Abstract
Genetic alterations identified in adjacent normal appearing tissue in bladder cancer patients are indicative of a field disease. Here we assessed normal urothelium transformation and intra-tumour heterogeneity (ITH) in four patients with bladder cancer. Exome sequencing identified private acquired mutations in a lymph node metastasis and local recurrences. Deep re-sequencing revealed presence of at least three and four subclones in two patients with multifocal disease, while no demarcation of subclones was identified in the two patients with unifocal disease. Analysis of adjacent normal urothelium showed low frequency mutations in patients with multifocal disease. Expression profiling showed intra-tumour and intra-patient co-existence of basal- and luminal-like tumour regions, and patients with multifocal disease had a greater degree of genomic and transcriptomic ITH, as well as transformation of adjacent normal cells, compared to patients with unifocal disease. Analysis of the adjacent urothelium may pave the way for therapies targeting the field disease.
Similar content being viewed by others
Introduction
Bladder cancer is a common malignant disease, and is the cause of 165.000 cancer related deaths annually1. When developing personalized medicine, it is important to understand the biological disease basis and to study disease evolution in order to guide treatment decisions and increase survival rates. Disease evolution and subclone development are associated with varying degrees of intra-tumour heterogeneity (ITH) in different cancer types2,3,4,5,6,7,8, including bladder cancer9. For administering optimal and rational targeted therapeutics, it is important to identify genomic alterations that arose early in cancer development, and hence are present in all cancer cells10, or e.g. are present in aggressive subclones giving rise to metastatic lesions.
Previous studies have proven that critical subclones may be missed by analysis of bulk tumours3, 4, whereas other studies have shown a more modest level of ITH5, or varying degree of ITH between patients2, 8. Studies in bladder cancer have shown a low level of ITH within single biopsies, but large differences between primary tumours and metastatic lesions9, 11. ITH has been largely overlooked in many studies, and this may be the reason why many biomarkers fail clinical validation12.
Multifocal and recurrent bladder tumours are hypothesized to originate from a bladder field disease13, 14. Studies analysing the adjacent normal appearing urothelium (field disease) have revealed that the urothelium is highly affected by the disease, harbouring genetic alterations shared with the tumours15,16,17,18. Furthermore, recent studies applying full-genome and exome sequencing have documented a clonal relationship between metachronous tumours, supporting the field disease model11, 19. The field disease and clonal relationship between tumours could be caused by intraepithelial migration and/or luminal seeding and implantation of carcinoma cells from existing tumours - eventually giving rise to recurrent tumours. Another explanation could be the transformation of a stem cell embedded in the urothelium followed by clonal expansion13, 14.
To investigate the level of ITH in bladder cancer, and to analyse the extend of mutations observed in adjacent normal urothelial cells we performed multi-regional whole exome sequencing (WES). This was followed by deep targeted sequencing of multiple laser micro-dissected (LMD) cells from tumour regions and normal biopsies from four patients with advanced bladder cancer. Simultaneously, we addressed transcriptional heterogeneity in the LMD regions. We identified varying degrees of mutational ITH, which was further reflected at the transcriptomic level in molecular subtypes. Finally, we observed multiple tumour specific mutations at low frequencies in the adjacent normal samples.
Results
Whole exome sequencing
DNA was extracted from 17 tumour samples and from leucocytes procured from four patients (patients 1 to 4) with advanced bladder cancer, treated with radical cystectomy and lymphadenectomy. Tumours from patients 1 and 2 were multifocal while tumours from patients 3 and 4 were unifocal. Clinical and histopathological details are listed in Supplementary Table S1. We performed WES of tumour DNA and matched leucocyte DNA as germline and obtained a mean read depth of 65x (31x–113x). We identified 232–755 mutations (categories 1–2; see Methods) in the four patients. Of these, 178–497 mutations were predicted to have a functional impact (Supplementary Table S2, see Methods). Analysis of mutations with a predicted functional impact revealed highly variable degree of ITH, and comparisons to a lymph node metastasis/local recurrences demonstrated acquisition of multiple private mutations and potentially novel disease driver mutations (Supplementary Fig. S1). We identified mutations in known cancer driver genes20 and in proposed drivers in bladder cancer21. Mutations in driver genes were identified, both as shared between all bulk exomes within a patient (60–95%), and as private being spatially confined to few or single exomes (5–40%).
Multi-region targeted amplicon sequencing and expression profiling analysis
In order to assess the mutational ITH, we designed two amplicon panels targeting all mutations with a predicted functional impact (n = 1435 and n = 802). These panels were used to sequence DNA procured from multiple LMD regions from the tumour samples initially analysed by WES (n = 129 LMD regions, Supplementary Figs S2–S5), DNA from a lymph node metastasis (n = 1), DNA from local recurrences (n = 2, see Supplementary Table S1), DNA from normal appearing urothelial cells (n = 28), and leucocyte DNA (n = 4). A mean read depth of 3049x (see Supplementary Table 2) was achieved leading to a better assessment of the presence of a mutation and its frequency compared to WES data. For validation purpose the amplicon panels were also used to sequence the bulk samples (n = 17) used for WES. WES identified mutations (categories 1–2) showed a validation rate of 93.3%, while the remaining mutations (category 3) showed a validation rate of 63.7%. Only validated mutations were included in subsequent analyses. Finally, gene expression profiling (Fluidigm) was used to assess basal- and luminal subtypes, cellular differentiation level, and disease aggressiveness22, 23.
Comprehensive analysis of intra tumour heterogeneity in patients 1–4
Patient 1
Patient 1 presented with a T3b tumour (named S1 in Fig. 1a), three Ta tumours (named S2, S3, and S4 in Fig. 1a), and a pelvic lymph node metastasis. We selected 207 mutations inferred from WES and performed targeted amplicon sequencing (mean read depth = 4250 reads) on 33 tumour DNA samples (including bulk biopsies) and 7 LMD samples from the adjacent urothelium. We identified a clonal origin for all analysed tumour regions (Fig. 1a). Cluster analysis defined three clusters with different mutational patterns. As expected based on histopathological features, cluster 1 (C1) comprised all regions originating from the T3b tumour (S1) and the lymph node metastasis; cluster 2 (C2) comprised all regions from one of the Ta tumours (S2) and cluster 3 (C3) comprised all regions from the two remaining Ta tumours (S3 and S4, Fig. 1a). Mutations in known driver genes (the tumour suppressor genes BAP1, MLL2 (also known as KMT2D), CREBBP, EP300, and the oncogene FGFR3) were shared between all samples while additional mutations in other oncogenes (DNMT1 and ERBB2) were found exclusively in the cluster containing muscle invasive tumour regions. Finally, an additional mutation in MLL2 was found only in cluster C2. Transcriptional profiling classified the Ta tumours as luminal (high expression of luminal markers such as GATA3, PPARG, FOXA1 and XBP1 as well as differentiation markers such as UPK1A and KRT20) as well as non-aggressive (high expression of SKAP2, FABP4, MBNL2 and ID1). The muscle invasive tumour, however, showed a basal subtype (higher expression of CDH3, CD44, KRT5 and KRT6A) and likewise high aggressiveness (higher expression of KPNA2, BIRC5, CDC25B, COL4A1, and MSN).
Detailed analysis of patient 1. (a) Upper heat map: Deep targeted sequencing was applied to 28 LMD regions from four tumour samples (one from each of the four tumours), a lymph node metastasis, as well as seven LMD adjacent normal samples. Tumour sample S1 was procured from the muscle invasive tumour (clinical stage T3b) and tumour samples S2–S4 were procured from three non-muscle invasive tumours (clinical stage Ta). Presented are all validated mutations. Furthermore, only mutations present in at least 5% of the tumour regions were included. LMD tumour regions were grouped using unsupervised hierarchical cluster analysis and clusters are indicated above the heat map. Data from normal samples were clustered independently (sample wise). Variants were classified as shared if present in more than 90% of the tumour samples. Oncogenes (red), tumour suppressor genes (blue), and IntOGen bladder cancer drivers (green) are annotated to the right of the heat map. Further, the Qiagen Clinical Insight Software was used to identify variants, for which therapeutics are available (T), in clinical trials (CT), or if the variant is pathogenic (P). Allele frequencies are presented ranging from >0 to 1 (an error rate of 1% was applied, hence if present, the variant is at least present at 1% in the sample). Grey indicates less than 4 alternate reads but an allele frequency greater than or equal to 1%, and could hence potentially be present if read depth was higher. Light blue indicates a failed amplicon. Dark blue equals no mutation. Lower heat map: transcriptomic profiling of corresponding regions presented in the upper heat map. Presented are normalized Ct values of genes of the following gene classes: luminal, differentiation, basal, high progression risk, and low progression risk. ND (grey): not determined. Missing value (white): sample has not been profiled. (b) Normal sample analysis: targeted sequencing of normal samples with a less stringent error correction applied (0.5%). The allele frequencies are presented on a different scale from present (>0) to 5%. (c) Illustration of sampling from cystectomy: see Supplementary Figure S2 for detailed overview of LMD regions.
Targeted amplicon sequencing of the adjacent urothelium showed that some mutations observed in the tumours were present at low frequencies in these samples (range: 1 to 18.8%, median: 2.1%). Especially shared mutations were frequently observed (Fig. 1a) in the normal urothelium compared to private mutations (p value < 0.001, Fischer’s exact test). Following, we applied a less stringent error correction (see Materials and methods) and additional mutations were identified in the adjacent urothelium (Fig. 1b) – especially mutations identified as shared in the tumours. Indeed, some mutations, including a mutation in BAP1, were present in all normal samples.
Accordingly, we observed a clonal relationship between all samples analysed, shared mutations were enriched in adjacent normal samples, and the different multifocal tumours had acquired several private mutations. Interestingly, the inter-tumour differences were reflected in different transcriptional subtypes with basal- and luminal-like characteristics.
Patient 2
Patient 2 presented with multifocal and muscle invasive disease with large parts of the bladder being tumorous (Supplementary Fig. S3 and Fig. 2c). WES was performed on seven tumour samples (S1a, S1b, S1c, S1d, S2, S3, and S4) and on a local recurrence. We selected 538 mutations inferred from WES and performed targeted amplicon sequencing on 71 samples (including bulk samples) and 7 adjacent normal samples (mean read depth = 2567 reads). Here a clonal origin was also observed and cluster analysis revealed four main clusters indicative of four major subclones (Fig. 2a). Cluster 1 (C1) and cluster 4 (C4) were mainly comprised of regions from tumour samples S1c and S1d, respectively. Cluster 2 (C2) was comprised of regions from tumour sample S3 and cluster 3 (C3) was a mix of regions from tumour samples S1a, S1b, S2, S4, and the remaining regions from S3. Mutations in STAG2, PIK3CA, CLTC, and CHEK2 appeared shared between all regions, whereas a mutation in TP53 was shared between all regions except from C1 and appeared only subclonal in C2, as the frequencies were markedly lower in this cluster. However, an additional mutation in TP53 was present only in cluster C1 and C2. ATRX and MLL3 (also known as KMT2C) were mutated in all regions in C3 except regions originating from tumour sample S2. Transcriptional profiling showed that samples in cluster C1 and C4 had luminal-like characteristics and expressed genes associated with low aggressiveness whereas samples in cluster C3 were basal-like and showed higher expression of genes associated with high aggressiveness. Accordingly, the local recurrence clustered within cluster C3 with more aggressive characteristics.
Detailed analysis of patient 2. Deep targeted sequencing was applied to 63 LMD tumour regions procured from multifocal tumour samples (4 samples from tumour 1 and one sample from each of tumour 2–4) as well as a sample from a local recurrence. Further, deep sequencing was applied to seven normal samples. The figure is annotated as Fig. 1. See Supplementary Figure S3 for detailed overview of LMD regions.
Targeted sequencing of adjacent normal samples revealed that some of the mutations observed in the tumours were present at low frequencies (range: 1 to 31%, median: 3.3%; Fig. 2a). Again, mutations identified as shared in the tumour were significantly more often identified in the normal samples compared to private mutations (p value < 0.001, Fisher’s exact test). Applying less stringent error correction to data from normal samples showed additional mutations identified as shared in the tumours. No mutations were identified in all normal samples in this patient.
Consequently, we observed a clonal relationship of all tumour regions and the subclones observed were not directly associated with physical location in the bladder. Also in this case, mutations identified as shared in the tumours were enriched in the surrounding normal samples, and differences at the genomic level were reflected at the transcriptomic level.
Patient 3 and patient 4
Patients 3 and 4 presented with unifocal tumours, and cluster analysis did not separate samples into major subclones in these two patients (Fig. 3a,b). Both patients had tumours with numerous mutations in known driver genes. The lack of genomic ITH was further reflected at the transcriptomic level where patient 3 showed a basal-like subtype and high aggressiveness in all regions from all four tumour biopsies and patient 4 showed a non-aggressive luminal-like subtype in all regions from both tumour biopsies. Few mutations were observed in the adjacent normal samples from these patients except from sample N1 in patient 4, which showed presence of most of the tumour specific mutations (Fig. 3a,b). Applying less stringent error correction did not reveal presence additional tumour specific mutations in the normal samples (data not shown).
Detailed analysis of patient 3 and patient 4. (a) Patient 3. Deep targeted sequencing was applied to 28 LMD regions from four tumour samples taken from one large unifocal tumour, a sample from a local recurrence, as well as five normal samples. (b) Patient 4. Deep targeted sequencing was applied to 10 LMD regions from two tumour samples from a unifocal tumour as well as nine normal samples. (c) Illustration of sampling from cystectomy for patient 3: see Supplementary Figure S4 for detailed overview of LMD regions. (d) Illustration of sampling from cystectomy for patient 4: see Supplementary Figure S5 for detailed overview of LMD regions. The figure is annotated as Fig. 1.
Consequently, a clonal relationship was observed for all samples analysed, but no major subclones were observed at the genomic or transcriptomic level. Hence the two patients presented with low spatial ITH, and the adjacent urothelium showed little evidence of field disease (apart from sample N1 in patient 4), which reflects the unifocal disease presentation observed in these two patients.
Identification of potential therapeutic targets
Finally, we annotated possible therapeutic targets in order to retrospectively look into the possibilities for administering “precision medicine”. Potential therapeutic targets (with FDA approved drugs available or drugs in clinical trials) were identified and a full list can be seen in Supplementary Table S3. A shared FGFR3 activating mutation was found in patient 1 and could potentially be targeted by FGFR inhibitors. Another mutation in ERBB2 found in the muscle invasive tumour (S1) could be a treatment target for the more aggressive subclone. For patient 2, mutations in PIK3CA and CHEK2 were identified in all tumour regions and may be potential therapeutic targets (drugs are still being tested in clinical trials). In patients 3 and 4, numerous mutations were potential therapeutic targets, though only few were identified in all tumour regions. In the case of patient 3, AKT1S1 was altered in all regions but one, indicating possible benefit of Everolimus. Finally, in patient 4, a mutation in TOP2B identified in all tumour regions could indicate that the patient would benefit from treatment with a topoisomerase inhibitor and another mutation in HSP90AA1 (also identified in all tumour regions) could possibly lead to a better response to anthracyclines and cisplatin.
Discussion
Here we report a comprehensive multi-regional analysis and an in-depth characterization of the heterogeneity in advanced bladder cancer in four patients. The genomic ITH was reflected at the transcriptomic level, revealing intra-patient differences in luminal- and basal-like subtypes and aggressiveness signatures. In addition, we found that some mutations mainly observed as shared in the tumours from patients with multifocal disease were also observed at low frequencies in the adjacent urothelium. Previously, a comparison of genomic and transcriptomic data obtained from tumour subpopulations procured by FACS from a single patient has been reported24.
Our analysis showed a clonal origin for all tumour regions in four patients with unifocal and multifocal advanced bladder cancer. Furthermore, patients with multifocal disease showed presence of subclonal evolution (three to four subclones), while patients with unifocal disease showed no subclonal diversification. This is in concordance with earlier studies of bladder tumours, where paired tumours have been analysed and few subclones were identified11, 19 and where multi-regional sequencing was performed9. A study applying single cell sequencing of a single bladder tumour also showed the presence of few subclones25. Whether the study applying single cell sequencing would have revealed a higher number of subclones if single cells from multi-regional biopsies had been analysed is unknown. In the present approach, we performed targeted amplicon sequencing based on mutations identified from WES. Consequently, our analysis is limited to the most frequent subclones detected at the obtained sequencing depth, and we may underestimate the number of subclones present. Future studies of additional patients are needed where small regions or preferable single cells are sequenced using e.g. whole exome or whole genome approaches to decipher the ITH further.
The level of ITH showed large differences between the four patients. Tumours from all patients showed presence of both shared and private mutations in driver genes. Patient 2 showed the highest degree of ITH, as four clusters were observed, with mutations in known disease drivers being subclonal. Whether some mutations in disease driver genes tend to be significantly more shared or private requires analyses of a large cohort and can therefore not be assessed in our study. Patient 3 and 4, on the other hand, showed a lower degree of ITH and clustering did not reveal any demarcation of subclones. The study by Zhang et al. showed that patients with lung adenocarcinomas with poor outcome had high ITH5. Whether the level of ITH in bladder cancer may serve as a prognostic marker requires further studies of larger patient cohorts.
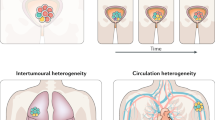
Synchronous tumours in patient 1 showed acquisition of private mutations in concordance with a previous study26. Furthermore, the urothelium revealed presence of numerous mutations at low frequencies initially identified in the tumours. Hence, the mutations do not appear to be shared between all cells in the normal samples. This may be explained either by the presence of normal healthy cells or by a mix of different transformed cells. Of the mutations identified in the normal samples, a significantly higher number of the mutations were classified as shared rather than private in the tumours (Fig. 1). Previous studies have shown genomic alterations (mutations or loss of RB1 or TP53 as well as copy number alterations of chromosome 9, 13 and 17) in the normal urothelium in cystectomy specimens15,16,17, 27,28,29. These studies relied on technologies, which would not have detected mutations of low frequencies as in our analyses. We here suggest that the earlier studies identified early common events (e.g. loss of 9p or 9q or mutations in TP53) occurring in an urothelial stem cell and giving rise to a clonal population of cells, each acquiring a unique set of mutations followed by parallel expansion. This may result in multiple clonally related intermixed transformed fields. Tumours arising from a given field will harbour clonal variants mirroring the field from which it arose. The multiple field hypothesis (see Fig. 4c) explains the presence of low frequency mutations in the pre-neoplastic cells, as other fields are overlapping with different mutations. This theory is adapted from the big bang model in early stage colorectal cancer development30 and the theory of punctuated equilibrium31. The big bang model proposes that multiple molecular events takes place at an early time point, resulting in intermixed cellular subclones and similarly, the theory of punctuated equilibrium proposes punctuations or burst of genetic events intervened by stasis. A recent report applying single cell sequencing on triple negative breast cancers showed punctuated equilibrium in copy number evolution32. To confirm our hypothesis, deep WES of samples from the urothelium may be applied to reveal the presence of other field mutations not detected in the tumours. Another approach could be single cell sequencing including both copy number analysis and genome or exome sequencing as previously described33. Alternatively, the presence of low frequency mutations in the normal samples could also be derived from intra-epithelial migration (Fig. 4a), where carcinoma cells migrate in the urothelium giving rise to low frequent mutations due to presence of normal healthy cells, or from luminal seeding of carcinoma cells (Fig. 4b). However, intra-epithelial migration would require carcinoma cells to undergo epithelial-to-mesenchymal transition, and luminal seeding would require shredding of carcinoma cells, followed by implantation. Both events are considered molecularly complex13. Furthermore, to reflect the low frequencies of mutations that we observe in the normal urothelial samples, intra-epithelial migration and luminal seeding should be associated with little or no expansion of the tumour clones for the frequencies to remain low.
Models of field disease development in bladder cancer. (a) Intra-epithelial migration of multiple subclones gives rise to tumours of a clonal origin and presence of variants throughout the urothelium. (b) Luminal seeding followed by implantation gives rise to tumours of clonal origin. (c) Acquisition genetic alterations such as loss of 9p or 9q or mutation in TP53 in an urothelial stem cell generates a pool of cancer stem cells of a clonal origin. Due to the increased proliferation, numerous mutations are acquired in an initial burst followed by intermixing and parallel expansion throughout the urothelium. This model gives rise to multiple fields.
Gene expression subtypes have prognostic potential and may have clinical utility34,35,36,37. Here we showed that although different parts of a tumour are clonally related, ITH in molecular subtypes exists. Tumours of basal- and luminal-like subtypes have been proposed to arise from distinct uro-progenitors38. Our data may question this hypothesis as both molecular subtypes were identified within the same tumour (patient 2) and between clonally related tumours within a single patient (patient 1). Our data could indicate the presence of cell plasticity rather than intrinsic/inherited subtypes. Further analysis should be performed to investigate which molecular changes may mediate this possible subtype switch. Our assessment of molecular subtypes is based on selected genes defining basal and luminal subtypes only while many subtypes have been identified in MIBC39. ITH associated with molecular subtypes should be considered if e.g. basal- and luminal-like subtypes are used for administering therapeutic treatment in future clinical trials40, 41.
Aspects of personalized medicine were further assessed in light of ITH. The analysis was limited to mutations proposed targetable by the Qiagen Clinical Insight software (Supplementary Table S3). Targets identified in all analysed regions were identified in all four patients indicative of treatment with targeted therapies as well as chemotherapeutics. It is possible, that multiple pathways should be targeted simultaneously to obtain tumour regression as recently shown in a patient with anaplastic thyroid cancer42. Shared mutations in patients 1 and 2 could potentially be targeted to eradicate the underlying field disease – patient 1 presents with a shared BAP1 mutation between the four tumours and BAP1 is mutated in all samples from the urothelium. A recent report indicates that mesothelioma cells with inactivated BAP1 are sensitive to EZH2 inhibition (epigenetic inhibitor)43. Patient 4 further showed a strong luminal-like subtype. Preliminary analysis has indicated a link between molecular subtypes of bladder cancer and response to PD-L1 inhibition, where patients with luminal tumours showed better response to PD-L1 inhibition44 pinpointing the importance of performing multi-regional subtyping. This study further sheds light on potential therapeutic targets in patients with advanced bladder cancer, and indicates possible treatment of pre-neoplastic cells surrounding the tumours.
Methods
Clinical samples
Patients included in the study where treated at Aarhus University Hospital in 2014. The patients underwent open radical cystectomy and extended lymph node dissection to the aortic bifurcation. All patients were cystectomised because of primary bladder cancer without neoadjuvant chemotherapy or radiation therapy. None of the patients had previously been diagnosed with bladder cancer. Biopsies from cystectomies were obtained, embedded in TissueTek OCTTM Compound (Sakura, Finetek, Vaerloese, Denmark), snap frozen in liquid nitrogen, and placed at −80 °C. Two to seven biopsies were obtained from tumours from each patient along with six to 12 samples throughout the surrounding urothelium. Formalin Fixed and Paraffin Embedded (FFPE) specimens from a lymph node metastasis and local recurrences were obtained from Department of Pathology, Aarhus University Hospital. Blood samples were stored at −80 °C in EDTA tubes. All patients gave their informed written consent and the Danish National Committees on Heath Research Ethics (#1300174) approved the study and experimental protocols. The methods in the study were carried out in accordance with the approved guidelines and regulations. Detailed information on DNA and RNA extraction is described in Supplementary Data.
Library construction and WES
WES was performed using either the Kapa Hyper Library Prep Kit (KapaBiosystems, Wilmington, MA, USA) for library construction followed by exome capture using Nimblegen SeqCap EZ Exome v3.0 Capture Kit (Roche) or the Nextera Rapid Capture Expanded Exome Kit (Illumina, San Diego, CA, USA). Input for the Kapa Hyper Library Prep was 1 µg of gDNA and input for the Nextera Rapid Capture was 50 ng of gDNA. Libraries were sequenced using the Illumina HiSeq 2000 or the NextSeq 500 platforms. WES was performed on bulk DNA from cross sections from each biopsy. The Kapa Hyper Library Prep kit was used for DNA procured from FFPE. When both library kits were used for a single patient, only overlapping genomic regions were investigated. For patient 1 libraries were constructed using pools of bulk DNA from cross sections (S1 + S2 and S3 + S4).
Alignment, mapping, and variant calling
Sequence data were aligned, mapped, and variants called as previously described11 – see Supplementary Data. Furthermore, variants were sorted into categories based on the confidence of the call and tiers based on their estimated functional impact as previously described11. In short, categories were based on Mutect scores, presence of the alternate allele in the germline, and the frequency of the variant. The estimated impact on the encoded protein was derived using snpEff45 with tier 0 encompassing nonsense variants, tier 1 encompassing non-synonymous variants, and tier 2 encompassing synonymous variants.
Targeted sequencing
Two TruSeq Custom Amplicon (TSCA) panels (Illumina) were designed for targeted re-sequencing of DNA from LMD regions based on variants identified from WES. We included all variants estimated to have functional impact by including all tier 0–1 variants with maximum one alternate allele detected in the germline to exclude sequencing errors (see Alignment, mapping, and variant calling). Additionally, if oncogenes or tumour suppressor genes20 were mutated, these were included in the amplicon panel disregarding functional impact estimation. This resulted in a small amplicon panel containing 207 mutations from patient 1 and 595 mutations from patient 3 and a large panel containing 538 mutations from patient 2 and 897 mutations from patient 4. TSCA libraries were constructed using the Illumina TruSeq Custom Amplicon v1.5 chemistry. Libraries were sequenced using the NextSeq 500 or the MiSeq platforms. Reads were stripped for adapters using ReadAdaptorTrimmer and mapped with BWA mem without further processing of the alignment.
NGS error correction
Error rates for the targeted amplicon sequencing were calculated for each amplicon panel. As mutations identified from two patients were included in each amplicon panel, all amplicons designed for mutations in one patient were wildtype when investigating data for the other patient. For this analysis, we removed amplicons, which showed presence of the alternate allele in the blood and further removed the upper quartile of data from read depth. This was done, as few amplicons sometimes generate vast amounts of reads and could potentially be more error prone. We determined error rates for each type of nucleotide change and the highest rate was then multiplied by three. Analysis of samples from the surrounding urothelium was also investigated with the error rate multiplied by only 1.5.
Fluidigm gene expression profiling
Expression profiling of RNA procured from LMD regions was performed using the Fluidigm 48.48 qPCR Dynamic Array microfluidic chips (Fluidigm/AH Diagnostics, Aarhus, Denmark). Detailed information is provided in Supplementary Data.
Statistical analysis
Fischer’s exact test was used to test for statistical significance between shared and private mutations present in adjacent urothelium samples.
Data availability
WES data is available via European Genome-phenome Archive (EGAC00001000145). All other data are available from the corresponding author upon request.
References
Antoni, S. et al. Bladder Cancer Incidence and Mortality: A Global Overview and Recent Trends. European urology 71, 96–108, doi:10.1016/j.eururo.2016.06.010 (2017).
de Bruin, E. C. et al. Spatial and temporal diversity in genomic instability processes defines lung cancer evolution. Science 346, 251–256, doi:10.1126/science.1253462 (2014).
Gerlinger, M. et al. Genomic architecture and evolution of clear cell renal cell carcinomas defined by multiregion sequencing. Nature genetics 46, 225–233, doi:10.1038/ng.2891 (2014).
Gerlinger, M. et al. Intratumor heterogeneity and branched evolution revealed by multiregion sequencing. The New England journal of medicine 366, 883–892, doi:10.1056/NEJMoa1113205 (2012).
Zhang, J. et al. Intratumor heterogeneity in localized lung adenocarcinomas delineated by multiregion sequencing. Science (New York, NY) 346, 256–259, doi:10.1126/science.1256930 (2014).
Harbst, K. et al. Multiregion Whole-Exome Sequencing Uncovers the Genetic Evolution and Mutational Heterogeneity of Early-Stage Metastatic Melanoma. Cancer research 76, 4765–4774, doi:10.1158/0008-5472.can-15-3476 (2016).
Haffner, M. C. et al. Tracking the clonal origin of lethal prostate cancer. The Journal of clinical investigation 123, 4918–4922, doi:10.1172/jci70354 (2013).
Bashashati, A. et al. Distinct evolutionary trajectories of primary high-grade serous ovarian cancers revealed through spatial mutational profiling. The Journal of pathology 231, 21–34, doi:10.1002/path.4230 (2013).
Thomsen, M. B. et al. Spatial and temporal clonal evolution during development of metastatic urothelial carcinoma. Mol Oncol 10, 1450–1460, doi:10.1016/j.molonc.2016.08.003 (2016).
Yap, T. A., Gerlinger, M., Futreal, P. A., Pusztai, L. & Swanton, C. Intratumor heterogeneity: seeing the wood for the trees. Science translational medicine 4, 127ps110, doi:10.1126/scitranslmed.3003854 (2012).
Lamy, P. et al. Paired Exome Analysis Reveals Clonal Evolution and Potential Therapeutic Targets in Urothelial Carcinoma. Cancer research 76, 5894–5906, doi:10.1158/0008-5472.CAN-16-0436 (2016).
Lee, A. J. & Swanton, C. Tumour heterogeneity and drug resistance: personalising cancer medicine through functional genomics. Biochemical pharmacology 83, 1013–1020, doi:10.1016/j.bcp.2011.12.008 (2012).
Hoglund, M. On the origin of syn- and metachronous urothelial carcinomas. European urology 51, 1185-1193; discussion 1193, doi:10.1016/j.eururo.2006.11.025 (2007).
Hoglund, M. Bladder cancer, a two phased disease? Seminars in cancer biology 17, 225–232, doi:10.1016/j.semcancer.2006.02.002 (2007).
Chaturvedi, V. et al. Superimposed histologic and genetic mapping of chromosome 17 alterations in human urinary bladder neoplasia. Oncogene 14, 2059–2070, doi:10.1038/sj.onc.1201044 (1997).
Czerniak, B. et al. Superimposed histologic and genetic mapping of chromosome 9 in progression of human urinary bladder neoplasia: implications for a genetic model of multistep urothelial carcinogenesis and early detection of urinary bladder cancer. Oncogene 18, 1185–1196, doi:10.1038/sj.onc.1202385 (1999).
Czerniak, B. et al. Genetic modeling of human urinary bladder carcinogenesis. Genes, chromosomes & cancer 27, 392–402 (2000).
Lee, S. et al. Forerunner genes contiguous to RB1 contribute to the development of in situ neoplasia. Proceedings of the National Academy of Sciences of the United States of America 104, 13732–13737, doi:10.1073/pnas.0701771104 (2007).
Nordentoft, I. et al. Mutational context and diverse clonal development in early and late bladder cancer. Cell reports 7, 1649–1663, doi:10.1016/j.celrep.2014.04.038 (2014).
Vogelstein, B. et al. Cancer genome landscapes. Science 339, 1546–1558, doi:10.1126/science.1235122 (2013).
Rubio-Perez, C. et al. In silico prescription of anticancer drugs to cohorts of 28 tumor types reveals targeting opportunities. Cancer Cell 27, 382–396, doi:10.1016/j.ccell.2015.02.007 (2015).
Damrauer, J. S. et al. Intrinsic subtypes of high-grade bladder cancer reflect the hallmarks of breast cancer biology. Proceedings of the National Academy of Sciences of the United States of America 111, 3110–3115, doi:10.1073/pnas.1318376111 (2014).
Dyrskjot, L. et al. Gene expression signatures predict outcome in non-muscle-invasive bladder carcinoma: a multicenter validation study. Clinical cancer research: an official journal of the American Association for Cancer Research 13, 3545–3551, doi:10.1158/1078-0432.ccr-06-2940 (2007).
Prado, K., Zhang, K. X., Pellegrini, M. & Chin, A. I. Sequencing of cancer cell subpopulations identifies micrometastases in a bladder cancer patient. Oncotarget 8, 45619–45625, doi:10.18632/oncotarget.17312 (2017).
Li, Y. et al. Single-cell sequencing analysis characterizes common and cell-lineage-specific mutations in a muscle-invasive bladder cancer. GigaScience 1, 12, doi:10.1186/2047-217x-1-12 (2012).
Acar, O. et al. Determining the origin of synchronous multifocal bladder cancer by exome sequencing. BMC cancer 15, 871, doi:10.1186/s12885-015-1859-8 (2015).
Kram, A. et al. Mapping and genome sequence analysis of chromosome 5 regions involved in bladder cancer progression. Laboratory investigation; a journal of technical methods and pathology 81, 1039–1048 (2001).
Majewski, T. et al. Understanding the development of human bladder cancer by using a whole-organ genomic mapping strategy. Laboratory investigation; a journal of technical methods and pathology 88, 694–721, doi:10.1038/labinvest.2008.27 (2008).
Yoon, D. S. et al. Genetic mapping and DNA sequence-based analysis of deleted regions on chromosome 16 involved in progression of bladder cancer from occult preneoplastic conditions to invasive disease. Oncogene 20, 5005–5014, doi:10.1038/sj.onc.1204612 (2001).
Sottoriva, A. et al. A Big Bang model of human colorectal tumor growth. Nature genetics 47, 209–216, doi:10.1038/ng.3214 (2015).
Cross, W., Graham, T. A. & Wright, N. A. New paradigms in clonal evolution: punctuated equilibrium in cancer. The Journal of pathology 240, 126–136, doi:10.1002/path.4757 (2016).
Gao, R. et al. Punctuated copy number evolution and clonal stasis in triple-negative breast cancer. Nature genetics 48, 1119–1130, doi:10.1038/ng.3641 (2016).
Hou, Y. et al. Single-cell triple omics sequencing reveals genetic, epigenetic, and transcriptomic heterogeneity in hepatocellular carcinomas. Cell research 26, 304–319, doi:10.1038/cr.2016.23 (2016).
Choi, W. et al. Identification of distinct basal and luminal subtypes of muscle-invasive bladder cancer with different sensitivities to frontline chemotherapy. Cancer Cell 25, 152–165, doi:10.1016/j.ccr.2014.01.009 (2014).
Hedegaard, J. et al. Comprehensive Transcriptional Analysis of Early-Stage Urothelial Carcinoma. Cancer cell, doi:10.1016/j.ccell.2016.05.004 (2016).
TCGA. Comprehensive molecular characterization of urothelial bladder carcinoma. Nature 507, 315-322, doi:10.1038/nature12965 (2014).
Sjodahl, G. et al. A molecular taxonomy for urothelial carcinoma. Clinical cancer research: an official journal of the American Association for Cancer Research 18, 3377–3386, doi:10.1158/1078-0432.CCR-12-0077-T (2012).
Czerniak, B., Dinney, C. & McConkey, D. Origins of Bladder Cancer. Annual review of pathology 11, 149–174, doi:10.1146/annurev-pathol-012513-104703 (2016).
Sjodahl, G., Eriksson, P., Liedberg, F. & Hoglund, M. Molecular classification of urothelial carcinoma: global mRNA classification versus tumour-cell phenotype classification. The Journal of pathology, doi:10.1002/path.4886 (2017).
Rebouissou, S. et al. EGFR as a potential therapeutic target for a subset of muscle-invasive bladder cancers presenting a basal-like phenotype. Science translational medicine 6, 244ra291, doi:10.1126/scitranslmed.3008970 (2014).
Biton, A. et al. Independent component analysis uncovers the landscape of the bladder tumor transcriptome and reveals insights into luminal and basal subtypes. Cell reports 9, 1235–1245, doi:10.1016/j.celrep.2014.10.035 (2014).
Gibson, W. J. et al. Genomic heterogeneity and exceptional response to dual pathway inhibition in anaplastic thyroid cancer. Clinical cancer research: an official journal of the American Association for Cancer Research, doi:10.1158/1078-0432.ccr-16-2154-t (2016).
LaFave, L. M. et al. Loss of BAP1 function leads to EZH2-dependent transformation. Nature medicine 21, 1344–1349, doi:10.1038/nm.3947 (2015).
Rosenberg, J. E. et al. Atezolizumab in patients with locally advanced and metastatic urothelial carcinoma who have progressed following treatment with platinum-based chemotherapy: a single-arm, multicentre, phase 2 trial. Lancet (London, England) 387, 1909–1920, doi:10.1016/s0140-6736(16)00561-4 (2016).
Cingolani, P. et al. A program for annotating and predicting the effects of single nucleotide polymorphisms, SnpEff: SNPs in the genome of Drosophila melanogaster strain w1118; iso-2; iso-3. Fly (Austin) 6, 80–92, doi:10.4161/fly.19695 (2012).
Acknowledgements
This work was funded by the Danish Cancer Research Foundation, the Danish Cancer Society, and the Danish Cancer Biobank (grant numbers are not applicable). We thank Mattias Höglund for constructive comments and feedback.
Author information
Authors and Affiliations
Contributions
M.B.H.T., C.K.M., and J.B.J. collected patient material. J.B.J. and S.H. performed clinical follow up and pathology evaluation. M.B.H.T. performed LMD experiments and L.R. assisted in gene expression experiments. M.B.H.T., P.L. and S.V. performed bioinformatic analysis. L.D., T.F.Ø., I.N., P.L. and M.B.H.T. designed the study, and interpreted data. M.B.H.T. and L.D. wrote the paper with input from all authors.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Thomsen, M.B.H., Nordentoft, I., Lamy, P. et al. Comprehensive multiregional analysis of molecular heterogeneity in bladder cancer. Sci Rep 7, 11702 (2017). https://doi.org/10.1038/s41598-017-11291-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-11291-0
This article is cited by
-
Urine-derived bladder cancer organoids (urinoids) as a tool for cancer longitudinal response monitoring and therapy adaptation
British Journal of Cancer (2024)
-
The evolution of metastatic upper tract urothelial carcinoma through genomic-transcriptomic and single-cell protein markers analysis
Nature Communications (2024)
-
Nondestructive protein sampling with electroporation facilitates profiling of spatial differential protein expression in breast tumors in vivo
Scientific Reports (2022)
-
Cadherin switches during epithelial-mesenchymal transition: CDH4/RCAD downregulation reduces bladder cancer progression
Cellular Oncology (2022)
-
A four-antibody immunohistochemical panel can distinguish clinico-pathological clusters of urothelial carcinoma and reveals high concordance between primary tumor and lymph node metastases
Virchows Archiv (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.