Abstract
A previous meta-analysis reported no benefit for silicone intubation during dacryocystorhinostomy. However, the power of this meta-analysis was 0.274. Therefore, the benefit of silicone intubation remains controversial. We undertook a cumulative meta-analysis to evaluate the success rate of dacryocystorhinostomy (DCR) with and without the use of a stent. Pubmed, EMBASE and the Cochrane Library were searched. Statistical power and trial sequential analyses were performed according to the result of the meta-analysis. Twelve randomized controlled trials involving 969 cases met the inclusion criteria. The success rates of DCR with and without intubation were significantly different (p = 0.006). The success rates of external DCR (EX-DCR) with and without intubation were also significantly different based on subgroup analysis (p = 0.002). The cumulative z-curves crossed the O’Brian-Fleming boundaries. There were no significant differences in the success rate in the endonasal endoscopic DCR (EN-DCR) subgroup or the occurrence of postoperative complications between the two groups based on the meta-analysis, and the z-curve did not intersect any trial sequential analysis boundaries. DCR with intubation achieved better results than DCR without intubation, especially in the EX-DCR subgroup. Differences in the success rate in the EN-DCR subgroup and postoperative complications between the two groups were underpowered to reach a conclusion.
Similar content being viewed by others
Introduction
Dacryocystorhinostomy (DCR) is the most popular operation for treating nasolacrimal duct obstruction or chronic dacryostenosis1. DCR is a surgical procedure to create drainage between the lacrimal sac and the nasal cavity2. DCR procedures include standard external DCR (EX-DCR), non-laser endonasal endoscopic DCR (EN-DCR), and endonasal endoscopic laser DCR (LA-DCR). Beginning in the 1970s, ophthalmologists began to favour DCR with silicone intubation over DCR without intubation3. They advocated its use and reported an increased postoperative patency rate because of maintenance of the opening of the ostium4. However, other studies reported a higher failure rate when using a silicone stent because of granulomatous inflammation5. The role of silicone intubation during DCR surgery has been discussed several times in the recent literature, with conflicting opinions6, 7. The aim of this study was to evaluate the success rate with and without the use of a stent during DCR and to compare the results with those of previously published studies. We hope the results of this study will give clinicians a more definitive set of guidelines and indications for tube use.
Materials and Methods
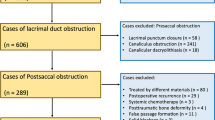
The following electronic databases were searched from January 1, 1990 to June 1, 2016: PubMed, EMBASE, the Cochrane Controlled Trials Register, Ovid, ScienceDirect, NGC, and EBSCO. We developed a search strategy including the following terms: “dacryocystorhinostomy”, “silicone intubation”, “stent”, “nasolacrimal duct obstruction” and “dacryocystitis”. The literature search only included English-language articles. The titles of all articles were read, and the relevant abstracts were evaluated. The full articles were retrieved if the title, abstract, or both of a study seemed to meet the objective of this review. The reference lists of original reports and review articles retrieved through the search were reviewed for additional studies not yet included in the computerized databases (Fig. 1).
Study inclusion criteria: 1. Design: Only randomized controlled trials were included. 2. Population: Adult patients who were confirmed to have nasolacrimal duct obstruction or chronic dacryocystitis based on the symptoms of epiphora and the results of lacrimal irrigation. 3. Intervention: DCR with silicone intubation versus DCR without silicone intubation were compared. DCR techniques could include EX-DCR, LA-DCR or EN-DCR. 4. Follow-up duration: At least 6 months of follow-up was required. 5. Outcome measures: The success rates of each group based on subjective or objective assessments were included as outcomes. Patients who had lacrimal sac tumours, canalicular obstruction, a history of lacrimal surgery and traumatic injury to the ocular or nasal regions were excluded. Studies were further excluded if the study cohorts included paediatric cases.
Data extraction was performed according to a customized protocol. The following categories of information were extracted: study characteristics (author, year and country of publication), patient characteristics (mean age, gender, number of participants and withdrawals) and intervention characteristics (type of surgical intervention, follow up duration, extubation time, outcomes and complications).
The risk of bias in each included study was assessed according to the Cochrane Collaboration tool for assessing the risk of bias8, which is structured into seven domains: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting and other sources of bias.
Document screening, information extraction and qualitative assessment were performed by two reviewers independently. Any disagreement was resolved by discussion or consensus involving a third reviewer when necessary.
Statistical Analysis
The statistical analysis was performed using the RevMan software package (version 5.3, The Cochrane Collaboration, London, England). A pooled risk ratio (RR) was calculated with a 95% confidence interval (CI). Statistical heterogeneity was assessed via I 2 statistics. The fixed-effects models were accepted if I 2 < 50%. Otherwise, random-effects models were used9. Subgroup analysis was performed based on the type of DCR technique. A p-value < 0.05 was considered statistically significant.
Cumulative meta-analysis models were performed using the Stata software package (version 11.0, Stata Corporation, College Station, TX, USA). Publication bias was assessed via Egger et al. regression asymmetry tests10 and Begg and Mazumdar’s adjusted rank correlation tests11. A funnel plot was also constructed to display publication bias. The statistical power was calculated using the Power and Precision software package (version 4, Biostat, Inc., Chicago, Illinois, USA), when negative results were obtained12.
The trial sequential analyses were performed using the TSA software package (version 0.9 beta, The Copenhagen Trial Unit, Copenhagen, Denmark), based on estimated information size with a risk of type I error of a = 0.05 and a risk of type II error of β = 20%13.
Results
A total of 412 records were identified, and 12 RCTs14,15,16,17,18,19,20,21,22,23,24,25 were included in the quantitative analysis. The studies included a total of 969 cases. Of these, 494 cases had undergone DCR with silicone intubation, and 475 cases had undergone DCR without silicone intubation. (Table 1). Each included study was assessed using the Cochrane Collaboration’s tool for assessing the risk of bias (Fig. 2).
All studies provided data regarding the success rate of both groups. The heterogeneity test indicated no significant heterogeneity (I 2 = 27%, p = 0.18), and a fixed-effects model was adopted. The forest plot revealed that DCR with silicone intubation had a much higher rate of success than DCR without silicone intubation. The difference was statistically significant (RR, 1.06; 95% CI [1.02–1.11], p = 0.006). The statistical power was 0.788 (Fig. 3).
We divided the studies into 3 groups depending on surgery type (EX-DCR, EN-DCR or LA-DCR) to perform subgroup analysis. The forest plot revealed that there was a significant difference in the EX-DCR group (p = 0.002) but no significant difference in the EN-DCR group (p = 0.63). The powers of the EX-DCR and EN-DCR subgroup analyses were 87.2% and 7.9%, respectively (Fig. 4). Only one study included in the LA-DCR group and reported that there was no significant difference between the success rates of the two groups (p = 0.769).
Of 12 RCTs, 9 studies14,15,16, 18, 20,21,22, 24, 25 reported postoperative complications, including granulation tissue formation, adhesion, infection, haemorrhage and other complications that were considered to be related to the silicone tube, such as punctual/canalicular laceration, tube displacement or loss and conjunctival irritation. Granulation tissue formation after DCR was only reported in 3 studies20, 22, 24, infection was reported in 2 studies14, 20, and adhesion was reported in 3 studies20, 24, 25. The forest plots all revealed no significant differences between DCR with and without silicone intubation (Figs 5,6 and 7). The powers of the three studies were 9.3%, 13.5% and 18.1%, respectively.
Sequential cumulative meta-analysed results for each year were calculated from 2005, and the overall effect of success rate began to have statistical significance in 2013. Figure 8 shows the results of the updated cumulative meta-analysis in chronological order.
In Figs 9 and 10, the cumulative z-score reached significance by crossing both the conventional boundaries and the O’Brian-Fleming boundaries, thus demonstrating the significant benefit of silicone intubation during EX-DCR. In the EN-DCR subgroup, the z-curve did not intersect any TSA boundaries, which indicates that the meta-analysis is underpowered to reach a conclusion (Fig. 11).
The publication bias of the study is revealed by the funnel plot (Fig. 12). There was no evidence of publication bias (Begg’s test, p = 0.891; Egger’s test, p = 0.988).
Discussion
In 2011, a previous meta-analysis6 regarding DCR with and without a silicone tube for the treatment of nasolacrimal duct obstruction reported equal success rates between DCR with and without intubation. The meta-analysis indicated that no benefit was found for silicone stent intubation in primary DCR. However, a growing number of prospective comparative studies published from 2010 onward have reported that the use of silicone intubation in primary DCR increased the success rate of DCR without intubation, although some increases had no statistical significance28, 29. Rather and Singh21 also conducted a large, randomized controlled trial and demonstrated that silicone intubation in DCR prevented the closure of the ostium, thereby enhancing the success rate of DCR. The previous meta-analysis only included 4 RCTs, and for the given effect size (population proportions 0.892 versus 0.943), sample size (111 and 105) and alpha (0.05, 2-tailed), the power of the meta-analysis was 0.274. The role of silicone intubation during DCR surgery was still undetermined. Therefore, we performed a cumulative meta-analysis to evaluate the success rate with and without the use of a stent in DCR and to compare the results with those of previously published studies.
This cumulative meta-analysis suggested that compared with DCR without intubation, DCR with intubation had a much better rate of success after surgery, especially in the EX-DCR subgroup. The difference was statistically significant [RR, 1.06; 95%CI (1.02–1.11), p = 0.006]. The conclusion was completely opposite that of the previous meta-analysis. The previous meta-analysis included fewer studies and had low statistical power, which may explain the different results. When a negative result is obtained, it is important to consider the power of the study30. Otherwise, investigators can make a type II error, and treatments that may be of benefit may be discarded.
Meta-analysis is a statistical methodology that combines the results of several independent studies considered by the analyst to be ‘combinable’. It acts to increase the sample size, reduce the random error and enhance the statistical power when the studies included are underpowered31. Of the 12 RCTs included in this cumulative meta-analysis, the results of 10 of them were negative. In this article, the results of the cumulative meta-analysis and the EX-DCR subgroup analysis were positive, and the statistical powers of the two analyses were 78.4% and 87.2%, respectively. Because cumulative meta-analyses are prone to produce spurious p < 0.05 because of the repeated testing of significance as trial data accumulate, trial sequential analysis should establish when there is firm evidence in a cumulative meta-analysis. The cumulative z-score crossed the O’Brian-Fleming boundaries, and the accrued information size in the EX-DCR subgroup was more than the required information size, which suggested preliminary termination of a clinical trial of the same type. Therefore, this study provided more convincing evidence of the significant benefits of silicone intubation during EX-DCR. In the EN-DCR subgroup, the statistical power of the subgroup analysis was 7.9%, and the z-curve did not intersect any TSA boundaries, which indicates that the meta-analysis was underpowered to reach a conclusion. To definitively determine whether silicone intubation during EN-DCR is beneficial, a large sample or multicentre, randomized, prospective intervention trial is required. The sample size based on trial sequential analysis should be 3784 patients (1892 in each group).
The common complications after surgery were intranasal tissue granulation, adhesion, infection, haemorrhage and other complications that were considered to be related with silicone tube, including punctual/canalicular laceration, tube displacement or loss and conjunctival irritation32. The opinion that the silicone tube itself may stimulate tissue granulation was controversial. Unlu et al.33 suggested that silicone intubation as a foreign inorganic material may predispose the patient to granulation formation with subsequent rhinostomy closure. The ostial size reduction has been reported by Longari et al. in higher percentage in the stent group, mainly due to peristomal granuloma, scar tissue formation, and turbinoseptal synaechia34. Owing to data restrictions regarding postoperative complications, which many included trials did not provide, this study only analysed complications quantitatively in term of tissue granulation hyperplasia, infection and adhesion. Postoperative complications such as canalicular laceration and tube displacement or loss could not be incorporated into the meta-analysis. The results of the meta-analysis indicated that the use of a silicone tube did not increase the risk of tissue granulation, infection or adhesion. However, the statistical powers for each complication were, respectively, 9.3%, 13.5% and 18.1%. Therefore, the conclusion that the silicone tube itself may stimulate tissue granulation is still unconfirmed.
In conclusion, this cumulative meta-analysis revealed that the success rate of DCR with silicone tubing was significantly better than that of DCR without silicone tubing, especially in the EX-DCR subgroup. The results indicated that silicone intubation was beneficial in treating nasolacrimal duct obstruction during external DCR. Although the meta-analyses revealed no significant differences in terms of success rates or postoperative complications, such as tissue granulation, infection and adhesion, in the EN-DCR subgroup, the meta-analysis was underpowered to reach a conclusion based on statistical power analysis and trail sequential analysis.
Limitations of this study
This meta-analysis only included twelve RCTs, we did not obtain unpublished study data, and the sample size was small. The type of DCR, the timing of tube removal, the follow-up time and the measurement indicators were not totally consistent across the RCTs. Only a few RCTs had recorded details of postoperative complications. These factors may cause bias. Because of the existing restrictions, it is suggested that a multicentre, large-sample, randomized controlled clinical study be performed to provide more convincing evidence of the efficacy of silicone intubation in EN-DCR for PNLDO.
Change history
12 December 2018
A correction to this article has been published and is linked from the HTML and PDF versions of this paper. The error has not been fixed in the paper.
References
Yakopson, V. S., Flanagan, J. C., Ahn, D. & Luo, B. P. Dacryocystorhinostomy: History, evolution and future directions. Saudi J. Ophthalmol. 25, 37–49, doi:10.1016/j.sjopt.2010.10.012 (2011).
Vazquez, A., Blake, D. M., Langer, P. & Eloy, J. A. Transillumination-guided endoscopic endonasal dacryocystorhinostomy: approach to revision cases and challenging anatomy. Otolaryngol. Head Neck Surg. 149, 265–266, doi:10.1177/0194599813496044a373 (2013).
Soll, D. B. Silicone intubation: an alternative to dacryocystorhinostomy. Ophthalmology 85, 1259–1266, doi:10.1016/S0161-6420(78)35558-5 (1978).
Griffiths, J. D. Nasal catheter use in dacryocystorhinostomy. Ophthal. Plast. Reconstr. Surg. 7, 177–186, doi:10.1097/00002341-199109000-00005 (1991).
Buttanri, I. B. & Serin, D. Silicone intubation indications in external dacryocystorhinostomy. Med. Hypothesis Discov. Innov. Ophthalmol. 3, 101–102 (2014).
Feng, Y. F., Cai, J. Q., Zhang, J. Y. & Han, X. H. A meta-analysis of primary dacryocystorhinostomy with and without silicone intubation. Can. J. Ophthalmol. 46, 521–527, doi:10.1016/j.jcjo.2011.09.008 (2011).
Gu, Z. & Cao, Z. Silicone intubation and endoscopic dacryocystorhinostomy: a meta-analysis. J. Otolaryngol. Head Neck Surg. 39, 710–713 (2010).
Higgins, J. P. T. et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343, d5928–d5928, doi:10.1136/bmj.d5928 (2011).
Sidik, K. & Jonkman, J. N. Simple heterogeneity variance estimation for meta-analysis. J. R. Stat. Soc. Ser. C Appl. Stat. 54, 367–384, doi:10.1111/rssc.2005.54.issue-2 (2005).
Egger, M., Davey Smith, G., Schneider, M. & Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 315, 629–634, doi:10.1136/bmj.315.7109.629 (1997).
Begg, C. B. & Mazumdar, M. Operating characteristics of a rank correlation test for publication bias. Biometrics 50, 1088–1101, doi:10.2307/2533446 (1994).
Borenstein, M., Rothstein, H. & Cohen, J. Power and precision: a computer program for statistical power analysis and confidence intervals. Pers. Psychol. 55, 1077–1080 (1997).
Wetterslev, J., Thorlund, K. J., Brok, J. & Gluud, C. Trial sequential analysis may establish when firm evidence is reached in cumulative meta-analysis. J. Clin. Epidemiol. 61, 64–75, doi:10.1016/j.jclinepi.2007.03.013 (2008).
Zaman, M., Babar, T. F. & Abdullah, A. Prospective randomized comparison of dacryocystorhinostomy (DCR) with and without intubation. Pak. J. Med. Res. 44, 75–78 (2005).
Smirnov, G., Tuomilehto, H., Teräsvirta, M., Nuutinen, J. & Seppä, J. Silicone tubing is not necessary after primary endoscopic dacryocystorhinostomy: a prospective randomized study. Am. J. Rhinol. 22, 214–217, doi:10.2500/ajr.2008.22.3132 (2008).
Unlu, H. H., Gunhan, K., Baser, E. F. & Songu, M. Long-term results in endoscopic dacryocystorhinostomy: is intubation really required? Otolaryngol. Head Neck Surg. 140, 589–595, doi:10.1016/j.otohns.2008.12.056 (2009).
Saiju, R., Morse, L. J., Weinberg, D., Shrestha, M. K. & Ruit, S. Prospective randomised comparison of external dacryocystorhinostomy with and without silicone intubation. Br. J. Ophthalmol. 93, 1220–1222, doi:10.1136/bjo.2008.147819 (2009).
Elmorsy, S. & Fayek, H. M. Rubber tube versus silicone tube at the osteotomy site in external dacryocystorhinostomy. Orbit 29, 76–82, doi:10.3109/01676830903294891 (2010).
Al-Qahtani, A. S. Primary endoscopic dacryocystorhinostomy with or without silicone tubing: a prospective randomized study. Am. J. Rhinol. Allergy 26, 332–334, doi:10.2500/ajra.2012.26.3789 (2012).
Dogan, R., Meric, A., Ozsütcü, M. & Yenigun, A. Diode laser-assisted endoscopic dacryocystorhinostomy: a comparison of three different combinations of adjunctive procedures. Eur Arch Otorhinolaryngol 270, 2255–2261, doi:10.1007/s00405-013-2351-1 (2013).
Rather, S. & Singh, T. External dacryocystorhinostomy with & without silicon tube intubation in chronic dacryocystitis with nasolacrimal duct block. JK Sci. 15, 24–27 (2013).
Chong, K. K. et al. Randomized trial on silicone intubation in endoscopic mechanical dacryocystorhinostomy (SEND) for primary nasolacrimal duct obstruction. Ophthalmology 120, 2139–2145, doi:10.1016/j.ophtha.2013.02.036 (2013).
Afzal, M. M., Mehmood, A., Maqbool, R., Malik, I. Q. & Rehman, A. To compare the success rate of external dacryocystorhinostomy with and without silicon intubation in patients of nasolacrimal duct obstruction. Pak. J. Med. Health Sci. 8, 53–55 (2014).
Shashidhar, K., Nagalotimath, U. & Dixit, D. Endoscopic dacryocystorhinostomy with and without silicone stenting: a comparative study. Al Ameen J. Med. Sci. 7, 244–247 (2014).
Reddy, Y. J., Reddy, Y. M., Kiran, M., Reddy, Y. G. & Kumar, S. A comparative study of outcomes of dacryocystorhinostomy with and without silicone stenting. IOSR J. Dent. Med. Sci. 14, 82–85 (2015).
Kakkar, V., Chugh, J. P. & Sachdeva, S. Endoscopic dacryocystorhinostomy with and without silicone stent: a comparative study. Internet J. Orl. 9, 1–5 (2009).
Abdelshafy, I. A. Trans nasal powered endoscopic dacryocystorhinostomy with and without stenting. J. Am. Sci. 9, 448–451 (2013).
Nabie, R. et al. The effect of bicanalicular intubation on success rate of primary acquired nasolacrimal duct obstruction. Bina J. Ophthalmol. 19, 265–270 (2014).
Yildirim, Y. et al. Comparison of transcanalicular multidiode laser dacryocystorhinostomy with and without silicon tube intubation. J. Ophthalmol. 2016, 6719529–5, doi:10.1155/2016/6719529 (2016).
Dulku, S., Murray, A. & Durrani, O. M. Prospective randomised comparison of external dacryocystorhinostomy with and without silicone intubation: considerations of power. Br. J. Ophthalmol. 95, 151–152, doi:10.1136/bjo.2009.173286 (2011).
Cohn, L. D. & Becker, B. J. How meta-analysis increases statistical power. Psychol. Methods 8, 243–253, doi:10.1037/1082-989X.8.3.243 (2003).
Allen, K. & Berlin, A. J. Dacryocystorhinostomy failure: association with nasolacrimal silicone intubation. Ophthal. Surg. 20, 486–489 (1989).
Unlu, H. H., Toprak, B., Aslan, A. & Guler, C. Comparison of surgical outcomes in primary endoscopic dacryocystorhinostomy with and without silicone intubation. Ann. Otol. Rhinol. Laryngol. 111, 704–709, doi:10.1177/000348940211100809 (2002).
Longari, F. et al. Endoscopic dacryocystorhinostomy with and without silicone intubation: 4 years retrospective study. Eur. Arch. Otorhinolaryngol. 273, 2079–2084, doi:10.1007/s00405-015-3876-2 (2016).
Author information
Authors and Affiliations
Contributions
Chuanqi Xie and Lingling Zhang designed the study, wrote the manuscript and approved the final version. Chuanqi Xie, Lingling Zhang, Hong Ma and Shuzhen Li conducted the literature search, identified the studies for exclusion and inclusion, extracted data from the retrieved studies and performed the meta-analysis. Yang Liu was responsible for the language revision. All authors reviewed and finally approved the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Xie, C., Zhang, L., Liu, Y. et al. Comparing the Success Rate of Dacryocystorhinostomy With and Without Silicone Intubation: A Trial Sequential Analysis of Randomized Control Trials. Sci Rep 7, 1936 (2017). https://doi.org/10.1038/s41598-017-02070-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-02070-y
This article is cited by
-
Success rate of external, endonasal, and transcanalicular laser DCR with or without silicone stent intubation for NLD obstruction: a network meta-analysis of randomized controlled trials
Graefe's Archive for Clinical and Experimental Ophthalmology (2023)
-
Endoscopic dacryocystorhinostomy for refractory nasolacrimal duct obstruction with a small lacrimal sac (≤ 5 mm in diameter)
European Archives of Oto-Rhino-Laryngology (2022)
-
Longitudinal randomized study to evaluate the long-term outcome of endoscopic primary dacryocystorhinostomy with or without silicone tube
European Archives of Oto-Rhino-Laryngology (2022)
-
Species-specific characteristics of the biofilm generated in silicone tube: an in vitro study
BMC Ophthalmology (2018)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.