Abstract
The aim of this study was to estimate the prevalence of concurrent diagnoses of asthma/COPD and examine its full spectrum of comorbid disorders in Germany. We used nationwide outpatient claims data comprising diagnoses of all statutory health insurees (40+ years) in 2017 (N = 40,477,745). The ICD-10 codes J44 (COPD) and J45 (asthma) were used to identify patients. The odds of 1,060 comorbid disorders were examined in a case–control study design. Of all insurees, 4,632,295 (11%) were diagnosed with either asthma or COPD. Of them, 43% had asthma only, 44% COPD only and 13% both diseases. The prevalence of concurrent asthma/COPD was 1.5% with a slightly higher estimate among females than males (1.6% vs. 1.4%) and constant increase by age in both sexes. Comorbid disorders were very common among these patients. 31 disorders were associated with a strong effect size (odds ratio > 10), including other respiratory diseases, but also bacterial (e.g., mycobacteria, including tuberculosis) and fungal infections (e.g., sporotrichosis and aspergillosis). Patients with concurrent asthma/COPD suffer from comorbid disorders involving various body systems, which points to the need of a multidisciplinary care approach. Regular screening for common comorbid disorders may result in better clinical course and prognosis as well as improvement of patients’ quality of life.
Similar content being viewed by others
Introduction
Asthma and chronic obstructive pulmonary disease (COPD) are common chronic diseases characterized by airflow obstruction. Some patients may display clinical features of both diseases, the condition called initially the asthma-COPD overlap syndrome (ACOS)1,2. However, the term ‘ACOS’ is no longer advised as it contains various clinical phenotypes with possibly different underlying pathophysiological mechanisms. Recently, the Global Initiative for Asthma (GINA) and the Global Initiative for Chronic Obstructive Lung Disease (GOLD) provided a stepwise approach to diagnose the asthma-COPD overlap (further referred to as ACO) and initial treatment strategy3. Many questions regarding etiology and underlying mechanisms remain still unanswered. In particular, there is no well-accepted definition of ACO; diagnostic criteria have not yet been developed either. It is still unknown whether ACO represents a distinct phenotypic condition or is just a disease that features clinical characteristics of both diseases. As a consequence, there is uncertainty regarding the actual disease occurrence. Previous studies reported prevalence estimates for ACO among patients with asthma or COPD varying widely from study to study from 15 to 55%4. The prevalence variations resulted mainly from different case definitions, but also from other methodological differences across studies. In contrast, there is agreement that patients with ACO exhibit higher morbidity and mortality compared to patients with asthma or COPD only1. Patients with ACO have more rapid and severe disease progression including more frequent exacerbations and a higher risk of some comorbid diseases5,6. In particular, cardiovascular diseases are more common among ACO patients as compared to individuals without ACO7 or patients with asthma or COPD alone8,9,10. This results in greater healthcare utilization and poorer quality of life8.
In Germany, research on the epidemiology of ACO is lacking. A recently published systematic review of the global prevalence of ACO reported a pooled estimate of 2.0% based on 27 population-based studies mostly from industrialized countries such as Canada, USA and several European countries11. No single study was found in Germany11. The aims of this study were thus to estimate the prevalence of concurrent diagnoses of asthma and COPD in the general German population for the first time and examine the full spectrum of comorbid disorders coexistent in these patients using nationwide ambulatory claims data comprising information on all statutory health insured (SHI) adults in Germany. Using a case–control study design we compared the odds of 1060 comorbid disorders in these patients and controls matched by sex, age and region of residence.
Results
Prevalence of concurrent diagnoses of asthma/COPD
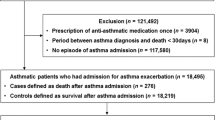
Of the 40,477,745 SHI-individuals, 4,632,295 (11%) were diagnosed with either asthma or COPD. Of them, 43% had asthma only and 44% COPD only (Fig. 1). The remaining 13% had both diagnoses. Among them, the proportion of female patients was higher than male patients (Table 1). The proportion of concurrent diagnoses among patients with asthma was 23.3%. On the other way around, the proportion of concurrent diagnoses among patients with COPD was 23.1%. The crude prevalence of concurrent diagnoses of asthma/COPD in the whole SHI-population was 1.50% (99% CI: 1.50–1.51%). The prevalence was slightly higher among females (1.57%) than males (1.42%) and increased by age in both sexes (Fig. 2); the lowest prevalence was observed among individuals in the youngest age group of 40–45 years in both sexes (males, 0.42%; females, 0.43%). It then increased almost linearly with advancing age reaching the peak in the age group of 80–84 years among males (2.37%) and 70–74 years among females (2.45%). The age-specific prevalence of concurrent asthma/COPD showed a distinctive pattern as compared to that of asthma or COPD only (Fig. 2). Whereas the prevalence of asthma decreased with advancing age, the prevalence of COPD increased (with a more prominent increase among males than females). The weighted prevalence estimate of concurrent asthma/COPD in the total German population ≥ 40 years was 1.39%.
Ranking of comorbid disorders in patients with concurrent asthma/COPD
The most prevalent disease groups among patients with concurrent asthma/COPD were diseases of the circulatory system (82%), followed by metabolic and musculoskeletal diseases (each 77%, Fig. 3). In addition, more than 50% of patients had mental, gastrointestinal or other pulmonary diseases. The prevalence of diseases in the control group is presented in Fig. 3B. The ranking of diseases in the control group yielded a similar pattern. Remarkably, all 14 disease groups examined were more prevalent among patients with asthma/COPD than in controls with the prevalence ratios (PR) ranging between 1.31 (99% CI: 1.31–1.31) (circulatory system) and 2.03 (99% CI: 2.01–2.05) (infectious and parasitic diseases) (Fig. 3C). As expected, other pulmonary diseases were more frequently observed among patients with asthma/COPD than in the control group (PR, 5.74; 99% CI: 5.71–5.77).
(Co)morbid disorders among adults of age 40 and older with and without asthma/COPD diagnoses, by disease group, 2017. aRanked by the prevalence of comorbid diseases in patients with concurrent diagnoses of asthma/COPD. bThe number on the y axis represents ranking in the control group. Control group was matched by sex, age and ASHIP of residence. A vertical dashed red line in panel C represents a prevalence ratio of 1. ASHIP, regional Associations of Statutory Health Insurance Physicians.
The top 20 specific comorbid disorders (at the level of the first three characters of the ICD-10 code) among patients with asthma/COPD are presented in Table 2. More than two-thirds of these patients suffered from primary hypertension, every fourth patient had a diagnosis of chronic ischemic heart disease and every sixth patient had chronic heart failure. The most prevalent metabolic disorders were disorders of lipoprotein metabolism and other lipidemias (43%), type 2 diabetes (38%), obesity (27%) and nontoxic goiter (17%). Every fourth patient with asthma/COPD had a diagnosis of depressive episode and every fifth patient had sleep disorders. All 20 top ranked comorbid diseases were more prevalent among patients with asthma/COPD than among controls.
Comorbidity profile
Out of the total 1079 three-character ICD-10 codes from 14 chapters, we identified 1064 codes among patients with asthma/COPD diagnoses and 1069 codes in the control population, with an overlap of 1060 codes found in both groups. Of the 1060 comorbid disorders examined, 987 (93%) disorders were significantly different among patients with asthma/COPD as compared to controls at the significance level of 5%. After Bonferroni correction, 879 (83%) remained significant (p ≤ 4.72 × 10–5). Figure 4 depicts a scatter plot of the odds ratios for comorbid disorders among patients with asthma/COPD over their prevalence estimates. In general, the odds of comorbid disorders were higher among patients than among controls. Comorbid disorders with significant OR < 1 were observed for seven disorders (Alzheimer disease and associated dementia and multiple sclerosis) reflecting survival bias; all other disorders were positively associated with concurrent asthma/COPD. Of the latter, associations can be roughly divided into three groups; those with a small (OR 1.0–1.5), moderate (OR 1.5–5.0) and large size effect (OR > 10). There were 99 disorders associated with asthma/COPD with a small size effect, for most of them the prevalence was very low (< 1%). The majority of comorbid disorders were associated with a medium size effect. Of them, 35 disorders had a prevalence of > 10% (including cardiovascular [e.g., primary hypertension, chronic ischemic heart disease and heart failure], metabolic [disorders of lipoprotein metabolism, type2 diabetes, obesity and nontoxic goiter], and mental disorders [depression and sleep disorders]). Thirty-one disorders had a strong size effect (OR > 10), but most of them were low prevalent (< 1%). As expected, this group mostly included other respiratory disorders. Two respiratory disorders with OR > 10 had prevalence over 10% (respiratory failure [11%] and emphysema [12%]). In addition, patients with concurrent asthma/COPD were more likely to have bacterial (e.g., mycobacteria, including tuberculosis) and fungal infections (e.g., sporotrichosis and aspergillosis).
Scatter plot depicting odds ratios for comorbid disorders among patients with concurrent asthma/COPD diagnoses over their prevalence estimates. Each circle represents a comorbid disorder defined by the first three characters of an ICD-10 code. In total, 940 comorbid disorders are depicted; 120 disorders had very low prevalence and could not be depicted due to data protection regulations (n < 30 either in cases or controls). Control group was matched by sex, age and ASHIP of residence. ASHIP, regional Associations of Statutory Health Insurance Physicians; COPD, chronic obstructive pulmonary disease; GERD, gastroesophageal reflux disease; CIHD, chronic ischemic heart disease; T2D, type 2 diabetes.
Discussion
We made use of the nationwide outpatient claims data comprising information of 86% of the general German population to estimate the prevalence of concurrent diagnoses of asthma/COPD and examine its comorbid disorders. To the best of our knowledge, this is the first epidemiological study to provide robust morbidity estimates of concurrent asthma/COPD in Germany. This is surprising since these patients represent a specific patient population with a greater disease burden as compared to individuals with asthma or COPD only8,12.
We observed that 1.50% of the general population was affected by concurrent diseases, corresponding to the absolute number of approximately 608,000 SHI-patients in Germany. The post-stratification weighting—which aims to adjust for possible demographic differences between the study and the source population and thus to provide a nationally representative estimate—resulted in a slightly lower prevalence of 1.39%. Recently, Hosseini et al. reported a global pooled prevalence of ACO in the general population of 2.0% (95% CI: 1.4–2.6%) with the lowest and highest estimates of 0.3% (the UK) and 5.0% (Australia), respectively11. The pooled estimate was based on 27 studies from mostly industrialized countries involving primarily adult study participants from 12 European studies (none from Germany). Thus, our weighted estimate of 1.39% is slightly lower than the pooled estimate reported by Hosseini et al., but lies within the 95% confidence interval. It is also in a good agreement with large-scale studies from Canada (1.6%, study participants aged 30+ years)13, Denmark (1.2%, 50–64 years)14, South Korea (1.4%, 40+ years)15 and the Netherlands (1.3%, 45–65 years)16. In addition, it should be noticed that our estimate was based on a nationwide population-based sample and can thus be considered highly representative.
According to previous studies, ACO affects on average every third asthma patient and every fourth COPD patient6. However, the prevalence estimates from international studies vary as well. In the above mentioned systematic review Hosseini et al. reported ACO estimates in asthma and COPD adult patients ranging between 11 and 51% and between 13 and 55%, respectively11. We observed comparable estimates of concurrent asthma/COPD in asthma and COPD patients (about 23%). In other words, every forth patient with asthma and COPD displayed concurrent diagnoses. The large variations in prevalence estimates across studies may be explained by varying case definitions but also by other methodological differences (e.g., study design and involved populations)16. A uniform, broadly accepted definition of ACO does not yet exist. A joined endeavor of GINA and GOLD resulted in a clinical description of ACO which involves “persistent airflow limitation with several features usually associated with asthma and several features usually associated with COPD”2. A few research groups published case definitions and diagnostic criteria based upon expert consensus which are restricted to certain countries17,18. Previous studies used various definitions based on laboratory findings, symptoms or diagnoses19. In the current analysis we used nationwide outpatient claims data which contain diagnoses of asthma and COPD coded according to the ICD-10-GM classification20. There is no specific ICD-10 code for ACO, and we used a combination of asthma and COPD diagnoses to define an overlap. We applied a very conservative case definition (diagnoses in at least two quarters) to largely exclude false positive cases. This approach is widely accepted in analysis of routine-based claims data and has already been used in studies on asthma and COPD21,22 and rather under- than overestimates morbidity. Our approach of defining the overlap is rather indirect and should be considered as approximation to an epidemiological prevalence assessed in a study design with objectively measured parameters. Nevertheless, our prevalence is similar to estimates from other studies which applied case definitions based on objectively measured parameters.
Comorbid disorders in patients with asthma or COPD have been extensively examined. Asthma is associated with allergic diseases such as allergic rhinitis, allergic conjunctivitis and atopic dermatitis23. In addition, asthmatics have higher risk of further respiratory, but also cardiovascular and metabolic diseases23. Due to the common risk factors (in particular smoking), COPD is associated with bronchial carcinoma and coronary heart disease24. Not surprisingly, mental disorders such as depression and anxiety are very common among both, asthma and COPD patients25,26. Research on comorbid disorders in patients with ACO is lacking. Existing evidence shows that patients with ACO have a more rapid disease progression than patients with asthma or COPD alone1. As a consequence, they have worse quality of life and higher rates of health care utilization. We found a few studies that focused only on specific comorbid disorders. For example, van Boven et al. examined the prevalence for 16 comorbid disorders in a sample of ACO patients treated in primary care in Spain (n = 5093)27. The most prevalent comorbid disorders in this study were hypertension (49%), anxiety (38%), diabetes (22%), osteoporosis (19%) and allergic rhinitis (16%). Ding et al. compared selected comorbid disorders in three patient groups (asthma, COPD and ACO) and observed that patients with ACO (n = 523) had higher prevalence of hypertension (56%), elevated cholesterol/hyperlipidemia (29%), arthritis (17%), depression (21%), obesity (13%) and gastroesophageal reflux disease (19%) (compared to asthma patients)10. In addition, ACO patients had higher estimates of diabetes (22%) and osteoporosis (11%) as compared to COPD-only patients10. In contrast to the above mentioned studies that focused on selected comorbid disorders, we applied a comprehensive exploratory approach by examining a wide spectrum of comorbid disorders (1060 disorders from 14 disease groups). Comorbid disorders were examined at the level of the first three characters of the ICD-10 code, which represent the main disease category. Overall, comorbid disorders were very common in patients with concurrent asthma/COPD as compared to the control group. Notably, 83% of the examined comorbid disorders were still significantly higher in patients with concurrent asthma/COPD after Bonferroni correction. We found disorders involving all body systems, including mental diseases. The most prevalent were disorders of the circulatory system as well as metabolic and musculoskeletal disorders. In addition, every second patient with asthma/COPD suffered from mental, gastrointestinal and other pulmonary diseases.
The large nationwide sample allowed us to identify comorbid disorders with a small size effect (i.e., OR < 1.5), but still significant after correction for multiple testing, which could not be observed in other studies with smaller sample sizes. Common risk factors may explain the coexistence of some diseases (e.g., smoking and bronchial carcinoma). Persistent systemic inflammation in ACO patients may contribute to the development of cardiovascular diseases28. Therapy with inhaled corticosteroid may explain the higher risk of osteoporosis as observed in COPD patients29, although the evidence is controversial30.
Strengths and limitations
We made use of nationwide claims data comprising information of about 86% of the total German population. Thus, prevalence estimates can be considered highly representative. In addition, data contain all diagnoses made in an outpatient setting which allows to obtain a nearly complete picture of the comorbidity profile of patients with concurrent asthma/COPD. We applied a hypothesis-free approach to examine the full spectrum of comorbid disorders in these patients. These are unique strengths of the study; to the best of our knowledge, such approach has never been done before.
Our study has potential limitations. Our analysis was based on outpatient claims data containing diagnoses coded according to the ICD-10-GM classification. There is no specific code for ACO, instead, we used the codes for asthma (J45) and COPD (J44) to indirectly define an overlap. Objectively measured, clinical and laboratory (e.g., spirometry) data were not available to validate the diagnosis. In addition, a short time period of one year in which the cases were identified might result in misclassification since diagnoses made outside this period were not considered. However, our sample comprised nearly 99% of all SHI-individuals in Germany in 2017. Also, a conservative case definition applied in our study (i.e., at least two diagnoses of each, asthma and COPD, in different quarters of the year) might further contribute to misclassification and result in prevalence underestimation. Thus, some patients, e.g. with well-controlled asthma might not be diagnosed in 2017 even if they visited a physician in that year. On the other hand, claims data are primarily collected for reimbursement purposes and not for morbidity estimation and are known to overestimate the true epidemiological prevalence, in particular, if a case definition is only based on a single diagnosis. Previous research on asthma and COPD based on routine data thus applies a more conservative case definition21,22,31,32,33. Furthermore, per case definition (i.e., diagnoses in at least two different quarters), patients with concurrent asthma/COPD diagnoses have higher rates of health care contacts, in particular, if patients visit different physicians as compared to controls. Thus, the chance of getting other (comorbid) diagnoses may be higher in these patients. In addition, we were restricted to the variables available in our dataset (i.e., sex, age and region of residence). Other potentially confounding variables such as socio-economic status were not available in the data. Finally, it has to be mentioned that some of the associations might still be false positive even after the correction for multiple testing. On the contrary, some real associations may have been overlooked due to the very strict p value.
Conclusions
This is the first study to provide morbidity estimates of possible ACO in Germany and examine its full spectrum of comorbid disorders. We observed the relatively low prevalence of concurrent asthma/COPD diagnoses at the national level. However, this population group was characterized by a considerable disease burden. (Multi)morbidity is very common in these patients and requires a special attention of researchers and clinicians. Due to the broad comorbidity spectrum, these patients might benefit from a multidisciplinary care approach. Timely identification of comorbid disorders may help to improve their clinical course, prognosis and quality of life.
Methods
Data and study population
The present study is based on outpatient claims data received from all regional Associations of Statutory Health Insurance Physicians (ASHIPs) in Germany. In total, there are 17 ASHIPs, of whom 15 coincide with 15 German federal states whereas two ASHIPs exist in the federal state of North Rhine-Westphalia. The data contain diagnoses of all SHI-individuals in Germany who visited a SHI-authorized physician in the year 2017. The diagnoses are coded according to the German modification of the 10th edition of the International Classification of Diseases and Related Health Problems (ICD-10-GM). The study population comprises insurees with available information on sex, age (40+ years) and region of residence (N = 40,477,745). The German population consisted of 47,185,969 inhabitants over 40 years in 201734, 41,062,196 of them were statutory insured35. Thus, the study population included approx. 86% of the total German population and nearly 99% of the total SHI-population.
Case ascertainment and prevalence estimation
We defined a patient with concurrent diagnoses, when each ICD-10 codes J44 ‘other chronic obstructive pulmonary disease’36,37 and J45 ‘asthma’21,31 were diagnosed in at least two different quarters in 2017, resulting in total of four diagnoses (i.e., two diagnoses of asthma in two different quarters and two COPD diagnoses in two different quarters). In addition, all diagnoses should have a diagnostic modifier “confirmed diagnosis” in contrast to ‘suspected disease’ or ‘cured disease’. The former is usually given for chronic disease cases and for those patients requiring pharmacological therapy38.
We first calculated the crude prevalence of concurrent diagnoses in patients with either asthma or COPD and in the whole study SHI-population. For the latter, we applied post-stratification weighting to obtain a nationally representative prevalence estimate. Sex and age (5-year age groups) distribution of the German population from the year 2017 obtained from the Federal Statistical Office34 was used to create the respective weights. A post-stratification weighting was only used in the total sample of the SHI-population to estimate a nationally representative prevalence of concurrent asthma/COPD diagnoses.
Comorbidity profile
Using the case–control study design we compared comorbid disorders among patients with and without concurrent diagnoses (i.e., a control group). A control group was retrieved from a sample of SHI-individuals who also visited a SHI-authorized physician in 2017 for reasons other than asthma and/or COPD. We selected SHI-insurees without a single diagnosis of asthma and/or COPD with available information on sex, age and region of residence (ASHIP). Of them, we only retrieved individuals matched by sex, age and regional ASHIP with the highest case-to-control ratio of 1:9 (n = 5,471,676). For all individuals, i.e., with and without asthma/COPD, we extracted all diagnoses using the procedure mentioned above (i.e., diagnoses with the highest diagnostic certainty “confirmed diagnosis” in at least two quarters of 2017). The ICD-10 consists of 22 chapters representing broad disease categories with codes containing 3–5 characters20. In this analysis we used codes with the first three characters, which represent the main disease category (e.g., the code A01 for typhoid and paratyphoid fevers). We included the first 14 chapters of the ICD-10-GM classification, which represent specific diseases (Fig. 3). The remaining chapters of the ICD-10-GM classification were excluded from the further analysis because they represent unspecific symptoms and conditions not directly relevant with regards to asthma/COPD (e.g., injuries, accidents, etc.). We undertook ranking of comorbid disorders among patients with asthma/COPD based on disease prevalence to identify the most relevant comorbid diseases. This was done by disease groups (14 chapters) and diseases based on the first three characters of the ICD-10 code. Furthermore, we compared the prevalence of comorbid disorders in patients with asthma/COPD diagnoses and in the control population separately for each ICD-10 code (at the level of three characters) and for each disease group. We estimated odds ratios (OR) and corresponding 95% confidence intervals (CI) for each of the 1,060 comorbid diseases in patients with and without asthma/COPD. Due to the exploratory character of this analysis, we applied the Bonferroni correction to address the problem of multiple testing (n = 1060 disorders)39. A Bonferroni corrected p-value of 4.72 × 10–5 (i.e., 0.05/1,060 disorders) was considered statistically significant.
Data availability
The datasets analysed during the current study are not publicly available due to data protection regulations by the German Social Security Code (Sozialgesetzbuch (SGB) V).
References
Gibson, P. G. & Simpson, J. L. The overlap syndrome of asthma and COPD: what are its features and how important is it?. Thorax 64, 728–735 (2009).
GINA, GOLD. Diagnosis of Diseases of Chronic Airflow Limitation: Asthma, COPD and Asthma-COPD Overlap Syndrome (ACOS). A joint project of GINA and GOLD. https://goldcopd.org/wp-content/uploads/2016/04/GOLD_ACOS_2015.pdf (2015).
GINA, GOLD. Diagnosis and Initial Treatment of Asthma, COPD and Asthma-COPD Overlap. A joint project of GINA and GOLD updated April 2017. https://ginasthma.org/wp-content/uploads/2019/11/GINA-GOLD-2017-overlap-pocket-guide-wms-2017-ACO.pdf (2017).
Uchida, A., Sakaue, K. & Inoue, H. Epidemiology of asthma-chronic obstructive pulmonary disease overlap (ACO). Allergol. Int. 67, 165–171 (2018).
Kauppi, P. et al. Overlap syndrome of asthma and COPD predicts low quality of life. J. Asthma 48, 279–285 (2011).
Leung, J. M. & Sin, D. D. Asthma-COPD overlap syndrome: pathogenesis, clinical features, and therapeutic targets. BMJ 358, j3772 (2017).
Yeh, J. J., Wei, Y. F., Lin, C. L. & Hsu, W. H. Association of asthma-chronic obstructive pulmonary disease overlap syndrome with coronary artery disease, cardiac dysrhythmia and heart failure: a population-based retrospective cohort study. BMJ Open 7, e017657 (2017).
Hardin, M. et al. The clinical features of the overlap between COPD and asthma. Respir. Res. 12, 127 (2011).
Menezes, A. M. B. et al. Increased risk of exacerbation and hospitalization in subjects with an overlap phenotype: COPD-asthma. Chest 145, 297–304 (2014).
Ding, B. & Small, M. Treatment trends in patients with asthma-COPD overlap syndrome in a COPD cohort: findings from a real-world survey. Int. J. Chron. Obstruct. Pulmon. Dis. 12, 1753–1763 (2017).
Hosseini, M., Almasi-Hashiani, A., Sepidarkish, M. & Maroufizadeh, S. Global prevalence of asthma-COPD overlap (ACO) in the general population: a systematic review and meta-analysis. Respir. Res. 20, 229 (2019).
Nielsen, M., Barnes, C. B. & Ulrik, C. S. Clinical characteristics of the asthma-COPD overlap syndrome - a systematic review. Int. J. Chron. Obstruct. Pulmon. Dis. 10, 1443–1454 (2015).
Senthilselvan, A. & Beach, J. Characteristics of asthma and COPD overlap syndrome (ACOS) in the Canadian population. J. Asthma 56, 1129–1137 (2019).
Baarnes, C. B., Andersen, Z. J., Tjonneland, A. & Ulrik, C. S. Incidence and long-term outcome of severe asthma-COPD overlap compared to asthma and COPD alone: a 35-year prospective study of 57,053 middle-aged adults. Int. J. Chron. Obstruct. Pulmon. Dis. 12, 571–579 (2017).
Kang, H. R. et al. Differences in the risk of mood disorders in patients with asthma-COPD overlap and in patients with COPD alone: a nationwide population-based retrospective cohort study in Korea. Respir. Res. 20, 80 (2019).
Bonten, T. N. et al. Defining asthma-COPD overlap syndrome: a population-based study. Eur. Respir. J. 49, 1602008 (2017).
Padrao, E. et al. Asthma-COPD overlap: a Portuguese survey. Pulmonology 24, 174–181 (2018).
Soler-Cataluna, J. J. et al. Consensus document on the overlap phenotype COPD-asthma in COPD. Arch. Bronconeumol. 48, 331–337 (2012).
Tho, N. V., Park, H. Y. & Nakano, Y. Asthma-COPD overlap syndrome (ACOS): a diagnostic challenge. Respirology 21, 410–418 (2016).
German Institute of Medical Documentation and Information. The International Statistical Classification Of Diseases and Related Health Problems, 10th revision, German Modification (ICD-10-GM). https://www.dimdi.de/dynamic/en/classifications/icd/icd-10-gm/index.html (2019).
Hasford, J. et al. Persistence with asthma treatment is low in Germany especially for controller medication: a population based study of 483,051 patients. Allergy 65, 347–354 (2010).
Shin, J. Y. et al. Changing patterns of adult asthma incidence: results from the National Health Insurance Service-National Sample Cohort (NHIS-NSC) database in Korea. Sci. Rep. 8, 15052 (2018).
Heck, S. et al. High probability of comorbidities in bronchial asthma in Germany. NPJ. Prim. Care Respir. Med. 27, 28 (2017).
Cavailles, A. et al. Comorbidities of COPD. Eur. Respir. Rev. 22, 454–475 (2013).
Dudeney, J. et al. Anxiety in youth with asthma: a meta-analysis. Pediatr. Pulmonol. 52, 1121–1129 (2017).
Yohannes, A. M. & Alexopoulos, G. S. Depression and anxiety in patients with COPD. Eur. Respir. Rev. 23, 345–349 (2014).
van Boven, J. et al. Prevalence of comorbidities in patients with asthma-COPD overlap syndrome (ACOS) in primary care. Eur. Resp. J. 46, OA4786 (2015).
Fu, J. J., McDonald, V. M., Gibson, P. G. & Simpson, J. L. Systemic inflammation in older adults with Asthma-COPD overlap syndrome. Allergy Asthma Immunol. Res. 6, 316–324 (2014).
Scanlon, P. D. et al. Loss of bone density with inhaled triamcinolone in Lung Health Study II. Am. J. Respir. Crit. Care Med. 170, 1302–1309 (2004).
Oh, J. Y. et al. Osteoporosis in patients with asthma-chronic obstructive pulmonary disease overlap syndrome. Tuberc. Respir. Dis. (Seoul. ) 81, 73–79 (2018).
Akmatov, M., Holstiege, J., Steffen, A. & Bätzing, J. Trends and regional distribution of outpatient claims for asthma, 2009–2016 Germany. Bull. World Health Org. 98, 40–51 (2020).
Pollmanns, J. et al. Impact of disease prevalence adjustment on hospitalization rates for chronic ambulatory care-sensitive conditions in Germany. Health Serv. Res. 53, 1180–1202 (2017).
Gray, C. L. et al. Associations between environmental quality and adult asthma prevalence in medical claims data. Environ. Res. 166, 529–536 (2018).
Federal Statistical Office. Population size: Germany. https://www.destatis.de (2019).
The Federal Health Reporting: Joint Service of the Robert Koch Institute and Federal Statistical Office. Numbers of members and jointly insured family members of the statutory health insurance on July 1st in 2017. https://www.gbe-bund.de (2017).
Kauhl, B. et al. Who is where at risk for Chronic Obstructive Pulmonary Disease? A spatial epidemiological analysis of health insurance claims for COPD in Northeastern Germany. PLoS ONE 13, e0190865 (2018).
Schwarzkopf, L. et al. Impact of chronic ischemic heart disease on the health care costs of COPD patients: an analysis of German claims data. Respir. Med. 118, 112–118 (2016).
National Association of Statutory Health Insurance Physicians. Diagnosis certainty and site location. Dtsch. Arztebl. 108, A271-274 (2011).
Shaffer, J. Multiple hypothesis testing. Annu. Rev. Psychol. 46, 561–584 (1995).
Acknowledgements
The authors would like to thank the 17 regional Associations of Statutory Health Insurance Physicians in Germany for provision of data.
Author information
Authors and Affiliations
Contributions
M.K.A and T.E designed the study and analysed the data. M.K.A wrote an initial version of the manuscript. J.H, A.S, D.S and J.B critically reviewed the manuscript. J.B supervised the project. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Akmatov, M.K., Ermakova, T., Holstiege, J. et al. Comorbidity profile of patients with concurrent diagnoses of asthma and COPD in Germany. Sci Rep 10, 17945 (2020). https://doi.org/10.1038/s41598-020-74966-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-74966-1
This article is cited by
-
Chronisch obstruktive Lungenerkrankung (COPD) und obstruktive Schlafapnoe (OSA) – Prävalenz des COPD-OSA-Overlap Syndroms in Deutschland seit 2017
Somnologie (2023)
-
COPD profiles and treatable traits using minimal resources: identification, decision tree and stability over time
Respiratory Research (2022)
-
Patients at high risk for a severe clinical course of COVID-19 — small-area data in support of vaccination and other population-based interventions in Germany
BMC Public Health (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.