Abstract
Antimicrobial resistance (AMR) in Neisseria gonorrhoeae is common, compromising gonorrhoea treatment internationally. Rapid characterisation of AMR strains could ensure appropriate and personalised treatment, and support identification and investigation of gonorrhoea outbreaks in nearly real-time. Whole-genome sequencing is ideal for investigation of emergence and dissemination of AMR determinants, predicting AMR, in the gonococcal population and spread of AMR strains in the human population. The novel, rapid and revolutionary long-read sequencer MinION is a small hand-held device that generates bacterial genomes within one day. However, accuracy of MinION reads has been suboptimal for many objectives and the MinION has not been evaluated for gonococci. In this first MinION study for gonococci, we show that MinION-derived sequences analysed with existing open-access, web-based sequence analysis tools are not sufficiently accurate to identify key gonococcal AMR determinants. Nevertheless, using an in house-developed CLC Genomics Workbench including de novo assembly and optimised BLAST algorithms, we show that 2D ONT-derived sequences can be used for accurate prediction of decreased susceptibility or resistance to recommended antimicrobials in gonococcal isolates. We also show that the 2D ONT-derived sequences are useful for rapid phylogenomic-based molecular epidemiological investigations, and, in hybrid assemblies with Illumina sequences, for producing contiguous assemblies and finished reference genomes.
Similar content being viewed by others
Introduction
Gonorrhoea is a sexually transmitted infection caused by Neisseria gonorrhoeae (gonococcus). In 2012, the World Health Organization (WHO) estimated that there were 78 million new gonorrhoea cases worldwide1, which can cause serious reproductive tract complications2,3,4. Resistance to ceftriaxone and azithromycin in N. gonorrhoeae threatens the recommended dual antimicrobial therapy (last remaining option for empiric therapy), mainly ceftriaxone 250–500 mg plus azithromycin 1–2 g, and no new therapeutic antimicrobials are available4,5,6,7,8,9,10,11,12,13,14,15. WHO included N. gonorrhoeae in its first list of AMR “priority pathogens” in 20178,16. Timely detection and surveillance of AMR gonococcal strains, their AMR determinants and their emergence and dissemination in the populations globally are crucial5,6,7,8,11,17,18,19.
Next generation sequencing (NGS) is ideal for the elucidation of the molecular determinants of AMR, their dissemination throughout the gonococcal population, and the emergence and dissemination of AMR strains in the human population, nationally and internationally20,21. Third-generation sequencing (TGS)22 has benefits such as increased read length, reduction of sequencing time and reduction of sequencing bias introduced by PCR amplification steps23. Individual DNA molecules can also be sequenced by monitoring their transfer through various types of pores24,25, which can potentially result in very long and unbiased sequence reads, because no amplification or chemical reactions are used for the sequencing26. Oxford Nanopore Technologies (ONT) (Oxford, UK) have introduced this approach with their single-molecule nanopore genome sequencing device MinION, a TGS platform with unique technology that was commercialized in mid-201526,27,28,29,30. When both strands are sequenced, a consensus sequence of the molecule can be produced; these consensus reads are termed two-directional reads (1D2 or 2D ONT reads) and generally have higher accuracy than reads from only a single pass of the molecule (1D ONT reads). The MinION provides several new advantages: small size (10 × 3 × 2 cm), portability, speed, low cost, and direct connection to a laptop through a USB 3.0 interface; the library construction involves simplified methods; no amplification step is required, and data acquisition and analysis occur in real time. The MinION is promising for microbiological applications including describing the microbiome31, rapid diagnostics32, transmission and surveillance33,34, de novo assemblies35,36,37, and microbial AMR profiling38,39. However, the high error rate for the MinION sequencer27,28 has limited its ability to compete with existing sequencing technologies and the MinION has not been previously evaluated for gonococci.
We evaluated the performance characteristics, ideal sequence analysis (tools and workflow for taxonomy, assembly, assembly improvement (“polishing”) and mapping), phylogenomic analysis, and prediction of decreased susceptibility or resistance to recommended therapeutic antimicrobials in N. gonorrhoeae isolates using the Oxford Nanopore MinION sequencer. We sequenced the 2016 WHO gonococcal reference genomes/strains40 and clinical gonococcal isolates, and evaluated the performance of ONT assemblies and hybrid assemblies including both ONT and Illumina reads. The assemblies were evaluated against the PacBio RS II-sequenced 2016 WHO gonococcal reference genomes (Bioproject PRJEB14020)40 for sequence variation and to assess whether the assemblies were of sufficient quality for characterisation of AMR determinants and phylogenomic-based molecular epidemiology of gonococci.
Methods
N. gonorrhoeae isolates, culture, antimicrobial susceptibility testing and DNA isolation
Twenty-eight gonococcal isolates, including the previously PacBio-sequenced 2016 WHO reference strains (n = 14)40,41 and 14 clinical isolates, were examined. The clinical isolates were selected from 140 isolates from the RaDAR-Go project, Switzerland, in 2015-201642. Selection was based on having decreased susceptibility or resistance to ceftriaxone and/or cefixime, resistance to azithromycin or ciprofloxacin, and to represent different AMR phenotypes. All clinical isolates were cultured as part of routine diagnostics, and no human clinical samples or information enabling patient identification was available for this study, so ethical approval was not required. All strains were subsequently cultivated and preserved as described43. We determined minimum inhibitory concentrations (MICs) of ceftriaxone, cefixime, azithromycin, spectinomycin, ciprofloxacin, tetracycline, and benzylpenicillin using the Etest (bioMérieux). Resistance breakpoints from the European Committee on Antimicrobial Susceptibility Testing (EUCAST; www.eucast.org/clinical_breakpoints/) were applied. Nitrocefin test (Thermo Fisher Scientific, Wilmington, DE, USA) was used to detect β-lactamase production. Genomic DNA was isolated using the Wizard Genomic DNA Purification Kit (Promega Corporation, Madison, WI, USA). Isolated DNA was quality controlled using fluorometric quantification (Qubit; Thermo Fisher Scientific) and electrophoresis (Tapestation; Agilent, Santa Clara, CA, USA).
Oxford Nanopore Technologies library preparation and MinION sequencing
Three µg of genomic DNA was sheared to an average fragment length of 8 kb with g-TUBES (Covaris, Woburn, WA, USA). Sequencing libraries were prepared according to the 2D library preparation protocol with the SQK-LSK208 2D ligation kit (Oxford Nanopore Technologies), including the DNA repair step with the NEBNext FFPE DNA repair module (New England Biolabs, Ipswich, MA, USA). The sequencing libraries were purified using MyOne C1 beads (Thermo Fisher Scientific), and 6 μl of sequencing library were loaded onto a R9.4 SpotON flow cell and sequenced with the MinION Mk 1B sequencing device (Oxford Nanopore Technologies) for 24 hours, including a top-up with additional 6 µl of DNA library after the first 6 hours of the sequencing run. Base-calling was performed using the Metrichor cloud software and all ONT reads (quality passed 1D and 2D) as well as only 2D ONT reads were then extracted using Poretools44 for downstream analysis.
Illumina library preparation and sequencing
The sequencing libraries for all clinical isolates (n = 14) were prepared using Nextera XT DNA library preparation kit (Illumina, San Diego, CA, USA) and sequenced on the MiSeq Platform (Illumina), according to manufacturer’s instructions, resulting in an average of 967,369 reads with an average read length of 257 bp after quality control and average coverage of 86.5× per base. The raw sequence files for the 2016 WHO gonococcal reference strains40 were obtained from the European Nucleotide Archive (ENA; Bioproject PRJEB14020). The 2D ONT reads and Illumina reads were species confirmed using the online tool One Codex (www.onecodex.com). All sequenced reads are available from the European Nucleotide Archive with the following accession number: PRJEB25703.
Assembly and assessment
To identify the ideal tool for obtaining a high quality de novo assembly using only ONT reads, we evaluated Canu (v1.6)45, Miniasm (vr122)46, PBcR (v8.3)47, and SMARTdenovo (available from https://github.com/ruanjue/smartdenovo) for assembly of all ONT reads (1D and 2D) and only the extracted 2D ONT reads. Canu was executed with default parameters including error correction and –genomesize 2.2M. Miniasm was run with default parameters. PBcR was executed with the following parameters: -length 500, -partitions 200 and –genomeSize = 2200000. SMARTdenovo was run with default parameters and –c 1 to run consensus step. Subsequently, hybridSPAdes (v3.11.1)48 and MaSuRCA (v3.2.2)49 were used separately to produce hybrid assemblies by including paired-end Illumina reads in the assembly process. hybridSPAdes was executed with the careful option and –nanopore command. MaSuRCA was performed using the following parameters: GRAPH_KMER_SIZE = auto, USE_LINKING_MATES = 0, LIMIT_JUMP_COVERAGE = 60, CA_PARAMETERS = cgwErrorRate = 0.25, NUM_THREADS = 64, JF_SIZE = 23000000, DO_HOMOPOLYMER_TRIM = 0.
The assemblies obtained from Miniasm using 2D ONT reads were error corrected twice using Racon (v1.3.0)50 and polished with the signal-level consensus software, nanopolish (v0.7.1) (available from: https://github.com/jts/nanopolish). Briefly, 2D ONT reads were mapped as all-vs-all read self-mapping using Minimap with the following options: -S, –w 5, -L 100, -m 0. Subsequently, Miniasm was executed with default options. The 2D ONT reads were mapped back to the assembly with Minimap (default parameters) and corrected with Racon with default parameters, and this was repeated one time. Burrows-Wheeler Aligner (v0.7.17-r1188) (BWA-MEM)51 with the –x ont2d option was then used to map all reads back to the Racon-corrected assembly to be used as the input for Nanopolish. Nanopolish was run with default parameters and --min-candidate-frequency 0.1. Furthermore, Canu assemblies were error corrected with Pilon (v1.22)52, Circlator (v1.5.3)53 and Nanopolish. All error corrections for the Canu assemblies with the above-mentioned tools were performed with default parameters.
Finally, to evaluate the accuracy of our assemblies, the ONT (corrected and non-corrected) and hybrid assemblies for the WHO reference strains were compared with the finished and closed 2016 WHO gonococcal reference genomes40. All 2D ONT reads were aligned to the genome sequence of the respective WHO reference strain, to be able to easily and directly determine the quality and accuracy using BWA-MEM (for mapping and phylogenetics) and Quast (v4.6.0) (for de novo assemblies). The top three assessed ONT de novo assemblies and the best hybrid assemblies were subjects for downstream analysis. Coding sequences (CDS) were annotated using Prokka (v1.12) on the chosen assemblies54.
Multiple-sequence alignment and phylogenetics
All Illumina and 2D ONT reads were mapped to the chromosome of FA1090 (GenBank: NC_002946.2) separately using BWA-MEM, the 2D ONT reads were specified using the nanopore option (-x –ont2d). All consensus sequences were merged into a multiple sequence alignment, single-nucleotide polymorphisms (SNPs) were called, and a maximum-likelihood phylogenetic tree based on SNPs was obtained using RAxML (version 8.2.8)55. This was also performed on Illumina sequences and 2D ONT sequences separately and the phylogeny was compared in a tanglegram.
Antimicrobial resistance determinants
To detect relevant gonococcal AMR determinants as quick and straight-forwardly as possible for future routine use of MinION sequencing, we evaluated several open-access and user-friendly web-based sequence analysis tools. The top three assessed ONT assemblies and the best hybrid assembly were examined using the Whole Genome Sequence Analysis (WGSA; www.wgsa.net)21 and the PubMLST N. gonorrhoeae AMR (still in development) scheme (www.pubmlst.org)56. The focus was on AMR determinants for ceftriaxone and cefixime (penA, mtrR, penB), azithromycin (23S rDNA, mtrR), ciprofloxacin (gyrA), tetracycline (rpsJ, tet(M) (plasmid-mediated resistance)), and benzylpenicillin (penA, ponA, mtrR, penB, blaTEM (plasmid-mediated resistance)). We only detected the AMR determinants on the plasmids and no additional downstream analysis was performed on the plasmids.
Furthermore, the 2D ONT reads were examined in our in house-customised CLC Genomics Workbench workflow to characterise the AMR determinants based on alleles in the N. gonorrhoeae Sequence Typing for Antimicrobial Resistance (NG-STAR) database (www.ngstar.canada.ca)57. The NG-STAR database lacked the possibility to run contig assemblies at the time of this study. The workflow employed de novo assembly without mapping and used BLAST with optimised algorithms for the identification, with the highest (%) hit being reported58.
The best performing tool of assembly and subsequent detection of AMR determinants was subsequently used to characterise the clinical isolates (n = 14).
Results
Overview of sequenced data
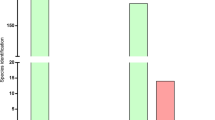
The 14 2016 WHO reference strains40 and 14 clinical isolates were sequenced using the ONT MinION platform. In these MinION runs, we obtained between 105 Mb and 922 Mb of 2D sequences with longest reads ranging from 26.0 to 58.6 kb and an average read length of 4.6–6.4 kb. The number of passed 2D ONT reads ranged from 17,500 to 147,700 with an average of 33% of all reads. For evaluation of the ONT sequences and further downstream analysis (taxonomy, hybrid assemblies and phylogeny), we used the 2 × 100 bp Illumina HiSeq paired-end reads with >250 depth for each WHO reference genome40 and 2 × 300 bp Illumina MiSeq paired-end reads with 80–100× depth for each clinical isolate. Taxonomy was defined for all reads using One Codex and 97–99% and 100% of all reads were classified as N. gonorrhoeae using ONT (Fig. 1) and Illumina MiSeq, respectively.
Readcount for the MinION (Oxford Nanopore Technologies (ONT)) dataset and read taxonomy classification of 2D ONT reads, when sequencing the 2016 WHO Neisseria gonorrhoeae reference strains (n = 14)40,41 and 14 clinical N. gonorrhoeae isolates. Percentage within each bar represents the proportion of reads classified as N. gonorrhoeae. The number above each bar represents the total number of reads that were classified.
Comparison of MinION de novo assemblies with the 2016 WHO gonococcal reference genomes
Assemblies were compared and selected based on the Quast results when comparing to the WHO reference genomes40 using the following criteria: lowest number of mismatches, misassemblies and number of contigs, and highest fraction of genome coverage (Supplementary Table). We selected and analysed ONT assemblies produced by Canu using only 2D ONT reads and polished with Nanopolish, Miniasm twice error corrected with Racon and polished with Nanopolish, and SMARTdenovo. Furthermore, the MaSuRCA hybrid assemblies (based on the ONT plus Illumina reads) were selected for downstream analysis (Table 1). Generally, ONT assemblies based on only the 2D ONT reads had a higher accuracy compared with assemblies using all reads (1D and 2D ONT reads) with fewer mismatches but very modest to no change in contiguity of the assemblies and fraction of the WHO reference genome covered. All error corrections were made using only 2D ONT reads and statistics such as mismatches and indels improved. Nanopolish had the best performance of the tested error correction tools and reduced the number of indels by up to 13 times. Assemblies produced with hybridSPAdes were more affected by the lower numbers of ONT reads, i.e. when using only 2D ONT reads. The hybrid assembly using SPAdes had less contiguity (up to 5.5 times more contigs) with higher numbers of mismatches (up to 4.4 more mismatches per 100 kb) and introductions of misassemblies (Supplementary Table). In general, the 2D ONT reads were used more efficiently by MaSuRCA for hybrid assembly, with overall improved statistics, especially for contiguity and mismatches.
Although the length of the assemblies based on the ONT sequences did not largely differ from the WHO reference genomes, the number of CDS was vastly different. The 2016 WHO gonococcal reference genomes include 2295–2450 CDS40. However, 3210–4712 CDS were identified using Prokka in our selected ONT assemblies. In contrast, Prokka identified 2228–2400 CDS in the MaSuRCA hybrid assemblies, which was more in line with the published WHO reference genomes (Table 1).
Error corrections using Pilon and Circlator, which is not designed for error correction, did not substantially improve the assemblies (Supplementary Table) and the assemblies error corrected with these tools were not used in the downstream analysis.
MinION for molecular epidemiology, including rapid outbreak investigations
The Illumina reads mapped to the PacBio-produced WHO reference genomes (n = 14)40 with no SNPs detected except for WHO M (one SNP) and a range of 93.3% to 96.4% of the reads mapped to the respective PacBio reference genome. The ONT reads mapped with 2–58 SNPs per genome sequence and 95.2% to 98.3% of the reads mapped. By executing BWA-MEM with the nanopore –x ont2d option, no SNPs between the ONT reads and the respective reference genomes were detected, but we found variation in the number of 2D ONT reads and percentage mapped to the FA1090 reference genome (Fig. 2). Therefore, the BWA-MEM nanopore option was used when mapping all 2D ONT reads to the FA1090 reference genome for the phylogenetic analysis (Figs 3 and 4). By creating the phylogeny with the ONT-produced genomes (n = 28) and Illumina MiSeq genomes (n = 28) separately, we showed that the ONT sequenced libraries produced a phylogenetic tree topology that was comparable with the one using the Illumina dataset (Fig. 4). The main difference in the tree topology was that WHO G and WHO N were closer to the root when Illumina sequences were used for the phylogeny. Moreover, all identical isolates separately sequenced with ONT and Illumina clustered together, except for some (n = 7) of the clinical isolates where the Illumina sequences were more closely related. In four of these cases (11 cervix (C)/12 rectum (R) and 13 (R)/14 urethra (U)), the isolates were from the same patients but from different anatomical sites. For three isolates (5, 6 and 7), the Illumina sequences were also more closely related but all of the separately sequenced datasets were still on the same branch showing that these isolates were very similar (Fig. 3).
Phylogenetic tree of the genome sequences of the 2016 WHO Neisseria gonorrhoeae reference strains (n = 14)40,41 and clinical gonococcal isolates (n = 14) sequenced with Illumina MiSeq and MinION (Oxford Nanopore Technologies (ONT)). The tree uses the genome of the N. gonorrhoeae reference strain FA1090 as reference (shown with black bar). The platform used, number of reads, average read length, and number of single nucleotide polymorphisms (SNPs) are displayed as colored bars next to each node in the tree. The numbers inside the SNP-bars is the pairwise distance between the Illumina and 2D ONT sequences.
MinION for detection of AMR determinants
To investigate the four final de novo assemblies using Canu (polished), Miniasm (polished), SMARTdenovo, and MaSuRCA (Illumina hybrid) for detection of AMR determinants in the 2016 WHO gonococcal reference genomes40, we used the WGSA (www.wgsa.net)21 and PubMLST (www.pubmlst.org).
WGSA is an easy-to-use web interface where you drag-and-drop the assemblies into the web browser and the characterisation is done in minutes21. We used this interface for all chosen assemblies (n = 112) and the analysis of AMR determinants took 15 minutes. We observed good concordance overall with the verified AMR determinants in the reference genomes (Table 2), with the exception of the 23S rDNA macrolide resistance determinant C2611T, which was incorrectly identified in the Canu (polished) and Miniasm (polished) assemblies. No ONT assembly was able to correctly characterise penA in WHO W and none, including the MaSuRCA hybrid assembly, was able to correctly characterise penA in WHO K (Table 2). The characterisation of plasmid-mediated AMR determinants was inaccurate in all four chosen assemblies for the detection of tet(M). Also, the chosen assemblies failed to detect blaTEM in WHO M, WHO O and WHO V and incorrectly reported presence of blaTEM in WHO G in the Miniasm (polished), SMARTdenovo and MaSuRCA assemblies (Table 3). Out of the 2D ONT assemblies, the SMARTdenovo assembly performed the best.
We also used the PubMLST database, which is another easy-to-use web-based tool, that can mine assembly data for various purposes. The database uses assemblies as input and delivers results in few minutes. The PubMLST database (www.pubmlst.org), using 2D ONT assemblies, was only able to characterise the mtrR AMR determinant and this was only done in the Canu assemblies. However, using the MaSuRCA hybrid assembly PubMLST had 100% concordance with the published reference genomes for detection of penA, mtrR, penB, ponA, 23S rDNA, gyrA, and tet(M). PubMLST does not include rpsJ in its gonococcal AMR characterisation module and also failed to detect the blaTEM gene in WHO M and WHO N (Table 3).
The NG-STAR database57, included in the WHO CC in house-customised CLC Genomics Workbench, gave 100% concordance for the presence of all AMR determinants characterised in NG-STAR57 with the reference genomes (Table 2). All the plasmid-mediated AMR determinants (Table 3) and the AMR determinants penB, 16S rDNA, and parC were also correctly characterised. The customised CLC Genomics Workbench was therefore used to characterise the AMR determinants in the clinical isolates using only the 2D ONT reads.
In house-customised CLC Genomics Workbench for characterisation of AMR determinants in clinical gonococcal isolates
The 14 isolates expressed decreased susceptibility (MIC ≥ 0.032 mg/L)59 or resistance to ceftriaxone (11/14) and cefixime (11/14), azithromycin (3/14), and ciprofloxacin (13/14) (Table 4). No isolate displayed spectinomycin resistance or produced β-lactamase. The in house-customised CLC Genomics Workbench including the NG-STAR database57 correctly characterised all AMR determinants in the isolates using only the 2D ONT reads and found 12, 1, and 13 of the 14 isolates carrying AMR mutations in penA (cefixime and ceftriaxone resistance determinant), 23S rDNA (azithromycin resistance determinant), and gyrA (ciprofloxacin resistance determinant), respectively. Twelve of the 14 isolates also harboured parC resistance mutations, which contribute to the high MICs in isolates with high-level ciprofloxacin resistance. Specific mutations in mtrR, resulting in an over-expression of the MtrCDE efflux pump, and porB1b (penB AMR determinant), causing a decreased influx of antimicrobials through PorB, were identified in 12 of the 14 isolates. No 16S rDNA resistance mutations (spectinomycin resistance determinant) or plasmid-mediated AMR determinants (high-level resistance to benzylpenicillin and tetracycline) were detected. Resistance mutation in rpsJ (decreased susceptibility/resistance to tetracycline) was found in all isolates. There was 100% concordance between the AMR determinants detected using the 2D ONT reads only and Illumina reads. Consequently, resistance or decreased susceptibility to extended-spectrum cephalosporins, azithromycin, spectinomycin, ciprofloxacin, tetracycline, and benzylpenicillin could be accurately predicted using solely 2D ONT reads (Table 4).
Discussion
In the present study, we show that gonococcal genomes can be de novo assembled with high accuracy and contiguity running assemblies with MinION 2D ONT reads in combination with Illumina reads using MaSuRCA. These assemblies varied from one to eight contigs and could be further investigated using tools like Circlator53 to obtain circular and finished gonococcal genomes. Furthermore, it is possible to obtain accurate de novo assemblies for AMR determinant detection by initially performing Illumina-based correction of individual ONT reads and subsequently using the reads for de novo assembly. It was also recently shown that complete hybrid genome assembly for gonococcal isolates can be obtained by combining short-read (Illumina) and long-read (ONT) sequence data14. However, this strategy makes the ONT platform dependent on additional Illumina sequencing. Nevertheless, this is another approach for producing accurate finished genomes and, accordingly, an alternative to PacBio sequencing of microbial reference genomes.
When relying only on the ONT data, the assemblies contained high numbers of mismatches (27–607 mismatches per 100 kb) and indels (641–1125 indels per 100 kb), using even the best ONT assemblies obtained using SMARTdenovo, Canu, and Miniasm with 2D ONT reads. There are several possible reasons for the high and incorrect number of CDSs in the ONT assemblies using Prokka, including sequencing artefacts, homopolymers and overall high error rate (SNPs, insertions and deletions) in the 2D ONT reads causing the assemblies to contain incorrect internal stop codons and false pseudogenes. Generally, the 2D ONT reads generated more accurate assemblies than the 1D ONT reads and were used in the majority of our downstream analysis. We aimed to obtain highly accurate de novo assemblies to be able to rapidly identify relevant gonococcal AMR determinants to predict AMR, using only user-friendly and rapid online sequence analysis tools such as WGSA (www.wgsa.net)21 and PubMLST (www.pubmlst.org). Using these online tools, the characterisation of AMR determinants was generally inaccurate using ONT assemblies and, as expected, highly accurate with hybrid assemblies. However, the in house-customised CLC Genomics Workbench workflow, including the NG-STAR database57, provided 100% concordance with the AMR determinants of the PacBio sequenced 2016 WHO gonococcal reference genomes40 using only 2D ONT reads. We can also extract additional AMR determinants and in general genes of interest that are not included in the online tools, because our AMR database is fully customisable. The software workflow is based on extraction of the genes of interest in the customised database from a de novo assembly using BLAST algorithms optimised for each AMR determinant and reporting the highest hit, i.e. not only the 100% hit, in also genes with premature stop codons. This is essential because the ONT de novo assemblies are prone to errors. The main limitations of any CLC Genomics Workbench are that it is commercial (not an open-source online tool) and it has fairly high system requirements (16–32 GB RAM). Nevertheless, it has a simple general user interface for users who are not familiar with command line bioinformatics and is available to all widely used operating systems. Hopefully, open-source tools and public databases that can handle error-prone assemblies will be inspired by this approach and incorporate e.g. NG-STAR data57 rendering costly software obsolete. NG-STAR can currently not use genome assemblies as input for determining the AMR profiles, which limits its possibilities when performing WGS.
Easy and rapid genome sequencing, using platforms such as the ONT MinION, in combination with algorithms that can appropriately predict AMR profiles using only genetic data could be very valuable in future surveillance of gonococcal AMR and spread of AMR gonococcal strains, nationally and internationally. Briefly, using the customised CLC Genomics Workbench, we showed that a mosaic penA allele or a penA A501 substitution was detected in all clinical isolates expressing decreased susceptibility to extended-spectrum cephalosporins (ESCs; cefixime and ceftriaxone) and predicted decreased susceptibility to ESCs with 100% sensitivity and specificity. However, these AMR determinants can also be found in gonococcal isolates susceptible to ESCs6,20, so the specificity of the prediction of decreased susceptibility or resistance to ESCs is expected to be lower in studies that test larger numbers of isolates. Detection of the C2611T mutation in all four alleles of the 23S rRNA gene predicted azithromycin resistance in one clinical isolate (MIC = 4 mg/L), but not in two isolates with low-level azithromycin resistance (MIC = 1 mg/L). Finally, detection of the GyrA S91F mutation predicted the resistance in all (100%) the 13 clinical ciprofloxacin resistant isolates. Molecular tests, including WGS, will probably never completely replace culture-based AMR testing because these methods can only detect known AMR determinants; some gonococcal AMR determinants remain unknown and new AMR determinants are continuously evolving. However, molecular AMR testing can complement culture-based AMR testing. In settings in which molecular diagnostics is replacing culture-based diagnostics, rapid and accurate detection of known AMR determinants would significantly increase the number of samples tested for antimicrobial susceptibility. Ideally, molecular AMR testing should use WGS to identify all known and potentially new AMR determinants that can be used to predict AMR and even the MICs of antimicrobials60.
The use of 2D ONT reads for phylogenomics of gonococci, e.g. for molecular epidemiological surveillance purposes, would be exceedingly valuable for outbreak investigations and monitoring in nearly real time in local, national and international gonococcal surveillance programmes, which aim to replace traditional, labour intensive and less accurate genotyping techniques such as N. gonorrhoeae multi-antigen sequence typing (NG-MAST) and multi-locus sequence typing (MLST) with WGS techniques21. Accordingly, we examined the accuracy of performing phylogenomic analysis using 2D ONT reads mapped to a reference genome using BWA-MEM with the nanopore option and building a phylogeny using the multiple sequence alignment. The ONT data produced a phylogenetic tree topology that was comparable with the one using the Illumina dataset and clustered all related isolates similarly (Figs 3 and 4). However, the number of isolates was limited and the genomic heterogeneity of the strains was high, which might have slightly biased our analysis.
Interestingly, the clustering of isolates was not highly dependent on the number of 2D ONT reads (Fig. 1). This suggests that the read length provides sufficient genome coverage even when a relatively low number of reads are available. For example, the lower number of 2D ONT reads for WHO G (Fig. 1) still provided a 99.96–100% genome fraction (Supplementary Table) and the read length compensated for the low number of reads. For the different WHO reference strains, 89.93–100% fraction of the PacBio-sequenced genomes were covered by the ONT reads (Supplementary Table). Consequently, for some purposes including gonococcal phylogenomic analysis, the MinION sequencer has likely collected enough reads in less than one day, which opens up new possibilities in running WGS to investigate gonorrhoea outbreaks in nearly real time, as well as directly from clinical samples.
The main benefits of using the MinION for genome sequencing included the very rapid turn-around time, high accessibility by connecting the small hand-held device to a laptop, and low cost of the sequencer. The main limitations included the lower accuracy and consistency compared to Illumina and PacBio sequencing reads and the high cost of each sequencing run. Cost remains a major obstacle to the use of MinION outside well-resourced research-focused laboratories. It is essential that the cost of MinION runs is reduced further, for example by using cheaper reagents or multiplexing libraries, and/or having international support and funding for use of MinION, or similar technologies, at national, regional and local levels in less-resourced settings. Furthermore, new bioinformatic tools for analysing the MinION reads are being developed continuously. Future studies should appropriately evaluate, for example, different basecalling tools (https://github.com/rrwick/Basecalling-comparison), assemblers such as Unicycler61, and mapping tools, e.g., minimap262 and GraphMap63.
In conclusion, we show, in the first MinION study for gonococci, that ONT sequences analysed with currently existing open-access, web-based sequence analysis tools are not sufficiently accurate to identify key gonococcal AMR determinants. However, using an appropriate analysis workflow such as an in house-developed CLC Genomics Workbench, we show that 2D ONT sequence data can be used for rapid and accurate identification of AMR determinants in N. gonorrhoeae isolates to predict decreased susceptibility or resistance to recommended therapeutic antimicrobials. We also show that 2D ONT sequence data can be useful for phylogenomics of N. gonorrhoeae, e.g. for molecular epidemiological investigations in nearly real time, and, using 2D ONT-Illumina hybrid assemblies, for producing contiguous assemblies and finished gonococcal reference genomes. The performance of MinION for WGS of N. gonorrhoeae directly from non-cultured nucleic acid amplification test samples now needs to evaluated.
References
Newman, L. et al. Global estimates of the prevalence and incidence of four curable sexually transmitted infections in 2012 based on systematic review and global reporting. PLoS. One. 10, e0143304, https://doi.org/10.1371/journal.pone.0143304 (2015).
Hook, E. W. III. & Handsfield H. Gonococcal infections in adults. In Sexually Transmitted Infections (eds Holmes K. K. et al), 4th edition, The McGraw-Hill Companies Inc., USA (2008).
Kerle, K. K., Mascola, J. R. & Miller, T. A. Disseminated gonococcal infection. Am. Fam. Physician. 45, 209–214 (1992).
World Health Organization (WHO). WHO guidelines for the treatment of Neisseria gonorrhoeae, http://www.who.int/reproductivehealth/publications/rtis/gonorrhoea-treatment-guidelines/en/ (2016).
World Health Organization. Global action plan to control the spread and impact of antimicrobial resistance in Neisseria gonorrhoeae, http://whqlibdoc.who.int/publications/2012/9789241503501_eng.pdf?ua=1 (2012).
Unemo, M. & Shafer, W. M. Antimicrobial resistance in Neisseria gonorrhoeae in the 21st century: past, evolution, and future. Clin. Microbiol Rev. 27, 587–613 (2014).
Unemo, M. et al. Sexually transmitted infections: challenges ahead. Lancet Infect. Dis. 17, e235–e279 (2017).
Wi, T. et al. Antimicrobial resistance in Neisseria gonorrhoeae: Global surveillance and a call for international collaborative action. PLoS. Med. 14, e1002344, https://doi.org/10.1371/journal.pmed.1002344 (2017).
Terkelsen, D. et al. Multidrug-resistant Neisseria gonorrhoeae infection with ceftriaxone resistance and intermediate resistance to azithromycin, Denmark, 2017. Euro. Surveill. 22, https://doi.org/10.2807/1560-7917.ES.2017.22.42.17-00659 (2017).
Fifer, H. et al. Failure of dual antimicrobial therapy in treatment of gonorrhea. N. Engl. J. Med. 374, 2504–2506 (2016).
Cole, M. J. et al. Overall low extended-spectrum cephalosporin resistance but high azithromycin resistance in Neisseria gonorrhoeae in 24 European countries, 2015. BMC. Infect. Dis. 17, 617, https://doi.org/10.1186/s12879-017-2707-z (2017).
Katz, A. R. et al. Cluster of Neisseria gonorrhoeae isolates with high-level azithromycin resistance and decreased ceftriaxone susceptibility, Hawaii, 2016. Clin. Infect. Dis. 65, 918–923 (2017).
Alirol, E. et al. Multidrug-resistant gonorrhea: A research and development roadmap to discover new medicines. PLoS. Med. 14, e1002366 (2017).
Eyre, D. W. et al. Gonorrhoea treatment failure caused by a Neisseria gonorrhoeae strain with combined ceftriaxone and high-level azithromycin resistance, England, February 2018. Euro. Surveill. 23, https://doi.org/10.2807/1560-7917.ES.2018.23.27.1800323 (2018).
Whiley, D. M., Jennison, A., Pearson, J. & Lahra, M. M. Genetic characterization of Neisseria gonorrhoeae resistant to both ceftriaxone and azithromycin. Lancet Infect. Dis. 18, 717–718 (2018).
World Health Organization (WHO). Global priority list of antibiotic-resistance bacteria to guide research, discovery, and development of new antibiotics. http://www.who.int/medicines/publications/WHO-PPL-Short_Summary_25Feb-ET_NM_WHO.pdf?ua=1 (2017).
World Health Organization (WHO). Global surveillance network for gonococcal antimicrobial susceptibility. http://apps.who.int/medicinedocs/documents/s16348e/s16348e.pdf (1990).
Spiteri, G. et al. The European gonococcal antimicrobial surveillance programme (Euro-GASP)–a sentinel approach in the European Union (EU)/European economic area (EEA). Sex. Transm. Infect. 89(Suppl 4), iv16–8, https://doi.org/10.1136/sextrans-2013-051117 (2013).
Kirkcaldy, R. D. et al. Neisseria gonorrhoeae antimicrobial susceptibility surveillance–the gonococcal isolate surveillance project, 27 sites, United States, 2014. MMWR. Surveill. Summ. 65, 1–19 (2016).
Donà, V., Low, N., Golparian, D. & Unemo, M. Recent advances in the development and use of molecular tests to predict antimicrobial resistance in Neisseria gonorrhoeae. Expert. Rev. Mol. Diagn. 17, 845–859 (2017).
Harris, S. R. et al. Public health surveillance of multidrug-resistant clones of Neisseria gonorrhoeae in Europe: a genomic survey. Lancet Infect. Dis. 18, 758–768 (2018).
Bleidorn, C. Third generation sequencing: technology and its potential impact on evolutionary biodiversity research. Syst. Biodiver. 14, 1–8 (2016).
Schadt, E. E., Turner, S. & Kasarskis, A. A window into third-generation sequencing. Hum. Mol. Genet. 19, R227–R240 (2010).
Kasianowicz, J. J., Brandin, E., Branton, D. & Deamer, D. W. Characterization of individual polynucleotide molecules using a membrane channel. Proc. Natl. Acad. Sci. 93, 13770–13773 (1996).
Venkatesan, B. M. & Bashir, R. Nanopore sensors for nucleic acid analysis. Nat. Nanotechnol. 6, 615–624 (2011).
Yang, Y. et al. Advances in nanopore sequencing technology. J. Nanosci. Nanotechnol. 13, 4521–4538 (2013).
Camilla, L. C. et al. MinION analysis and reference consortium: Phase 1 data release and analysis. F1000Res. 4, 1075, https://doi.org/10.12688/f1000research.7201.1 (2015).
Miten, J. et al. MinION analysis and reference consortium: Phase 2 data release and analysis of R9.0 chemistry. F1000Res 6, 760, https://doi.org/10.12688/f1000research.11354.1 (2017).
Clarke, J. et al. Continuous base identification for single-molecule nanopore DNA sequencing. F1000Res 4, 265–270 (2009).
Stoddart, D., Heron, A. J., Mikhailova, E., Maglia, G. & Bayley, H. Single-nucleotide discrimination in immobilized DNA oligonucleotides with a biological nanopore. F1000Res 106, 7702–7707 (2009).
Kerkhof, L. J., Dillon, K. P., Häggblom, M. M. & McGuinness, L. R. Profiling bacterial communities by MinION sequencing of ribosomal operons. Microbiome. 5, 116, https://doi.org/10.1186/s40168-017-0336-9 (2017).
Imai, K. et al. A novel diagnostic method for malaria using loop-mediated isothermal amplification (LAMP) and MinION™ nanopore sequencer. BMC. Infect. Dis. 17, 621, https://doi.org/10.1186/s12879-017-2718-9 (2017).
Faria, N. R. et al. Establishment and cryptic transmission of Zika virus in Brazil and the Americas. Nature. 546, 406–410 (2017).
Quick, J. et al. Real-time, portable genome sequencing for Ebola surveillance. Nature. 530, 228–232 (2016).
Deschamps, S. et al. Characterization, correction and de novo assembly of an Oxford Nanopore genomic dataset from Agrobacterium tumefaciens. Sci. Rep. 6, 28625, https://doi.org/10.1038/srep28625 (2016).
Loman, N. J., Quick, J. & Simpson, J. T. A complete bacterial genome assembled de novo using only nanopore sequencing data. Nat. Methods. 12, 733–735 (2015).
Istace, B. et al. de novo assembly and population genomic survey of natural yeast isolates with the Oxford Nanopore MinION sequencer. Gigascience. 6, 1–13 (2017).
van der Helm, E. et al. Rapid resistome mapping using nanopore sequencing. Nucleic Acids Res. 45, e61, https://doi.org/10.1093/nar/gkw1328 (2017).
Judge, K., Harris, S. R., Reuter, S., Parkhill, J. & Peacock, S. J. Early insights into the potential of the Oxford Nanopore MinION for the detection of antimicrobial resistance genes. J. Antimicrob. Chemother. 70, 2775–2778 (2015).
Unemo, M. et al. The novel 2016 WHO Neisseria gonorrhoeae reference strains for global quality assurance of laboratory investigations: phenotypic, genetic and reference genome characterization. J. Antimicrob. Chemother. 71, 3096–3108 (2016).
El-Rami, F. E., Zielke, R. A., Wi, T., Sikora, A. E. & Unemo, M. Quantitative proteomics of the 2016 WHO Neisseria gonorrhoeae reference strains surveys vaccine candidates and antimicrobial resistance determinants. Mol. Cell Proteomics, https://doi.org/10.1074/mcp.RA118.001125 (2018).
Donà, V. et al. Mismatch amplification mutation assay-based real-time PCR for rapid detection of Neisseria gonorrhoeae and antimicrobial resistance determinants in clinical specimens. J. Clin. Microbiol. Aug 27, 56(9), https://doi.org/10.1128/JCM.00365-18 (2018).
Unemo, M., Olcén, P., Berglund, T., Albert, J. & Fredlund, H. Molecular epidemiology of Neisseria gonorrhoeae: sequence analysis of the porB gene confirms presence of two circulating strains. J. Clin. Microbiol 40, 3741–3749 (2002).
Loman, N. J. & Quinlan, A. R. Poretools: a toolkit for analyzing nanopore sequence data. Bioinformatics. 30, 3399–3401 (2014).
Koren, S., Walenz, B. P., Berlin, K., Miller, J. R. & Phillippy, A. M. Canu: scalable and accurate long-read assembly via adaptive k-mer weighting and repeat separation. Genome Res. 27, 722–736 (2017).
Li, H. Minimap and miniasm: fast mapping and de novo assembly for noisy long sequences. Bioinformatics. 32, 2103–2110 (2016).
Koren, S. et al. Hybrid error correction and de novo assembly of single-molecule sequencing reads. Nat. Biotechnol. 30, 693–700 (2012).
Antipov, D., Korobeynikov, A., McLean, J. S. & Pevzner, P. A. hybridSPAdes: an algorithm for hybrid assembly of short and long reads. Bioinformatics. 32, 1009–1015 (2016).
Zimin, A. V. The MaSuRCA genome assembler. Bioinformatics. 29, 2669–2677 (2013).
Vaser, R., Sovic, I., Nagarajan, N. & Sikic, M. Fast and accurate de novo genome assembly from long uncorrected reads. Genome Res. 27, 737–746 (2017).
Li, H. & Durbin, R. Fast and accurate long-read alignment with Burrows-Wheeler transform. Bioinformatics. 26, 589–595 (2010).
Walker, B. J. Pilon: an integrated tool for comprehensive microbial variant detection and genome assembly improvement. PLoS. One. 9, e112963, https://doi.org/10.1371/journal.pone.0112963 (2014).
Hunt, M. Circlator: automated circularization of genome assemblies using long sequencing reads. Genome Biol. 16, 294, https://doi.org/10.1186/s13059-015-0849-0 (2015).
Seemann, T. Prokka: rapid prokaryotic genome annotation. Bioinformatics. 30, 2068–2069 (2014).
Stamatakis, R. RAxML version 8: a tool for phylogenetic analysis and post-analysis of large phylogenies. Bioinformatics. 30, 1312–1313 (2014).
Jolley, K. A. & Maiden, M. C. BIGSdb: Scalable analysis of bacterial genome variation at the population level. BMC. Bioinformatics. 11, 595, https://doi.org/10.1186/1471-2105-11-595 (2010).
Demczuk, W. et al. Neisseria gonorrhoeae Sequence Typing for Antimicrobial Resistance, a novel antimicrobial resistance multilocus typing scheme for tracking global dissemination of N. gonorrhoeae strains. J. Clin. Microbiol. 55, 1454–1468 (2017).
Zankari, E. et al. Identification of acquired antimicrobial resistance genes. J. Antimicrob. Chemother. 67, 2640–2644 (2012).
Golparian, D., Hellmark, B., Fredlund, H. & Unemo, M. Emergence, spread and characteristics of Neisseria gonorrhoeae isolates with in vitro decreased susceptibility and resistance to extended-spectrum cephalosporins in Sweden. Sex. Transm. Infect. 86, 454–460 (2010).
Eyre, D. W. et al. WGS to predict antibiotic MICs for Neisseria gonorrhoeae. J. Antimicrob. Chemother. 72, 1937–1947 (2017).
Wick, R. R., Judd, L. M., Gorrie, C. L. & Holt, K. E. Unicycler: resolving bacterial genome assemblies from short and long sequencing reads. PLoS. Comput. Biol. 13, e1005595 (2017).
Li, H. Minimap2: pairwise alignment for nucleotide sequences. Bioinformatics 34, 3094–3100 (2018).
Sović, I. et al. Fast and sensitive mapping of nanopore sequencing reads with GraphMap. Nat Commun 7, 11307, https://doi.org/10.1038/ncomms11307 (2016).
Acknowledgements
We are grateful to Sara Kasraian for laboratory work in RaDAR-Go and Dianne Egli-Gany for her contribution to the management of RaDAR-Go and organisation of the specimens for this study. We are also grateful for the financial support provided by Örebro County Council Research Committee and the Foundation for Medical Research at Örebro University Hospital, Örebro, Sweden and the SwissTransMed initiative (Translational Research Platforms in Medicine, project number #25/2013: Rapid Diagnosis of Antibiotic Resistance in Gonorrhoea, RaDAR-Go) from the Rectors’ Conference of the Swiss Universities (CRUS). LSB and SRH were supported by Wellcome Grant number 098051. We would like to thank the Pathogen Informatics Group at the Wellcome Sanger Institute for support.
Author information
Authors and Affiliations
Contributions
D.G., V.D., A.E., N.L. and M.U. planned and designed the study. V.D. performed the MinION sequencing. D.G. performed the Illumina sequencing and all the bioinformatic analysis, with support from S.H. and L.S.-B. D.G. supported by M.U. wrote a draft of the manuscript. D.G., V.D., L.S.-B., S.F., S.H., A.E., N.L. and M.U. commented on and approved the final manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Golparian, D., Donà, V., Sánchez-Busó, L. et al. Antimicrobial resistance prediction and phylogenetic analysis of Neisseria gonorrhoeae isolates using the Oxford Nanopore MinION sequencer. Sci Rep 8, 17596 (2018). https://doi.org/10.1038/s41598-018-35750-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-35750-4
Keywords
This article is cited by
-
Antimicrobial resistance and heterogeneity of Neisseria gonorrhoeae isolated from patients attending sexually transmitted infection clinics in Lusaka, Zambia
BMC Genomics (2024)
-
Neisseria gonorrhoeae Antimicrobial Resistance: Past to Present to Future
Current Microbiology (2021)
-
Metagenomic next-generation sequencing of rectal swabs for the surveillance of antimicrobial-resistant organisms on the Illumina Miseq and Oxford MinION platforms
European Journal of Clinical Microbiology & Infectious Diseases (2021)
-
High quality genome assemblies of Mycoplasma bovis using a taxon-specific Bonito basecaller for MinION and Flongle long-read nanopore sequencing
BMC Bioinformatics (2020)
-
Benchmarking hybrid assembly approaches for genomic analyses of bacterial pathogens using Illumina and Oxford Nanopore sequencing
BMC Genomics (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.