Key Points
-
The nature of a given active surveillance (AS) protocol is dependent on the three core components of AS: criteria for selection, monitoring strategy, and triggers for intervention
-
Among large AS programmes, selection criteria range from very-low-risk to intermediate-risk disease, and monitoring protocols vary widely in frequency of prostate biopsy; histological upgrading is a trigger for intervention in most programmes
-
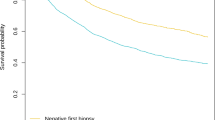
In AS cohorts with at least 5 years of available follow-up data, treatment was pursued in 24–40% of men; metastatic disease occurred in 0.1–2.8%, and prostate-cancer-specific death in 0–1.5%
-
Intermediate-term outcomes are dependent on programme-specific criteria; intensive programmes (close monitoring, low intervention thresholds) are associated with high rates of treatment and low rates of adverse oncological outcomes
-
In the absence of a single optimal AS protocol, individualizing AS intensiveness to each man's risks and expectations is a reasonable approach, only once he has been counselled on the existing data and its known limitations
-
Accurate measurement and reporting of time-dependent data are critical in order to establish reliable benchmarks for counselling and pave the way toward identifying an optimized approach
Abstract
Prostate cancer remains one of the most commonly diagnosed malignancies worldwide. Early diagnosis and curative treatment seem to improve survival in men with unfavourable-risk cancers, but significant concerns exist regarding the overdiagnosis and overtreatment of men with lower-risk cancers. To this end, active surveillance (AS) has emerged as a primary management strategy in men with favourable-risk disease, and contemporary data suggest that use of AS has increased worldwide. Although published surveillance cohorts differ by protocol, reported rates of metastatic disease and prostate-cancer-specific mortality are exceedingly low in the intermediate term (5–10 years). Such outcomes seem to be closely associated with programme-specific criteria for selection, monitoring, and intervention, suggesting that AS — like other management strategies — could be individualized based on the level of risk acceptable to patients in light of their personal preferences. Additional data are needed to better establish the risks associated with AS and to identify patient-specific characteristics that could modify prognosis.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Schröder, F. H. et al. Screening and prostate cancer mortality: results of the European Randomised Study of Screening for Prostate Cancer (ERSPC) at 13 years of follow-up. Lancet 384, 2027–2035 (2014).
Bill-Axelson, A. et al. Radical prostatectomy or watchful waiting in early prostate cancer. N. Engl. J. Med. 370, 932–942 (2014).
Wilt, T. J. et al. Radical prostatectomy versus observation for localized prostate cancer. N. Engl. J. Med. 367, 203–213 (2012).
Loeb, S. et al. Overdiagnosis and overtreatment of prostate cancer. Eur. Urol. 65, 1046–1055 (2014).
Heijnsdijk, E. A. M. et al. Quality-of-life effects of prostate-specific antigen screening. N. Engl. J. Med. 367, 595–605 (2012).
Cooperberg, M. R., Carroll, P. R. & Klotz, L. Active surveillance for prostate cancer: progress and promise. J. Clin. Oncol. 29, 3669–3676 (2011).
Choo, R. et al. Feasibility study: watchful waiting for localized low to intermediate grade prostate carcinoma with selective delayed intervention based on prostate specific antigen, histological and/or clinical progression. J. Urol. 167, 1664–1669 (2002).
Carter, H. B., Walsh, P. C., Landis, P. & Epstein, J. I. Expectant management of nonpalpable prostate cancer with curative intent: preliminary results. J. Urol. 167, 1231–1234 (2002).
Cooperberg, M. R., Broering, J. M., Kantoff, P. W. & Carroll, P. R. Contemporary trends in low risk prostate cancer: risk assessment and treatment. J. Urol. 178, S14–S19 (2007).
Cooperberg, M. R. & Carroll, P. R. Trends in management for patients with localized prostate cancer, 1990–2013. JAMA 314, 80–82 (2015).
Murphy, D. G. & Loeb, S. Prostate cancer: growth of AS in the USA signals reduction in overtreatment. Nat. Rev. Urol. 12, 604–605 (2015).
Ingimarsson, J. P., Celaya, M. O., Laviolette, M., Rees, J. R. & Hyams, E. S. Trends in initial management of prostate cancer in New Hampshire. Cancer Causes Control 26, 923–929 (2015).
Womble, P. R. et al. Contemporary use of initial active surveillance among men in Michigan with low-risk prostate cancer. Eur. Urol. 67, 44–50 (2014).
Filson, C. P. et al. Expectant management of veterans with early-stage prostate cancer. Cancer 122, 626–633 (2015).
Loeb, S., Berglund, A. & Stattin, P. Population based study of use and determinants of active surveillance and watchful waiting for low and intermediate risk prostate cancer. J. Urol. 190, 1742–1749 (2013).
Weerakoon, M. et al. The current use of active surveillance in an Australian cohort of men: a pattern of care analysis from the Victorian Prostate Cancer Registry. BJU Int. 115 (Suppl.), 50–56 (2015).
Mitsuzuka, K. et al. Current use of active surveillance for localized prostate cancer: a nationwide survey in Japan. Int. J. Urol. 22, 754–759 (2015).
Louis, A. S. et al. Oncologic outcomes following radical prostatectomy in the active surveillance era. Can. Urol. Assoc. J. 7, E475–E480 (2013).
Huland, H. & Graefen, M. Changing trends in surgical management of prostate cancer: the end of overtreatment? Eur. Urol. 68, 175–178 (2015).
Tosoian, J. J. et al. Intermediate and longer-term outcomes from a prospective active-surveillance program for favorable-risk prostate cancer. J. Clin. Oncol. 33, 3379–3385 (2015).
Klotz, L. et al. Long-term follow-up of a large active surveillance cohort of patients with prostate cancer. J. Clin. Oncol. 33, 272–277 (2015).
Godtman, R. A., Holmberg, E., Khatami, A., Stranne, J. & Hugosson, J. Outcome following active surveillance of men with screen-detected prostate cancer. Results from the Göteborg randomised population-based prostate cancer screening trial. Eur. Urol. 63, 101–107 (2013).
Welty, C. J. et al. Extended followup and risk factors for disease reclassification in a large active surveillance cohort for localized prostate cancer. J. Urol. 193, 807–811 (2015).
Selvadurai, E. D. et al. Medium-term outcomes of active surveillance for localised prostate cancer. Eur. Urol. 64, 981–987 (2013).
Thompson, J. E. et al. Medium-term oncological outcomes for extended versus saturation biopsy and transrectal versus transperineal biopsy in active surveillance for prostate cancer. BJU Int. 115, 884–891 (2015).
Bul, M. et al. Active surveillance for low-risk prostate cancer worldwide: the PRIAS study. Eur. Urol. 63, 597–603 (2013).
Thomsen, F. B., Røder, M. A., Hvarness, H., Iversen, P. & Brasso, K. Active surveillance can reduce overtreatment in patients with low-risk prostate cancer. Dan. Med. J. 60, A4575 (2013).
Soloway, M. S. et al. Careful selection and close monitoring of low-risk prostate cancer patients on active surveillance minimizes the need for treatment. Eur. Urol. 58, 831–835 (2010).
Epstein, J. I., Walsh, P. C. & Brendler, C. B. Radical prostatectomy for impalpable prostate cancer: the Johns Hopkins experience with tumors found on transurethral resection (stages T1A and T1B) and on needle biopsy (stage T1C). J. Urol. 152, 1721–1729 (1994).
Bastian, P. J., Mangold, L. A., Epstein, J. I. & Partin, A. W. Characteristics of insignificant clinical T1c prostate tumors. Cancer 101, 2001–2005 (2004).
Mohler, J. L. et al. Clinical Practice Guidelines in Oncology (NCCN Guideline): Prostate Cancer. Version 2 (2016).
Umbehr, M. H. et al. Serum prostate-specific antigen (PSA) concentration is positively associated with rate of disease reclassification on subsequent active surveillance prostate biopsy in men with low PSA density. BJU Int. 113, 561–567 (2014).
Faisal, F. A. et al. Outcomes of men with an elevated prostate-specific antigen (PSA) level as their sole preoperative intermediate- or high-risk feature. BJU Int. 114, E120–E129 (2014).
Reese, A. C., Landis, P., Han, M., Epstein, J. I. & Carter, H. B. Expanded criteria to identify men eligible for active surveillance of low risk prostate cancer at Johns Hopkins: a preliminary analysis. J. Urol. 190, 2033–2038 (2013).
Loeb, S. et al. Active surveillance for prostate cancer: a systematic review of clinicopathologic variables and biomarkers for risk stratification. Eur. Urol. 67, 619–626 (2015).
Adamy, A. et al. Role of prostate specific antigen and immediate confirmatory biopsy in predicting progression during active surveillance for low risk prostate cancer. J. Urol. 185, 477–482 (2011).
Soloway, M. S. et al. Active surveillance; a reasonable management alternative for patients with prostate cancer: the Miami experience. BJU Int. 101, 165–169 (2008).
Ross, A. E. et al. Prostate-specific antigen kinetics during follow-up are an unreliable trigger for intervention in a prostate cancer surveillance program. J. Clin. Oncol. 28, 2810–2816 (2010).
Whitson, J. M. et al. The relationship between prostate specific antigen change and biopsy progression in patients on active surveillance for prostate cancer. J. Urol. 185, 1656–1660 (2011).
Klotz, L. Defining 'progression' and triggers for curative intervention during active surveillance. Curr. Opin. Urol. 25, 258–266 (2015).
Iremashvili, V. et al. Comprehensive analysis of post-diagnostic prostate-specific antigen kinetics as predictor of a prostate cancer progression in active surveillance patients. BJU Int. 111, 396–403 (2013).
Patel, H. D. et al. Prostate specific antigen velocity risk count predicts biopsy reclassification for men with very low risk prostate cancer. J. Urol. 191, 629–637 (2013).
San Francisco, I. F. et al. Risk stratification and validation of prostate specific antigen density as independent predictor of progression in men with low risk prostate cancer during active surveillance. J. Urol. 185, 471–476 (2011).
Catalona, W. J. et al. A multicenter study of [-2]pro-prostate specific antigen combined with prostate specific antigen and free prostate specific antigen for prostate cancer detection in the 2.0 to 10.0 ng/ml prostate specific antigen range. J. Urol. 185, 1650–1655 (2011).
Loeb, S. et al. The Prostate Health Index selectively identifies clinically significant prostate cancer. J. Urol. 193, 1163–1169 (2014).
Tosoian, J. J. et al. Association of [-2]proPSA with biopsy reclassification during active surveillance for prostate cancer. J. Urol. 188, 1131–1136 (2012).
Hirama, H., Sugimoto, M., Ito, K., Shiraishi, T. & Kakehi, Y. The impact of baseline [−2]proPSA-related indices on the prediction of pathological reclassification at 1 year during active surveillance for low-risk prostate cancer: the Japanese multicenter study cohort. J. Cancer Res. Clin. Oncol. 140, 257–263 (2013).
Lin, D. W. et al. Urinary TMPRSS2:ERG and PCA3 in an active surveillance cohort: results from a baseline analysis in the canary prostate active surveillance study. Clin. Cancer Res. 19, 2442–2450 (2013).
Tosoian, J. J. et al. Accuracy of PCA3 measurement in predicting short-term biopsy progression in an active surveillance program. J. Urol. 183, 534–538 (2010).
Cornu, J.-N. N. et al. Urine TMPRSS2:ERG fusion transcript integrated with PCA3 score, genotyping, andbiological features are correlated to the results of prostatic biopsies in men at risk of prostate cancer. Prostate 73, 242–249 (2013).
Cuzick, J. et al. Prognostic value of a cell cycle progression signature for prostate cancer death in a conservatively managed needle biopsy cohort. Br. J. Cancer 106, 1095–1099 (2012).
Bishoff, J. T. et al. Prognostic utility of the cell cycle progression score generated from biopsy in men treated with prostatectomy. J. Urol. 192, 409–414 (2014).
Freedland, S. J. et al. Prognostic utility of cell cycle progression score in men with prostate cancer after primary external beam radiation therapy. Int. J. Radiat. Oncol. Biol. Phys. 86, 848–853 (2013).
Crawford, E. D. et al. Cell cycle progression score and treatment decisions in prostate cancer: results from an ongoing registry. Curr. Med. Res. Opin. 30, 1025–1031 (2014).
Klein, E. A. et al. A 17-gene assay to predict prostate cancer aggressiveness in the context of Gleason grade heterogeneity, tumor multifocality, and biopsy undersampling. Eur. Urol. 66, 550–560 (2014).
Cullen, J. et al. A biopsy-based 17-gene genomic prostate score predicts recurrence after radical prostatectomy and adverse surgical pathology in a racially diverse population of men with clinically low- and intermediate-risk prostate cancer. Eur. Urol. 68, 123–131 (2014).
Blume-Jensen, P. et al. Development and clinical validation of an in situ biopsy based multi-marker assay for risk stratification in prostate cancer. Clin. Cancer Res. http://dx.doi.org/10.1158/1078-0432.CCR-14-2603 (2015).
Hamoen, E. H. J., de Rooij, M., Witjes, J. A., Barentsz, J. O. & Rovers, M. M. Use of the Prostate Imaging Reporting and Data System (PI-RADS) for prostate cancer detection with multiparametric magnetic resonance imaging: a diagnostic meta-analysis. Eur. Urol. 67, 1112–1121 (2014).
Dianat, S. S. et al. Association of quantitative magnetic resonance imaging parameters with histological findings from MRI/ultrasound fusion prostate biopsy. Can. J. Urol. 22, 7965–7972 (2015).
Russo, F. et al. Detection of prostate cancer index lesions with multiparametric magnetic resonance imaging (mp-MRI) using whole-mount histological sections as the reference standard. BJU Int. http://dx.doi.org/10.1111/bju.13234 (2015).
Vargas, H. A. et al. Updated prostate imaging reporting and data system (PIRADS v2) recommendations for the detection of clinically significant prostate cancer using multiparametric MRI: critical evaluation using whole-mount pathology as standard of reference. Eur. Radiol. http://dx.doi.org/10.1007/s00330-015-4015-6 (2015).
Fütterer, J. J. et al. Can clinically significant prostate cancer be detected with multiparametric magnetic resonance imaging? A systematic review of the literature. Eur. Urol. 68, 1045–1053 (2015).
Siddiqui, M. M. et al. Comparison of MR/ultrasound fusion-guided biopsy with ultrasound-guided biopsy for the diagnosis of prostate cancer. JAMA 313, 390 (2015).
de Cobelli, O. et al. Predicting pathological features at radical prostatectomy in patients with prostate cancer eligible for active surveillance by multiparametric magnetic resonance imaging. PLoS ONE 10, e0139696 (2015).
Maxeiner, A. et al. Added value of multiparametric ultrasonography in magnetic resonance imaging and ultrasonography fusion-guided biopsy of the prostate in patients with suspicion for prostate cancer. Urology 86, 108–114 (2015).
Meng, X. et al. Relationship between prebiopsy multiparametric magnetic resonance imaging (MRI), biopsy indication, and MRI-ultrasound fusion-targeted prostate biopsy outcomes. Eur. Urol. 69, 512–517 (2015).
Eggener, S. E. et al. Predicting 15-year prostate cancer specific mortality after radical prostatectomy. J. Urol. 185, 869–875 (2011).
Cooperberg, M. R. et al. Outcomes of active surveillance for men with intermediate-risk prostate cancer. J. Clin. Oncol. 29, 228–234 (2011).
Bechis, S. K., Carroll, P. R. & Cooperberg, M. R. Impact of age at diagnosis on prostate cancer treatment and survival. J. Clin. Oncol. 29, 235–241 (2011).
Campodonico, F. & Maffezzini, M. Active surveillance in young patients with prostate cancer: the unanswered question. J. Clin. Oncol. 28, e211; author reply e212 (2010).
Lin, D. W., Porter, M. & Montgomery, B. Treatment and survival outcomes in young men diagnosed with prostate cancer. Cancer 115, 2863–2871 (2009).
Howlader, N. et al. SEER cancer statistics review, 1975–2011. National Cancer Institute [online], (2014).
Hampson, L. A., Cowan, J. E., Zhao, S., Carroll, P. R. & Cooperberg, M. R. Impact of age on quality-of-life outcomes after treatment for localized prostate cancer. Eur. Urol. 68, 480–486 (2015).
McGinley, K. F., Tay, K. J. & Moul, J. W. Prostate cancer in men of African origin. Nat. Rev. Urol. 13, 99–107 (2016).
Odom, B. D. et al. Active surveillance for low-risk prostate cancer in African American men: a multi-institutional experience. Urology 83, 364–368 (2014).
Silberstein, J. L. et al. Active surveillance of prostate cancer in African American men. Urology 84, 1255–1261 (2014).
Ha, Y.-S. et al. Increased incidence of pathologically nonorgan confined prostate cancer in African-American men eligible for active surveillance. Urology 81, 831–835 (2013).
Sundi, D. et al. African American men with very low-risk prostate cancer exhibit adverse oncologic outcomes after radical prostatectomy: should active surveillance still be an option for them? J. Clin. Oncol. 31, 2991–2997 (2013).
Moul, J. W. Prostate cancer: active surveillance in African American men. Nat. Rev. Urol. 10, 311–312 (2013).
Iremashvili, V., Soloway, M. S., Rosenberg, D. L. & Manoharan, M. Clinical and demographic characteristics associated with prostate cancer progression in patients on active surveillance. J. Urol. 187, 1594–1600 (2012).
Abern, M. R. et al. Race is associated with discontinuation of active surveillance of low-risk prostate cancer: results from the Duke Prostate Center. Prostate Cancer Prostatic Dis. 16, 85–90 (2012).
Sundi, D. et al. Pathologic examination of radical prostatectomies in men with very-low-risk disease at biopsy reveals distinct zonal distribution of cancer in African American men. J. Urol. 191, 60–67 (2013).
Pettaway, C. A. et al. Prostate specific antigen and pathological features of prostate cancer in black and white patients: a comparative study based on radical prostatectomy specimens. J. Urol. 160, 437–442 (1998).
Schreiber, D., Chhabra, A., Rineer, J., Weedon, J. & Schwartz, D. A. Population-based study of men with low-volume low-risk prostate cancer: does African-American race predict for more aggressive disease? Clin. Genitourin. Cancer 13, e259–e264 (2015).
Pietzak, E. J. et al. Impact of race on selecting appropriate patients for active surveillance with seemingly low-risk prostate cancer. Urology 85, 436–440 (2015).
Pound, C. R. et al. Natural history of progression after PSA elevation following radical prostatectomy. JAMA 281, 1591–1597 (1999).
Punnen, S., Pavan, N. & Parekh, D. J. Finding the wolf in sheep's clothing: the 4Kscore is a novel blood test that can accurately identify the risk of aggressive prostate cancer. Rev. Urol. 17, 3–13 (2015).
Sammon, J. D. et al. Predicting life expectancy in men diagnosed with prostate cancer. Eur. Urol. 68, 756–765 (2015).
Kent, M. & Vickers, A. J. A. Systematic literature review of life expectancy prediction tools for patients with localized prostate cancer. J. Urol. 193, 1938–1942 (2015).
El Hajj, A. et al. Patient selection and pathological outcomes using currently available active surveillance criteria. BJU Int. 112, 471–477 (2013).
Ploussard, G. et al. Can we expand active surveillance criteria to include biopsy Gleason 3+4 prostate cancer? A multi-institutional study of 2,323 patients. Urol. Oncol. 33, 71.e1–71.e9 (2015).
Ankerst, D. P. et al. Precision medicine in active surveillance for prostate cancer: development of the Canary–Early Detection Research Network Active Surveillance Biopsy Risk Calculator. Eur. Urol. 68, 1083–1088 (2015).
Tosoian, J. J. et al. Pathological outcomes in men with low risk and very low risk prostate cancer: implications on the practice of active surveillance. J. Urol. 190, 1218–1222 (2013).
Mamawala, M. et al. Risk prediction tool for grade reclassification in active surveillance. J. Urol. (in the press).
Alam, R., Carter, H. B., Landis, P., Epstein, J. I. & Mamawala, M. Conditional probability of reclassification in an active surveillance program for prostate cancer. J. Urol. 193, 1950–1955 (2015).
Linder, B. J. et al. Standard and saturation transrectal prostate biopsy techniques are equally accurate among prostate cancer active surveillance candidates. Int. J. Urol. 20, 860–864 (2013).
Inoue, L. Y. T., Trock, B. J., Partin, A. W., Carter, H. B. & Etzioni, R. Modeling grade progression in an active surveillance study. Stat. Med. 33, 930–939 (2014).
Radtke, J. P. et al. Comparative analysis of transperineal template-saturation prostate biopsy versus MRI-targeted biopsy with MRI-US fusion-guidance. J. Urol. 193, 87–94 (2014).
Bjurlin, M. A. et al. Optimization of initial prostate biopsy in clinical practice: sampling, labeling and specimen processing. J. Urol. 189, 2039–2046 (2013).
Berglund, R. K. et al. Pathological upgrading and up staging with immediate repeat biopsy in patients eligible for active surveillance. J. Urol. 180, 1964–1967; discussion 1967–1968 (2008).
Kates, M. et al. Indications for intervention during active surveillance of prostate cancer: a comparison of the Johns Hopkins and PRIAS protocols. BJU Int. 115, 216–222 (2014).
National Comprehensive Cancer Network. About NCCN. [online]
Pierorazio, P. M., Walsh, P. C., Partin, A. W. & Epstein, J. I. Prognostic Gleason grade grouping: data based on the modified Gleason scoring system. BJU Int. 111, 753–760 (2013).
Acknowledgements
S.L. is supported by the Laura & Isaac Perlmutter NYU Cancer Center (P30CA016087), the Louis Feil Charitable Lead Trust and the National Institutes of Health under Award Number K07CA178258. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
J.J.T., A.L. and S.L. researched data for the article. All authors contributed to discussion of content, wrote the manuscript, and reviewed and edited the article before submission.
Corresponding author
Ethics declarations
Competing interests
S.L. has acted as an advisor for Bayer Corp. The other authors declare no competing interests.
Glossary
- Favourable-risk
-
Defined herein as a composite group consisting of NCCN very-low-risk and low-risk prostate cancer.
- Progression
-
A variably defined term, typically in reference to an increase in risk classification. Depending on source, progression can be defined according to any number of measures, including, but not limited, to clinical stage, serological findings, histological findings, radiographic imaging, symptomatology, and requirement of initial or additional therapies. As such, progression should be explicitly defined when used, and its use should be deferred in favour of more specific language as possible.
- Reclassification
-
Increase in risk categorization based specifically on prostate biopsy findings; the term reclassification includes volume reclassification and grade reclassification.
- National Comprehensive Cancer Network
-
(NCCN). An alliance of leading US cancer centres devoted to patient care, research, and education. The NCCN develops and communicates scientific, evaluative information to better inform the decision-making process between patients and physicians102.
- Low-intermediate risk
-
A subpopulation within the NCCN intermediate-risk category that includes only those men with Gleason score 3 + 4 = 7 disease (prognostic grade group 2 as defined by Pierorazio et al.103).
- Risk classification
-
Use of patient-specific data to classify patients according to their risk of disease recurrence or progression. Unless otherwise indicated, risk categorization is herein based upon NCCN definitions of very-low-risk, low-risk, intermediate-risk, or high-risk clinically localized disease31.
- Volume reclassification
-
Increase in risk categorization based on increased volume of cancer on prostate biopsy. As very-low-risk cancer is the only risk category based on cancer-volume-specific criteria, volume reclassification occurs only in men harbouring very-low-risk disease.
- Grade reclassification
-
Increase in risk categorization based on evidence of a higher grade of cancer on prostate biopsy (Gleason score upgrading). The term traditionally refers to men on AS with Gleason score 3 + 3 = 6 cancer who are subsequently found to have any Gleason pattern 4 or 5 cancer.
Rights and permissions
About this article
Cite this article
Tosoian, J., Carter, H., Lepor, A. et al. Active surveillance for prostate cancer: current evidence and contemporary state of practice. Nat Rev Urol 13, 205–215 (2016). https://doi.org/10.1038/nrurol.2016.45
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrurol.2016.45
This article is cited by
-
Evaluation of AR, AR-V7, and p160 family as biomarkers for prostate cancer: insights into the clinical significance and disease progression
Journal of Cancer Research and Clinical Oncology (2024)
-
Active surveillance in intermediate-risk prostate cancer with PSA 10–20 ng/mL: pathological outcome analysis of a population-level database
Prostate Cancer and Prostatic Diseases (2022)
-
The role of metformin, statins and diet in men on active surveillance for prostate cancer
World Journal of Urology (2022)
-
Longitudinal evaluation of apparent diffusion coefficient values as a predictor of Prostate Cancer Research International Active Surveillance reclassification
Abdominal Radiology (2022)
-
Long-term use of 5-alpha-reductase inhibitors is safe and effective in men on active surveillance for prostate cancer
Prostate Cancer and Prostatic Diseases (2021)