safety and Efficacy of Thrombolysis with Intravenous Alteplase in Older Stroke Patients
Drugs & Aging (2013)
-
Ergebnisse und Prädiktoren der geriatrischen Frührehabilitation im Akutkrankenhaus
Zeitschrift für Gerontologie und Geriatrie (2012)