Abstact
Background
Studies comparing C-RARP and RS-RARP have reported different results and the choice between the two operation methods remains controversia.
Methods
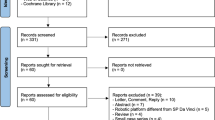
We present the meta-analysis on the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-analyses) guidelines. The meta-analysis was carried out using Review Manager 5.3 (Cochrane Collaboration, Oxford, United Kingdom) and Stata SE 14.0. The mean difference (MD) with 95% confidence intervals (CI) were used to describe the results of continuous data; odds ratio (OR) with 95% CI were used to describe dichotomous data. Statistical significance was set at P < 0.05.
Results
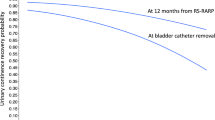
The meta-analysis revealed that RS-RARP had a statistically significant advantage in terms of continence recovery immediately after operation (OR: 0.40, 95% CI: 0.20–0.77; P = 0.007) (Fig. 2a), after 1 month (OR: 0.17, 95% CI: 0.10–0.29; P < 0.00001) (Fig. 2b), after 3 months (OR: 0.18, 95% CI: 0.09–0.36; P < 0.00001) (Fig. 2c), after 6 months (OR: 0.26, 95% CI: 0.15–0.46; P < 0.00001) (Fig. 2d) and after 12 months (OR: 0.50, 95% CI: 0.28–0.89; P = 0.02) (Fig. 2e).
Conclusions
This meta-analysis found that RS-RARP had better postoperative continence recovery than C-RARP, while sexual function recovery rates were not significantly different. There were also no significant differences in operation time, intraoperative blood loss, length of stay, positive margin rate and complications.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Siegel RL, Miller KD, Fuchs HF, Jemal A. Cancer Statistics, 2021. CA Cancer J Clin. 2021;71:7–33.
China Source: Globocan 2020. The Global Cancer Observatory, All Rights Reserved-March, 2021. Available at: https://gco.iarc.fr/today/data/factsheets/populations/160-china-fact-sheets.pdf.
Checcucci E, Amparore D, De Luca S, Autorino R, Fiori C, Porpigliaet F. Precision prostate cancer surgery: an overview of new technologies and techniques. Minerva Urol Nefrol. 2019;71:487–501.
Galfano A, Ascione A, Grimaldi S, Petralia G, Strada E, Bocciardiet AM. A new anatomic approach for robot-assisted laparoscopic prostatectomy: a feasibility study for completely intrafascial surgery. Eur Urol. 2010;58:457–61.
Galfano A, Di Trapani D, Sozzi F, Strada E, Petralia G, Bramerio M, et al. Beyond the learning curve of the Retzius-sparing approach for robot-assisted laparoscopic radical prostatectomy: oncologic and functional results of the first 200 patients with ≥ 1 year of follow-up. Eur Urol. 2013;64:974–80.
Menon M, Dalela D, Jamil M, Diaz M, Tallman C, Abdollah F, et al. Functional recovery, oncologic outcomes and postoperative complications after robot-assisted radical prostatectomy: an evidence-based analysis comparing the Retzius sparing and standard approaches. J Urol. 2018;199:1210–7.
Jiang YL, Zheng GF, Jiang ZP, Li Z, Zhou XL, Zhou J, et al. Comparison of Retzius-sparing robot-assisted laparoscopic radical prostatectomy vs standard robot-assisted radical prostatectomy: a meta-analysis. BMC Urol. 2020;20:114.
Phukan C, Mclean A, Nambiar A, Mukherjee A, Somani B, Krishnamoorthy R, et al. Retzius sparing robotic assisted radical prostatectomy vs. conventional robotic assisted radical prostatectomy: a systematic review and meta-analysis. World J Urol. 2020;38:1123–34.
Checcucci E, Veccia A, Fiori C, Amparore D, Manfredi M, Dio MD, et al. Retzius-sparing robot-assisted radical prostatectomy vs the standard approach: a systematic review and analysis of comparative outcomes. BJU Int. 2020;125:8–16.
Dirie NI, Pokhrel G, Guan W, Mumin MA, Yang J, Masau JF, et al. Is Retzius-sparing robot-assisted radical prostatectomy associated with better functional and oncological outcomes? Literature review and meta-analysis. Asian J Urol. 2019;6:174–82.
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1.
Clark HD, Wells GA, Hu€et C, McAlister FA, Salmi LR, Fergusson D, et al. Assessing the quality of randomized trials: reliability of the Jadad scale. Control Clin Trials. 1999;20:448–52.
Stang A. Critical evaluation of the Newcastle-Ottawa Scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25:603–5.
Centre for Evidence-based Medicine Oxford University: Levels of Evidence (March 2009). Updated by Jeremy Howick March 2009. Available at: https://www.cebm.ox.ac.uk/resources/levels-of-evidence/oxford-centre-for-evidence-based-medicine-levels-of-evidence-march-2009.
Abu-Ghanem Y, Dotan Z, Ramon J, Zilberman DE. Retzius space reconstruction following transperitoneal laparoscopic robot-assisted radical prostatectomy: does it have any added value? J Robot Surg. 2018;12:475–9.
Lim SK, Kim KH, Shin TY, Han WK, Chung BH, Hong SJ, et al. Retzius-sparing robot-assisted laparoscopic radical prostatectomy: combining the best of retropubic and perineal approaches. BJU Int. 2014;114:236–44.
Eden CG, Moschonas D, Soares R. Urinary continence four weeks following Retzius-sparing robotic radical prostatectomy: The UK experience. J Clin Urol. 2017;11:15–20.
Asimakopoulos AD, Topazio L, De Angelis M, Agrò EF, Pastore AL, Fuschi A, et al. Retzius-sparing versus standard robot-assisted radical prostatectomy: a prospective randomized comparison on immediate continence rates. Surg Endosc. 2019;33:2187–96.
Sayyid R, Simpson WG, Lu C, Terris MK, Klaassen Z, Madi R. Retzius-sparing robotic-assisted laparoscopic radical prostatectomy: a safe surgical technique with superior continence outcomes. J Endourol. 2017;31:1244–50.
Dalela D, Jeong W, Prasad MA, Sood A, Abdollah F, Diaz M, et al. A pragmatic randomized controlled trial examining the impact of the retzius-sparing approach on early urinary continence recovery after robot-assisted radical prostatectomy. Eur Urol. 2017;72:677–85.
Liao PC, Hung SC, Hu JC, Chiu KY. Retzius-sparing robotic-assisted radical prostatectomy facilitates early continence regardless of neurovascular bundle sparing. Anticancer Res. 2020;40:4075–80.
Egan J, Marhamati S, Carvalho FLF, Davis M, O’Neill J, Lee H, et al. Retzius-sparing robot-assisted radical prostatectomy leads to durable improvement in urinary function and quality of life versus standard robot-assisted radical prostatectomy without compromise on oncologic efficacy: single-surgeon series and step-by-step guide. Eur Urol. 2021;79:839–57. Epub 2020 Jun 11
Ota Y, Hamamoto S, Matsuyama N, Hamakawa T, Iwatsuki S, Etani T, et al. Pelvic anatomical features after Retzius-sparing robot-assisted radical prostatectomy intended for early recovery of urinary symptoms. J Endourol. 2021;35:296–304.
Lee J, Kim HY, Goh HJ, Heo JE, Almujalhem A, Alqahtani AA, et al. Retzius sparing robot-assisted radical prostatectomy conveys early regain of continence over conventional robot-assisted radical prostatectomy: a propensity score matched analysis of 1,863 patients. J Urol. 2020;203:137–44.
Umari P, Eden C, Cahill D, Rizzo M, Eden D, Sooriakumaran P. Retzius-sparing versus standard robot-assisted radical prostatectomy: a comparative prospective study of nearly 500 patients. J Urol. 2021;205:780–90.
Freire MP, Weinberg AC, Lei Y, Soukup JR, Lipsitz SR, Prasad SM, et al. Anatomic bladder neck preservation during robot-assisted laparoscopic radical prostatectomy: description of technique and outcomes. Eur Urol. 2009;56:972–80.
Lee S, Kim KB, Jo JK, Ho JN, Oh JJ, Jeong SJ, et al. Prognostic value of focal positive surgical margins after radical prostatectomy. Clin Genitourin Cancer. 2016;14:e313–9.
Kowalczyk KJ, Madi RH, Eden CG, Sooriakumaran P, Fransis K, Raskin Y, et al. Comparative outcomes of salvage Retzius-sparing versus standard robotic prostatectomy: an international, multi-surgeon series. J Urol. 2021;206:1184–91.
Madi R, Sayyid RK, Hiffa A, Thomas E, Terris MK, Klaassen Z. Early experience with salvage Retzius-sparing robotic-assisted radical prostatectomy: oncologic and functional outcomes. Urology. 2021;149:117–21.
Acknowledgements
This work was supported by grants from the Natural Science Foundation of Chongqing (cstc2019jcyj-msxmX0732), and Chongqing Science and Technology Commission (cstc2017shms-zdyf0319).
Author information
Authors and Affiliations
Contributions
JYL, JDZ and DLW contributed to the conception and design this study. ZKY, QYL, WYZ and ZZQ were responsible for the development of the methology and data interpretation. JYL, JDZ and ZKY analyzed and interpreted the data. YWX and JDZ wrote the paper. JYL, JDZ, and DLW revised the paper. JYL and JDZ contributed equally and should share first authorship. All authors read and approved the final paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Liu, J., Zhang, J., Yang, Z. et al. Comparison of Retzius-sparing and conventional robot-assisted laparoscopic radical prostatectomy regarding continence and sexual function: an updated meta-analysis. Prostate Cancer Prostatic Dis 25, 47–54 (2022). https://doi.org/10.1038/s41391-021-00459-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41391-021-00459-5
This article is cited by
-
Comparison of sexual function after robot-assisted radical prostatectomy and carbon-ion radiotherapy for Japanese prostate cancer patients using propensity score matching
BMC Cancer (2024)
-
Comparison of senhance and da vinci robotic radical prostatectomy: short-term outcomes, learning curve, and cost analysis
Prostate Cancer and Prostatic Diseases (2024)
-
Single port robot-assisted radical and simple prostatectomy: a systematic review and meta-analysis
Prostate Cancer and Prostatic Diseases (2024)
-
Preliminary comparison of the modified extraperitoneal free-PORT single incision technique and transabdominal multi-incision robot-assisted laparoscopic radical prostatectomy
Scientific Reports (2023)
-
Retzius-sparing vs. standard robot-assisted radical prostatectomy for clinically localised prostate cancer: a comparative study
Prostate Cancer and Prostatic Diseases (2023)