Abstract
Current WHO guidelines recommend initiating ART regardless of CD4+ cell count. In response, we conducted an observational cohort study to assess the effects of pre-ART CD4+ cell count levels on death, attrition, and death or attrition in HIV treated patients. This large HIV treatment cohort study (n = 49,155) from 2010 to 2015 was conducted in Guangxi, China. We used a Cox regression model to analyze associations between pre-ART CD4+ cell counts and death, attrition, and death or attrition. The average mortality and ART attrition rates among all treated patients were 2.63 deaths and 5.32 attritions per 100 person-years, respectively. Compared to HIV patients with <350 CD4+ cells/mm3 at ART initiation, HIV patients with >500 CD4+ cells/mm3 at ART initiation had a significantly lower mortality rate (Adjusted hazard ratio: 0.56, 95% CI: 0.40–0.79), but significantly higher ART attrition rate (AHR: 1.17, 95% CI: 1.03–1.33). Results from this study suggest that HIV patients with high CD4+ cell counts at the time of ART initiation may be at greater risk of treatment attrition. To further reduce ART attrition, it is imperative that patient education and healthcare provider training on ART adherence be enhanced and account for CD4 levels at ART initiation.
Similar content being viewed by others
Introduction
Since its development in 1996, highly active antiretroviral therapy (HAART) has been shown to rejuvenate the immune system of HIV infected individuals, prevent onset of opportunistic infections that often lead to death among HIV patients, and generally improve the quality of life among HIV infected persons worldwide1,2,3,4. Moreover, successful ART has had significant effects on viral suppression and reducing transmission from partner to partner. Recently, a randomized clinical trial and a several observational studies showed that ART can significantly reduce transmissions in serodiscordant heterosexual couples5,6,7,8,9,10. Due to its impact on immunocompetence and HIV transmission, HAART has led to significant declines in AIDS-related morbidity and premature mortality.
Research in recent years has indicated that early initiation of ART can delay time to AIDS-related events and decrease incidences of morbidity and mortality, and high current CD4+ T cell count can be associated with suboptimal adherence to ART11,12,13,14,15,16,17. Given the clinical benefits and significant reductions in HIV transmission associated with early ART initiation, the World Health Organization (WHO) revised their ART guidelines in 2010 by increasing the threshold for ART eligibility in developed countries from <200 CD4+ cells/ mm3 to <350 CD4+ cells/ mm3 18, 19. In an effort to end the HIV epidemic by 2030, ART guidelines were again revised in 2015, whereby all people living with HIV were recommended for ART, regardless of WHO clinical stage or CD4 cell count20. Implementation of these new guidelines will provide a critical contribution to achieving the UNAIDS’ “90-90-90” target: 90% of all people living with HIV diagnosed, 90% of all people diagnosed with HIV receiving cART, and 90% of all people receiving cART virally suppressed20, 21. However, despite recommendations to initiate ART at any CD4 cell count, there exists limited understanding about mortality, attrition, and primary treatment outcomes among HIV patients with ≥500 CD4+ cells/mm3over long-durations of ART in real-world settings.
In China, HIV-related mortality has significantly declined since the National Free Antiretroviral Treatment Program (NFATP) was initiated in 2002 and rapidly scaled up22,23,24,25,26. Following updated WHO ART guidelines in 2010, China further expanded ART services in order to reduce overall mortality among HIV infected patients, prevent transmission among key populations, and provide ART to those with higher CD4 counts7, 10, 26. By the end of 2015, more than 382,139 patients had received ART treatment27. Today, China aims to achieve significant reductions in HIV incidence and HIV-related mortality by adopting the UNAIDS 90–90–90 policy.
In Southwest China, the Guangxi Zhuang Autonomous Region accounts for 10% of all reported HIV cases nationwide28, and is critical in the country’s HIV prevention and treatment campaign. Situated in the middle of major heroin trafficking routes that begin in Southeast Asia and Southwest China, and continue on towards Guangdong and Hong Kong29, 30, injection drug use was the main mode of HIV transmission in the earlier years of the epidemic. However, by the end of 2015, sexual transmission had become the dominant mode of transmission, with heterosexual transmission accounting for 92% of reported HIV cases in Guangxi28. Based on a large ART treatment database from Guangxi, we conducted an observational cohort study in order to examine the effects of high CD4+ cell counts (≥500 cells/mm3) on treatment outcomes among HIV infected patients receiving ART in a real-world setting.
Results
General characteristics of study population
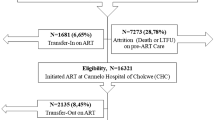
A total of 49309 HIV patients initiated ART between 2010 and 2015 in Guangxi,China, 125 of whom were less than 18 years old, and 29 of whom had no follow-up data. Thus, 49155 eligible study participants were included in this prospective follow-up study. Table 1 presents general characteristics of HIV patients. Patients over 40 years old represented 59.9% of all study participants. The percentage of males was 67.1%, and 68.7% of HIV participants were married. The main route of HIV infection was heterosexual intercourse (88.4%), followed by injection drug use (7.3%), homosexual intercourse (2.1%), and other routes of transmission (2.2%). Prior to ART initiation, patients with CD4+ counts <350 cells/mm3, 350–499 cells/mm3, and ≥500 cells/mm3 accounted for 84.5%, 10.0% and 3.7% of all patients, respectively. Those classified as WHO clinic stage III/IV before ART represented 41.2% of all patients. The percentage of patients who initiated ART with first-line ART and second-line ART was 90.3% and 9.7%, respectively. First-line ART constituted 84.5% of current regimens.
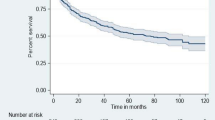
Mortality rates
Among all eligible HIV infected patients who initiated ART between 2010 and 2015 in Guangxi, China, 3411 deaths were observed, 4507 patients lost to follow-up, and 2396 patients stopped ART. Of the 2396 patients who stopped ART, 1358 (56.7%) were due to poor adherence, 437 (18.2%) were due to drug side effects, 70 (2.9%) were due to economic issues, and 531(22.2%) were due to other reasons. The average mortality rate was 2.63 deaths per 100 person-years among all patients (Table 2).
Attrition rates
Among all eligible HIV infected patients who initiated ART between 2010 and 2015 in Guangxi, China, 6903 attritions were observed. Of 6903 patient attritions, 4507 patients were lost to follow-up, and 2396 patients stopped ART. The average attrition rate was 5.32 attritions per 100 person-years among all treated patients (Table 3).
Death + attrition rates
Among all eligible HIV infected patients who initiated ART between 2010 and 2015 in Guangxi, China, 10314 death + attritions were observed. The average death + attrition rate was 7.94 per 100 person-years among all treated patients (Table 4).
Effects of pre-ART CD4 count on death
Table 5 presents the unadjusted and adjusted effects of pre-ART CD4 counts on death after ART initiation. In the adjusted models, 350–499 CD4 cells/mm3 before ART (compared to <350 cells/mm3 before ART, AHR = 0.45, 95% CI: 0.36–0.56) and ≥500 CD4 cells/mm3 before ART (compared to <350 cells/mm3 before ART, AHR = 0.56, 95% CI: 0.40–0.79) were both inversely significantly associated with death in HIV patients who started ART. Similar effects of pre-ART CD4 counts on death after ART initiation were observed even after excluding individuals with missing baseline CD4 counts (Supplementary Table 2).
Effects of pre-ART CD4 count on attrition
Table 6 presents the unadjusted and adjusted effects of pre-ART CD4+ count on attrition after ART initiation. Compared to having <350 CD4 cells/mm3 pre-ART initiation, having 350–499 CD4 cells/mm3 at pre-ART initiation was marginally significantly associated with attrition (adjusted hazard ratio (AHR = 1.08, 95% CI: 0.99–1.17), and having ≥500 CD4 cells/mm3 at pre-ART initiation was significantly associated with attrition (AHR = 1.17, 95% CI: 1.03–1.33). Similar effects of pre-ART CD4 counts on attrition after ART initiation were observed even after excluding individuals with missing baseline CD4 counts (Supplementary Table 3).
Effects of pre-ART CD4 count on death + attrition
Table 7 presents the unadjusted and adjusted effects of pre-ART CD4+ count on death + attrition after ART initiation. Compared to having <350 CD4+ cells/mm3 pre-ART initiation, neither having 350–499 CD4+ cells/mm3 at pre-ART initiation nor having ≥ 500 CD4+ cells/mm3 at pre-ART initiation was significantly associated with death + attrition (AHR = 0.94, 95% CI: 0.87–1.01 and AHR = 1.04, 95% CI: 0.93–1.18, respectively). Similar effects of pre-ART CD4 counts on death + attrition after ART initiation were observed even after excluding individuals with missing baseline CD4 counts (Supplementary Table 4).
Effects of CD4 count before ART on loss to follow-up and medication cessation
We conducted a separate analysis for loss to follow-up and medication cessation as the outcomes of interest (Supplementary Tables 6–9). Generally, the effect of ≥500 CD4 cells/mm3 at pre-ART baseline on attrition was similar to its effects on loss to follow-up and medication cessation.
Discussion
Although the “90-90-90” targets and corresponding HIV treatment guidelines have already been endorsed by UNAIDS20, additional high quality evidence is needed to better understand death and attrition rates among those who initiate ART with pre-ART ≥500 CD4+ cells/mm3. However, most relevant studies that have examined patient death and treatment attrition after ART initiation, have defined early treatment as initiating ART when CD4+ counts were ≥350 (cells/mm3)11,12,13, 15,16,17. To better understand the effects of high CD4+ cell counts (≥500 cells/mm3) on death and treatment attrition among HIV infected patients receiving ART in a real-world setting, we conducted a large observational cohort study among 49309 HIV+ patients receiving ART in rural Southwest China.
Our study found that the overall mortality rate was 2.63 per 100 person-years in HIV infected patients who started ART between 2010 and 2015 in Guangxi, China. Despite the achievements of China’s NFATP, this mortality rate remains much higher than that in developed countries2, 3. Continued improvement in the quality of HIV treatment and care is needed to further reduce the mortality rate in Chinese patients.
This large observational cohort study also showed that higher pre-ART CD4 cell counts (350–499 CD4+ cells/mm3 and >500 CD4+ cells/mm3 versus <350 cells/mm3) were associated with lower mortality risk, confirming the results of previous studies11,12,13, 15,16,17. Such findings lend strong support to China’s adoption of the UNAIDs “90–90–90” policy, which includes continued expansion of HIV counseling and testing, and ART uptake by 90% of all people with diagnosed HIV infection20, 21.
The overall attrition rate among HIV patients in this study was 5.32 per 100 person-years, which is lower than that in other developing countries, but higher than that in developed countries31, 32. Compared with pre-ART CD4 counts <350 cells/mm3, attrition was marginally significantly associated with pre-ART CD4 counts 350–499 cells/mm3, and significantly associated with pre-ART CD4 counts >500 cells/mm3. One major concern with initiating cART among patients with a high CD4+ cell counts is increased risk of poor adherence. Given that patients with higher CD4+ cell counts are more likely to be AIDS asymptomatic, such individuals may be less willing or motivated to take cART33,34,35,36. High current CD4+ counts was strongly associated with lower adherence to ART, thus indicating that enhancement of adherence education is needed, especially for patients with high CD4+ counts17. In addition, attritions were associated with both individual and contextual factors, such as younger age, male gender, being single or divorced, poor adherence and drug side effects33. Given that retention in ART and care can help improve individual clinical outcomes, evaluating and optimizing HIV clinical care is essential for developing effective adherence interventions to reduce attrition. In China, TDF has replaced both stavudine (D4T) and zidovudine (AZT) given its more favorable toxicity profile, dosing, and cost-effectiveness37. It is imperative for China to identify suitable timing to implement policies recommending initiation of ART regardless of CD4 cell counts. Rates of both death and attrition were highest among participants with missing CD4 count data, possibly due to a high proportion of individuals with WHO clinic stage III/IV before ART (31%) and possibly poor linkage to care. This study is arguably the first large, empirical study to suggest negative population-level consequences of initiating ART among HIV patients with pre-ART CD4+ counts ≥500 cells/mm3.
Our study has several limitations which warrant noting. First, although we controlled for numerous potential confounders in multivariable modeling, selection bias in the observational cohort study may have been an issue. As the study did not include individuals who were diagnosed with HIV but did not initiate ART, it is possible that individuals with poorer health-seeking behaviors were underrepresented in the study. Second, the median duration of follow-up was not very long. As time allows for longer-term studies of the new WHO treatment guidelines, future studies should consider using marginal structural models to evaluate the long-term effects of pre-ART CD4+ counts on treatment outcomes among HIV-infected patients receiving ART. Third, our study used all-cause mortality rather than HIV-related death, which arguably would have been more accurate for evaluating treatment effects. Fourth, this study was conducted in Guangxi, which only represents 13% of all HIV patients on ART in China28. Findings might not be fully representative of China. Fifth, parameter estimates may have been partially biased by the presence of unobserved time-varying confounders. Sixth, because lost to follow-up may have been associated with earlier time to death, mortality rate estimates may have been lower than the true rate.
To our knowledge, this is the first large-scale observational cohort study in a developing country to evaluate the effects of high CD4+ cell counts on treatment outcomes among HIV infected patients receiving ART. Novel results from this study provide compelling evidence for policy-makers to prioritize ART healthcare provider training, ART patient education, and the availability of simpler, more effective, safer and better tolerated regimens, especially when initiating ART among HIV-infected patients with high CD4+ cell counts. Currently, China’s HIV treatment policies reflect the WHO and UNAIDS recommended guidelines to initiate treatment among all HIV patients regardless of CD4+ count, but further monitoring of treatment outcomes is needed to elucidate the determinants of long-term programmatic success.
Methods
Study design and study participants
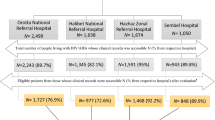
This HIV ART observational cohort study was conducted in Guangxi, rural southwest China. Patients initiating free ART through the NFATP between January 1, 2010 and October 31, 2015 were included. Patients who did not initiate ART during that time frame were not included in the study. Individuals who initiated free ART and were at least 18 years old at the time of ART initiation and provided informed consent were eligible to participate in the study. The Chinese national ART treatment criteria since 2010 was: (1) CD4 cell count <350/mm3; or (2) World Health Organization (WHO) stage III/IV clinic conditions; or (3) willingness to receive ART, regardless of the criteria 1 and 2, such as initiating ART at high CD4+ cell counts37. Currently, first-line ART regimens consist of [tenofovir (TDF) or azidothymidine (AZT)] + lamivudine (3TC) + [efavirenz (EFV) or nevirapine (NVP)]. Second-line ART regimens consist of TDF + 3TC + EFV/(LPV/r). By the end of 2015, more than 62,967 HIV patients had received ART in Guangxi, representing 13% of the total number of HIV patients on treatment in China28. This study and all methods were approved by the institutional review board (IRB) of the Guangxi Center for Disease Control and Prevention. All research methods in this study were carried out in accordance with the approved guidelines.
Data collection
Variables collected at baseline enrollment into the HIV ART observational cohort included: age, sex, ethnicity, marital status, route of HIV infection, CD4 count in the six months before ART, WHO clinic stage in the six months before ART, initial ART regimen, current ART regimen, and year of ART initiation. Variables collected at each follow-up included: transferals to another clinic, cessation of ART, loss to follow-up, duration of ART, and survival status. The follow up visits occurred at 0.5, 1, 2, and 3 months following ART initiation, and then every 3 months thereafter. Lost to follow-up was defined as missing more than 90 days after the last date seen in clinic, which was also defined as the date of withdrawal.
Statistical analysis
We conducted a prospective cohort analysis using Guangxi data from the NFATP. Treatment outcomes included death and attrition. Attrition was defined as cessation of ART or lost to follow-up as reported through the NFATP database. Time zero was defined as the date of ART initiation, and data were censored at April 30, 2016. Incidence rates were calculated based on Poisson distributions. Death, attrition, and death or attrition (death + attrition) incidence rates and their 95% confidence intervals (CI) were analyzed with incidence densities per 100 person-years of follow-up.
Cause-specific Cox proportional hazard models38 were used to evaluate effects of CD4+ count levels before ART on death, attrition, and death + attrition. Competing risks for cause-specific hazard models were censored accordingly. In order to control for potential confounding, the following baseline covariates of the adjusted model were included: age, sex, ethnicity, marital status, route of HIV infection, WHO clinic stage before ART, initial ART regimen, and year initiated ART. A two-sided p-value of 0.05 or less was regarded as statistically significant. Statistical Analysis System (SAS 9.1TM for Windows; SAS Institute Inc., NC, USA) was used for all the analyses.
Management of missing baseline CD4 data
A sensitivity analysis was conducted to assess for potential bias resulting from the 1.8% of individuals with missing baseline CD4 data, the only covariate with any missing data. First, we compared baseline demographics and treatment variables for complete cases (n = 48,271) and cases with missing baseline CD4 data (n = 884) (Supplementary Table 1). Results showed that demographics were similar between complete and missing cases, although cases with missing CD4 data appeared slightly less likely to be diagnosed as WHO clinic stage III/IV, compared to complete cases overall (31.4% vs 41.3%). Then, we re-analyzed the data using a complete-case analysis approach, whereby individuals with missing CD4 data were excluded from analysis (Supplementary Tables 2–4). Results of the sensitivity analysis indicated that effects of pre-ART CD4 counts on death, attrition, and death + attrition, were not meaningfully influenced by inclusion or exclusion of individuals with missing baseline CD4 data.
We also examined the proportion of individuals diagnosed as WHO clinic stage III/IV, stratified by baseline CD4 count in order to draw inferences about baseline CD4 counts among individuals with missing baseline CD4 data (Supplementary Table 5). Results showed that individuals with missing baseline CD4 data were four times more likely to be diagnosed as WHO clinic stage III/IV, compared to individuals with baseline CD4 counts greater than 500 cells/mm3 (31.5% vs 8.1%). Given that 46.8% of individuals with baseline CD4 counts <350 cells/mm3 were diagnosed as WHO clinic stage II/IV and assuming moderate to strong correlation between WHO clinical staging and baseline CD4 counts, these results suggest that the majority of individuals with missing baseline CD4 counts had actual CD4 counts below 350 cells/mm3.
References
Moore, R. D. & Chaisson, R. E. Natural history of HIV infection in the era of combination antiretroviral therapy. Aids 13, 1933–1942 (1999).
Palella, F. J. Jr. et al. Declining morbidity and mortality among patients with advanced human immunodeficiency virus infection. HIV Outpatient Study Investigators. The New England journal of medicine 338, 853–860, doi:10.1056/nejm199803263381301 (1998).
May, M. T. et al. HIV treatment response and prognosis in Europe and North America in the first decade of highly active antiretroviral therapy: a collaborative analysis. Lancet 368, 451–458, doi:10.1016/S0140-6736(06)69152-6 (2006).
Lewden, C. et al. Disease patterns and causes of death of hospitalized HIV-positive adults in West Africa: a multicountry survey in the antiretroviral treatment era. Journal of the International AIDS Society 17, 18797, doi:10.7448/IAS.17.1.18797 (2014).
Quinn, T. C. et al. Viral load and heterosexual transmission of human immunodeficiency virus type 1. Rakai Project Study Group. The New England journal of medicine 342, 921–929, doi:10.1056/NEJM200003303421303 (2000).
Fideli, U. S. et al. Virologic and immunologic determinants of heterosexual transmission of human immunodeficiency virus type 1 in Africa. AIDS research and human retroviruses 17, 901–910, doi:10.1089/088922201750290023 (2001).
Jia, Z. et al. Antiretroviral therapy to prevent HIV transmission in serodiscordant couples in China (2003–11): a national observational cohort study. Lancet 382, 1195–1203, doi:10.1016/S0140-6736(12)61898-4 (2013).
Fang, C. T. et al. Decreased HIV transmission after a policy of providing free access to highly active antiretroviral therapy in Taiwan. The Journal of infectious diseases 190, 879–885, doi:10.1086/422601 (2004).
Cohen, M. S. et al. Prevention of HIV-1 infection with early antiretroviral therapy. The New England journal of medicine 365, 493–505, doi:10.1056/NEJMoa1105243 (2011).
Tang, Z. et al. HIV-1 Treatment-as-Prevention: A Cohort Study Analysis of Serodiscordant Couples in Rural Southwest China. Medicine 94, e902, doi:10.1097/MD.0000000000000902 (2015).
Grinsztejn, B. et al. Effects of early versus delayed initiation of antiretroviral treatment on clinical outcomes of HIV-1 infection: results from the phase 3 HPTN 052 randomised controlled trial. The Lancet. Infectious diseases 14, 281–290, doi:10.1016/S1473-3099(13)70692-3 (2014).
Cain, L. E. et al. When to initiate combined antiretroviral therapy to reduce mortality and AIDS-defining illness in HIV-infected persons in developed countries: an observational study. Annals of internal medicine 154, 509–515, doi:10.7326/0003-4819-154-8-201104190-00001 (2011).
Kitahata, M. M. et al. Effect of early versus deferred antiretroviral therapy for HIV on survival. The New England journal of medicine 360, 1815–1826, doi:10.1056/NEJMoa0807252 (2009).
Sterne, J. A. et al. Timing of initiation of antiretroviral therapy in AIDS-free HIV-1-infected patients: a collaborative analysis of 18 HIV cohort studies. Lancet 373, 1352–1363, doi:10.1016/s0140-6736(09)60612-7 (2009).
Lima, V. D. et al. Initiation of antiretroviral therapy at high CD4+ cell counts is associated with positive treatment outcomes. Aids 29, 1871–1882, doi:10.1097/qad.0000000000000790 (2015).
Clouse, K. et al. Initiating antiretroviral therapy when presenting with higher CD4 cell counts results in reduced loss to follow-up in a resource-limited setting. Aids 27, 645–650, doi:10.1097/QAD.0b013e32835c12f9 (2013).
Pasternak, A. O., de Bruin, M., Bakker, M., Berkhout, B. & Prins, J. M. High Current CD4+ T Cell Count Predicts Suboptimal Adherence to Antiretroviral Therapy. PloS one 10, e0140791, doi:10.1371/journal.pone.0140791 (2015).
World Health Organization. Rapid advice antiretroviral therapy for HIV infection in adults and adolescents http://www.who.int/hiv/pub/arv/advice/en/index.html (2009).
World Health Organization.Antiretroviral Therapy for HIV Infection in Adults and Adolescents: Recommendations for a Public Health Approach: 2010 Revision. http://www.who.int/hiv/pub/arv/adult2010/en/index.html (2010).
The Joint United Nations Programme on HIV/AIDS. 90-90-90: An ambitious treatment target to help end the AIDS epidemic http://www.unaids.org/en/resources/documents/2014/90–90–90 (2014).
World Health Organization. Guideline on when to start antiretroviral therapy and on pre-exposure prophylaxis for HIV http://www.who.int/hiv/pub/guidelines/earlyrelease-arv/en/ (2015).
Shen, Z. et al. Effects of CD4 Cell Counts and Viral Load Testing on Mortality Rates in Patients With HIV Infection Receiving Antiretroviral Treatment: An Observational Cohort Study in Rural Southwest China. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America 63, 108–114, doi:10.1093/cid/ciw146 (2016).
Zhang, F. et al. Effect of earlier initiation of antiretroviral treatment and increased treatment coverage on HIV-related mortality in China: a national observational cohort study. The Lancet. Infectious diseases 11, 516–524, doi:10.1016/s1473-3099(11)70097-4 (2011).
Zhang, F. et al. Five-year outcomes of the China National Free Antiretroviral Treatment Program. Annals of internal medicine 151, 241–251, W-252 (2009).
Zhang, F. et al. The effect of highly active antiretroviral therapy on mortality among HIV-infected former plasma donors in China. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America 47, 825–833, doi:10.1086/590945 (2008).
Zhao, D. C. et al. Expansion of China’s free antiretroviral treatment program. Chinese medical journal 125, 3514–3521 (2012).
NCAIDS, NCSTD, and China CDC. Update on the AIDS/STD epidemic in China and main response in control and prevention in December, 2015. Chinese journal of AIDS & STD 22, 2(2): 69–70, doi:10.13419/j.cnki.aids.2015.0501 (2016).
Guangxi Public Health Department. Annual Report on Provincial AIDSSTD Surveillance in 2015. Guangxi: Guangxi Public Health Department (2015).
Yu, X. F. et al. Emerging HIV infections with distinct subtypes of HIV-1 infection among injection drug users from geographically separate locations in Guangxi Province, China. Journal of acquired immune deficiency syndromes (1999) 22, 180–188 (1999).
Beyrer, C. et al. Overland heroin trafficking routes and HIV-1 spread in south and south-east Asia. Aids 14, 75–83 (2000).
Geng, E. H. et al. Understanding reasons for and outcomes of patients lost to follow-up in antiretroviral therapy programs in Africa through a sampling-based approach. Journal of acquired immune deficiency syndromes (1999) 53, 405–411, doi:10.1097/QAI.0b013e3181b843f0 (2010).
Braitstein, P. et al. Mortality of HIV-1-infected patients in the first year of antiretroviral therapy: comparison between low-income and high-income countries. Lancet 367, 817–824, doi:10.1016/s0140-6736(06)68337-2 (2006).
Zhu, H. et al. Attrition among human immunodeficiency virus (HIV)- infected patients initiating antiretroviral therapy in China, 2003–2010. PloS one 7, e39414, doi:10.1371/journal.pone.0039414 (2012).
Nachega, J. B. et al. Addressing the Achilles’ heel in the HIV care continuum for the success of a test-and-treat strategy to achieve an AIDS-free generation. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America 59(Suppl 1), S21–27, doi:10.1093/cid/ciu299 (2014).
Katz, I. T. et al. Antiretroviral therapy refusal among newly diagnosed HIV-infected adults. Aids 25, 2177–2181, doi:10.1097/QAD.0b013e32834b6464 (2011).
Ford, N. et al. Early initiation of antiretroviral therapy and associated reduction in mortality, morbidity and defaulting in a nurse-managed, community cohort in Lesotho. Aids 24, 2645–2650, doi:10.1097/QAD.0b013e32833ec5b2 (2010).
Manual of the National Free Antiretroviral Treatment, third edition. http://www.chinaaids.cn/zlgh/jswj4/201301/t20130110_75457.htm (2012).
Austin, P. C., Lee, D. S. & Fine, J. P. Introduction to the Analysis of Survival Data in the Presence of Competing Risks. Circulation 133, 601–609, doi:10.1161/circulationaha.115.017719 (2016).
Acknowledgements
Data in this manuscript were collected by Guangxi Center for Disease Control and Prevention. Principal investigators included Z.T., Z.S., and Q.Z. (Guangxi Center for Disease Control and Prevention). This study was supported by the National Natural Science Foundation of China (grants 81460510, 81360442 and 81502862), Guangxi Science and Technology Bureau (AB16380213), Guangxi Bagui Honor Scholars, Ministry of Science and Technology of China (grant 2012ZX10001-002), Chinese State Key Laboratory of Infectious Disease Prevention and Control, and the International Development Research Center of Canada (grant 104519-010).
Author information
Authors and Affiliations
Contributions
Z.T., S.W.P., Y.R., Z.S. and Y.S. were responsible for study design and planning; X.L., Q.Z., Z.S., Y.C., G.L. contributed to data collection and management; Y.R., X.L., J.S., Q.Z. and H.Z. contributed to data analysis. Z.T., S.W.P., Y.R., Z.S., Y.C., G.L., H.X., L.L., Y.F. and Y.S. contributed to interpretation. Z.T., S.W.P., Y.R., X.L. and Y.S. contributed to writing the report. All authors approved the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tang, Z., Pan, S.W., Ruan, Y. et al. Effects of high CD4 cell counts on death and attrition among HIV patients receiving antiretroviral treatment: an observational cohort study. Sci Rep 7, 3129 (2017). https://doi.org/10.1038/s41598-017-03384-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-03384-7
This article is cited by
-
HIV transmission and associated factors under the scale-up of HIV antiretroviral therapy: a population-based longitudinal molecular network study
Virology Journal (2023)
-
Baseline and Process Factors of Anti-Retroviral Therapy That Predict Loss to Follow-up Among People Living with HIV/AIDS in China: A Retrospective Cohort Study
AIDS and Behavior (2022)
-
Modeling the survival in patients with HIV by the presence of competing risks for death: sub-distribution and cause-specific hazard approach
Journal of Public Health (2022)
-
Effect of AIDS-defining events at initiation of antiretroviral therapy on long-term mortality of HIV/AIDS patients in Southwestern China: a retrospective cohort study
AIDS Research and Therapy (2020)
-
Effects of HIV-1 genotype on baseline CD4+ cell count and mortality before and after antiretroviral therapy
Scientific Reports (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.