Abstract
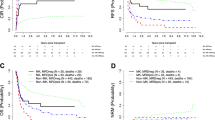
We conducted a nationwide retrospective study to evaluate the prognostic influence of +1, der(1;7)(q10;p10) [hereafter der(1;7)] and −7/del(7q) after allogeneic hematopoietic stem cell transplantation (allo-HSCT) for de novo myelodysplastic syndromes (MDS). In this database, 69 MDS patients with der(1;7), 75 with −7/del(7q), and 511 with normal karyotype (NK) underwent allo-HSCT at advanced disease status. The 3-year overall survival (OS) and cumulative incidence of relapse (CIR) were 50.4 and 19.4% for those with der(1;7), 36.2 and 38.4% for −7/del(7q), and 51.1 and 20.7% for NK, respectively. In the multivariate analysis, the presence of −7/del(7q) correlated with a significantly shorter OS (HR [95% CI], 1.38 [1.00–1.89]; P = 0.048) and higher CIR (HR, 2.11 [1.36–3.28]; P = 0.001) than those with NK. There were 23 patients with der(1;7), 29 with −7/del(7q), and 347 with NK who underwent allo-HSCT at early disease status. The 3-year OS and CIR were as follows: 47.3 and 9.5% for the der(1;7) group, 70.5 and 13.8% for −7/del(7q), and 70.9 and 5.6% for NK, respectively. No significant differences were observed in OS and CIR among three groups. The impact of the loss of chromosome 7q on OS and CIR may differ based on its type and disease status after allo-HSCT for MDS.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Tefferi A, Vardiman JW. Myelodysplastic syndromes. N Engl J Med. 2009;361:1872–85.
Greenberg P, Cox C, LeBeau MM, Fenaux P, Morel P, Sanz G, et al. International scoring system for evaluating prognosis in myelodysplastic syndromes. Blood. 1997;89:2079–88.
Greenberg PL, Tuechler H, Schanz J, Sanz G, Garcia-Manero G, Solé F, et al. Revised international prognostic scoring system for myelodysplastic syndromes. Blood. 2012;120:2454–65.
Chang C, Storer BE, Scott BL, Bryant EM, Shulman HM, Flowers ME, et al. Hematopoietic cell transplantation in patients with myelodysplastic syndrome or acute myeloid leukemia arising from myelodysplastic syndrome: similar outcomes in patients with de novo disease and disease following prior therapy or antecedent hematologic disorders. Blood. 2007;110:1379–87.
Flynn CM, Hirsch B, Defor T, Barker JN, Miller JS, Wagner JE, et al. Reduced intensity compared with high dose conditioning for allotransplantation in acute myeloid leukemia and myelodysplastic syndrome: a comparative clinical analysis. Am J Hematol. 2007;82:867–72.
Robin M, Porcher R, Zinke-Cerwenka W, van Biezen A, Volin L, Mufti G, et al. Allogeneic haematopoietic stem cell transplant in patients with lower risk myelodysplastic syndrome: a retrospective analysis on behalf of the Chronic Malignancy Working Party of the EBMT. Bone Marrow Transpl. 2017;52:209–15.
Sutton L, Chastang C, Ribaud P, Jouet JP, Kuentz M, Attal M, et al. Factors influencing outcome in de novo myelodysplastic syndromes treated by allogeneic bone marrow transplantation: a long-term study of 71 patients Société Française de Greffe de Moelle. Blood. 1996;88:358–65.
Nevill TJ, Fung HC, Shepherd JD, Horsman DE, Nantel SH, Klingemann HG, et al. Cytogenetic abnormalities in primary myelodysplastic syndrome are highly predictive of outcome after allogeneic bone marrow transplantation. Blood. 1998;92:1910–7.
Deeg HJ, Scott BL, Fang M, Shulman HM, Gyurkocza B, Myerson D, et al. Five-group cytogenetic risk classification, monosomal karyotype, and outcome after hematopoietic cell transplantation for MDS or acute leukemia evolving from MDS. Blood. 2012;120:1398–408.
Díez Campelo M, Sánchez-Barba M, de Soria VG, Martino R, Sanz G, Insunza A, et al. Results of allogeneic stem cell transplantation in the Spanish MDS registry: prognostic factors for low risk patients. Leuk Res. 2014;38:1199–206.
Shaffer L, Tommerup NE. An international System for Human Cytogenetic Nomenclature (2005). Basel: Karger; 2005.
Sanada M, Uike N, Ohyashiki K, Ozawa K, Lili W, Hangaishi A, et al. Unbalanced translocation der(1;7)(q10; p10) defines a unique clinicopathological subgroup of myeloid neoplasms. Leukemia. 2007;21:992–7.
Slovak ML, O’Donnell M, Smith DD, Gaal K. Does MDS with der(1;7)(q10;p10) constitute a distinct risk group? A retrospective single institutional analysis of clinical/pathologic features compared to -7/del(7q) MDS. Cancer Genet Cytogenet. 2009;193:78–85.
Hsiao HH, Sashida G, Ito Y, Kodama A, Fukutake K, Ohyashiki JH. et al. Additional cytogenetic changes and previous genotoxic exposure predict unfavorable prognosis in myelodysplastic syndromes and acute myeloid leukemia with der(1;7)(q10; p10). Cancer Genet Cytogenet. 2006;165:161–6.
Hussain FT, Nguyen EP, Raza S, Knudson R, Pardanani A, Hanson CA, et al. Sole abnormalities of chromosome 7 in myeloid malignancies: spectrum, histopathologic correlates, and prognostic implications. Am J Hematol. 2012;87:684–6.
Schanz J, Tüchler H, Solé F, Mallo M, Luño E, Cervera J, et al. New comprehensive cytogenetic scoring system for primary myelodysplastic syndromes (MDS) and oligoblastic acute myeloid leukemia after MDS derived from an international database merge. J Clin Oncol. 2012;30:820–9.
Atsuta Y. Introduction of transplant registry unified management program 2 (TRUMP2): scripts for TRUMP data analyses, part I (variables other than HLA-related data). Int J Hematol. 2016;103:3–10.
Kanda J. Scripts for TRUMP data analyses. Part II (HLA-related data): statistical analyses specific for hematopoietic stem cell transplantation. Int J Hematol. 2016;103:11–19.
Atsuta Y, Suzuki R, Yoshimi A, Gondo H, Tanaka J, Hiraoka A, et al. Unification of hematopoietic stem cell transplantation registries in Japan and establishment of the TRUMP System. Int J Hematol. 2007;86:269–74.
Bennett JM, Catovsky D, Daniel MT, Flandrin G, Galton DA, Gralnick HR, et al. Proposals for the classification of the myelodysplastic syndromes. Br J Haematol. 1982;51:189–99.
Giralt S, Ballen K, Rizzo D, Bacigalupo A, Horowitz M, Pasquini M, et al. Reduced-intensity conditioning regimen workshop: defining the dose spectrum. Report of a workshop convened by the center for international blood and marrow transplant research. Biol Blood Marrow Transpl. 2009;15:367–9.
Bacigalupo A, Ballen K, Rizzo D, Giralt S, Lazarus H, Ho V, et al. Defining the intensity of conditioning regimens: working definitions. Biol Bone Marrow Transpl. 2009;15:1628–33.
Atsuta Y, Suzuki R, Nagamura-Inoue T, Taniguchi S, Takahashi S, Kai S, et al. Disease-specific analyses of unrelated cord blood transplantation compared with unrelated bone marrow transplantation in adult patients with acute leukemia. Blood. 2009;113:1631–8.
Inamoto Y, Kimura F, Kanda J, Sugita J, Ikegame K, Nakasone H, et al. Comparison of graft-versus-host disease-free, relapse-free survival according to a variety of graft sources: antithymocyte globulin and single cord blood provide favorable outcomes in some subgroups. Haematologica. 2016;101:1592–602.
Saber W, Cutler CS, Nakamura R, Zhang MJ, Atallah E, Rizzo JD, et al. Impact of donor source on hematopoietic cell transplantation outcomes for patients with myelodysplastic syndromes (MDS). Blood. 2013;122:1974–82.
Aoki K, Ishikawa T, Ishiyama K, Aoki J, Itonaga H, Fukuda T, et al. Allogeneic haematopoietic cell transplantation with reduced-intensity conditioning for elderly patients with advanced myelodysplastic syndromes: a nationwide study. Br J Haematol. 2015;168:463–6.
Gooley TA, Leisenring W, Crowley J, Storer BE. Estimation of failure probabilities in the presence of competing risks: new representations of old estimators. Stat Med. 1999;18:695–706.
Fine JP, Gray RJ. A proportional hazards model for subdistribution of a competing risk. J Am Stat Assoc. 1999;94:496–509.
Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transpl. 2013;48:452–8.
Miyazaki Y, Tuechler H, Sanz G, Schanz J, Garcia-Manero G, Solé F, et al. Differing clinical features between Japanese and Caucasian patients with myelodysplastic syndromes: analysis from the international working group for prognosis of MDS. Leuk Res. 2018;73:51–7.
Zhang T, Xu Y, Pan J, Li H, Wang Q, Wen L, et al. High frequency of RUNX1 mutation in myelodysplastic syndrome patients with whole-arm translocation of der(1;7)(q10; p10). Leukemia. 2017;31:2257–60.
Damaj G, Duhamel A, Robin M, Beguin Y, Michallet M, Mohty M, et al. Impact of azacitidine before allogeneic stem-cell transplantation for myelodysplastic syndromes: a study by the Société Française de Greffe de Moelle et de Thérapie-Cellulaire and the Groupe-Francophone des Myélodysplasies. J Clin Oncol. 2012;30:4533–40.
Gerds AT, Gooley TA, Estey EH, Appelbaum FR, Deeg HJ, Scott BL. Pretransplantation therapy with azacitidine vs induction chemotherapy and posttransplantation outcome in patients with MDS. Biol Blood Marrow Transplant. 2012;18:1211–8.
Field T, Perkins J, Huang Y, Kharfan-Dabaja MA, Alsina M, Ayala E, et al. 5-Azacitidine for myelodysplasia before allogeneic hematopoietic cell transplantation. Bone Marrow Transplant. 2010;45:255–60.
Makishima H, Yoshizato T, Yoshida K, Sekeres MA, Radivoyevitch T, Suzuki H, et al. Dynamics of clonal evolution in myelodysplastic syndromes. Nat Genet. 2017;49:204–12.
Grimwade D, Freeman SD. Defining minimal residual disease in acute myeloid leukemia: which platforms are ready for “prime time. Blood. 2014;124:3345–55.
Cruz NM, Mencia-Trinchant N, Hassane DC, Guzman ML. Minimal residual disease in acute myelogenous leukemia. Int J Lab Hem. 2017;39(Suppl. 1):53–60.
Mo XD, Qin YZ, Zhang XH, Xu LP, Wang Y, Yan CH, et al. Minimal residual disease monitoring and preemptive immunotherapy in myelodysplastic syndrome after allogeneic hematopoietic stem cell transplantation. Ann Hematol. 2016;95:1233–40.
Schroeder T, Rautenberg C, Haas R, Germing U, Kobbe G. Hypomethylating agents for treatment and prevention of relapse after allogeneic blood stem cell transplantation. Int J Hematol. 2018;107:138–50.
El-Cheikh J, Massoud R, Fares E, Kreidieh N, Mahfouz R, Charafeddine M, et al. Low-dose 5-azacytidine as preventive therapy for relapse of AML and MDS following allogeneic HCT. Bone Marrow Transplant. 2017;52:918–21.
Craddock C, Jilani N, Siddique S, Yap C, Khan J, Nagra S, et al. Tolerability and clinical activity of post-transplantation azacitidine in patients allografted for acute myeloid leukemia treated on the RICAZA trial. Biol Blood Marrow Transplant. 2016;22:385–90.
de Lima M, Giralt S, Thall PF, de Padua Silva L, Jones RB, Komanduri K, et al. Maintenance therapy with low-dose azacitidine after allogeneic hematopoietic stem cell transplantation for recurrent acute myelogenous leukemia or myelodysplastic syndrome: a dose and schedule finding study. Cancer . 2010;116:5420–31.
Han S, Kim YJ, Lee J, Jeon S, Hong T, Park GJ, et al. Model-based adaptive phase I trial design of post-transplant decitabine maintenance in myelodysplastic syndrome. J Hematol Oncol. 2015;8:118.
Oshikawa G, Kakihana K, Saito M, Aoki J, Najima Y, Kobayashi T, et al. Post-transplant maintenance therapy with azacitidine and gemtuzumab ozogamicin for high-risk acute myeloid leukaemia. Br J Haematol. 2015;169:756–9.
Pusic I, Choi J, Fiala MA, Gao F, Holt M, Cashen AF, et al. Maintenance therapy with decitabine after allogeneic stem cell transplantation for acute myelogenous leukemia and myelodysplastic syndrome. Biol Blood Marrow Transpl. 2015;21:1761–9.
McClune BL, Weisdorf DJ, Pedersen TL, Tunes da Silva G, Tallman MS, Sierra J, et al. Effect of age on outcome of reduced-intensity hematopoietic cell transplantation for older patients with acute myeloid leukemia in first complete remission or with myelodysplastic syndrome. J Clin Oncol. 2010;28:1878–87.
Scott BL, Pasquini MC, Logan BR, Wu J, Devine SM, Porter DL, et al. myeloablative versus reduced-intensity hematopoietic cell transplantation for acute myeloid leukemia and myelodysplastic syndromes. J Clin Oncol. 2017;35:1154–61.
Choi EJ, Lee JH, Lee JH, Kim DY, Park HS, Seol M, et al. Non-myeloablative conditioning for lower-risk myelodysplastic syndrome with bone marrow blasts less than 5%—a feasibility study. Ann Hematol. 2016;95:1151–61.
Lee SE, Kim YJ, Yahng SA, Cho BS, Eom KS, Lee S, et al. Survival benefits from reduced-intensity conditioning in allogeneic stem cell transplantation for young lower-risk MDS patients without significant comorbidities. Eur J Haematol. 2011;87:510–20.
de Lima M, Anagnostopoulos A, Munsell M, Shahjahan M, Ueno N, Ippoliti C, et al. Nonablative versus reduced-intensity conditioning regimens in the treatment of acute myeloid leukemia and high-risk myelodysplastic syndrome: dose is relevant for long-term disease control after allogeneic hematopoietic stem cell transplantation. Blood. 2004;104:865–72.
Christiansen DH, Andersen MK, Pedersen-Bjergaard J. Mutations of AML1 are common in therapy-related myelodysplasia following therapy with alkylating agents and are significantly associated with deletion or loss of chromosome arm 7q and with subsequent leukemic transformation. Blood. 2004;104:1474–81.
Inaba T, Honda H, Matsui H. The enigma of monosomy 7. Blood. 2018;131:2891–8.
Yoshizato T, Nannya Y, Atsuta Y, Shiozawa Y, Iijima-Yamashita Y, Yoshida K, et al. Genetic abnormalities in myelodysplasia and secondary acute myeloid leukemia: impact on outcome of stem cell transplantation. Blood. 2017;129:2347–58.
Bejar R, Stevenson KE, Caughey B, Lindsley RC, Mar BG, Stojanov P, et al. Somatic mutations predict poor outcome in patients with myelodysplastic syndrome after hematopoietic stem-cell transplantation. J Clin Oncol. 2014;32:2691–8.
Della Porta MG, Gallì A, Bacigalupo A, Zibellini S, Bernardi M, Rizzo E, et al. Clinical effects of driver somatic mutations on the outcomes of patients with myelodysplastic syndromes treated with allogeneic hematopoietic stem-cell transplantation. J Clin Oncol. 2016;34:3627–37.
Duncavage EJ, Jacoby MA, Chang GS, Miller CA, Edwin N, Shao J, et al. Mutation clearance after transplantation for myelodysplastic syndrome. N Engl J Med. 2018;379:1028–41.
Bacher U, Shumilov E, Flach J, Porret N, Joncourt R, Wiedemann G, et al. Challenges in the introduction of next-generation sequencing (NGS) for diagnostics of myeloid malignancies into clinical routine use. Blood. Cancer J. 2018;8:113.
Lee JH, Lee JH, Lim SN, Kim DY, Kim SH, Lee YS, et al. Allogeneic hematopoietic cell transplantation for myelodysplastic syndrome: prognostic significance of pre-transplant IPSS score and comorbidity. Bone Marrow Transpl. 2010;45:450–7.
Nevill TJ, Shepherd JD, Sutherland HJ, Abou Mourad YR, Lavoie JC, Barnett MJ, et al. IPSS poor-risk karyotype as a predictor of outcome for patients with myelodysplastic syndrome following myeloablative stem cell transplantation. Biol Blood Marrow Transpl. 2009;15:205–13.
Della Porta MG, Alessandrino EP, Bacigalupo A, van Lint MT, Malcovati L, Pascutto C, et al. Predictive factors for the outcome of allogeneic transplantation in patients with MDS stratified according to the revised IPSS-R. Blood. 2014;123:2333–42.
Acknowledgements
This work was supported in part by the Practical Research Project for Allergic Diseases and Immunology (Research Technology of Medical Transplantation) from the Japan Agency for Medical Research and Development, AMED. The authors would like to thank all the physicians and data managers at the various institutes who contributed valuable data on transplantation to the Japan Society for Hematopoietic Cell Transplantation (JSHCT) and all the members of the data management committees of JSHCT; a complete membership list of the “Adult Myelodysplastic Syndrome Working Group of the JSHCT” appears in the “Appendix”.
Author information
Authors and Affiliations
Contributions
HI and YM designed the research, organized the project, analyzed the data, and wrote the manuscript. HI, KA, JA, TI, KI, and YM collected data from TRUMP. HI, KA, JA, TI, KI, NU, TF, YO, SO, NU, TE, KI, YO, MT, TI, YA, and YM interpreted data and reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors state that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
The following institutions and hematologists contributed to this study: Nagasaki University: Dr. H. Itonaga and Dr. Y. Miyazaki; Kyoto University: Dr. A. Takeda and Dr. K. Aoki; Kanagawa Cancer Center: Dr. J. Aoki, Dr. M. Tanaka, and Dr. T Takahana; Kanazawa University Hospital: Dr. K. Ishiyama; Kobe City Medical General Hospital: Dr. Y. Shimomura and Dr. T. Ishikawa; Keio University School of Medicine: Drs. J. Kato and S. Okamoto; Japanese Red Cross Nagoya First Hospital: Dr. Y. Ozawa; Tokyo Metropolitan Cancer and Infectious Disease Centre Komagome Hospital: Drs. K. Kakizoe and N. Doki; JA Aichi Konan Kosei Hospital: Dr. A. Kohno; Toranomon Hospital: Dr. S. Takagi; Aichi Medical University: Dr. A. Takami; Hyogo College of Medicine: Dr. H. Tamaki; Akita University Hospital: Dr. M. Hirokawa; Mishuku Hospital: Dr. K. Masuoka; Niigata University: Dr. M. Masuko; Kinki University: Dr. K. Ashizawa and Dr. T. Ashida; NTT Medical Center Tokyo: Dr. R. Kida and Dr. K. Usuki; Hamanomachi Hospital: Dr. T. Eto; Sapporo Hokuyu Hospital: Dr. K. Minauchi and Dr. S. Ohta; Tohoku University Hospital: Dr. Y. Onishi; Kanazawa University Graduate School of Medical Sciences: Dr. S. Nakao; Shizuoka Cancer Center: Dr. T. Enami and Dr. T. Ikeda; Kansai Medical University Hirakata Hospital: Dr. K. Ishii; Tokyo Metropolitan Geriatric Hospital: Dr. S. Kobayashi; Tokai University School of Medicine: Dr. S. Machida; Osaka City University: Dr. H. Koh; National Cancer Center Hospital: Dr. T. Suzuki; The University of Tokyo: Dr. T. Konuma; Nagoya University Graduate School of Medicine: Dr. K. Miyao and Dr. T. Morishita; Tokyo Women’s Medical University: Dr. K. Yoshinaga; Ishikawa Prefectural Central Hospital: Dr. Y. Mizumaki and Dr. C. Sugimori; Kokura Memorial Hospital: Dr. A. Yonezawa; Okawama University Hospital: Dr S. Fujii.
Supplementary information
Rights and permissions
About this article
Cite this article
Itonaga, H., Ishiyama, K., Aoki, K. et al. Clinical impact of the loss of chromosome 7q on outcomes of patients with myelodysplastic syndromes treated with allogeneic hematopoietic stem cell transplantation. Bone Marrow Transplant 54, 1471–1481 (2019). https://doi.org/10.1038/s41409-019-0469-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-019-0469-5
This article is cited by
-
Allogeneic transplantation of bone marrow versus peripheral blood stem cells from HLA-identical relatives in patients with myelodysplastic syndromes and oligoblastic acute myeloid leukemia: a propensity score analysis of a nationwide database
Annals of Hematology (2023)
-
Increased opportunity for prolonged survival after allogeneic hematopoietic stem cell transplantation in patients aged 60–69 years with myelodysplastic syndrome
Annals of Hematology (2019)