Abstract
Background
To test the hypothesis that dopamine is associated with impaired cerebral autoregulation (ICA) in a dose-dependent fashion.
Methods
Non a priori designed secondary analysis of a prospectively enrolled cohort study subjects <12 h of life between 240 and 296 weeks gestation. Cerebral saturations (rScO2) and mean arterial blood pressure (MAP) were continuously monitored every 30 s for 96 h. ICA was defined by a 10 min epoch rScO2-MAP correlation coefficient of >0.5.
Results
Twenty-three of 61 subjects (38%) required dopamine. Time spent with ICA was 23% in dopamine-exposed subjects vs. 14% in those not exposed (p = 0.0001). On the epoch level, time spent with ICA was 15%, 29%, 34%, 37%, and 23% in epochs with dopamine titration of 0, 1–5, 6–10, 11–15, and 16–20 μg/kg/min, respectively. Using mixed-effect modeling, ICA for each dopamine titration was significantly higher than unexposed times when controlling for gestation, presence of a patent ductus arteriosus, day of life, MAP less than gestational age, and illness severity score (p < 0.02).
Conclusions
Dopamine exposure during the first 96 h was associated with ICA. Time periods with ICA increased with dopamine exposure in a dose-dependent fashion peaking at a concentration of 11–15 μg/kg/min.
Similar content being viewed by others
Introduction
Up to 50% of premature infants will be diagnosed with hypotension during the first 4 days of life, and of those up to half will be treated with vasopressor therapy.1,2,3 Hypotension, although not well defined in this population, is known to be associated with increased morbidity (intraventricular hemorrhage (IVH) and neurologic impairments) and mortality, especially when requiring vasopressor therapy.4,5,6,7,8 Dopamine is the most commonly used vasopressor in neonatal care because of its ability to effectively increase mean arterial pressure (MAP), but its effect on cerebral blood flow is uncertain.4,5
In the premature infant, impaired cerebral autoregulation (ICA) is common, and has been associated with increased mortality and cerebral injury such as IVH and periventricular leukomalacia (PVL).5,9,10,11 Near-infrared spectroscopy has been used to measure cerebral oxygen saturation (rScO2) and is used as a surrogate marker of cerebral blood flow. In neonates, the correlation of MAP and rScO2 has been used to evaluate ICA, with a correlation coefficient >0.5 indicative of ICA.4,5,12,13,14
Generally, infants with a greater severity of illness are more likely to be treated with dopamine; however, the treatment of hypotension with dopamine has an unclear effect on the neonatal vasculature. Although there is evidence that dopamine exposure is associated with ICA during the first days of life,4,5 understanding of this association continues to be limited. The effect of different dopamine doses on cerebral autoregulation has not been well studied, but research suggests percent time spent with impaired autoregulation increases with higher doses of dopamine.15 In addition, cerebral autoregulation may remain impaired despite a restoration of blood pressure in response to dopamine, suggesting that dopamine exposure may play a role in this impairment independent of blood pressure.4 This study aims to test the hypothesis that dopamine is associated with ICA in a dose-dependent fashion.
Methods
Population and data collection
This is a non a priori designed secondary analysis of a prospectively enrolled cohort study of subjects 240–296 weeks gestation admitted to the University of Maryland Medical Center level IV neonatal intensive care unit (NICU) between June 2013 and September 2016 who had continuous intra-arterial blood pressure monitoring within the first 12 h of life.10 Subjects were excluded for parental refusal of participation, major congenital anomalies, or <12 h of monitoring. Demographic and clinical data were obtained from the medical record for each patient. The SNAPPE-II (Score for Neonatal Acute. Physiology-Perinatal Extension II) illness severity score was calculated for each patient.16 The presence of a patent ductus arteriosus (PDA) was confirmed by echocardiography. Head ultrasounds were obtained at the discretion of the clinician, but generally performed within the first 72 h of life. Although there was no specific blood pressure treatment protocol, generally, MAP less than gestational age (GA) and signs of systemic hypoperfusion were criteria used to direct management. Dopamine was the first line vasopressor used.
Continuous data monitoring and processing
Cerebral saturations were evaluated with the NIRS device (INVOS 5100C, Covidien, Mansfield, MA, USA) using a neonatal sensor within 12 h of life and continued for 96 h or until intra-arterial line was removed. MAP was continuously monitored by using indwelling umbilical or peripheral arterial catheter. Data were continuously recorded and time synchronized every 30 s using a data aggregation device (Vital Sync, Covidien, Mansfield, MA, USA). The data were retrospectively reviewed and artifacts in MAP and rScO2, such as those due to blood sampling and movement, were filtered by requiring the MAP to be between 15 and 70 mmHg, requiring more than a 2 mmHg difference between systolic and diastolic blood pressure, and removing time periods of non-physiologic rScO2 changes. Time periods with significant hypoxemia, SpO2 <80%, were removed from analysis according to the previous methodology.10,13
Every 10 min epoch for each patient was categorized into dopamine exposure or no dopamine exposure. Then, each epoch was further subdivided into titrations of dopamine (no dopamine, 1–5 μg/kg/min, 6–10 μg/kg/min, 11–15 μg/kg/min, and 16–20 μg/kg/min). Epochs that contained time points with varying dopamine titration were removed.
Statistical analysis
Statistical analysis was performed using SAS V.9.3 software (SAS Institute). Continuous data are presented as mean ± standard deviation or median (range) depending on the distribution. Categorical data are presented as number (%). Subjects with and without dopamine exposure were compared for demographic and clinical characteristics using t test, Wilcoxon’s rank sum, χ2, or Fischer’s exact test as appropriate for the type and distribution of the data. For each subject, the median and maximum dopamine titration was calculated. For each dopamine titration category, the percent time spent with MAP less than GA was calculated and groups were compared using mixed-effect analysis.
The study period was divided into 10 min contiguous epochs with time of birth as time zero. For each epoch, the Pearson’s correlation coefficient (r) between MAP and rScO2 was calculated. If the correlation coefficient was >0.5, the subject was considered to have ICA.10,17 For each subject, the percent of the total recording time spent with ICA was calculated and compared for subjects with and without dopamine exposure using t test. The frequency of impaired epochs was compared for periods with and without dopamine exposure using χ2 testing. Further, using mixed-effect modeling to account for repeated measures and within patient clustering (random intercept), we determined the percent of impaired epochs for different levels of dopamine titration. We controlled for factors a priori that were considered to be relevant confounders—GA, day of life, MAP less than GA, presence of a PDA, and SNAPPE-II score. Other potential covariates were evaluated in a stepwise fashion and kept in the model if the addition resulted in a 10% change. In addition, we performed the analysis on both the entire cohort and just those exposed to dopamine during the monitoring period.
Results
Subject demographic and clinical outcomes
Sixty-two subjects were enrolled in the study, one subject was removed due to monitoring for <12 h. The mean birth weight (BW) of the remaining 61 subjects was 849 ± 234 g and the mean GA was 26.3 ± 1.6 weeks. Twenty-three subjects (38%) were treated with dopamine with varying dose and duration in the first 96 h of life, 20 were exposed during active monitoring—3 subjects were off dopamine prior to the start of monitoring. Demographic and clinical characteristics of those with and without dopamine exposure were compared and are outlined in Table 1. No major difference in demographics such and GA, BW, and sex was noted. The SNAPPE-II score was significantly higher in the dopamine group than the no dopamine group (63.6 ± 25.1 vs. 40.2 ± 22.2, p = 0.0004). There was a significant increase in conventional and high-frequency ventilator use, PDA, severe grade IVH, and mortality in the dopamine group. Although head ultrasound timing was variable, three subjects in the dopamine group and one subject in the no dopamine group had no or low-grade IVH that evolved to severe IVH by day of life 3.
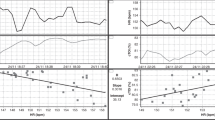
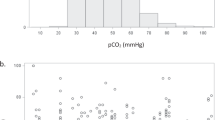
The mean duration of monitoring was 87.5 h, with a range of 14.5–96 h. The median dose of dopamine for each subject during the monitoring period ranged from 0 to 20 μg/kg/min and the maximum dosage ranged from 3 to 20 μg/kg/min (Fig. 1). The percent time with MAP below GA for dopamine titration groups 1–5, 11–15, and 16–20 μg/kg/min was significantly higher as compared to no dopamine exposure, but there was no significant difference between the dopamine exposure groups (Fig. 2). The subjects in the dopamine group spent significantly more time with ICA (23 ± 10% vs. 14 ± 7%, p = 0.0001)
Association of ICA and dopamine at the epoch level
For the overall cohort of 61 subjects, epochs without dopamine exposure (n = 22,997) were associated with ICA 14.5% of the time vs. 30.7% in epochs with dopamine exposure (n = 5100) (p < 0.0001). In evaluating only the 20 subjects with dopamine exposure during study monitoring, epochs without dopamine exposure (n = 4760) were likely to be impaired 15.5% of the time, which was similar to the overall cohort.
While epochs without dopamine exposure were dysregulated 14.5% of the time, epochs with dopamine titration of 1–5 μg/kg/min (n = 1796) were impaired 29.3% of the time, epochs with a dopamine titration of 6–10 μg/kg/min (n = 2266) were impaired 34% of the time, epochs with a dopamine titration of 11–15 μg/kg/min (n = 366) were impaired 36.6% of the time, and epochs with a dopamine titration of 16–20 μg/kg/min (n = 672) had ICA 22.5% of the time (Fig. 3).
*p < 0.0001 when compared to no dopamine, **p = 0.03 compared with no dopamine, and †p = 0.003 when compared to the 1 to 5 titration, ǂp < 0.0001 when compared to the 11 to 15 titration; all p values are based on mixed modeling adjusted for day of life, GA, MAP less than GA, PDA status, and SNAPPE-II score.
Using mixed-effect modeling, the increase in the percent of impaired epochs between times without dopamine exposure and each level of dopamine titration was significant (p ≤ 0.03). There was a significant increase in percent time with ICA in the 6–10 μg/kg/min titration group vs. the 1–5 μg/kg/min group, p = 0.003. There was a significant decrease noted in the percent of epochs with ICA from the 11–15 μg/kg/min titration to the 16–20 μg/kg/min titration, p < 0.0001. Day of life, MAP less than GA, and SNAPPE-II score significantly affected the model, while GA and PDA status had no effect (Table 2). Other potential confounders, severe grade IVH, ventilator support, gender, and so on were explored, but resulted in less than a 10% change and were not included in the model. When including only the data from the 20 subjects exposed to dopamine during the monitoring period in the model, the results were similar to the above overall cohort with the exception that SNAPPE-II score and day of life were no longer noted to be a significant confounders.
Discussion
In this study, we found that subjects exposed to dopamine spent more time with ICA, and that time with ICA peaked at a dopamine titration of 11–15 μg/kg/h. To our knowledge, this is the first study in this patient population to evaluate dopamine titrations at the time point rather than the subject level, allowing for a more robust and time synchronized assessment of the association between dopamine titration and cerebral autoregulation.
Thirty-six percent of subjects were treated with dopamine, which is similar to what has been reported in the literature.1,2,5 Infants treated with dopamine did not differ in demographic characteristics such as BW, GA, and sex from the neonates not exposed to dopamine. However, these subjects were significantly more likely to have a higher SNAPPE-II illness severity score, were exposed to high-frequency ventilation, had severe (grades 3 and 4) IVH, and have increased mortality, suggesting a higher acuity in this population. Although it is difficult to determine if the effect on autoregulation is due to dopamine therapy vs. general instability of the subject, we used methods to evaluate data at the time point level while accounting for clustering at the patient level and controlling for severity scoring, blood pressure, and other factors to minimize this influence. In addition, previous studies have also noted an association between dopamine and adverse outcomes even when controlling for patient severity factors.2,18,19 Severe grade IVH was not found to significantly affect the relationship between dopamine titration and ICA. This may be due to the possibility that IVH occurs secondary to ICA. Previously, studies have shown that ICA may precede the development of severe grade IVH;10,13 in addition, it has been shown that dopamine exposure may lead to pressure passive blood flow despite restoration of blood pressure leaving patients vulnerable to reperfusion injury.4
It is known that dopamine can cause vasodilation and/or vasoconstriction with the activation of dopaminergic receptors, β receptors, and at higher doses, α receptors. It is possible that the use of dopamine may shift the autoregulatory thresholds creating ICA at a blood pressure that would otherwise be considered normotensive as shown in the study by Munro et al.4 α-Adrenergic stimulation has been associated with a shift in the autoregulation curve to the right, requiring higher cerebral perfusion pressures to maintain stable cerebral blood flow.20 In addition, pressure-induced cerebral arterial vasoconstriction may be dampened by exposure to dopamine causing a steeper slope of the autoregulatory plateau.3,21 Wong et al.22 speculate, however, that dopamine may regulate cerebral microvascular tone improving flow-metabolism coupling through unclear mechanisms. Inconsistencies may stem from the fact that the response of the premature infant to dopamine is mediated by receptor maturational differences and downregulation, and adrenal insufficiency.23 This uncertainty and concern for changes to cerebral hemodynamics independent of blood pressure underscores the need for close monitoring and maintenance of blood pressure within a tight range during dopamine exposure.
An unexpected finding of this study is that the highest titration of dopamine (16–20 μg/kg/min) resulted in a decrease in percent time with ICA. This may be secondary to a number of factors. In general, the dose response of dopamine is stimulation of dopaminergic receptors (2–4 μg/kg/min), followed by β-receptor stimulation (5–10 μg/kg/min), and finally followed by α-receptor stimulation (11–20 μg/kg/min). In premature infants, due to GA differences in α- and β-adrenergic receptor expression, the stimulation of α-adrenergic receptors may be noted at lower titrations than β-adrenergic receptor activation,23 potentially leading to maximal α-receptor-mediated autoregulatory changes in the mid-range titration. In an animal model,24 it was found that autoregulatory capacity increased as dopamine dosage was increased above 20 μg/kg/min, but expected improvements in cerebral blood flow or oxygenation were not noted. Cerebral artery myogenic tone may also be biphasic with vasodilation at lower dopamine concentrations and vasoconstriction noted at higher concentrations.25 In addition, we speculate that the severity of illness when requiring high doses of dopamine leads to the addition of other medications, such as additional inotropes and hydrocortisone, fluid resuscitation, and blood products exposure, all of which may affect the autoregulatory threshold. In this cohort, 11 subjects were treated with these additional interventions; however, the relatively small number of infants and multiple interventions limits our ability to analyze the specific effects of interventions such as steroids on cerebral autoregulation in this study.
This study is not without limitations that should be noted. The single center design and lack of a standard approach to vasopressor initiation may limit the generalizability of this study. Some of the subjects enrolled were exposed to dopamine prior to enrollment, which did not allow for a before-during-after temporal assessment of dopamine in relation to cerebral autoregulation. In addition, although we controlled for patient illness severity and other potential confounders, we acknowledge that there may be multiple factors contributing to ICA that were not accounted for such as carbon dioxide levels, oxygen requirement, sedation exposure, treatment with steroids, and so on. Furthermore, the half-life of dopamine is not well known, although research has suggested that it may be between 2.5 and 6.9 min.26,27 Other factors that may have an effect on dopamine clearance such as infant’s GA, postnatal age, dopamine dose, and changes in infusion rate have not been well studied. Since it is possible that the half-life dopamine is shorter than each 10-min epoch, it is unclear how changes in dopamine dose before and during each epoch could affect cerebral autoregulation. More robust studies into time to steady state and clearance of dopamine need to be completed to better understand its effect on dopamine and cerebral autoregulation.
In conclusion, we found that neonates <29 weeks gestation who were exposed to dopamine during the first 96 h of life spent more time with ICA. Time periods with ICA increased with dopamine exposure in a dose-dependent manner peaking at a concentration of 11–15 μg/kg/min. This underscores the need for uniform parameters for dopamine use and close patient monitoring when exposed to avoid blood pressure fluctuations. Future large-scale studies are warranted to determine dopamine initiation and dosage parameters in order to optimize cerebral autoregulation.
References
Al-Aweel, I. et al. Variations in prevalence of hypotension, hypertension, and vasopressor use in NICUs. J. Perinatol. 21, 272–278 (2001).
St Peter, D., Gandy, C. & Hoffman, S. B. Hypotension and adverse outcomes in prematurity: comparing definitions. Neonatology 111, 228–233 (2017).
Eriksen, V. R. Rational use of dopamine in hypotensive newborns: improving our understanding of the effect on cerebral autoregulation. Dan. Med. J. 64, B5388 (2017).
Munro, M. J., Walker, A. M. & Barfield, C. P. Hypotensive extremely low birth weight infants have reduced cerebral blood flow. Pediatrics 114, 1591–1596 (2004).
Eriksen, V. R., Hahn, G. H. & Greisen, G. Dopamine therapy is associated with impaired cerebral autoregulation in preterm infants. Acta Paediatr. 103, 1221–1226 (2014).
Batton, B. et al. Early blood pressure, antihypotensive therapy and outcomes at 18–22 months’ corrected age in extremely preterm infants. Arch. Dis. Child Fetal Neonatal Ed. 101, F201–F206 (2016).
Dempsey, E. M. & Barrington, K. J. Treating hypotension in the preterm infant: when and with what: a critical and systematic review. J. Perinatol. 27, 469–478 (2007).
Vargo, L. & Seri, I. New NANN Practice Guideline: the management of hypotension in the very-low-birth-weight infant. Adv. Neonatal Care 11, 272–278 (2011).
Wong, F. Y. et al. Impaired autoregulation in preterm infants identified by using spatially resolved spectroscopy. Pediatrics 121, e604–e611 (2008).
Hoffman, S. B., Cheng, Y. J., Magder, L. S., Shet, N. & Viscardi R. M. Cerebral autoregulation in premature infants during the first 96h of life and relationship to adverse outcomes. Arch. Dis. Child Fetal Neonatal Ed. 104, F473–F479 (2019).
Levene, M. I., Fawer, C. L. & Lamont, R. F. Risk factors in the development of intraventricular haemorrhage in the preterm neonate. Arch. Dis. Child. 57, 410–417 (1982).
Soul, J. S. et al. Fluctuating pressure-passivity is common in the cerebral circulation of sick premature infants. Pediatr. Res. 61, 467–473 (2007).
Alderliesten, T. et al. Cerebral oxygenation, extraction, and autoregulation in very preterm infants who develop peri-intraventricular hemorrhage. J. Pediatr. 162, 698–704.e2 (2013).
Gilmore, M. M. et al. Relationship between cerebrovascular dysautoregulation and arterial blood pressure in the premature infant. J. Perinatol. 31, 722–729 (2011).
Alderliesten, T. et al. Hypotension in preterm neonates: low blood pressure alone does not affect neurodevelopmental outcome. J. Pediatr. 164, 986–991 (2014).
Richardson, D. K., Corcoran, J. D., Escobar, G. J. & Lee, S. K. SNAP-II and SNAPPE-II: simplified newborn illness severity and mortality risk scores. J. Pediatr. 138, 92–100 (2001).
Polavarapu, S. R., Fitzgerald, G. D., Contag, S. & Hoffman, S. B. Utility of prenatal Doppler ultrasound to predict neonatal impaired cerebral autoregulation. J. Perinatol. 38, 474–481 (2018).
Dempsey, E. M., Al Hazzani, F. & Barrington, K. J. Permissive hypotension in the extremely low birthweight infant with signs of good perfusion. Arch. Dis. Child Fetal Neonatal Ed. 94, F241–F244 (2009).
Abdul Aziz, A. N. et al. Early inotropes use is associated with higher risk of death and/or severe brain injury in extremely premature infants. J. Matern. Fetal Neonatal Med. 22, 1–8 (2019).
Paulson, O. B., Waldemar, G., Schmidt, J. F. & Strandgaard, S. Cerebral circulation under normal and pathologic conditions. Am. J. Cardiol. 63, 2C–5C (1989).
Lagaud, G., Gaudreault, N., Moore, E. D., Van Breemen, C. & Laher, I. Pressure-dependent myogenic constriction of cerebral arteries occurs independently of voltage-dependent activation. Am. J. Physiol. Heart Circ. Physiol. 283, H2187–H2195 (2002).
Wong, F. Y., Barfield, C. P., Horne, R. S. & Walker, A. M. Dopamine therapy promotes cerebral flow-metabolism coupling in preterm infants. Intens. Care Med. 35, 1777–1782 (2009).
Noori, S. & Seri, I. Neonatal blood pressure support: the use of inotropes, lusitropes, and other vasopressor agents. Clin. Perinatol. 39, 221–238 (2012).
Eriksen, V. R., Rasmussen, M. B., Hahn, G. H. & Greisen, G. Dopamine therapy does not affect cerebral autoregulation during hypotension in newborn piglets. PLoS ONE 12, e0170738 (2017).
Eriksen, V. R., Abdolalizadeh, B., Trautner, S., Greisen, G. & Sheykhzade, M. Mechanical and vasomotor properties of piglet isolated middle cerebral artery. Pharm. Res. Perspect. 5, e00279 (2017).
Rasmussen, M. B., Gramsbergen, J. B., Eriksen, V. R. & Greisen, G. Dopamine plasma clearance is increased in piglets compared to neonates during continuous dopamine infusion. Acta Paediatr. 107, 249–254 (2018).
Bhatt-Mehta, V., Nahata, M. C., McClead, R. E. & Menke, J. A. Dopamine pharmacokinetics in critically ill newborn infants. Eur. J. Clin. Pharm. 40, 593–597 (1991).
Acknowledgements
This work was funded by the Mentored Population and Clinical Research Program of the American Heart Association, Award #14CRP18140003 to S.B.H.
Author information
Authors and Affiliations
Contributions
N.S.S. was responsible for the original draft, collection, analysis and interpretation of data, and drafting and revising the manuscript. S.B.H. was responsible for the concept and design, collection, analysis and interpretation of data, and drafting and revising the manuscript. Both authors have approved the manuscript as submitted.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Solanki, N.S., Hoffman, S.B. Association between dopamine and cerebral autoregulation in preterm neonates. Pediatr Res 88, 618–622 (2020). https://doi.org/10.1038/s41390-020-0790-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-020-0790-0
This article is cited by
-
Association between early echocardiography screening of low systemic blood flow and intraventricular hemorrhage in preterm infants: a multicenter cohort study
Journal of Perinatology (2024)
-
Near-infrared spectroscopy monitoring of neonatal cerebrovascular reactivity: where are we now?
Pediatric Research (2023)
-
Blood pressure values and hypotension management in extremely preterm infants: a multi-center study
Journal of Perinatology (2022)
-
Clinical determinants of cerebrovascular reactivity in very preterm infants during the transitional period
Pediatric Research (2022)
-
Dopamine or norepinephrine for sepsis-related hypotension in preterm infants: a retrospective cohort study
European Journal of Pediatrics (2022)