Key Points
-
Clinical assessment of testicular masses must involve evaluation of the risk factors for testicular cancer, namely undescended testes, familial testis cancer, and previous contralateral tumour
-
Grey-scale ultrasonography with high frequency probes (≥10 MHz or more) is the recommended first-line imaging modality for exploration of the scrotum
-
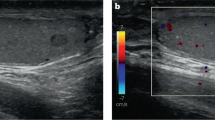
Colour Doppler ultrasonography is a valuable adjunct to grey-scale ultrasonography for the evaluation of testicular mass vascularization
-
Contrast-enhanced ultrasonography and real-time elastography are emerging techniques that can be used to characterize small intratesticular tumours <1 cm in diameter
-
Scrotal MRI is a powerful second-line imaging modality
-
Frozen section examination can be used during testicular surgery to identify suitable candidates for testis-sparing procedures
Abstract
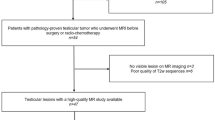
Diagnostic work-up of testicular masses should begin with a complete patient history and palpation of the testes with both hands. First-line imaging of the scrotum should be performed using multiparametric ultrasonography, that is the sequential use of grey-scale ultrasonography, colour Doppler ultrasonography (CDUS), and, if available, contrast-enhanced ultrasonography (CEUS) and real-time elastography (RTE). Increased vascularization—a characteristic of malignancy and inflammation—is visualized on CDUS and CEUS. RTE provides additional information for distinguishing between benign and malignant tissue by measuring tissue elasticity of lesions. MRI is another powerful modality, typically used for second-line imaging of intrascrotal disorders. MRI can provide images with a broad field of view of the scrotal contents. Cancerous lesions are identified on MRI by their signal enhancement after injection of contrast agent. Testicular germ cell tumours require treatment by inguinal orchiectomy. Testis-sparing surgery is advocated for benign tumours and in solitary testicles provided the tumour is <3 cm and the preoperative serum testosterone level is normal. For intraoperative decision-making with regard to testis-sparing surgery, frozen section histological examination can be used, which has a false-negative rate of <10%.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout








Similar content being viewed by others
References
Donohue, J. P. Editorial comment. J. Urol. 123, 130 (1980).
Altaffer, L. F. & Steele, S. M. Scrotal explorations negative for malignancy. J. Urol. 124, 617–619 (1980).
Banks, K. et al. Cryptorchidism and testicular germ cell tumors: comprehensive meta-analysis reveals that association between these conditions diminished over time and is modified by clinical characteristics. Front. Endocrinol. (Lausanne) 3, 182 (2012).
Dieckmann, K. P. & Pichlmeier, U. Clinical epidemiology of testicular germ cell tumors. World J. Urol. 22, 2–14 (2004).
McGlynn, K. A. & Trabert, B. Adolescent and adult risk factors for testicular cancer. Nat. Rev. Urol. 9, 339–349 (2012).
Moul, J. W. Timely diagnosis of testicular cancer. Urol. Clin. North Am. 34, 109–117 (2007).
Dieckmann, K. P., Becker, T. & Bauer, H. W. Testicular tumors: presentation and role of diagnostic delay. Urol. Int. 42, 241–247 (1987).
Hassan, H. C., Cullen, I. M., Casey, R. G. & Rogers, E. Gynaecomastia: an endocrine manifestation of testicular cancer. Andrologia 40, 152–157 (2008).
Trombetta, C. et al. in Scrotal Pathology (eds Bertolotto, M. & Trombetta, C.) 35–40 (Springer Verlag, 2012).
Field, T. E. Common errors occurring in the diagnosis of testicular neoplasms and the effect of these errors on prognosis. J. R. Army Med. Corps 110, 152–155 (1964).
Chapple, A., Ziebland, S. & McPherson, A. Qualitative study of men's perceptions of why treatment delays occur in the UK for those with testicular cancer. Br. J. Gen. Pract. 54, 25–32 (2004).
Connolly, S. S. et al. Terminology and details of the diagnostic process for testis cancer. J. Urol. 185, 876–880 (2011).
Ehrlich, Y., Beck, S. D., Foster, R. S., Bihrle, R. & Einhorn, L. H. Serum tumor markers in testicular cancer. Urol. Oncol. 31, 17–23 (2013).
Barlow, L. J., Badalato, G. M. & McKiernan, J. M. Serum tumor markers in the evaluation of male germ cell tumors. Nat. Rev. Urol. 7, 610–617 (2010).
Gilligan, T. D. et al. American Society of Clinical Oncology Clinical Practice Guideline on uses of serum tumor markers in adult males with germ cell tumors. J. Clin. Oncol. 28, 3388–3404 (2010).
Meistrich, M. L. Effects of chemotherapy and radiotherapy on spermatogenesis. Eur. Urol. 23, 136–142 (1993).
Kratochwil, A., Gasser, G. & Mayr, H. G. Ultrasound diagnosis in urology [German]. Wien. Klin. Wochenschr. 82, 795–800 (1970).
Staehler, G., Gebauer, A. & Mellin, H. E. Sonographic examination in diseases of the scrotal area (author's transl.) [German]. Urologe A 17, 247–250 (1978).
Miskin, M., Buckspan, M. & Bain, J. Ultrasonographic examination of scrotal masses. J. Urol. 117, 185–188 (1977).
McDonald, M. W., Reed, A. B., Tran, P. T. & Evans, L. A. Testicular tumor ultrasound characteristics and association with histopathology. Urol. Int. 89, 196–202 (2012).
De Zordo, T. et al. Multiparametric ultrasonography of the testicles. Nat. Rev. Urol. 10, 135–148 (2013).
Dogra, V. S., Gottlieb, R. H., Oka, M. & Rubens, D. J. Sonography of the scrotum. Radiology 227, 18–36 (2003).
Carkaci, S., Ozkan, E., Lane, D. & Yang, W. T. Scrotal sonography revisited. J. Clin. Ultrasound 38, 21–37 (2010).
Mirochnik, B., Bhargava, P., Dighe, M. K. & Kanth, N. Ultrasound evaluation of scrotal pathology. Radiol. Clin. North Am. 50, 317–332 (2012).
Albers, P. et al. Diagnosis, staging, and risk factors: SIU/ICUD Consensus Meeting on Germ Cell Tumors (GCT), Shanghai 2009. Urology 78, S427–S434 (2011).
Howard, G. C. & Nairn, M. Management of adult testicular germ cell tumours: summary of updated SIGN guideline. BMJ 342, d2005 (2011).
Motzer, R. J. et al. Testicular cancer. J. Natl Compr. Canc. Netw. 10, 502–535 (2012).
Horstman, W. G., Middleton, W. D., Melson, G. L. & Siegel, B. A. Color Doppler US of the scrotum. Radiographics 11, 941–957 (1991).
Hamm, B. Differential diagnosis of scrotal masses by ultrasound. Eur. Radiol. 7, 668–679 (1997).
Stengel, J. W. & Remer, E. M. Sonography of the scrotum: case-based review. AJR Am. J. Roentgenol. 190, S35–S41 (2008).
Horstman, W. G., Melson, G. L., Middleton, A. W. & Andriole, G. L. Testicular tumors: findings with color Doppler US. Radiology 185, 733–737 (1992).
Eifler, J. B. Jr, King, P. & Schlegel, P. N. Incidental testicular lesions found during infertility evaluation are usually benign and may be managed conservatively. J. Urol. 180, 261–265 (2008).
Ragheb, D. & Higgins, J. L. J. Ultrasonography of the scrotum: technique, anatomy, and pathologic entities. J. Ultrasound Med. 21, 171–185 (2002).
Bertolotto, M., Valentino, M. & Sidhu, P. S. in Scrotal Pathology (eds Bertolotto, M. & Trombetta, C.) 343–352 (Springer Verlag, 2012).
Wilson, S. R. & Burns, P. N. Microbubble-enhanced US in body imaging: what role? Radiology 257, 24–39 (2010).
Valentino, M. et al. Role of contrast enhanced ultrasound in acute scrotal diseases. Eur. Radiol. 21, 1831–1840 (2011).
Schurich, M., Aigner, F., Frauscher, F. & Pallwein, L. The role of ultrasound in assessment of male fertility. Eur. J. Obstet. Gynecol. Reprod. Biol. 144 (Suppl. 1), S192–S198 (2009).
Moschouris, H., Stamatiou, K., Lampropoulou, E., Kalikis, D. & Matsaidonis, D. Imaging of the acute scrotum: is there a place for contrast-enhanced ultrasonography? Int. Braz. J. Urol. 35, 692–702 (2009).
Yamaguchi, A. et al. Testicular torsion: usefulness of contrast-enhanced power Doppler sonography. Int. J. Urol. 12, 849–851 (2005).
Lung, P. F. et al. Contrast-enhanced ultrasound in the evaluation of focal testicular complications secondary to epididymitis. AJR Am. J. Roentgenol. 199, W345–W354 (2012).
Yusuf, G., Sellars, M. E., Kooiman, G. G., Diaz-Cano, S. & Sidhu, P. S. Global testicular infarction in the presence of epididymitis: clinical features, appearances on grayscale, color Doppler, and contrast-enhanced sonography, and histologic correlation. J. Ultrasound Med. 32, 175–180 (2013).
Hedayati, V., Sellars, M. E., Sharma, D. M. & Sidhu, P. S. Contrast-enhanced ultrasound in testicular trauma: role in directing exploration, debridement and organ salvage. Br. J. Radiol. 85, e65–e68 (2012).
Lock, G., Schmidt, C., Helmich, F., Stolle, E. & Dieckmann, K. P. Early experience with contrast-enhanced ultrasound in the diagnosis of testicular masses: a feasibility study. Urology 77, 1049–1053 (2011).
Patel, K., Sellars, M. E., Clarke, J. L. & Sidhu, P. S. Features of testicular epidermoid cysts on contrast-enhanced sonography and real-time tissue elastography. J. Ultrasound Med. 31, 115–122 (2012).
Sarvazyan, A. et al. An overview of elastography—an emerging branch of medical imaging. Curr. Med. Imaging Rev. 7, 255–282 (2011).
Goddi, A., Bonardi, M. & Alessi, S. Breast elastography: a literature review. J. Ultrasound 15, 192–198 (2012).
Bamber, J. et al. EFSUMB guidelines and recommendations on the clinical use of ultrasound elastography. Part 1: basic principles and technology. Ultraschall. Med. 34, 169–184 (2013).
Salomon, G. et al. Evaluation of prostate cancer detection with ultrasound real-time elastography: a comparison with step section pathological analysis after radical prostatectomy. Eur. Urol. 54, 1354–1362 (2008).
Grasso, M., Blanco, S., Raber, M. & Nespoli, L. Elasto-sonography of the testis: preliminary experience. Arch. Ital. Urol. Androl. 82, 160–163 (2010).
Goddi, A., Sacchi, A., Magistretti, G., Almolla, J. & Salvadore, M. Real-time tissue elastography for testicular lesion assessment. Eur. Radiol. 22, 721–730 (2012).
Aigner, F. et al. Real-time sonoelastography for the evaluation of testicular lesions. Radiology 263, 584–589 (2012).
Kantarci, F., Cebi Olgun, D. & Mihmanli, I. Shear-wave elastography of segmental infarction of the testis. Korean J. Radiol. 13, 820–822 (2012).
Huang, D. Y. & Sidhu, P. S. Focal testicular lesions: colour Doppler ultrasound, contrast-enhanced ultrasound and tissue elastography as adjuvants to the diagnosis. Br. J. Radiol. 85, S41–S53 (2012).
Toren, P. J. et al. Small incidentally discovered testicular masses in infertile men—is active surveillance the new standard of care? J. Urol. 183, 1373–1377 (2010).
Stoehr, B. et al. Routine scrotal ultrasonography during the follow-up of patients with testicular cancer leads to earlier detection of asynchronous tumours and a high rate of organ preservation. BJU Int. 105, 1118–1120 (2009).
Kim, W. et al. US MR imaging correlation in pathologic conditions of the scrotum. Radiographics 27, 1239–1253 (2007).
Muglia, V. et al. Magnetic resonance imaging of scrotal diseases: when it makes the difference. Urology 59, 419–423 (2002).
Rholl, K. S., Lee, J. K., Ling, D., Heiken, J. P. & Glazer, H. S. MR imaging of the scrotum with a high-resolution surface coil. Radiology 163, 99–103 (1987).
Watanabe, Y. in Scrotal Pathology (eds Bertolotto, M. & Trombetta, C.) 17–26 (Springer Verlag, 2012).
Tsili, A. C. et al. Diffusion-weighted MR imaging of normal and abnormal scrotum: preliminary results. Asian J. Androl. 14, 649–654 (2012).
Rifkin, D. & Cochlin, L. Imaging of the Scrotum & Penis (Martin Dunitz, 2002).
Cassidy, F. H. et al. MR imaging of scrotal tumors and pseudotumors. Radiographics 30, 665–683 (2010).
Aganovic, L. & Cassidy, F. Imaging of the scrotum. Radiol. Clin. North Am. 50, 1145–1165 (2012).
Terai, A. et al. Dynamic contrast-enhanced subtraction magnetic resonance imaging in diagnostics of testicular torsion. Urology 67, 1278–1282 (2006).
Philips, S. et al. Benign non-cystic scrotal tumors and pseudotumors. Acta Radiol. 53, 102–111 (2012).
Mäkelä, E. et al. Magnetic resonance imaging of acute scrotum. Scand. J. Surg. 100, 196–201 (2011).
Bhatt, S., Jafri, S., Wasserman, N. & Dogra, V. S. Imaging of non-neoplastic intratesticular masses. Diagn. Interv. Radiol. 17, 52–63 (2011).
Dieckmann, K. P., Frey, U., Feyerabend, B., Pust, A. & Lock, G. Tubular ectasia of rete testis: a pitfall in ultrasonographic diagnostics of intratesticular cysts [German]. Urologe A 50, 57–63 (2011).
Parizel, P. M., Van Goethem, J. W., Ozsarlak, O., Maes, M. & Phillips, C. D. New developments in the neuroradiological diagnosis of craniocerebral trauma. Eur. Radiol. 15, 569–581 (2005).
Heinemann, V., Frey, U., Linke, J. & Dieckmann, K. P. Testicular microlithiasis. One case and for points to note. Scand. J. Urol. Nephrol. 37, 515–518 (2003).
Seidenwurm, D. et al. Testes and scrotum: MR imaging at 1.5 T. Radiology 164, 393–398 (1987).
Thurnher, S., Hricak, H., Carroll, P. R., Pobiel, R. S. & Filly, R. A. Imaging the testis: comparison between MR imaging and US. Radiology 167, 631–636 (1988).
Sohn, M., Neuerburg, J., Bohndorf, K., Sikora, R. & Daus, H. J. The value of magnetic resonance imaging at 1.5 T in the evaluation of the scrotal content. Urol. Int. 44, 284–291 (1989).
Cramer, B. M., Schlegel, E. A. & Thueroff, J. W. MR imaging in the differential diagnosis of scrotal and testicular disease. Radiographics 11, 9–21 (1991).
Just, M. et al. MR tomography in testicular processes. The significance of Gd-DTPA enhanced sequences in comparison with plain T2-weighted sequences [German]. Rofo 156, 527–531 (1992).
Derouet, H. et al. Nuclear magnetic resonance tomography for improving the differential diagnosis of pathologic changes in the scrotal contents [German]. Urologe A 32, 327–333 (1993).
Muller-Leisse, C. et al. Gadolinium-enhanced T1-weighted versus T2-weighted imaging of scrotal disorders: is there an indication for MR imaging? J. Magn. Reson. Imaging 45, 389–399 (1994).
Kaiser, W. A., Reinges, M. H., Miersch, W. D. & Vogel, J. Differentiation of testicular diseases using dynamic MRT [German]. Aktuelle Radiol. 4, 1–11 (1994).
Nagler-Reus, M., Guhl, L., Volz, C., Wuerstlin, S. & Arlart, I. P. Magnetic resonance tomography of the scrotum. Experiences with 129 patients [German]. Radiologe 35, 494–503 (1995).
Menzner, A., Kujat, C., Konig, J., Pahl, S. & Kramann, B. MRI in testicular diagnosis: differentiation of seminoma, teratoma and inflammation using a statistical score [German]. Rofo 166, 514–521 (1997).
Serra, A. D. et al. Inconclusive clinical and ultrasound evaluation of the scrotum: impact of magnetic resonance imaging on patient management and cost. Urology 51, 1018–1021 (1998).
Salamand, P., Mianne, D., Briant, J. F. & Richez, P. An MRI study of primary testicular tumors [French]. J. Radiol. 79, 865–870 (1998).
Andipa, E., Liberopoulos, K. & Asvestis, C. Magnetic resonance imaging and ultrasound evaluation of penile and testicular masses. World J. Urol. 22, 382–391 (2004).
Parenti, G. C. et al. Imaging of the scrotum: role of MRI [English, Italian]. Radiol. Med. 114, 414–424 (2009).
Tsili, A. C., Argyropoulou, M. I., Giannakis, D., Sofikitis, N. & Tsampoulas, K. MRI in the characterization and local staging of testicular neoplasms. AJR Am. J. Roentgenol. 194, 682–689 (2010).
Mohrs, O. K. et al. MRI of patients with suspected scrotal or testicular lesions: diagnostic value in daily practice. AJR Am. J. Roentgenol. 199, 609–615 (2012).
Woldrich, J. M., Im, R. D., Hughes-Cassidy, F., Aganovic, L. & Sakamoto, K. Magnetic resonance imaging for intratesticular and extratesticular scrotal lesions. Can. J. Urol. 20, 6855–6859 (2013).
Pizzocaro, G. & Guarneri, A. Inguinal orchidectomy for testicular cancer. BJU Int. 103, 704–716 (2009).
Goldstein, M. & Waterhouse, K. When to use the Chevassu maneuver during exploration of intrascrotal masses. J. Urol. 130, 1199–1200 (1983).
Nazeer, T., Ro, J. Y., Kee, K. H. & Ayala, A. G. Spermatic cord contamination in testicular cancer. Mod. Pathol. 9, 762–766 (1996).
Donohue, J. P., Zachary, J. M. & Maynard, B. R. Distribution of nodal metastases in nonseminomatous testis cancer. J. Urol. 128, 315–320 (1982).
Thorek, M. The human testis. (Lippincott, 1924).
Markland, C. Special problems in managing patients with testicular cancer. Urol. Clin. North Am. 4, 427–451 (1977).
Wilhelmi, B. J., Blackwell, S. J. & Philips, L. G. Langer's lines: to use or not to use. Plast. Reconstruct. Surg. 104, 208–212 (1999).
Heidenreich, A. & Albers, P. Ablatio testis and enucleation resection [German]. Aktuelle Urol. 40, 179–187 (2009).
Al-Assiri, M., Kevin, Z., Binsaleh, S. & Chan, P. T. Surgical approach of giant testicular cancer. Case report and literature review. Can. J. Urol. 12, 2557–2559 (2005).
Ashdown, D. A., Bodiwala, D. & Liu, S. Is high cord radical orchidectomy always necessary for testicular cancer? Ann. R. Coll. Surg. Engl. 86, 289–291 (2004).
Subik, M. K., Gordetsky, J., Yao, J. L., di Sant'Agnese, P. A. & Miyamoto, H. Frozen section assessment in testicular and paratesticular lesions suspicious for malignancy: its role in preventing unnecessary orchiectomy. Hum. Pathol. 43, 1514–1519 (2012).
Elert, A. et al. Accuracy of frozen section examination of testicular tumors of uncertain origin. Eur. Urol. 41, 290–293 (2002).
Connolly, S. S., D'Arcy, F. T., Bredin, H. C., Callaghan, J. & Corcoran, M. O. Value of frozen section analysis with suspected testicular malignancy. Urology 67, 162–165 (2006).
Hopps, C. V. & Goldstein, M. Ultrasound guided needle localization and microsurgical exploration for incidental nonpalpable testicular tumors. J. Urol. 168, 1084–1087 (2002).
Müller, T. et al. Management of incidental impalpable intratesticular masses of < or = 5 mm in diameter. BJU Int. 98, 1001–1004 (2006).
Avci, A., Erol, B., Eken, C. & Ozgok, Y. Nine cases of nonpalpable testicular mass: an incidental finding in a large scale ultrasonography survey. Int. J. Urol. 15, 833–836 (2008).
Powell, T. M. & Tarter, T. H. Management of nonpalpable incidental testicular masses. J. Urol. 176, 96–98 (2006).
Leroy, X., Rigot, J. M., Aubert, S., Ballereau, C. & Gosselin, B. Value of frozen section examination for the management of nonpalpable incidental testicular tumors. Eur. Urol. 44, 458–460 (2003).
Giannarini, G., Dieckmann, K. P., Albers, P., Heidenreich, A. & Pizzocaro, G. Organ-sparing surgery for adult testicular tumours: a systematic review of the literature. Eur. Urol. 57, 780–790 (2010).
Browne, R. F. et al. Technical report. Intra-operative ultrasound-guided needle localization for impalpable testicular lesions. Clin. Radiol. 58, 566–569 (2003).
Sheynkin, Y. R., Sukkarieh, T., Lipke, M., Cohen, H. L. & Schulsinger, D. A. Management of nonpalpable testicular tumors. Urology 63, 1163–1167 (2004).
Hallak, J. et al. Organ-sparing microsurgical resection of incidental testicular tumors plus microdissection for sperm extraction and cryopreservation in azoospermic patients: surgical aspects and technical refinements. Urology 73, 887–891 (2009).
Kirkham, A. P. et al. Targeted testicular excision biopsy: when and how should we try to avoid radical orchidectomy? Clin. Radiol. 64, 1158–1165 (2009).
Huyghe, E. et al. Conservative management of small testicular tumors relative to carcinoma in situ prevalence. J. Urol. 173, 820–823 (2005).
Passman, C. et al. Testicular lesions other than germ cell tumours: feasibility of testis-sparing surgery. BJU Int. 103, 488–491 (2009).
Ehrlich, Y., Konichezky, M., Yossepowitch, O. & Baniel, J. Multifocality in testicular germ cell tumors. J. Urol. 181, 1114–1120 (2009).
Dieckmann, K. P. et al. Treatment of testicular testicular neoplasia (intratubular germ cell neoplasia unspecified) with local radiotherapy or with platinum-based chemotherapy: a survey of the German Testicular Cancer Study Group. Ann. Oncol. 24, 1332–1337 (2013).
Ye, L., Wang, X., Zhang, Y., Ding, Q. & Wang, Y. Nonpalpable testicular masses incidentally discovered by ultrasound [Chinese]. Zhonghua Wai Ke Za Zhi 37, 168–170 (1999).
Tal, R., Holland, R., Belenky, A., Konichezky, M. & Baniel, J. Incidental testicular tumors in infertile men. Fertil. Steril. 82, 469–471 (2004).
Carmignani, L. et al. Prognostic parameters in adult impalpable ultrasonographic lesions of the testicle. J. Urol. 174, 1035–1038 (2005).
Connolly, S. S. et al. Carefully selected intratesticular lesions can be safely managed with serial ultrasonography. BJU Int. 98, 1005–1007 (2006).
Assaf, G. J. Non-palpable testicular lesion: the case for testicular preservation. Can. J. Urol. 13, 3034–3038 (2006).
Rolle, L. et al. Microsurgical “testis-sparing” surgery for nonpalpable hypoechoic testicular lesions. Urology 68, 381–385 (2006).
Onur, M. R. et al. Scrotal ultrasonography: should it be used in routine evaluation of infertile men? Andrologia 40, 58–61 (2008).
Acknowledgements
The authors are grateful to Dr Evelyn Stolle, Dr Claudia Schröder and Dr Christa Schmidt for fruitful discussions and valuable advice during preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
K.-P. Dieckmann and G. Lock researched data and wrote the article. All authors contributed to the discussion of content and reviewed the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
PowerPoint slides
Rights and permissions
About this article
Cite this article
Dieckmann, KP., Frey, U. & Lock, G. Contemporary diagnostic work-up of testicular germ cell tumours. Nat Rev Urol 10, 703–712 (2013). https://doi.org/10.1038/nrurol.2013.254
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrurol.2013.254
This article is cited by
-
Contrast-enhanced and microvascular ultrasound imaging features of testicular lymphoma: report of five cases and review literature
BMC Urology (2022)
-
Serum levels of microRNA-371a-3p are not elevated in testicular tumours of non-germ cell origin
Journal of Cancer Research and Clinical Oncology (2021)
-
Application of miRNAs in the diagnosis and monitoring of testicular germ cell tumours
Nature Reviews Urology (2020)
-
Testicular epidermoid cysts: a reevaluation
BMC Urology (2019)
-
Kontrastmittelsonographie bei Hodentumoren
Der Urologe (2019)