Abstract
BACKGROUND:
To assess the impact of the degree of extraprostatic extension (EPE) on biochemical recurrence (BCR) and utility of the original Epstein’s criteria to define EPE in a cohort of pT3aN0 without positive surgical margin (PSM).
METHODS:
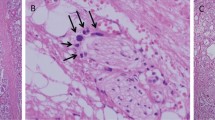
A two-center retrospective analysis was performed on data from 490 pT3aN0 patients who underwent radical prostatectomy between 2000 and 2012. Patients with neoadjuvant and/or adjuvant therapy, detectable PSA and PSM were excluded. Our pathologists used Epstein’s criteria to report the degree of EPE. When pathology reports did not reflect the terms 'focal' or 'established' (non-focal), slides were analyzed by a single genitourinary pathologist for final evaluation. The end point was defined by BCR.
RESULTS:
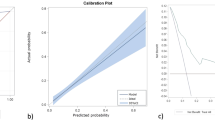
Selection criteria yielded 247 patients. Mean follow-up was 56.3±4.6 months; mean age at surgery was 62.5 years. Sixty-one (24.7%) patients experienced BCR during follow-up. Patients with focal extension had a 5-year recurrence-free survival of 89% versus 80% for those with non-focal extension (P=0.0018). In multivariate analysis, both pathologic Gleason score (hazard ratio 2.5; 95% confidence interval 1.4–4.5; P=0.002) and the extent of EPE (hazard ratio 1.8; 95% confidence interval 1.1–3.5; P=0.029) were significant predictors of BCR.
CONCLUSIONS:
The extent of EPE is an independent predictor of BCR in pT3aN0 prostate cancer without PSM. This study reinforces the utility of the subjective Epstein approach already adopted by most pathologists for quantification of the extent of EPE.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Srigley JR . Key issues in handling and reporting radical prostatectomy specimens. Arch Pathol Lab Med. 2006; 130: 303–317.
Cheng L, Darson MF, Bergstralh EJ, Slezak J, Myers RP, Bostwick DG . Correlation of margin status and extraprostatic extension with progression of prostate carcinoma. Cancer 1999; 86: 1775–1782.
Swanson GP, Riggs M, Hermans M . Pathologic findings at radical prostatectomy: risk factors for failure and death. Urol Oncol. 2007; 25: 110–114.
Epstein JI, Carmichael MJ, Pizov G, Walsh PC . Influence of capsular penetration on progression following radical prostatectomy: a study of 196 cases with long-term followup. J Urol. 1993; 150: 135–141.
Wheeler TM, Dillioglugil O, Kattan MW, Arakawa A, Soh S, Suyama K et al. Clinical and pathological significance of the level and extent of capsular invasion in clinical stage T1-2 prostate cancer. Hum Pathol. 1998; 29: 856–862.
Davis BJ, Pisansky TM, Wilson TM, Rothenberg HJ, Pacelli A, Hillman DW et al. The radial distance of extraprostatic extension of prostate carcinoma: implications for prostate brachytherapy. Cancer 1999; 85: 2630–2637.
Sung M-T, Lin H, Koch MO, Davidson DD, Cheng L . Radial distance of extraprostatic extension measured by ocular micrometer is an independent predictor of prostate-specific antigen recurrence: a new proposal for the substaging of pT3a prostate cancer. Am J Surg Pathol. 2007; 31: 311–318.
Magi- Galluzzi C, Evans AJ, Delahunt B, Epstein JI, Griffiths DF, Van der Kwast TH et al. International Society of Urological Pathology (ISUP) consensus conference on handling and staging of radical prostatectomy specimens. working group 3: extraprostatic extension, lymphovascular invasion and locally advanced disease. Modern Pathol 2011; 24: 26–38.
Roehl KA, Han M, Ramos CG, Antenor JA, Catalona WJ . Cancer progression and survival rates following anatomical radical retropubic prostatectomy in 3478 consecutive patients: long-term results. J Urol. 2004; 172: 910–914.
Danneman D, Wiklund F, Wiklund NP, Egevad L . Prognostic significance of histopathological features of extraprostatic extension of prostate cancer. Histopathology 2013; 63: 580–589.
Ball MW, Partin AW, Epstein JI . Extent of extraprostatic extension independently influences biochemical recurrence-free survival: evidence for further pT3 subclassification. Urology 2015; 85: 161–164.
Jeong BC, Chalfin HJ, Lee SB, Feng Z, Epstein JI, Trock BJ et al. The relationship between the extent of extraprostatic extension and survival following radical prostatectomy. Eur Urol. 2015; 67: 342–346.
Schmid HP, McNeal JE . An abbreviated standard procedure for accurate tumor volume estimation in prostate cancer. Am J Surg Pathol. 1992; 16: 184–191.
Epstein JI, Allsbrook WCJ, Amin MB, Egevad LL, ISUP Grading Committee. The 2005 International Society of Urological Pathology (ISUP) Consensus Conference on Gleason Grading of Prostatic Carcinoma. Am J Surg Pathol 2005; 29: 1228–1242.
Ohori M, Wheeler TM, Kattan MW, Goto Y, Scardino PT . Prognostic significance of positive surgical margins in radical prostatectomy specimens. J Urol. 1995; 154: 1818–1824.
Yossepowitch O, Briganti A, Eastham JA, Epstein J, Graefen M, Montironi R et al. Positive surgical margins after radical prostatectomy: a systematic review and contemporary update. Eur Urol. 2014; 65: 303–313.
Budäus L, Isbarn H, Eichelberg C, Lughezzani G, Sun M, Perrotte P et al. Biochemical recurrence after radical prostatectomy: multiplicative interaction between surgical margin status and pathological stage. J Urol. 2010; 184: 1341–1346.
D’Amico AV, Whittington R, Malkowicz SB, Schultz D, Tomaszewski JE, Wein A . Prostate specific antigen outcome based on the extent of extracapsular extension and margin status in patients with seminal vesicle negative prostate carcinoma of Gleason score < or = 7. Cancer 2000; 88: 2110–2115.
Johnson MT, Ramsey ML, Ebel JJ, Abaza R, Zynger DL et al. Do robotic prostatectomy positive surgical margins occur in the same location as extraprostatic extension? World J Urol 2014; 32: 761–767.
Sakr WA, Tefilli MV, Grignon DJ, Banerjee M, Dey J, Gheiler EL et al. Gleason score 7 prostate cancer: a heterogeneous entity? correlation with pathologic parameters and disease-free survival. Urology 2000; 56: 730–734.
Cheng L, Montironi R, Bostwick DG, Lopez-Beltran A, Berney DM . Staging of prostate cancer. Histopathology 2012; 60: 87–117.
Ayala AG, Ro JY, Babaian R, Troncoso P, Grignon DJ . The prostatic capsule: does it exist? Its importance in the staging and treatment of prostatic carcinoma. Am J Surg Pathol. 1989; 13: 21–27.
van Veggel BAMH, van Oort IM, Witjes JA, Kiemeney LALM, Hulsbergen-van de Kaa CA . Quantification of extraprostatic extension in prostate cancer: different parameters correlated to biochemical recurrence after radical prostatectomy. Histopathology 2011; 59: 692–702.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Maubon, T., Branger, N., Bastide, C. et al. Impact of the extent of extraprostatic extension defined by Epstein’s method in patients with negative surgical margins and negative lymph node invasion. Prostate Cancer Prostatic Dis 19, 317–321 (2016). https://doi.org/10.1038/pcan.2016.24
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pcan.2016.24
This article is cited by
-
Prediction of extraprostatic extension on multi-parametric magnetic resonance imaging in patients with anterior prostate cancer
European Radiology (2020)
-
Digital versus light microscopy assessment of extraprostatic extension in radical prostatectomy samples
Virchows Archiv (2019)
-
Preoperative Predictors of Extraprostatic Extension of Prostate Cancer (pT3a) in a Contemporary Indian Cohort
Indian Journal of Surgical Oncology (2017)