Abstract
We performed this meta-analysis to examine the diagnostic accuracy of MRI for the diagnosis of anterior cruciate ligament (ACL) injury in comparison to arthroscopy. We also compared the diagnostic accuracy of MRI with magnetic field intensities (MFI) greater than or equal to 1.5T with those below 1.5T, in addition to different MRI sequences. Studies relevant to the diagnosis of ACL injury by MRI and arthroscopy were analyzed. Computer and manual retrieval were carried out on studies published between January 1, 2006 and May 31, 2016. Twenty-one papers were included. Neither threshold nor non-threshold effects were present (p = 0.40, p = 0.06). The pooled sensitivity (SE), specificity (SP), positive likelihood ratio (LR+), negative likelihood ratio (LR−) and diagnostic odds ratio (DOR) with 95% confidence interval (CI) were 87% (84–90%), 90% (88–92%), 6.78 (4.87–9.44), 0.16 (0.13–0.20) and 44.70 (32.34–61.79), respectively. The area under the curve (AUC) was 0.93. The risk of publication bias was negligible (p = 0.75). In conclusion, examination by MRI is able to provide appreciable diagnostic performance. However, the principle, which states that the higher the MFI, the better the diagnostic accuracy, could not be verified. Additionally, conventional sequences (CSs) associated with proton density-weighted imaging (PDWI) are only slightly better than CSs alone, but not statistically different.
Similar content being viewed by others
Introduction
The anterior cruciate ligament (ACL) extends from the posterior surface of the medial femoral condyle and attaches to the intercondylar process of the tibia. Its average length is 31–38 mm and its average intersecting surface area is 36 mm2 in females and 44 mm2 in males1. It can be divided into anteromedial and posterolateral bundles. The main function of the ACL is to limit the forward slip of the tibia on the femur. The anteromedial bundle of the ACL can prevent excessive external rotation of the leg, whereas the posterolateral bundle prevents excessive internal rotation. With the posterior cruciate ligament, the ACL limits excessive flexion, and excessive extension in combination with the posterior cruciate ligament, the medial and lateral collateral ligaments, the articular capsule and the oblique popliteal ligament2. It also contributes to restriction of lateral slip and rotation with the articular capsule, the medial and laterial collateral ligaments and the posterior cruciate ligament3.
Injuries of the ACL are generally sports-related traumas with nearly three quarters being non-contact4. They are a major problem worldwide with approximately 200,000 cases per year in the United States alone5. Isolated injuries of the ACL are most frequently caused by forced extension stress associated with “kissing contusions” of the anterior portion of the lateral femoral condyle and of the lateral tibial plateau. It is less frequently caused by forced flexion stress associated with avulsion fracture of the tibial eminence. Associated injuries of the ACL and other structures are caused by a variety of events: (i) ACL injury associated with medial collateral ligament and medial meniscus injury is caused by forced flexion-external rotation stress; (ii) damage associated with lateral compartment injury is caused by forced flexion-internal rotation stress; (iii) when associated with lateral and medial compartment injury it is caused by different associations of varus-valgus and rotatory stress; (iv) when associated with posterior cruciate ligament injury it is caused by posterior displacement of the tibia and knee hyperextension4, 6.
Arthroscopy allows direct visualization of all intra-articular structures and thus provides a high level of accuracy for both diagnosis and treatment, which makes arthroscopy the gold standard for evaluation of internal disorders and other lesions of the knee7. However, arthroscopy constitutes a relatively expensive and invasive examination8. Besides, it is less effective for the assessment of extracapsular soft tissues9.
Magnetic resonance imaging (MRI) is a non-invasive method with good soft tissue contrast, high spatial resolution, multi-parameter and multi-range imaging for the evaluation of knee lesions10. It can clearly display the injury site of the ACL, the extent of the damage, the degree of injury and the damage to the related structures. Although MRI has recently played an increasing role in the evaluation of knee lesions, its diagnostic potential for ACL injury is limited and diagnosis fallible9.
Recent studies have compared the diagnostic accuracy of 1.5T MRI with 3.0T MRI11, MRI combined with ultrasonography12, and MRI combined with physical examination8, 13. However, the exact diagnostic accuracy of MRI for ACL injury is unknown, as are the differences in diagnostic accuracy between MRI with magnetic field intensities (MFI) greater than or equal to 1.5T compared with those below 1.5T, or between different MRI sequences, The objectives of this meta-analysis were to (i) systematically examine the diagnostic accuracy of MRI for the diagnosis of ACL injury; (ii) compare the diagnostic accuracy of MFI greater than or equal to 1.5T with MFI below 1.5T; and (iii) compare the diagnostic accuracy of different MRI sequences.
Results
Study selection
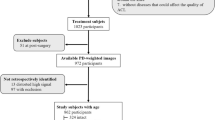
A total of 1922 articles were initially retrieved for this meta-analysis: 481 from PubMed, 783 from EMBASE, 470 from Ovid, 129 from BIOSIS Previews, 53 from the Cochrane library and 6 articles obtained from manual retrieval of relevant references by sending e-mails to authors. 759 reports were then eliminated out of 1232 duplicated reports as they originated from the same team or the same set of data. According to the inclusion and exclusion criteria for the initial screening, a total of 110 articles were thus selected after reading the title and abstract (71 from PubMed, 24 from EMBASE, 11 from Ovid and 4 from the Cochrane library) and the articles were marked with 1 star in EndNote software. By evaluating the full text, two researchers (K.L. and J.D.) then selected 31 papers that strictly complied with the inclusion and exclusion criteria and marked them with 2 stars in EndNote. Ten studies were excluded after re-assessing the full text during the third screening. Finally, 21 articles9, 14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33 were chosen and marked with 3 stars, articles for which true positive (TP), false positive (FP), true negative (TN) and false negative (FN) results could be extracted or accurately calculated through 2 × 2 contingency tables (16 from PubMed and 5 from EMBASE). These articles consisted of 16 prospective studies and 5 retrospective studies, for a total of 1722 cases. The literature search, the screening process and the results are shown in Fig. 1. The basic characteristics of the studies which were included are displayed in Table 1. From a chronological point of view, 38% (8/21) of these studies were published between 2006–2009 inclusive and 62% (13/21) in the period 2012–2016.
Flow of information through the different phases of the meta-analysis. From: Moher, D., Liberati, A., Tetzlaff, J. & Altman, D. G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS medicine 6, e1000097, doi:10.1371/journal.pmed.1000097 (2009).
Assessment of risk of bias within studies
The methodological quality assessment of risk of bias within eligible studies is shown in Fig. 2, according to the Quality Assessment of Diagnostic Accuracy Studies 2 (QUADAS-2) tool. Overall, the number of low and unclear risk of bias was 39 and 45, respectively, for the four domains (patient selection, index test, reference standard, and flow and timing). The number of high, unclear and low concerns regarding applicability was 42, 8 and 13, respectively for the three domains (patient selection, index test and reference standard).
Heterogeneity test of individual studies
Results of the heterogeneity test for the threshold effect were as follows: the variation tendency of sensitivity (SE) and specificity (SP) or positive likelihood ratio (LR+) and negative likelihood ratio (LR−) were not negatively correlated in forest plots (Fig. 3A–D). The distribution of accuracy estimates of each independent study did not show the “shoulder arm” shape in the summary receiver operator characteristic (sROC) plane (Fig. 4). Results of the Spearman correlation (p = 0.40 and r = 0.194) between the logit of sensitivity and the logit of 1-specificity indicates that the threshold effect was absent. Regarding the heterogeneity test for the non-threshold effect, results of the Cochran-Q test (p = 0.06) indicates that the non-threshold effect was also absent (Fig. 5).
Forest plot of sensitivity, specificity, positive LR and negative LR of MRI for the diagnosis of ACL injury. (A) Sensitivity for MRI. (B) Specificity for MRI. (C) Positive LR for MRI. (D) Negative LR for MRI. Corresponding indices, 95% CI and the pooled indices are represented by red circles, horizontal lines and red diamonds, respectively. LR: likelihood ratio; CI: confidence interval.
The sROC plane for heterogeneity test of threshold effect of each independent study. The sROC (middle line) with 95% CI (the other two lines) of MRI in diagnosing of ACL injury. sROC: summary receiver operator characteristic; CI: confidence interval; AUC: area under the curve; Q*: Q index value; SE: standard error.
A random effects model was used for pooled SE [p < 0.001, inconsistency index (I 2) = 57.9%], pooled SP (p < 0.001, I 2 = 72.7%) and pooled LR+ (p < 0.001, I 2 = 64.3%) (Fig. 3A–C). A fixed effects model was used for pooled LR− (p = 0.12, I 2 = 27.2%) (Fig. 3D) and pooled diagnostic odds ratio (DOR) (p = 0.06, I 2 = 34.5%) (Fig. 5) respectively. The I 2 statistics based on Chi square (where Q is the chi-square statistic) was used to quantify the degree of heterogeneity in eligible studies and expresses the percentage of total variation observed across studies caused by heterogeneity rather than by chance. There is no observed heterogeneity when I 2 = 0, implying that all the variability observed in the effect estimates is due to sampling errors rather than because of heterogeneity amongst trials. Heterogeneity that is low, moderate, or high relates to I 2 < 25%, 50% < I 2 < 75%, I 2 > 75% respectively. Values of I 2 = 25%, 50% or 75% are defined as 1/4, 1/2 or 3/4 of the variability observed in the effect estimates being attributable to inconsistency among trials.
Synthesis of results
The pooled SE was 87% [95% confidence interval (CI), 84–90%] and the pooled SP 90% (95% CI, 88–92%), whereas the pooled LR+ was 6.78 (95% CI, 4.87–9.44) and the pooled LR− 0.16 (95% CI, 0.13–0.20) (Fig. 3). The pooled DOR was 44.70 (95% CI, 32.34–61.79) (Fig. 5) and the area under the curve (AUC) was 0.93 (Fig. 4).
Subgroup analysis
The differences between subgroups were calculated according to the MFI, the year of publication and the type of MRI sequence [conventional sequences (CSs) and CSs with proton density weighted imaging (PDWI)]. The results are listed in Table 2 and include the pooled SE, SP, LR+, LR−, DOR and AUC values.
Publication bias in the literature evaluation
The Deeks’ funnel plot asymmetry test for DOR presented basic symmetry (Fig. 6). Nevertheless, results showed no significant risk of publication bias (p = 0.75).
Discussion
Overall, ACL injury is a common clinical form of knee damage. Timely and accurate diagnosis and treatment could prevent the emergence of cartilage degeneration, the progression of bone contusion, the aggravation of traumatic arthritis or the occurrence of knee joint dysfunction34.
Magnetic resonance imaging is a noninvasive technique that remains a physician’s first choice for the clinical diagnosis of ACL injury. It has the advantages of good soft tissue contrast, high spatial resolution and allows multi-parameter evaluation of morphological changes in an injured ACL. However, it is likely that overuse of the MRI technique in the diagnosis of ACL injury leads to misdiagnosis (estimated at 47%), especially in a chronic incomplete tear which might be due to the special sensitivity to the hydrogen atom and could be associated with volume effects and synovial hyperplasia18. Additionally, different studies have attributed different values for sensitivity and specificity, ranging from 63.6%14 to 100%9, 19, 29 and from 68.4%26 to 100%16, 19, 28 respectively, owing to the slightly oblique angle of the ACL crossing the knee joint and to the difficulty of displaying the full ACL in the true sagittal plane via a single MRI scan22. Meanwhile, the accuracy of MRI diagnosis depends on the scanning technique and the experience of the musculoskeletal radiologist30. Thus, the precise diagnostic accuracy of MRI for ACL injury is unknown. It is necessary, therefore, to carry out high level evidence-based medical research on the accuracy of MRI diagnosis for ACL injury.
Our meta-analysis focused on the diagnostic accuracy of MRI for ACL injury compared with arthroscopy. The pooled SE and SP are 87% (95% CI, 84–90%) and 90% (95% CI, 88–92%) respectively, indicating that the rate of missed diagnosis and misdiagnosis reach 13% and 10%, respectively. Furthermore, a good diagnostic test may have a LR+ superior to 10 and a LR− inferior to 0.1. Our study revealed that the pooled LR+ reaches 6.78 (95% CI, 4.87–9.44), which means that it is possible that ACL injury occurred in suspected cases when the MRI result was positive. Moreover, the pooled LR− had a value of 0.16 (95% CI, 0.13–0.20). In other words, there is a real possibility of excluding an ACL injury in suspected injured patients when the MRI result was negative. In addition, DOR represents a summary measure of the power of the test and the higher this measure, the better the performance of the inspection method35. The pooled DOR was 44.70 (95% CI, 32.34–61.79) in the present study, which predicts that the odds of obtaining a positive result using MRI are 44.7 times higher for an ACL injury than for an intact knee. In addition, the area under the curve (AUC) was 0.93, which indicates that MRI examination has a high diagnostic accuracy. Low, medium and appreciable accuracies of diagnosis are considered for AUC values ranging from 0.5 to 0.7, 0.7 to 0.9 and ≥0.9, respectively. The maximum AUC value of 1 predicts that the diagnostic test is perfect for differentiation in diagnostic test evaluation. In contrast, an AUC value < 50% indicates a poor performance of the diagnostic test13.
The MFI of MRI is one of the most important factors affecting accuracy of diagnosis. Smith et al. (2016) proved that there is no evidence that 3T scanners had superior diagnostic efficacy for ACL injury when compared with 1.5T machines11. Similarly, Phelan et al. (2015) and Smith et al. (2012) also reported that magnetic field strength had no significant effect on accuracy12, 36. Our results indicate that there are no significant differences in SE, SP, LR+, LR− and DOR between MFI greater than or equal to 1.5T and MFI below 1.5T (p = 0.85, p = 0.76, p = 0.84, p = 0.75, p = 0.84, respectively), which is not only consistent with the results of previous studies, but also corroborate previous studies.
Another important factor that affects the diagnostic accuracy is the MRI sequence. Oei et al. (2003) reported that improving the MRI sequence could improve diagnostic accuracy37. However, no study has yet compared the accuracy of diagnosis between different MRI sequences. Our meta-analysis provides evidence that there are no significant differences in SE, SP, LR+, LR− or DOR between CSs and CSs + PDWI (p = 0.95, p = 0.34, p = 0.53, p = 0.90, p = 0.45, respectively). Moreover, the SE of the two groups were equal (SE = 0.87). However, we found that the SP, LR+, LR− and DOR values were better in CSs + PDWI than in CSs.
In previous reviews, the impact of the study’s year of publication was found to be variable. Oei et al. (2003) reported that recent studies had better diagnostic accuracy than older studies37, which is likely due to improvements made in imaging technology such as the use of specific knee coils, improved sequences and radiologist familiarity with MRI over time. In contrast, Crawford et al. (2007) found that there is a negative trend in diagnostic accuracy with more recent studies38, which may be due to differences in the prevalence of ACL tears in the selected studies. They also reported that older studies had better methodological quality than recent studies. Therefore, they included all studies regardless of the year of publication. Our meta-analysis found that SP was significantly different between studies published during the periods 2006–2009 and 2012–2016 (SP = 0.93 vs. SP = 0.89, respectively; p = 0.04). Through a detailed reading of the literature included in the meta-analysis, we found that this was due to SP values of three articles that reached 100%16, 19, 28, which may be related to the MRI sequence or the specific knee coil used in their original study, such as fat-suppressed PD-weighted TSE-sequence and 3-minute three-dimensional isovoxel true FISP MR sequence or MRI devices using an eight-channel phased-array knee coil with coronal short tau inversion recovery sequence. On the other hand, there are seven studies that did not mention the sequence that was used and six of them were published during the 2012–2016 period. Meanwhile, our results indicated that there were no significant differences in SE (p = 0.08), LR+ (p = 0.09), LR− (p = 0.11) or DOR (p = 0.75) values between studies published during the 2006–2009 period and those during the 2012–2016 period. The SE and LR− values were better in recent studies than in older studies, while the LR+ and DOR values were better in older studies. Therefore, we could not draw any conclusion regarding which publication period produced better results. This aspect would need further investigation.
Our meta-analysis has not only updated, verified, supplemented and improved previous studies, but it has also provided an objective and systematic evaluation of the value of MRI diagnosis for ACL injury, including its diagnostic accuracy and methodology. Additionally, our research suggested new direction for future diagnosis experiments. Firstly, future studies should attempt when possible to use the standards for reporting of diagnostic accuracy (STARD) in their diagnostic tests, and try to evaluate in detail the authenticity, reliability and clinical importance of their diagnostic tests, in order to make their results more accurate, complete and conclusive39. Secondly, the diagnostic and control tests should be performed as soon as possible during the study process, and acquisition conditions clearly defined. Ultimately, the assessment of the test results should be double-blinded. Finally, by comparing different MFIs and the different sequences used for ACL injury, we provided reference and guidance for clinicians who choose MRI for patients with ACL damage.
Even though this meta-analysis showed optimistic results for the diagnostic accuracy of ACL injury, the outcomes should be viewed cautiously due to several limitations related to this meta-analysis. Firstly, the selected studies varied greatly in sample size, continuity of enrolled patients and patient race in addition to scanning conditions. Besides, the MFI parameter, the method used to blind participants and assessors or the familiarity of the radiologist were not mentioned in several studies that were included. Secondly, our method cannot identify an accurate cut-off point on the sROC curve, which is in agreement with other meta-analysis of diagnostic accuracy. The reason is that there is no precisely measured value for the MR image and a threshold is not used in clinical examination13.
In conclusion, current evidence of our meta-analysis indicates that MRI examination is able to provide appreciable diagnostic performance for DOR and AUC in the detection of ACL injury with high SE and SP (greater than 85%). Yet, there is not enough evidence to show that a higher MFI results in better diagnostic accuracy when MFI greater than or equal to 1.5T was compared with MFI below 1.5T. In addition, CSs + PDWI sequences are only slightly better than CSs, but without any statistical difference.
Materials and Methods
Inclusion and exclusion criteria
The inclusion and exclusion criteria were formulated based on the PICOS principles (participants, intervention, comparison, outcome and study design) of preferred reporting items for systematic reviews and meta-analyses (PRISMA)40. Studies relevant to the diagnosis of ACL injury by MRI and Arthroscopy were included. Inclusion criteria contained the following five conditions.
Participants and intervention measures
Patients suspected of having ACL injury/tear, examined by MRI and arthroscopy. Patients’ age, gender or race did not limit inclusion.
Comparison
MRI versus arthroscopy.
Outcomes
We obtained the pooled SE, SP, LR+, LR−, DOR and the sROC curve by extracting (directly or indirectly) the raw data (TP, FP, TN and FN results).
Study design
Prospective or retrospective study.
Languages and publication time
Studies in English published from January 1, 2006 to May 31, 2016 were included.
Exclusion criteria
Studies were excluded if they met one of the following conditions: (1) the type of article was a review, an abstract or a conference paper; (2) the study was performed on animals or cadavers; (3) the sample size of the study was less than 25 cases; (4) the raw data was not complete, thus preventing the calculation of TP, FP, FN or TN; (5) the patients were not examined using MRI and arthroscopy simultaneously; (6) clinical data were insufficient; (7) repeated reports came from the same team or the same set of data.
Search strategy
Computer retrieval of English studies from PubMed, EMBASE, and Ovid databases, in addition to BIOSIS Previews and the Cochrane library was performed from January 1, 2006 to May 31, 2016. In addition, a manual retrieval was achieved based on references, magazines, ResearchGate, the national library reference service platform or by sending emails to authors. We used the following MeSH heading and keywords: magnetic resonance imaging AND anterior cruciate ligament AND arthroscopy.
Screening and literature selection
The screening of the original literature should be strictly followed by the inclusion and exclusion criteria. There were four steps in the selection process. Firstly, the two researchers eliminated duplicated reports coming from the same team or the same set of data. Secondly, the two researchers selected the papers by reading titles and abstracts according to the inclusion and exclusion criteria. Thirdly, by evaluating the full text, the two researchers screened the potentially available studies conforming to the inclusion and exclusion criteria. Fourthly, to re-assess the full text, the two researchers chose the studies for which TP, FP, TN and FN could be extracted and calculated. The two researchers completed the screening process independently. When their opinions differed, they discussed the results until they reached the same conclusions.
Data extraction
The two researchers designed a standardized abstract form, extracted data respectively and mutually checked their data. Disagreements relating to values or assessment were resolved by discussion. Extracted variables included: the author, the year of publication, the country where the study had been performed, the study designation, MFI, the number of samples, the demographic characteristics, the blinding process and TP, FP, TN, FN, SE and SP values.
Quality evaluation
The methodological assessments of the quality of eligible studies were graded by two researchers independently, according to the QUADAS-2 tool (Agency for Healthcare Research and Quality, Cochrane Collaboration, and the U.K. National Institute for Health and Care Excellence)41, which is recommended for use in systematic reviews of diagnostic accuracy based on sources of bias and variation. The following four aspects are required to use the QUADAS-2 tool: (1) summarize the evaluation question; (2) develop the tool and produce evaluation with guidance; (3) construct a flow diagram for the original study; and (4) judge bias and applicability. The QUADAS-2 tool can provide obvious grades of bias and applicability of primary diagnostic accuracy studies. It comprises four significant domains including: (1) patient selection; (2) index test; (3) reference standard; and (4) the flow and timing. Each domain contains several signal questions used to help judge the risk of bias (low, high or unclear)41. The two researchers completed the screening process independently. Disagreement in the process of answering questions was discussed until consensus was reached. A final decision of “yes (satisfactorily elaborated)”, “no (unsatisfactorily elaborated)” or “unclear (data are insufficient making a judgment difficult)” was made by the researchers after systematic discussion. If the answers to all the signal problems were “yes”, a low risk of bias was attributed to the study; if the answers to all the signal problems had one or more “no” or “unclear” values, an unclear risk of bias was used; if the answers to all the signal problems contained at least one “no” but no “yes” answers, a high risk of bias was attributed. QUADAS-2 tabular and graphical display can be retrieved from the Web page, http://www.bris.ac.uk/quadas/quadas-2.
Statistical analysis
Meta-Disc 1.4 for Windows (XI Cochrane Colloquium, Barcelona, Spain) statistical software was used for the heterogeneity test, outcomes combination and subgroup analysis42. Stata 14.0 (Stata Corp., College Station, TX, USA) was used for publication bias. A two-sided statistical test was considered suitable and statistical significance was set at p < 0.05.
Heterogeneity is usually caused by threshold and non-threshold effects. If the threshold effect exists, the pairs of accuracy estimates (SE and SP, or LR+ and LR−) are negatively correlated (or SE is positively correlated with 1 - SP), or vice versa; the accuracy estimates distribution of each independent study shows a typical “shoulder arm” shape in the sROC curve; or the Spearman correlation coefficient reflects a significant relationship between the logit of sensitivity and the logit of 1-specificity according to p and r values. Besides the threshold effect, non-threshold effects also cause heterogeneity, including population (such as disease severity and complications), test conditions (such as different technologies, laboratory tests and operators), standard tests and so on. This can be detected through Chi-square and Cochran-Q statistical tests. If non-threshold effects exist, then p < 0.0543.
A fixed effects model was used with no heterogeneity among individual studies when p > 0.05 and I 2 < 50%. This calculation model of the combined effect indicated that all the variation in the eligible studies was caused by chance. In other words, the model assumed that the measurements over all effects were from the same population. Otherwise, a meta-regression analysis can be used to explore the potential factors of heterogeneity (such as the participants, the test, the standard test, the methodological characteristics, etc.). When persistent heterogeneity among eligible studies exists, a random effects model can be used to analyze the sampling error (variance) and the variance of the research with p < 0.05 and I 2 ≥ 50%44, and estimate the uncertainty of the results by 95% CI, because of the clinical importance of some indices. This calculation model could give a wider CI than the fixed effects model when the heterogeneity is caused by other potential factors.
A fixed effects model with the Mantel-Haenszel method or a random effects model with the DerSimonian-Laird method was applied to calculate the pooled SE, SP, LR+, LR− and DOR with 95% CI based on the level of heterogeneity of the eligible study presenting in forest plots. The sROC curve with 95% CI was established by combining data, which could evaluate the potential association between SE and SP in a metamorphic approach. A value of ½ was added to all cells of studies when data with a zero value appeared.
A subgroup analysis was subsequently assessed in a more homogeneous group according to MFI (≥1.5T versus <1.5T), year of publication (2006 to 2009 versus 2012 to 2016) and MRI sequences (CSs versus CSs + PDWI), which was comprised more than 3 studies. Differences between subgroups were calculated through t test or rank sum test45.
A Deeks’ funnel plot asymmetry test was used with a significance level set at p < 0.05 to predict the existence of publication bias46, which is of great concern for meta-analysis of diagnostic studies.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Anderson, A. F., Dome, D. C., Gautam, S., Awh, M. H. & Rennirt, G. W. Correlation of anthropometric measurements, strength, anterior cruciate ligament size, and intercondylar notch characteristics to sex differences in anterior cruciate ligament tear rates. The American journal of sports medicine 29, 58–66, doi:10.1177/03635465010290011501 (2001).
Irarrazaval, S., Albers, M., Chao, T. & Fu, F. H. Gross, Arthroscopic, and Radiographic Anatomies of the Anterior Cruciate Ligament: Foundations for Anterior Cruciate Ligament Surgery. Clinics in sports medicine 36, 9–23, doi:10.1016/j.csm.2016.08.002 (2017).
Mallett, K. & Arruda, E. M. Digital image correlation-aided mechanical characterization of the anteromedial and posterolateral bundles of the anterior cruciate ligament. Acta biomaterialia. doi:10.1016/j.actbio.2017.03.045 (2017).
Boden, B. P., Sheehan, F. T., Torg, J. S. & Hewett, T. E. Noncontact anterior cruciate ligament injuries: mechanisms and risk factors. The Journal of the American Academy of Orthopaedic Surgeons 18, 520–527 (2010).
Xiao, W. F. et al. Risk factors for noncontact anterior cruciate ligament injury: Analysis of parameters in proximal tibia using anteroposterior radiography. The Journal of international medical research 44, 157–163, doi:10.1177/0300060515604082 (2016).
De Maria, M. et al. Biomechanical correlations of lesions associated with traumatic diseases of the anterior cruciate ligament. Analysis with magnetic resonance. La Radiologia medica 91, 693–699 (1996).
Rossbach, B. P. et al. Indications requiring preoperative magnetic resonance imaging before knee arthroscopy. Archives of medical science: AMS 10, 1147–1152, doi:10.5114/aoms.2014.47825 (2014).
Swain, M. S. et al. Accuracy of clinical tests in the diagnosis of anterior cruciate ligament injury: a systematic review. Chiropractic & manual therapies 22, 25, doi:10.1186/s12998-014-0025-8 (2014).
Khan, H. A. et al. Correlation between magnetic resonance imaging and arthroscopic findings in the knee joint. Trauma monthly 20, e18635, doi:10.5812/traumamon.18635 (2015).
Vassalou, E. E., Klontzas, M. E., Kouvidis, G. K., Matalliotaki, P. I. & Karantanas, A. H. Rotational Knee Laxity in Anterior Cruciate Ligament Deficiency: An Additional Secondary Sign on MRI. AJR. American journal of roentgenology 206, 151–154, doi:10.2214/ajr.15.14816 (2016).
Smith, C. et al. Diagnostic Efficacy of 3-T MRI for Knee Injuries Using Arthroscopy as a Reference Standard: A Meta-Analysis. AJR. American journal of roentgenology 207, 369–377, doi:10.2214/ajr.15.15795 (2016).
Phelan, N., Rowland, P., Galvin, R. & O’Byrne, J. M. A systematic review and meta-analysis of the diagnostic accuracy of MRI for suspected ACL and meniscal tears of the knee. Knee surgery, sports traumatology, arthroscopy: official journal of the ESSKA 24, 1525–1539, doi:10.1007/s00167-015-3861-8 (2015).
Huang, W., Zhang, Y., Yao, Z. & Ma, L. Clinical examination of anterior cruciate ligament rupture: a systematic review and meta-analysis. Acta orthopaedica et traumatologica turcica 50, 22–31, doi:10.3944/aott.2016.14.0283 (2016).
Thomas, S., Pullagura, M., Robinson, E., Cohen, A. & Banaszkiewicz, P. The value of magnetic resonance imaging in our current management of ACL and meniscal injuries. Knee surgery, sports traumatology, arthroscopy: official journal of the ESSKA 15, 533–536, doi:10.1007/s00167-006-0259-7 (2007).
Siddiqui, M. A. et al. Clinical examination vs. MRI: evaluation of diagnostic accuracy in detecting ACL and meniscal injuries in comparison to arthroscopy. Polish orthopedics and traumatology 78, 59–63 (2013).
Schaefer, F. K. et al. Value of fat-suppressed PD-weighted TSE-sequences for detection of anterior and posterior cruciate ligament lesions–comparison to arthroscopy. European journal of radiology 58, 411–415, doi:10.1016/j.ejrad.2005.12.034 (2006).
Rayan, F., Bhonsle, S. & Shukla, D. D. Clinical, MRI, and arthroscopic correlation in meniscal and anterior cruciate ligament injuries. International orthopaedics 33, 129–132, doi:10.1007/s00264-008-0520-4 (2009).
Orlando Junior, N., de Souza Leao, M. G. & de Oliveira, N. H. Diagnosis of knee injuries: comparison of the physical examination and magnetic resonance imaging with the findings from arthroscopy. Revista brasileira de ortopedia 50, 712–719, doi:10.1016/j.rboe.2015.10.007 (2015).
Sampson, M. J. et al. Three Tesla MRI for the diagnosis of meniscal and anterior cruciate ligament pathology: a comparison to arthroscopic findings. Clinical radiology 63, 1106–1111 (2008).
Navali, A. M., Bazavar, M., Mohseni, M. A., Safari, B. & Tabrizi, A. Arthroscopic evaluation of the accuracy of clinical examination versus MRI in diagnosing meniscus tears and cruciate ligament ruptures. Archives of Iranian medicine 16, 229–232, doi:013164/aim.008 (2013).
Lee, C. S., Davis, S. M., McGroder, C., Stetson, W. B. & Powell, S. E. Analysis of Low-Field Magnetic Resonance Imaging Scanners for Evaluation of Knee Pathology Based on Arthroscopy. Orthopaedic journal of sports medicine 1, 2325967113513423, doi:10.1177/2325967113513423 (2013).
Kostov, H., Stojmenski, S. & Kostova, E. Reliability assessment of arthroscopic findings versus MRI in ACL injuries of the knee. Acta Informatica Medica 22, 111–114 (2014).
Khanda, G. E., Akhtar, W., Ahsan, H. & Ahmad, N. Assessment of menisci and ligamentous injuries of the knee on magnetic resonance imaging: correlation with arthroscopy. JPMA. The Journal of the Pakistan Medical Association 58, 537–540 (2008).
Helmark, I. C., Neergaard, K. & Krogsgaard, M. R. Traumatic knee extension deficit (the locked knee): can MRI reduce the need for arthroscopy? Knee surgery, sports traumatology, arthroscopy: official journal of the ESSKA 15, 863–868, doi:10.1007/s00167-006-0244-1 (2007).
Gupta, M. K. et al. MRI evaluation of knee injury with arthroscopic correlation. Journal of Nepal Health Research Council 12, 63–67 (2014).
Grubor, P., Asotic, A., Grubor, M. & Asotic, M. Validity of magnetic resonance imaging in knee injuries. Acta Informatica Medica 21, 200–204 (2013).
Dutka, J., Skowronek, M., Skowronek, P. & Dutka, Ł. Arthroscopic verification of objectivity of the orthopaedic examination and magnetic resonance imaging in intra-articular knee injury. Retrospective study. Wideochirurgia I Inne Techniki Maloinwazyjne 7, 13–18 (2012).
Duc, S. R., Pfirrmann, C. W., Koch, P. P., Zanetti, M. & Hodler, J. Internal knee derangement assessed with 3-minute three-dimensional isovoxel true FISP MR sequence: preliminary study. Radiology 246, 526–535, doi:10.1148/radiol.2462062092 (2008).
De Maio, P., White, L. M., Bleakney, R., Menezes, R. J. & Theodoropoulos, J. Diagnostic accuracy of an iPhone DICOM viewer for the interpretation of magnetic resonance imaging of the knee. Clinical journal of sport medicine: official journal of the Canadian Academy of Sport Medicine 24, 308–314, doi:10.1097/jsm.0000000000000005 (2014).
Challen, J., Tang, Y. M., Hazratwala, K. & Stuckey, S. Accuracy of MRI diagnosis of internal derangement of the knee in a non-specialized tertiary level referral teaching hospital. Australasian Radiology 51, 426–431 (2007).
Chagas-Neto, F. A. et al. Diagnostic performance of 3D TSE MRI versus 2D TSE MRI of the knee at 1.5T, with prompt arthroscopic correlation, in the detection of meniscal and cruciate ligament tears. Radiologia brasileira 49, 69–74, doi:10.1590/0100-3984.2015.0042 (2016).
Bari, A. A., Kashikar, S. V., Lakhkar, B. N. & Ahsan, M. S. Evaluation of MRI versus arthroscopy in anterior cruciate ligament and meniscal injuries. Journal of clinical and diagnostic research: JCDR 8, Rc14–18, doi:10.7860/jcdr/2014/10980.5331 (2014).
Ai, T., Zhang, W., Priddy, N. K. & Li, X. Diagnostic performance of CUBE MRI sequences of the knee compared with conventional MRI. Clinical radiology 67, e58–63, doi:10.1016/j.crad.2012.07.020 (2012).
Ahn, J. H., Jeong, S. H. & Kang, H. W. Risk Factors of False-Negative Magnetic Resonance Imaging Diagnosis for Meniscal Tear Associated With Anterior Cruciate Ligament Tear. Arthroscopy: the journal of arthroscopic & related surgery: official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. doi:10.1016/j.arthro.2015.11.046 (2016).
Tewari, A., Padma, S. & Sundaram, P. S. Single photon emission computed tomography in detection of anterior cruciate ligament tear. Indian journal of nuclear medicine: IJNM: the official journal of the Society of Nuclear Medicine, India 27, 211–212, doi:10.4103/0972-3919.112755 (2012).
Smith, T. O. et al. The diagnostic accuracy of anterior cruciate ligament rupture using magnetic resonance imaging: A meta-analysis. European Journal of Orthopaedic Surgery and Traumatology 22, 315–326, doi:10.1007/s00590-011-0829-3 (2012).
Oei, E. H., Nikken, J. J., Verstijnen, A. C., Ginai, A. Z. & Myriam Hunink, M. G. MR imaging of the menisci and cruciate ligaments: a systematic review. Radiology 226, 837–848, doi:10.1148/radiol.2263011892 (2003).
Crawford, R., Walley, G., Bridgman, S. & Maffulli, N. Magnetic resonance imaging versus arthroscopy in the diagnosis of knee pathology, concentrating on meniscal lesions and ACL tears: a systematic review. British medical bulletin 84, 5–23, doi:10.1093/bmb/ldm022 (2007).
Bossuyt, P. M. et al. The STARD statement for reporting studies of diagnostic accuracy: explanation and elaboration. The Standards for Reporting of Diagnostic Accuracy Group. Croatian medical journal 44, 639–650 (2003).
Liberati, A. et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ (Clinical research ed.) 339, b2700, doi:10.1136/bmj.b2700 (2009).
Whiting, P. F. et al. QUADAS-2: A Revised Tool for the Quality Assessment of Diagnostic Accuracy Studies. Annals of Internal Medicine 155, 529–536, doi:10.7326/0003-4819-155-8-201110180-00009 (2011).
Zamora, J., Abraira, V., Muriel, A., Khan, K. & Coomarasamy, A. Meta-DiSc: a software for meta-analysis of test accuracy data. BMC medical research methodology 6, 31, doi:10.1186/1471-2288-6-31 (2006).
Lijmer, J. G., Bossuyt, P. M. M. & Heisterkamp, S. H. Exploring sources of heterogeneity in systematic reviews of diagnostic tests. Statistics in Medicine 21, 1525–1537, doi:10.1002/sim.1185 (2002).
Wang, N. et al. A systematic review of the diagnostic accuracy of cardiovascular magnetic resonance for pulmonary hypertension. The Canadian journal of cardiology 30, 455–463, doi:10.1016/j.cjca.2013.11.028 (2014).
Altman, D. G. & Bland, J. M. Interaction revisited: the difference between two estimates. BMJ (Clinical research ed.) 326, 219 (2003).
Deeks, J. J., Macaskill, P. & Irwig, L. The performance of tests of publication bias and other sample size effects in systematic reviews of diagnostic test accuracy was assessed. Journal of clinical epidemiology 58, 882–893, doi:10.1016/j.jclinepi.2005.01.016 (2005).
Author information
Authors and Affiliations
Contributions
K.L., J.D., L.X.H. and H.L.Y. designed the research. K.L., J.D., L.N. and T.L. contributed to the study search. K.L. and J.D. screened and selected relevant literature, extracted data and evaluated quality. K.L., J.D. and L.N. analyzed the data. K.L. and J.D. prepared the manuscript. T.L. and H.L.Y. critically revised the manuscript. All authors reviewed and finally approved the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Li, K., Du, J., Huang, LX. et al. The diagnostic accuracy of magnetic resonance imaging for anterior cruciate ligament injury in comparison to arthroscopy: a meta-analysis. Sci Rep 7, 7583 (2017). https://doi.org/10.1038/s41598-017-08133-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-08133-4
This article is cited by
-
Application of machine learning-based multi-sequence MRI radiomics in diagnosing anterior cruciate ligament tears
Journal of Orthopaedic Surgery and Research (2024)
-
A new modified MR dual precision positioning of thin-slice oblique sagittal fat suppression proton density weighted imaging: its diagnostic accuracy in anterior cruciate ligament injury
Scientific Reports (2024)
-
The potential of posterior cruciate ligament buckling phenomenon as a sign for partial anterior cruciate ligament tears
Archives of Orthopaedic and Trauma Surgery (2024)
-
Lightweight Attentive Graph Neural Network with Conditional Random Field for Diagnosis of Anterior Cruciate Ligament Tear
Journal of Imaging Informatics in Medicine (2024)
-
Effective automatic detection of anterior cruciate ligament injury using convolutional neural network with two attention mechanism modules
BMC Medical Imaging (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.